Pathophysiology II - Exam 4 - Dementia 💭
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
what is dementia?
a syndrome of progressive memory loss with 1+ cognitive deficit that interferes with occupation or social functioning
- common, but NOT normal!
what is the most common cause of dementia in older adults?
Alzheimer's disease
- 8-10 year survival after being diagnosed with AD
one of the common etiologies of Alzheimer's (AD) is an alteration in chromosomes; which chromosomes are affected, and how do these alterations cause disease?
chromosomes 1, 14, and 21; impact the processing of amyloid precursor proteins (APP: α, β, and γ-secretase to β-amyloid proteins)
--- α-secretase: responsible for non-pathologic fragments
--- alterations in β or γ-secretase may result in pathological fragments
one of the common etiologies of Alzheimer's (AD) is apolipoprotein E (APOE); which subtype is the biggest risk?
APOE4
- 1 allele: 2-3x risk of AD
- 2 alleles: 12x risk of AD
- risk of earlier onset AD
what are some environmental risk factors of AD?
- age (65+ yo)
- reduced brain reserve capacity (developmental disability)
- head injury (CTE, boxers, football players, etc.)
- Down's syndrome
- depression
- mild cognitive impairment
- risk for vascular disease (obesity, HTN, hyperlipidemia, etc.)
what are the common microscopic features observed with AD?
- neurofibrillary tangles (NFTs)
- amyloid plaques (drug target!)
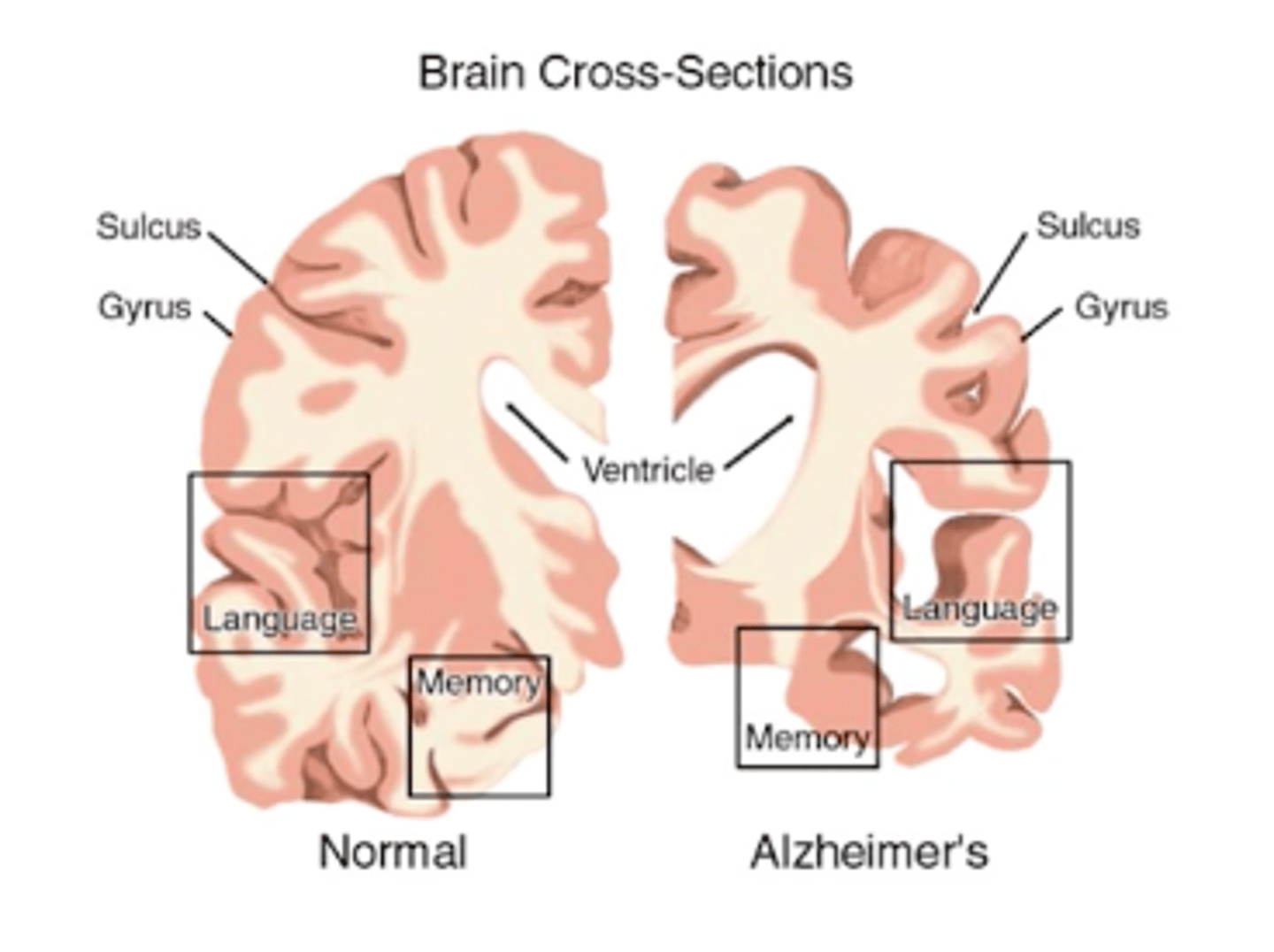
what changes to brain structure and neurons are observed with AD?
cortical atrophy and loss of neurons
- parietal and temporal lobes
- ventricular enlargement → hydrocephalus
what neurochemical changes are observed with AD?
decreased choline acetyltransferase
what are amyloid plaques? describe the amyloid cascade hypothesis of AD
patches of degenerating nerve terminals around a core of β-amyloid protein (Aβ)
- EC lesions found in the brain and cerebral vasculature
- form due to an imbalance between Aβ production and clearance, leading to accumulation of the proteins
- it is unknown if Aβ inside or outside of plaques is responsible for pathogenesis!
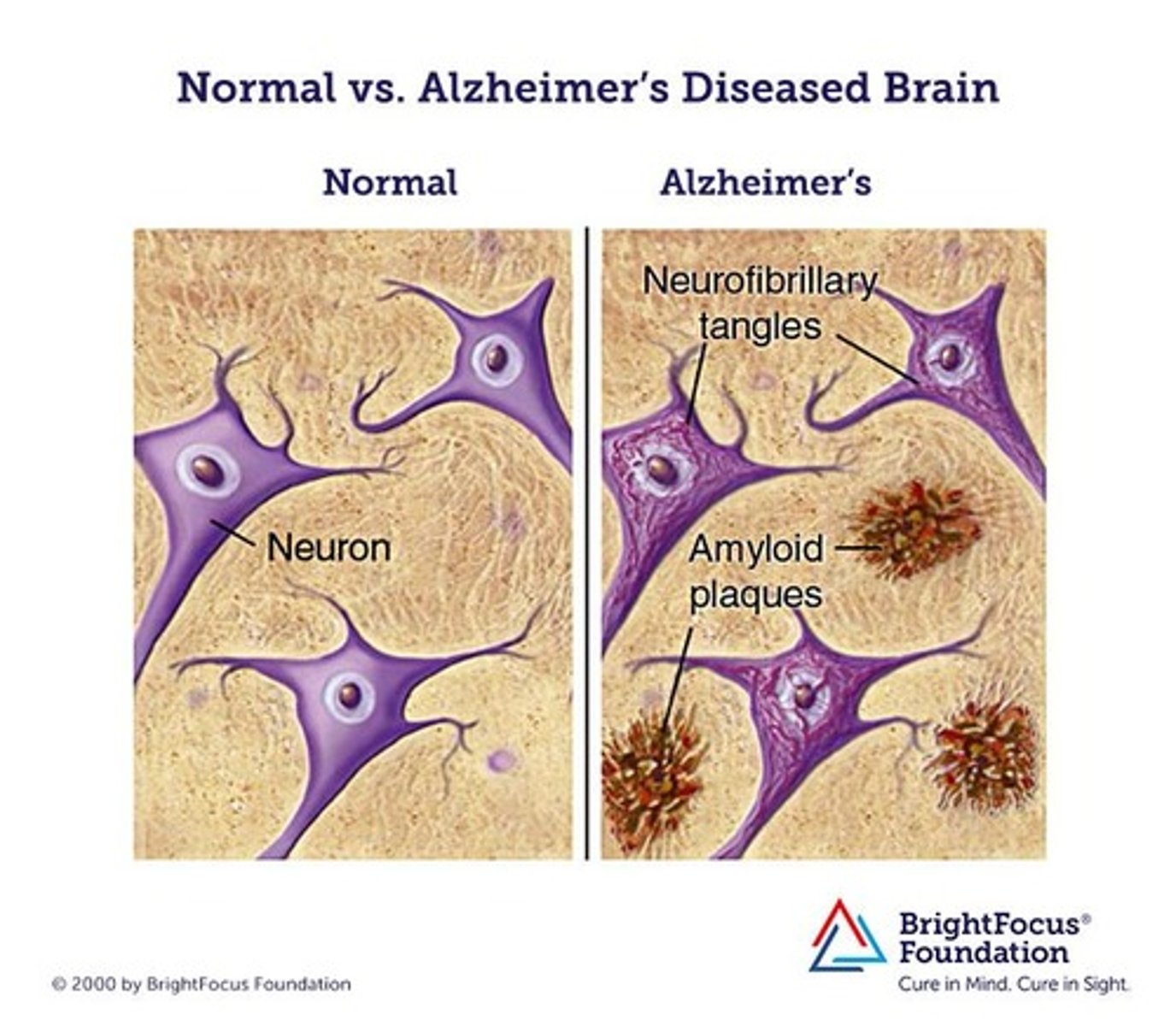
what are neurofibrillary tangles (NFTs)? what protein is involved in formation?
abnormal fibrous inclusions within pyramidal neurons
- found in the cytoplasm of cells in the hippocampus and cerebral cortex
- NFT density correlates with disease severity
- caused by Tau Proteins, which normally support microtubules in neurons
--- if hyper-phosphorylated, it loses its helical pattern and can no longer bind to the microtubules, leading to their collapse
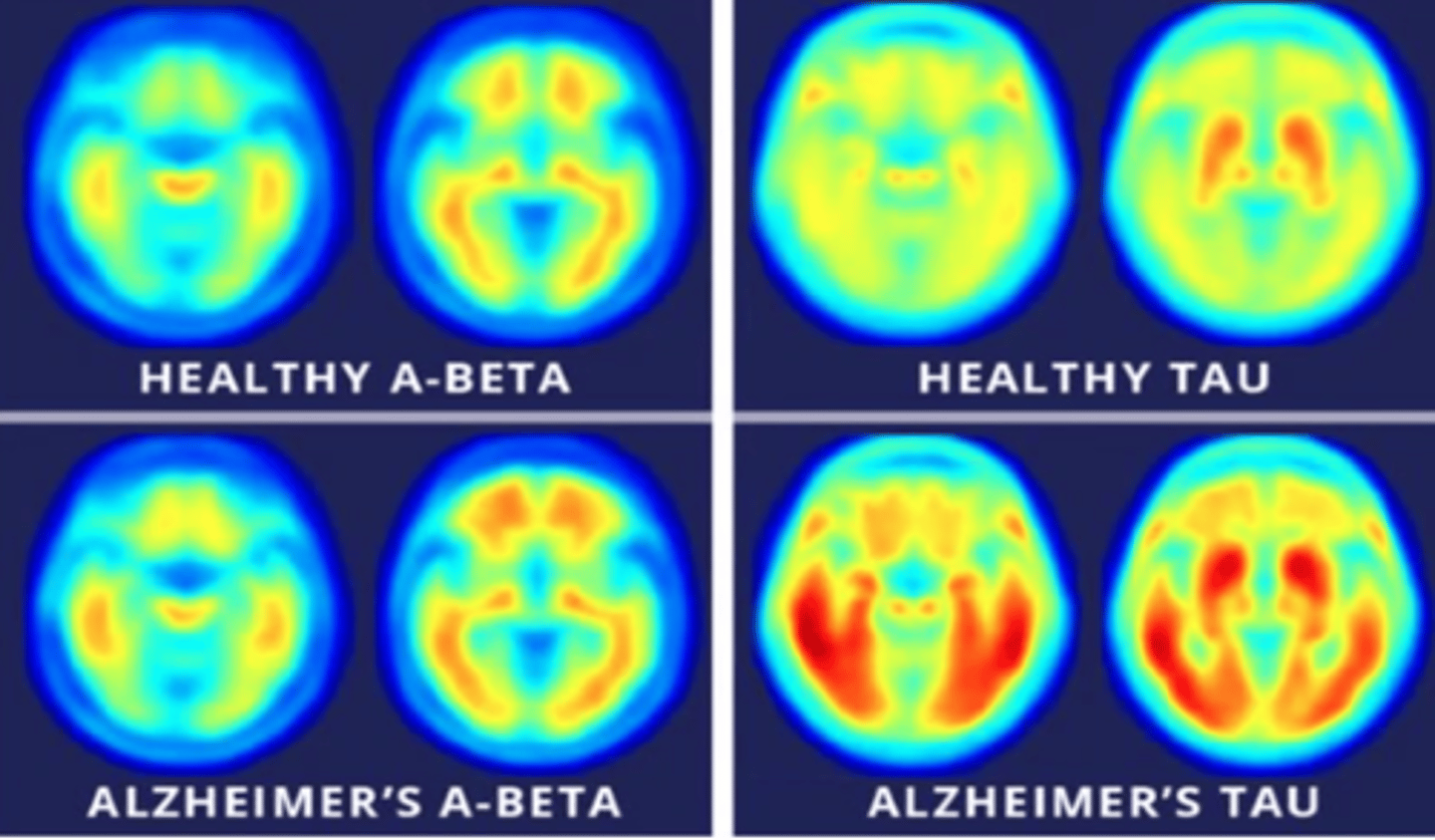
what are the 3 primary locations in which plaques and tangles are found in AD?
- neocortex → part of the cerebral cortex
- hippocampus → part of the limbic system within the temporal lobe
- amygdala → located within the temporal lobe
what are the neocortex, hippocampus, and amygdala responsible for in the brain?
- neocortex → sensory perception, language, motor commands, spatial reasoning
- hippocampus → short-term memory, spatial reasoning
- amygdala → memory, emotional processing
how might inflammatory mediators play a role in the pathophysiology of AD?
amyloid deposition is associated with the release of cytokines and radical species, which may increase inflammation and promote neuronal injury
what are the 2 main components of the cholinergic hypothesis of AD?
- many neuronal paths are destroyed → prominent loss of cholinergic neurons; correlated with severity
- loss of nicotinic R's in the hippocampus and cortex → presynaptic R's control the release of ACh, glutamate, 5-HT, and NE
what changes are observed in NT's like 5-HT neurons, MAO type B, and glutamate in the brains of AD patients?
- decreased 5-HT neurons
- increased MAO type B → metabolizes DA
- abnormal glutamate → excitatory NT that can become neurotoxic through the release of IC Ca2+; altered by blockage of NMDA R
what conditions are associated with an increased risk of vascular dementia?
- HTN
- DM → associated with metabolic syndrome, toxic glucose metabolites, and disturbances in insulin signaling
- increased LDL, decreased HDL
how might vascular disease lead to dementia?
the lack of healthy brain tissue and adequate blood flow may...
- impair the delivery of nutrients
- reduce clearance of Aβ
how might oxidative stress, mitochondrial dysfunction, and loss of estrogen lead to dementia?
- oxidative stress → accumulation of free radicals
- mitochondrial dysfunction → disruption of neuronal energy metabolism
- loss of estrogen → postmenopausal women are at a higher risk; estrogen supports neuronal growth!
T/F: the onset of AD dementia is rapid, over days-weeks
FALSE
- onset is gradual; it can take years to realize the cognitive changes
- patients can compensate for minor changes for some time
- however, some patients progress faster than others
list some of the cognitive manifestations of AD dementia
- memory loss (recall, loss of items; short-term degrades before long-term)
- aphasia (loss of ability to understand or express speech)
- apraxia (unable to perform tasks or movements when asked)
- agnosia (can't recognize and identify objects, persons, or sounds)
- disorientation and inadaptability (don't do well in new environments!)
- impaired executive function
list some of the behavioral manifestations of AD dementia
- insomnia and sun-downing (worsens at night)
- wandering, falling
- inability to perform ADLs
- inappropriate social behavior
- emotion lability and depression
- restlessness, agitation
- aggressiveness and catastrophic reactions
- diminished driving skills
- delusion, hallucinations
- incontinence
- gait disturbances, immobility
- indifferences to food
- inability to communicate
what is the primary evidence of cognitive decline? what is explicitly excluded?
complex attention, executive function, learning/memory, language, perceptual-motor, or social cognition
- deficits interfere with independence in ADLs/IADLs
- delirium is EXCLUDED!
AD dementia is primarily a ____________ diagnosis
clinical Dx
- mostly reliant on memory complaints and functional disability, often provided by family/caregivers
what must be ruled out when assessing a patient for AD dementia?
- depression
- vitamin B12 and folate deficiency
- hyper-/hypo-thyroidism
- neuro-syphillis
- HIV
- anemia
- renal and hepatic dysfunction
- electrolyte imbalance
AD dementia diagnoses can be confirmed via...?
- brain biopsy (AFTER patient has passed)
- in vivo plaque detection
what are the 3 main scales used for assessment of AD dementia patients? which is the only one used more in clinical practice than in research (starred)?
- global deterioration scale (GDS; shows the stages of cognitive decline)
- Alzheimer's disease assessment scale (ADAS-cog)
- ★Folstein mini-mental status exam (MMSE; staging is mild, moderate, or severe)
what MMSE scores classify a patient as mild, moderate, or severe? what characteristics are often observed in patients under each classification?
MILD: score 26-21
- decline is IADLs
- difficulty remembering recent events
MODERATE: score 20-10
- requires help with ADLs
- disoriented, agitated, paranoid
- forgets details of their own life and names of family members
SEVERE: score 9-0
- lost ability to speak, walk, and feed themselves
- incontinent, requires 24-hour care (may also be needed in moderate patients)
what medications are associated with cognitive impairment?
- benzodiazepines (ex: alprazolam)
- sedative hypnotics (ex: zolpidem)
- anticholinergics (ex: diphenhydramine)
- opioids (ex: morphine)
- antipsychotics
- anticonvulsants
what medications are associated with delirium?
- NSAIDs
- H2RA
- digoxin
- amiodarone
- steroids
what type of dementia accounts for 20-25% of dementias and is associated with HTN, DM, MI, and PVD? describe its onset and physical findings
vascular dementia
- onset can be sudden OR gradual
- NOT associated directly with atherosclerosis, but with infarcts throughout the brain
- infarcts may appear on CT scans
what is frontotemporal dementia? how does it often manifest?
global term for dementias that attack the frontal lobe
- may manifest as behavioral or personality changes
what is mild cognitive impairment (MCI)?
syndrome of memory complaints that can NOT be diagnosed as a dementia
- no trouble with ADLs, no behavioral changes, etc.
- 10-15% chance per year of progressing to AD