clinical pathophysiology midterm
1/91
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
92 Terms
what does the motor function assessment test for?
muscle strength
muscle size
muscle tone
spinal reflex activity
coordination of movement
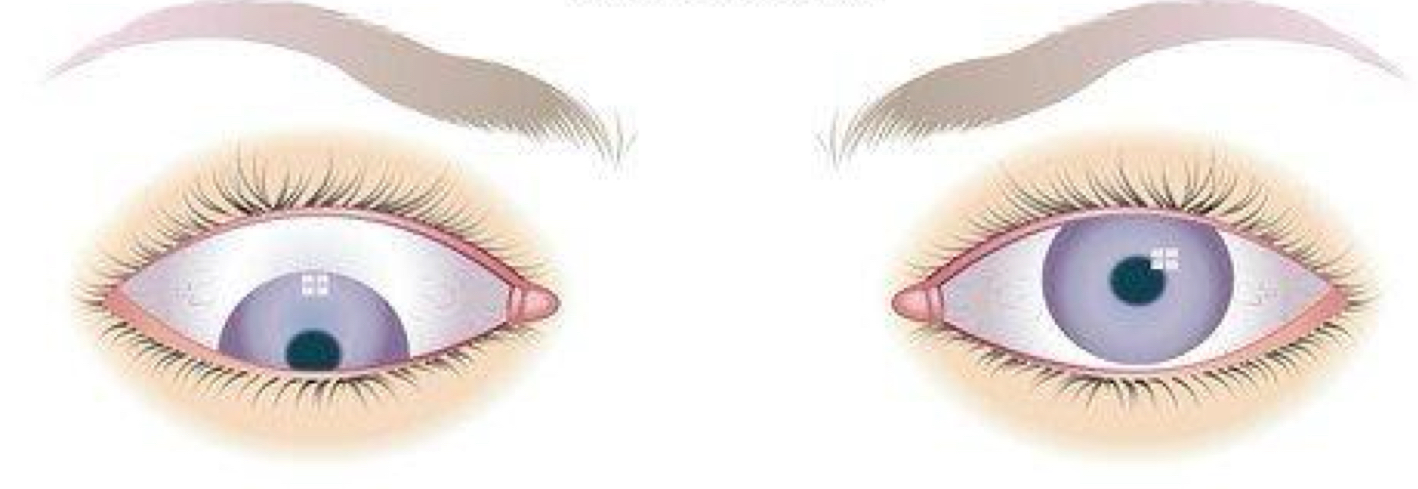
what is esotropia?
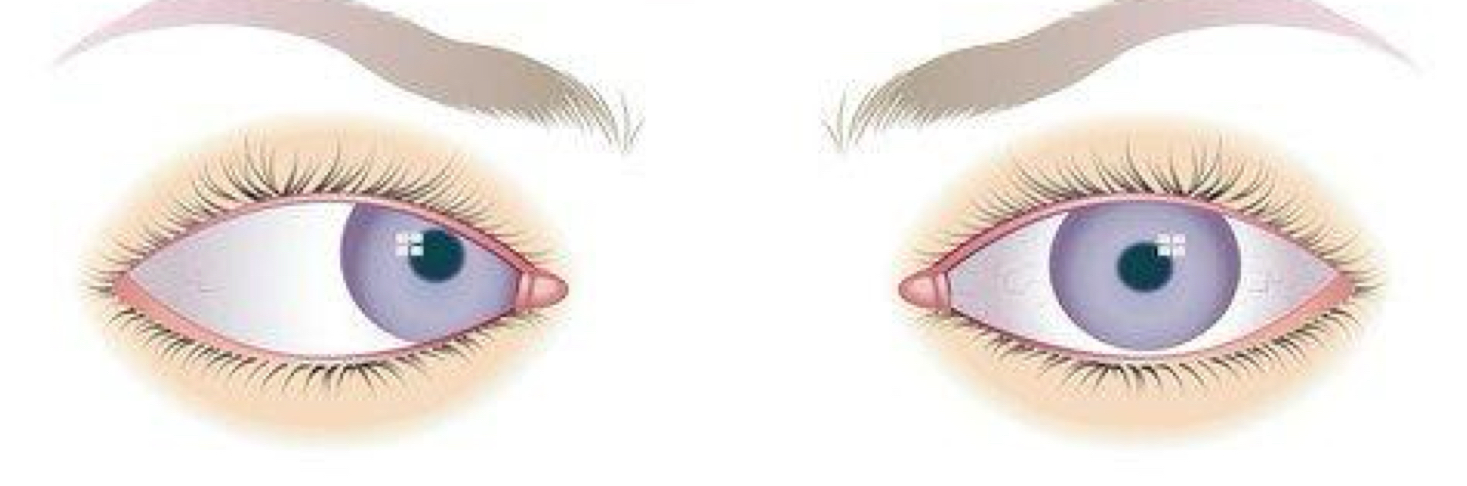
what is exotropia?
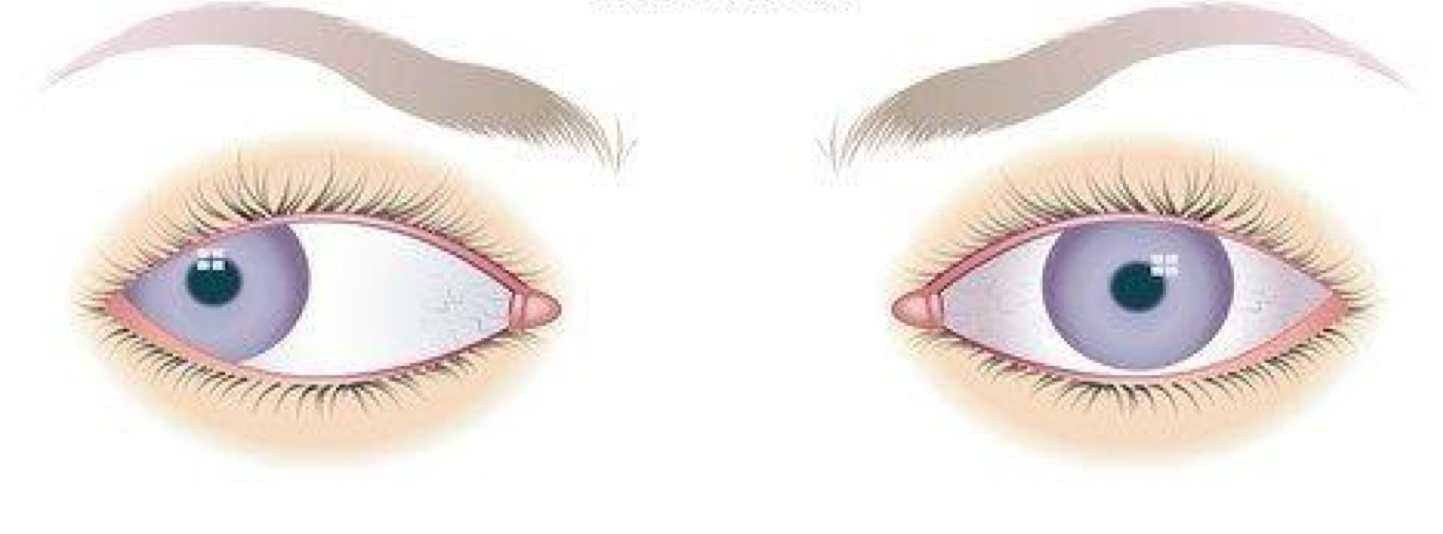
what is hypertropia?
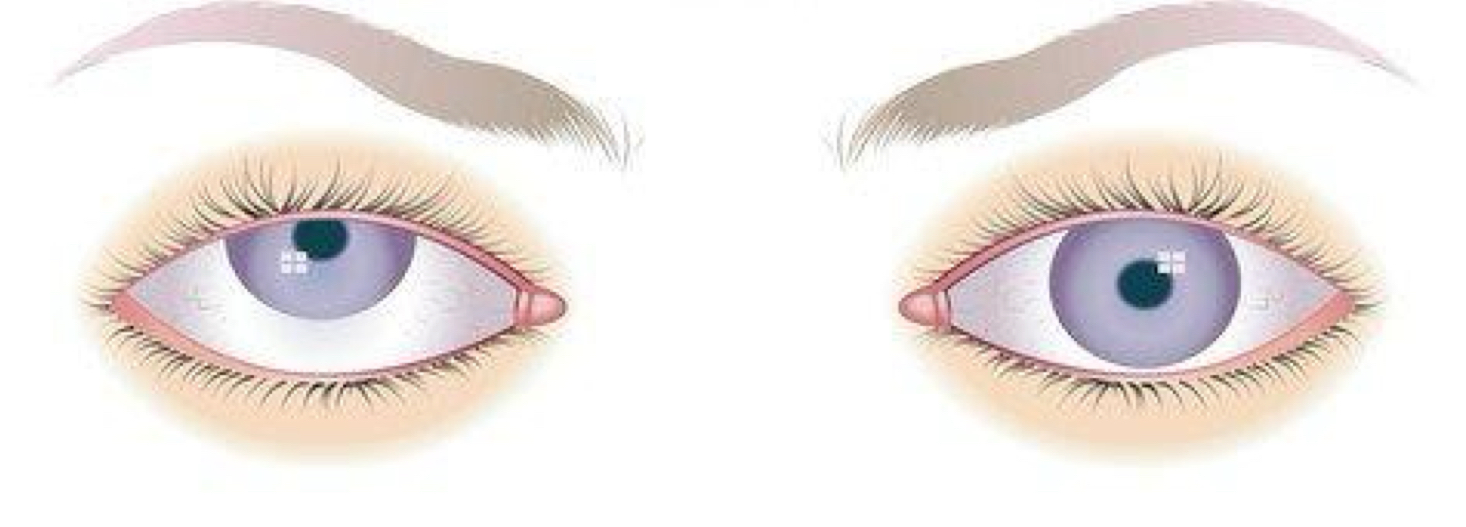
what is hypotropia?
what is penicillin?
treat streptococcal and staphylococcal infections, syphilis and gonorrhea
side effects: GI issues like nausea, vomiting, diarrhea, and abdominal pain
what are cephalosporins?
treat a variety of issues including urinary tract and respiratory tract infections
caution: may be contraindicated for people with allergies to penicillin
what are aminoglycosides?
treat infection with gram-negative bacteria
ex: gentamicin and tobramycin
adverse effects: ototoxicity and nephrotoxicity
what are tetracyclines?
treat various infections
contraindicated for pregnancy people and children under age 8
what are macrolides?
treat mild to moderate respiratory infections
ex: azithromycin
contraindicated for people who are lactating or who have hepatic dysfunction
what are fluoroquinolones?
treat gram-negative and gram-positive infections of the urinary and respiratory tracts
adverse reactions: tendon rupture and CNS effects
what are examples of isolation precautions?
contact
droplet
airborne
what are analgesics (a pharmacological treatment)?
drugs that act on the nervous system to decrease or eliminate pain without inducing loss of consciousness
do not cure the underlying cause
enable a person to achieve mobility after surgery, when exercises such as coughing or deep breathing may be required
what is neuropathic pain?
a type of chronic pain caused by nerve damage, often described as burning, stabbing, or tingling
what is neuralgia?
sharp, sudden pain along the path of a nerve, usually due to nerve irritation or damage
what is phantom limb pain?
sensations or pain felt in a limb that has been amputated, as if it is still present
what is the spinal cord?
function: transmits signals between the brain and body; controls reflexes
structure: a long, cylindrical structure extending from the brainstem to the lower back
role in neural function: involved in basic motor control and sensation; damage can lead to paralysis or loss of sensation
what is the brain stem?
function: regulates essential life functions such as heart rate, breathing, and swallowing
structure: includes the midbrain, pons, and medulla oblongata
role in neural function: acts as a communication pathway between the brain and spinal cord; controls autonomic functions, and manages reflexes
what is the motor cortex?
function: responsible for voluntary movement control
structure: located in the frontal lobe, specifically in the precentral gyrus
role in neural function: sends signals to the muscles to produce voluntary movements. damage can lead to motor impairments or paralysis
what is the cerebellum?
function: coordinates movement and maintains balance
structure: located at the back of the brain, below the occipital lobes
role in neural function: fine-tunes motor activity and ensures smooth, coordinated movements. damage can cause ataxia (loss of coordination)
what is muscle atrophy?
a skeletal muscle disorder that causes the weakening or shrinking of muscles due to disuse, injury, or disease
what is muscular dystrophy?
a skeletal muscle disorder where a group of genetic disorders causing progressive muscle weakness and degeneration
what is carpal tunnel syndrome?
a skeletal muscle disorder
caused by a compression of the median nerve in the wrist
leads to pain, numbness, and tingling in the hand
what is Guillain-Barre syndrome?
a skeletal muscle disorder
rare neurological disorder where the immune system attacks the peripheral nerves
leading to muscle weakness and paralysis
what is a herniated intervertebral disk?
a skeletal muscle disorder
condition where a disk in the spine ruptures or slips
causing pain and nerve compression
what is Parkinson’s disease?
a skeletal muscle disorder
a neurodegenerative disorder characterized by tremors, rigidity, and bradykinesia due to the loss of dopamine-producing cells in the brain
what happens during a cervical injury?
paralysis below neck (level of injury)
quadriplegia: 4 limbs paralyzed
quad=4; diplegia=sounds like paralyzed
breathing impaired - life threatening
happens to a lot of sports figures
what happens during a thoracic injury?
trunk of body
paraplegic ( 2 legs)
legs, pelvic organs
what happens during a lumbar injury?
legs and leaky bladder

what are examples of disruption of the autonomic nervous system function?
vasovagal response
autonomic dysreflexia
postural hypotension
what is vasovagal response?
a sudden drop in heart rate and blood pressure
leading to fainting, often triggered by stress, pain, or standing up too quickly
what is autonomic dysreflexia?
a potentially life-threatening condition in individuals with spinal cord injuries
causing a dangerously high spike in blood pressure due to overstimulation of the autonomic nervous system
what is postural hypotension?
a condition where blood pressure drops significantly when standing up from a sitting or lying position
leading to dizziness or fainting
what is the Glasglow coma scale’s eye response?
this relates to how awake and alert you are
spontaneous - 4
to sound - 3
to pain - 2
no response - 1
what is the Glasglow coma scale’s verbal response?
this tests how well certain brain abilities work, including thinking, memory, attention span and awareness of your surroundings
oriented - 5
confused - 4
coherent single words - 3
sounds - 2
no response - 1
what is the Glasglow coma scale’s motor response?
this part is about how well your brain can control muscle movement. it can also show if there are any issues with connections between you brain and the rest of your body
obeys commands - 6
moves to localized stimulation or pain - 5
withdrawal response to pain - 4
abnormal flexion - 3
abnormal extension - 2
no response - 1
what is a ischemic stroke?
results from blockage (clot)
what is a hemorrhagic stroke?
involves bleeding into/around the brain. associated with a higher mortality rate, more immediately dangerous due to increased ICP
what is conductive hearing loss?
hearing loss caused by problems in the outer or middle ear that prevent sound waves from reaching the inner ear
what is sensorineural hearing loss?
hearing loss due to damage to the inner ear (cochlea) or auditory nerve pathways
what is impacted cerumen?
accumulation of cerumen that causes a blockage in the ear canal
causes: overproduction of cerumen, use of cotton swabs, narrow ear canals, or hearing aids
symptoms:
hearing loss
ear fullness or pressure
earache
tinnitus (ringing in the ear)
dizziness or balance issues
management:
removal by a healthcare provider (avoid cotton swabs)
over-the-counter ear drops
irrigations
what is otitis externa (aka swimmer’s ear)?
infection or inflammation of the external auditory canal, often due to bacteria or fungi
causes:
water exposure (swimming, bathing)
mechanical injury (scratching, use of cotton swabs)
allergies or skin conditions (eczema, psoriasis)
symptoms:
itching in the ear canal
pain or tenderness, especially when touching the ear or pulling the earlobe
redness or swelling in the ear canal
discharge (clear, yellow, or pus-like)
management:
ear drops (antibiotic or antifungal)
pain relief (acetaminophen or ibuprofen)
avoid water exposure or scratching
what is barotrauma?
ear pain or damage resulting from rapid changes in air pressure or imbalances between the middle ear and the atmosphere
causes:
rapid ascent or descent (airplane, scuba diving)
Eustachian tube dysfunction
symptoms:
pain or discomfort in the ear
hearing loss
fullness or pressure
possible ear bleeding or rupture of the eardrum
management:
prevention: yawning, swallowing, chewing gum
use of nasal decongestants prior to flying or diving
if rupture occurs, seeks medical attention for possible ear drop treatment or antibiotics
what is otosclerosis?
a disease of the bone of the otic capsule that causes the formation of new spongy bone around the stapes and oval window
causes:
genetic factors (familial patterns)
more common in women and may worsen during pregnancy
symptoms:
gradual hearing loss, particularly in low frequencies
tinnitus
difficulty hearing in noisy environments
managements:
hearing aids to amplify sound
surgery (stapedectomy, removal of the affected bone)
in some cases, a prosthetic device to replace the stapes
what is the impact of hearing loss on language development?
even mild or unilateral hearing loss can affect a young child’s language development, with 1 to 3 babies per 1,000 born with permanent hearing loss
what causes hearing impairment in children?
it can be conductive or sensorineural. genetic causes contribute to about 50% of sensorineural hearing loss
what are postnatal causes for hearing loss in children?
after birth, sensorineural hearing loss can be caused by infections like bacterial meningitis or sepsis, toxins (e.g., ototoxic drugs), or trauma. congenital cytomegalovirus is a leading cause of hearing loss in newborns
what are screening and interventions for hearing loss in children?
the AAP recommend universal screening for all infants before 1 month of age, with intervention by 6 months. children with risk factors for delayed hearing loss should receive ongoing monitoring, and a developmental and speech evaluation is needed once hearing loss is identified
what is presbycusis?
refers to age-related degenerative hearing loss, affecting approximately 45% of individuals aged 65+
it’s a common social and health issue due to its high prevalence
characteristics: the hearing loss is gradual, bilateral, and typically involves high-frequency loss. it leads to difficulty in understanding speech, especially in noisy environments, and challenges with sound localization
causes and symptoms: likely results from a combination of aging, auditory stress, trauma, and otologic diseases. a common complaint is difficulty understanding speech rather than the inability to hear, especially for high-frequency sounds like beepers or alarms
screening and treatment: annual screening is recommended for older adults, typically using the question, “do you have a hearing problem?” hearing aids, lipreading, and assistive devices are effective treatments. Cochlear implants are recommended for severe hearing loss unresponsive to hearing aids
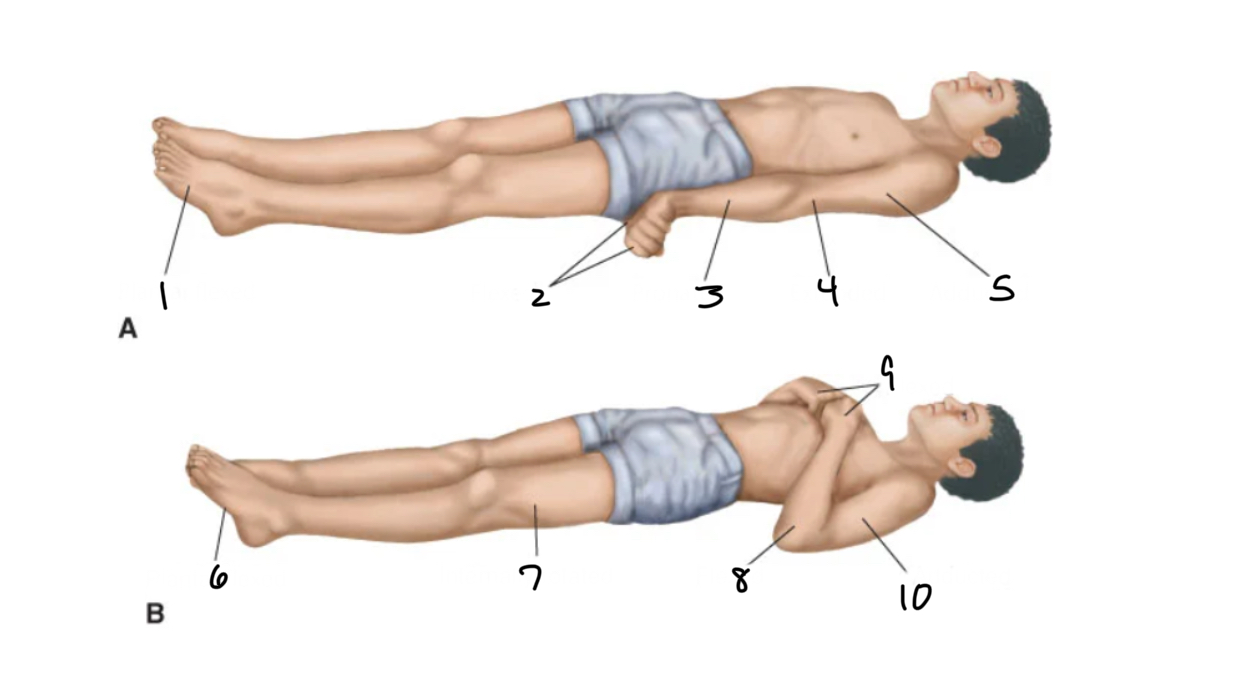
what does posture “A” mean?
patient is alive
plantar flexed
flexed
pronated
extended
adducted
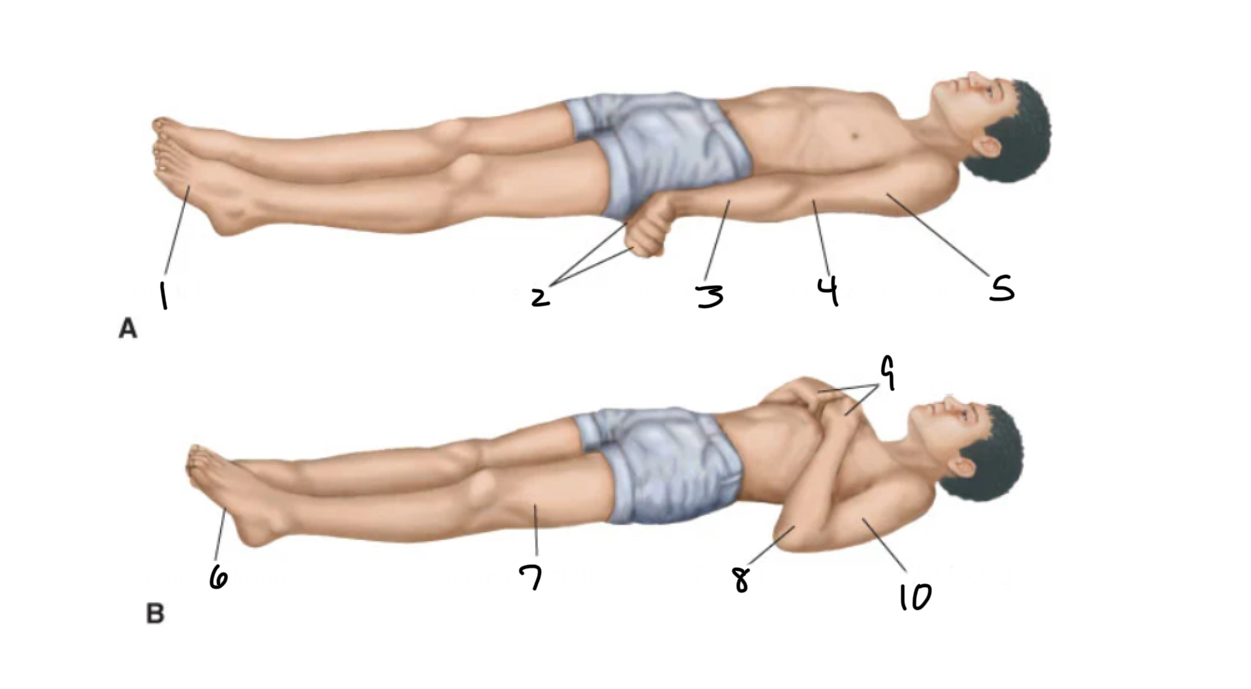
what does posture “B” mean?
patient is dead
plantar flexed
internally rotated
flexed
flexed
adducted
what is intraocular pressure?
the fluid pressure inside the eye, which helps maintain its shape and is important for proper eye function
what is glaucoma?
a group of eye conditions that cause damage to the optic nerve, often associated with high intraocular pressure, leading to vision loss
what is primary open-angle?
The most common form of glaucoma, when the eye’s drainage canals become clogged over time, causing gradual vision loss without noticeable symptoms
what is angle-closure?
a type of glaucoma where the iris is pushed forward blocking the drainage angle and causing a sudden increase in intraocular pressure, leading to acute pain and vision loss
sudden glaucoma
what is amblyopia?
a condition where one eye has poor vision due to abnormal visual development, even though the eye itself appears around
LAZY EYE
treatment: patches; eye drops
can lead to this if strabismus is left untreated
what is nystagmus?
involuntary, rhythmic oscillations or jerking of the eyes, which can be horizontal, vertical, or rotary
common in people with albinism
what is strabismus?
a condition where the eyes are not properly aligned, causing them to point in different directions (e.g., one eye may turn inward, outward, upward, and downward)
one eye is straying away
CROSS-EYED
treatment: patches over the strong eye to make the weak eye to work on muscles
what is myopia?
nearsightedness; eyeball too long
what is astigmatism?
Nonuniform curvature of the refractive medium with regard to the horizontal and vertical planes
the result of an asymmetric bowing of the cornea, or defects in the cornea, lens, or the retina
what is hyperopia?
farsightedness; eyeball is too short, the image is theoretically focused posterior to (behind) the retina
what is the Romberg test?
oldest sensory tests used to demonstrate disorders of static vestibular function
POSITIVE: bad—swaying w/ eyes opened or closed
NEGATIVE: good—no swaying
what is tinnitus?
is the perception of abnormal ear or head noises that are not produced by an external stimulus… RINGING
causes:
impacted cerumen— benign cause
noise-induced hearing loss
presbycusis
hypertension
atherosclerosis
head injury
cochlear or labyrinthine
diagnosis:
audiological exam
physical exam
MRI or CT scan
management:
white noise therapy
cognitive hearing therapy
stress management
what is peripheral vestibular apparatus?
contained in the bony labyrinth of the inner ear
detects movement and maintains balance
what is vertigo?
Disorders of vestibular function in which an illusion of motion occurs
frequently describe a sensation of spinning, “to-and-fro” motion, or falling.
dizziness or spinning
what is motion sickness?
form of normal physiologic vertigo. It is caused by repeated rhythmic stimulation of the vestibular system, such as that encountered in car, air, or boat travel
conflicting sensory input
brain sends mismatch signals from hearing and sight
what is meniere disease?
disorder of the inner ear because of distention of the endolymphatic compartment of the inner ear.
symptoms include hearing loss, vertigo, and tinnitus.
What is the normal WBC?
4,500-11,000
what is the normal hemoglobin count?
11-18 g/dL
what is the normal hematocrit percentage in women?
36-44%
what is the normal hematocrit percentage in men?
41-50%
what is the normal platelet count?
150,000-450,000
What is the complete blood count (CBC)?
RBC, WBC, hemoglobin, hematocrit, and platelets
hemoglobin and hematocrit: H&H blood tests are often performed to rule out anemia
what is the importance of type & screening?
identifies patient’s blood type and presence of antibodies (follow facility policy)
what is blood type?
the patient’s RBC are types for their ABO and Rh (D) blood type
what are antibodies?
the patient’s plasma is screened for the presence of ______ that could cause transfusion reaction
what are the steps to adverse reactions?
start administration slowly (approximately 2-3 mL/min for the first 15 minutes)
stay with the patient for the first 15 minutes of transfusion
assess that patient at least every 30 minutes for adverse reactions
stop the blood transfusion if you suspect a reaction. quickly replace the blood tubing with a new administration set primed with normal saline for IV infusion
initiate an infusion of normal saline for IV at a keep open rate, usually 40 mL/hr. obtain vital signs. notify the healthcare team and the blood bank/transfusion service
what is anemia?
a condition where there is a deficiency of RBC or hemoglobin, leading to fatigue and weakness; also released in decreased oxygen delivery to tissue
symptoms: fatigue, weakness, pale skin, dizziness, shortness of breath, and cold hands/feet
causes: iron deficiency, vitamin B12 deficiency, chronic disease, blood loss, or genetic factors
treatment: iron supplements, vitamin B12 injections, medications for underlying causes, or blood transfusions
visual: diaphragm comparing normal red blood cells with those seen in anemia
what is sickle cell disease?
a genetic disorder where RBC become abnormally shaped (crescent or sickle-shaped), causing blockages in blood flow and pain
symptoms: pain episodes (crises), anemia fatigue, frequent infections, delayed growth in children
causes: inherited from both parents, leading to abnormal hemoglobin (HbS)
treatment: pain management, blood transfusions, hydroxyurea, and in some cases, stem cell transplant
visual: a comparison of normal red blood cells versus sickle-shaped cells
what is thalassemia?
a genetic blood disorder characterized by the reduced production of hemoglobin, leading to anemia
symptoms: fatigue, weakness, pale skin, slow growth in children, bone deformities, and enlarged spleen or liver
causes: mutations in the genes responsible for hemoglobin production
treatment: blood transfusion, iron chelation therapy, folic acid supplements, and stem cell transplant
visual: diaphragm of red blood cells showing abnormalities
what is polycythemia?
a condition where there is an overproduction of RBC, which can increase the risk of blood clots
symptoms: headache, dizziness, itching (especially after a hot shower), fatigue, and redness in the skin
causes: primary (polycythemia vera) or secondary due to chronic low oxygen levels, such as in lung disease
treatment: phlebotomy (removal of blood), medications to reduce blood thickness, and treatment of underlying conditions
visual: a blood smear showing increased RBC count
what is neutropenia?
a condition characterized by low levels of neutrophils, increasing the risk of infections
symptoms: increased susceptibility
causes: can result from chemotherapy, certain medications, bone marrow disorder, or autoimmune diseases
treatment: depends on the cause, including antibiotics, growth factors, and sometimes a bone marrow transplant
visual: a diaphragm of a blood cell with neutrophil levels compared to normal and low counts
what are non-hodgkin lymphomas (NHL)?
a group of cancers that originate in the lymphatic system, affecting WBC
symptoms: swollen lymph nodes, fever, weight loss, night sweats, fatigue
causes: genetics, infections (e.g., epstein-barr virus), or weakened immune systems
treatment: chemotherapy, radiation, immunotherapy, or stem cell transplant
visual: lymph node image highlights tumor development
what is leukemia?
cancers of the bone marrow and blood, leading to the overproduction of abnormal WBC
types: acute and chronic, including acute lymphoblastic leukemia (ALL) and chronic myelogenous leukemia (CML)
symptoms: fatigue, frequent infections, easy bruising, weight loss, and swollen lymph nodes
treatment: chemotherapy, radiation, bone marrow transplant, targeted therapies
visual: a blood smear showing leukemia cells
what is multiple myeloma?
a cancer of plasma cells in the bone marrow, which leads to the overproduction of abnormal blood cells
symptoms: bone pain, fatigue, kidney problems, frequent infections, and anemia
causes: unknown, but certain genetic factors, age, ad family history may play a role
treatment: chemotherapy, stem cell transplants, immunotherapy, and targeted therapies
visual: diaphragm of plasma cells in the bone marrow showing abnormal growth
what does a high GCS score mean?
13/15-15/15
indicates an awake, alert, oriented person
what does a moderate GCS score mean?
9/15-12/15
needs attention
what does a low GCS score mean?
<8/15
considered comatose
what is the glasglow coma scale used for?
Used as part of a neurological exam
where you might have a decrease in how conscious you are
includes injury-related conditions like concussions and traumatic brain injuries
also help with conditions that don’t involve injuries
hypoglycemia, poisoning, or after a seizure
what is contact precaution?
used to prevent diseases from spreading after touching a patient or objects in the patient’s room
wear gown and gloves
ex:
clostridium difficle (c. diff)
methicillin-resistant staphylococcus aureus (mrsa)
respiratory syncytial virus (rsv)
scabies
what is droplet precaution?
used to to help keep individuals safe from diseases that spread through particles that come out of the mouth during talking or coughing, or from drainage from the nose
wear a surgical mask and eye protection
ex:
influenza
mumps
pertussis (whooping cough)
rubella
what is airborne precaution?
used to keep individuals safe from diseases that spread through the air from person to person
wear a N95 respirator
ex:
tuberculosis (tb)
measles
varicella (chickenpox)
covid-19