AOS 3 - Biology - Immune System
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
What is an antigen?
The immune system uses antigens to recognise if a cell or molecule is self or non-self. If it is identified as non-self, an immune response is initiated.
So they are any molecule that may trigger an immune response.
They can be attached to a pathogen, cell or free-float
Can come in different types - proteins, sugars, DNA, RNA
What are self antigens?
Self-antigens, which are located on the surface of cells, mark the cells of an organism as ‘self’ so that the immune system doesn’t attack them. They can take the form of major histocompatibility complex (MHC) markers, which can be divided into two different classes.
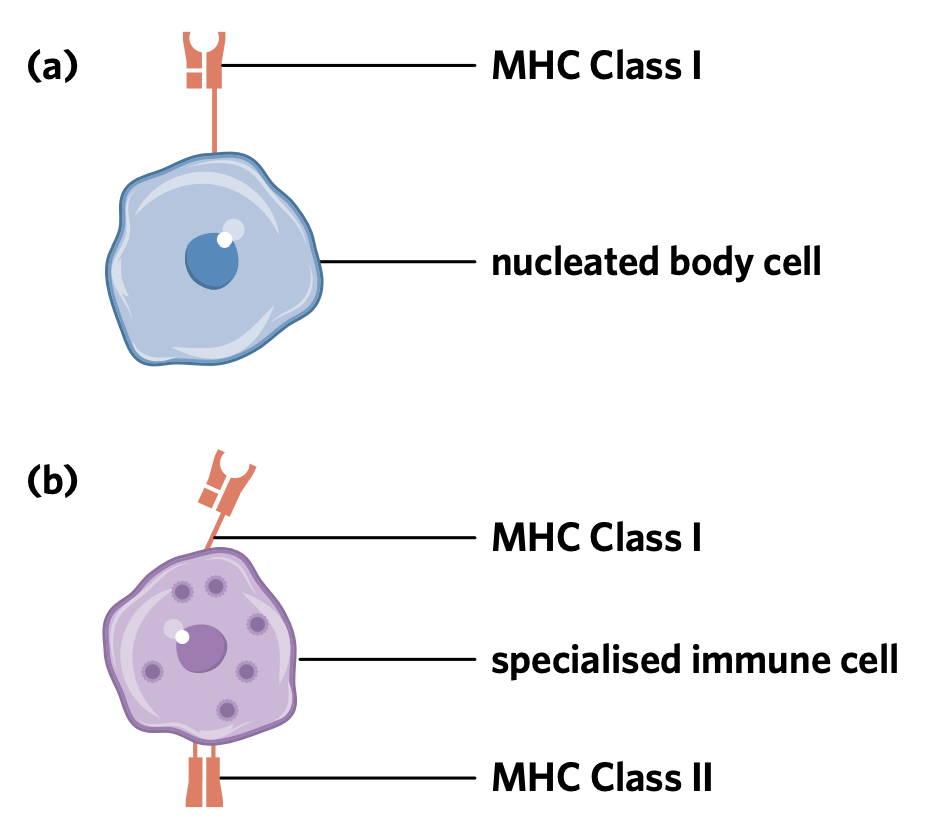
What are the MHC I and MHC II markers?
These markers are found on the surface of cells, that labels a cell as ‘self’
MHC Class I markers are expressed on all nucleated cells in the body. So, all cells in the human body except for those without a nucleus (e.g. red blood cells)
MHC Class II markers are found on specialised cells of the immune system.
What are non-self antigens?
Non-self antigens are antigens that the immune system reads as ‘foreign’ or not belonging to that individual - so when these a recognised the immune system is alerted to allow for this to be destroyed.
What is an example of a non-self antigen?
If a pathogen such as a bacterium enters the body, the immune system will recognise specific bacterial proteins present on its surface as foreign and launch an attack in response - in this case the bacterium is the antigen.
What is a pathogen?
An agent that causes disease
What are all the pathogen microbes?
Viruses
Bacteria
Worms
Prions
Protozoa
Fungi
Which pathogens are cellular pathogens?
Bacteria - Unicellular prokaryotes that can infect almost any part of the body. Bacteria can cause disease through toxin/enzyme production
Fungi - Eukaryotic organisms such as yeasts + moulds
Worms - Multicellular invertebrates parasites whose development will involve multiple stages
Protozoa - Single-celled eukaryotes that can be free-living or parasitic, with many different mechanisms of action.
Which pathogens are non-cellular pathogens?
Viruses - An infectious agent composed of genetic material inside a protein coat. Viruses don’t reproduce independently, they insert their genetic info into a host cell, and use it to replicate
Prions - Abnormally folded proteins that have the ability to induce normal proteins nearby to become misfolded.
What is the difference between an antigen and a pathogen?
Antigens are molecules (like proteins or polysaccharides) that trigger an immune response, while pathogens are disease-causing organisms or agents (like bacteria, viruses, or fungi) that contain these antigens.
What is an allergen?
An allergen is an environmental substance that triggers an immune response despite not being intrinsically harmful - so that are types of antigens that trigger an allergic immune response.
What is the innate immune system? What how does it involve the first line of defence?
The innate immune system is composed of two different defences known as the first and second lines of defences. Both of these mechanisms involve a non-specific and rapid response to foreign antigens, responding the same way regardless of the type of pathogen or antigen present.
What is the first line of defense?
A component of the innate immune system characterised by the presence of physical, chemical, and microbiological barriers to keep pathogens out of the host organism.
This defense reacts the same way to all infections
Has no ‘memory’ of prior infections
Has the same level of response for each infection of the same organism
What are some physical barriers in plants?
Physical - barriers that prevent or impede entry of pathogens
Thick bark
waxy cuticles of leaves
formation of galls to prevent the spread of infection
presence of thorns to deter insects
Closing of stomata
What are some chemical barriers in plants?
Chemical - barriers that inhibit the growth or development of pathogens/destroy them. These carriers can be harmful to pathogens or repel insects
Chitinases - enzymes that have antifungal properties
Phenols - secreted by wounded plants, repelling invading microorganisms
Denfis - peptides that are toxic to microbes
Saponins - disrupt membranes of gungi
Oxalic acid - toxic if ingested
What are some physical barriers in humans?
Physical - barriers that impede or prevent entry of pathogens
Intact skin
Mucous secretions or hairs in respiratory tract - trap organisms to be dispelled
What are some chemical barriers in humans?
Chemical - barriers that inhibit the growth or development of pathogens/destroy them. These carriers can be harmful to pathogens or repel insects
Presence of lysosomal enzymes in tears/saliva that destroy bacterial walls
acidic sweat destroys pathogens
stomach acid destroys pathogens
antibacterial compounds in earwax
low vaginal pH
antibacterial proteins in semen
What are some microbiological barriers in humans?
Microbiological - non-pathogenic bacteria that prevents growth of pathogenic microorganisms as they compete for space
Presence of bacteria on the skin, and in the lower gastrointestinal tract and the vagina.
What is the second line of defence?
Pathogens can breach the first line of defence so the second line of defence comes in which is also - non specific and immediate. This line of defense involves many cells that are leukocytes
What are leukocytes?
A group of blood cells responsible for protecting the body against pathogens and foreign material. Also known as white blood cells
What are phagocytes?
A group of leukocytes responsible for the endocytosis and destruction of pathogens, foreign material, and cell debris
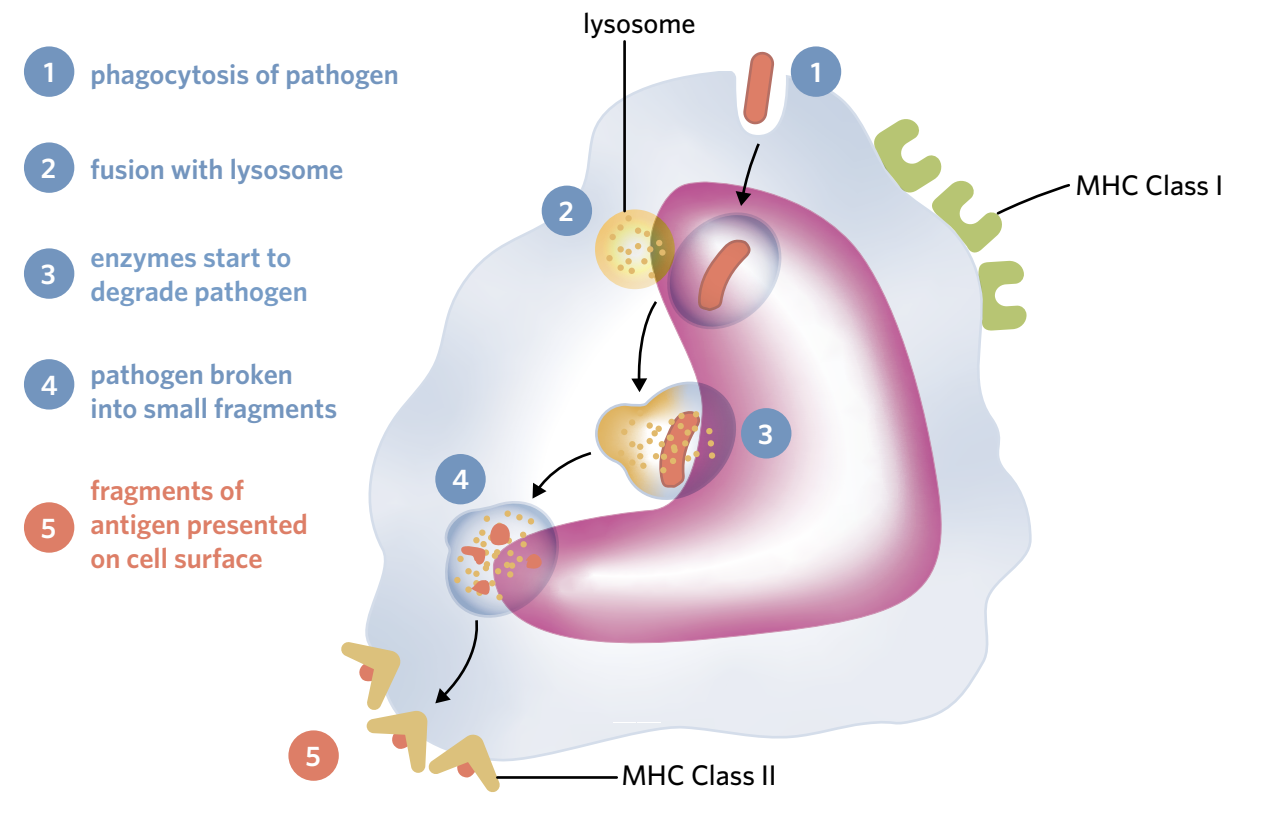
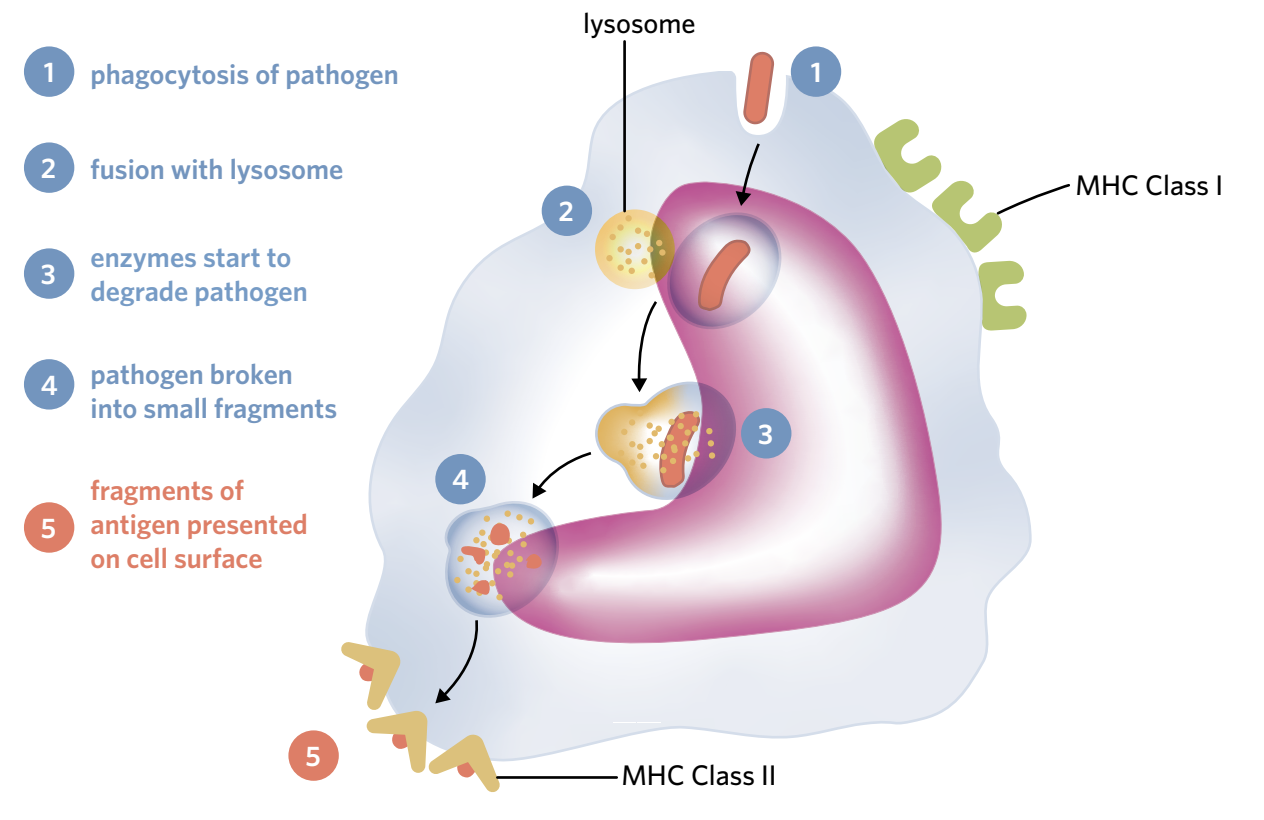
What is phagocytosis?
A process completed by phagocytes - where they consume and destroy foreign or dead material present in the body by engulfing it through the process of endocytosis. Once engulfed, lysosomes containing antimicrobial enzymes called lysozymes present in the cell destroy the foreign or dead material by fusing with the vesicles containing the engulfed material.
What phagocytes are involved the second line of defence?
Neutrophils
Macrophages
Dendritic cells.
What are antigen-presenting cells?
These cells not only consume and destroy foreign material, but they also present antigens from consumed material on their surface. As learnt, MHC Class II markers are only expressed on the body of specific immune cells, this is what APCs are, they use these markers to present their consumed antigens.
Macrophages and dendritic cells are APCs
What are cytokines?
To communicate within the immune system, phagocytes release a number of substances like cytokines that are important cell signalling molecules that help protect against pathogens - guiding immune cells to the site of infection or injury
List the three cells that are key components of the second line of defence
Natural killer cells
Mast cells
Eosinophils
What are natural killer cells?
Large, granulated cells which target abnormal and virally infected cells, with killer inhibitory and activation receptors
Inhibitory: examines surface of cell for MHC I markers
Activation: binds to infected cells/cells undergoing stress - initiating cell death/apoptosis in this cell
The presence of MHC Class I markers can be altered due to different disease processes, which can destroy or suppress the production of MHC Class I markers
What are mast cells?
Reside in connective tissues, when they detect injury or are stimulated by antigens or allergens, they become activated and degranulate - releasing histamine
Histamine plays a key role in the inflammatory response.
What are eosinophils?
Large, granulated cells that contain various toxic chemical mediators like DNases, RNases and proteases which help destroy invading pathogens. They target pathogens which are too large to be phagocytosed by degranulating on contact with them.
List the three cells key components of the second line of defence
Inferons
Complement proteins
Fever
What are interferons?
A type of cytokine that infected cells release - these interact with the receptors on neighbouring cells, causing them to undergo changes that make them less susceptible to viral infection
What are complement proteins?
These proteins interact with each other in different ways in the presence of pathogens, to create a series of reactions called complement cascade.
Opsonization: They stick on the surface of pathogens, making them easier to identify as foreign
Chemotaxis: They gather near a pathogen attracting phagocytes
Lysis: They join together on the surface of pathogens forming a Membrane Attack Complex (MAC) which creates pores in their membrane which release fluid into the pathogen causing it to burst.
What is a fever, and its effectiveness?
An innate response to potential infections
It increases the body’s temperature to a level that pathogens can’t function/survive in, but proteins that strengthen the defences are activated
A prolonged fever is bad due to it placing stress on cells that no longer function at their optimal temp.
What is the inflammatory response designed to do?
Eliminate the effects of an injury
Defend against potential pathogens
Clear out cells that may have been damaged or destroyed
Initiate repair
It is a complex, non-specific process that functions in the same way regardless of the pathogen or injury
What are the steps of the inflammatory response?
Initiation
Vasodilation
Migration
Explain the three steps of the inflammatory response
Initiation - Macrophages in the tissues are activated, releasing cytokines. Mast cells degranulate, releasing histamines
Vasodilation - The histamine travels to the blood vessels, causing vasodilation where blood vessels are dilated, increasing blood flow - causing swelling, redness and warmth
Migration - the vasodilation and increased permeability of blood vessels allows for more innate immune system components to leave the bloodstream and enter the injury site. Phagocytes (macrophages and neutrophils) are hided to the injury site by cytokines where they digest and phagocytose pathogens. And complement proteins arrive to attract phagocytes.
What is the third line of defense?
This line of defense is specific - in that it responds to each distinct pathogen in a unique/tailored way, and that it has immunological memory so it produces cells that allow the body to respond to future re-infections more quickly.
This defense is comprised of two pathways:
Humoral Immune response
Cell-mediated immune response
What are the differences between the humoral and cell-mediated responses?
Humoral
Responds to extracellular pathogens
Involves B cells and antibodies
Cell-mediated
Respond to intracellular pathogens
Involve cytotoxic T cells
Why is antigen presentation important in the third line of defence?
A key step in starting the adaptive immune response is the activation of T helper cells through antigen presentation. Antigen-presenting cells (APCs) engulf pathogens, break them down, and display their antigens on MHC Class II proteins. They then travel to lymph nodes and present these antigens to T helper cells. If a T helper cell has a matching receptor, it binds to the antigen, becomes activated, and helps trigger either the humoral or cell-mediated immune response.
Why are B lymphocytes important in the third line of defense, and initiation of it?
B lymphocytes (white blood cell), are the key mediators of humoral immunity. They’re covered in B cell receptors (antibodies). They travel around the body in the bloodstream, residing in high numbers within lymph nodes. The activation of these B lymphocytes occurs through their interaction with pathogenic antigens and T helper cells.
What are the steps of the humoral immunity pathway?
A pathogen with an antigen that has a complementary antigen-binding site to the receptor of a B cell interacts with the B cell, ‘selecting’ it.
A T helper cell selected through antigen presentation, which also has a complementary receptor to the antigen, will recognise the selected B cell, secreting a number of different cytokines. These cytokines cause the B cell to undergo clonal expansion, through which many copies of the selected B cell are produced.
T helper cells also stimulate the selected B cell, via cytokines, to undergo the process of differentiation, in which the clones of the selected B cell are driven to differentiate into two different types of B cells – B memory cells and effector cells which in this instance are called plasma cells.
Plasma cells are differentiated clones of the selected B cell. After differentiating, they secrete antibodies into the blood in order to defend against the selected pathogen
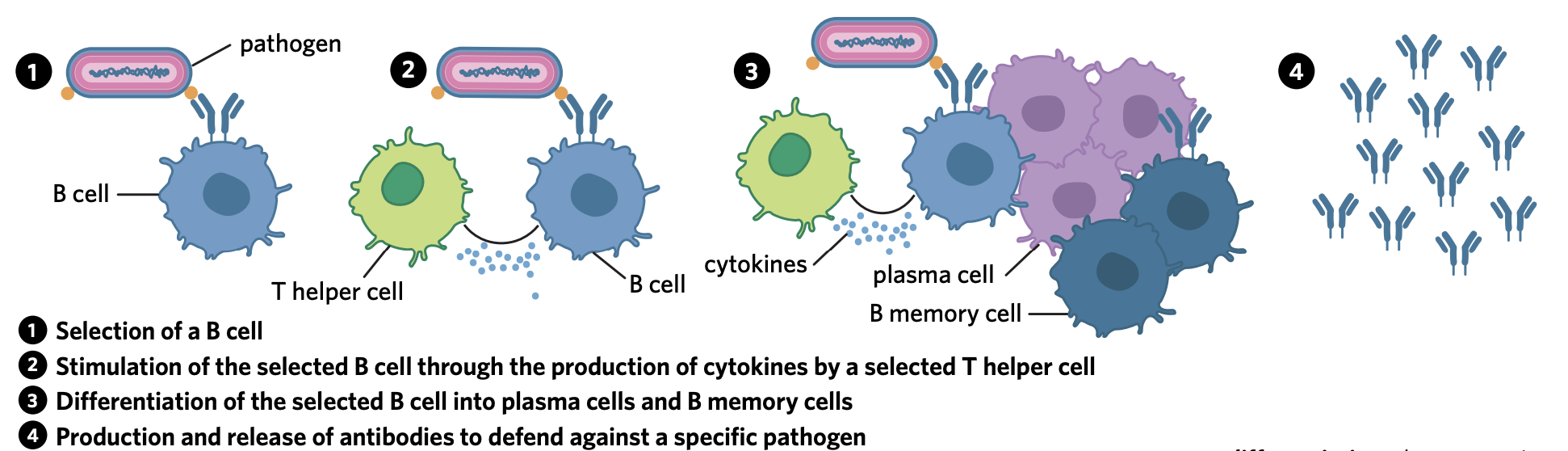
What are the B memory cells then used for?
Additionally, the other product of B cell differentiation – B memory cells – are clones of the selected B cell that reside in the body for a prolonged period of time and are responsible for immunological memory
What are antibodies?
Antibodies released by plasma cells are proteins with a quaternary structure. They are composed of four polypeptide chains, including two heavy chains and two light chains. They have binding sites for the same specific complementary antigen. This allows antibodies to bind with antigens on the surface of pathogens. As there are two antigen binding sites present, an antibody can bind with two pathogens at once
What are the different functions of an antibody?
Neutralisation - They block the sites of pathogens that are used to attack host cells
Agglutination - Antibodies bind with antigens on two seperate pathogens forming large antigen-antibody complexes - making it easier for phagocytes to recognise them
Immobilisation - Restrict movement of pathogens through forming large antigen complexes
Opsonization - Bind to the surface of a pathogen to make it easier to phagocytose
Activation of complement proteins - Attach to the pathogen surfaces to facilitate ‘membrane attack complexes’
What role do cytotoxic T cells play in cell-mediated immunity
They are a type of T lymphocyte, and are key players in that they primarily carry out their role of assessing the MHC Class I marker of infected cells (self-recognition role).
What are the steps of cell-mediated immuinity?
Antigen-presenting cells present digested foreign antigens on their surface MHC II - these then travel to the lymph nodes
These cells may also come upon naive T cells with a T cell receptor that matches the antigens being presented - selecting and activating them - allowing cytokines ot be secreted, and the selected T helper cells to undergo clonal selection and differentiation.
The clones are driven to differentiate into cytotoxic T cells and T memory cells. The memory cells remain in the body for immunological memory, the cytotoxic leave the lymph nodes to reach the site of infection.
Due to the process of clonal selection, the cytotoxic T cells that arrive at the site of infection all have T cell receptors that are specific to the foreign antigen selected for. Once the cytotoxic T cell has found an abnormal cell that is presenting complementary foreign antigens on its MHC Class I complex, it binds to it via interactions between its T cell receptor and the antigen-MHC Class I complex (Figure 12a). Chemicals, such as perforin, are then secreted by the cytotoxic T cell to induce apoptosis in the cell
How do B memory cells and T memory cells contribute to the immunological memory
B memory cells - they rapidly divide to form new antibody producing plasma cells
T memory cells - divide into T helper cells and cytotoxic T cells.
Why is immunological memory important?
This memory creates a more rapid and effective immune response upon re-infection. As antibodies and cytotoxic T cells are produced at a more rapid rate to kill infected cells.
What are the main functions of the Lymphatic System?
Transportation of antigen-presenting cells to secondary lymphoid tissues for antigen recognition and initiation of the adaptive immune response
Production of leukocytes (primary lymphoid tissues - bone marrow)
Removal of fluid from tissues around the body
Absorption of fatty acids from the digestive system
What are the main components of the Lymphatic system?
Primary and Secondary lymphoid tissues
What do the Primary lymphoid tissues do?
They create and complete the maturation of lymphocytes, these include bone marrow and thymus
What do the Secondary lymphoid tissues do?
Maintain mature lymphocytes and initiate the adaptive immune response, these include the lymph nodes, tonsils and spleen
What are the key steps of the Lymphatic system?
Lymphatic drainage
Lymphatic flow
Lymphatic surveillance
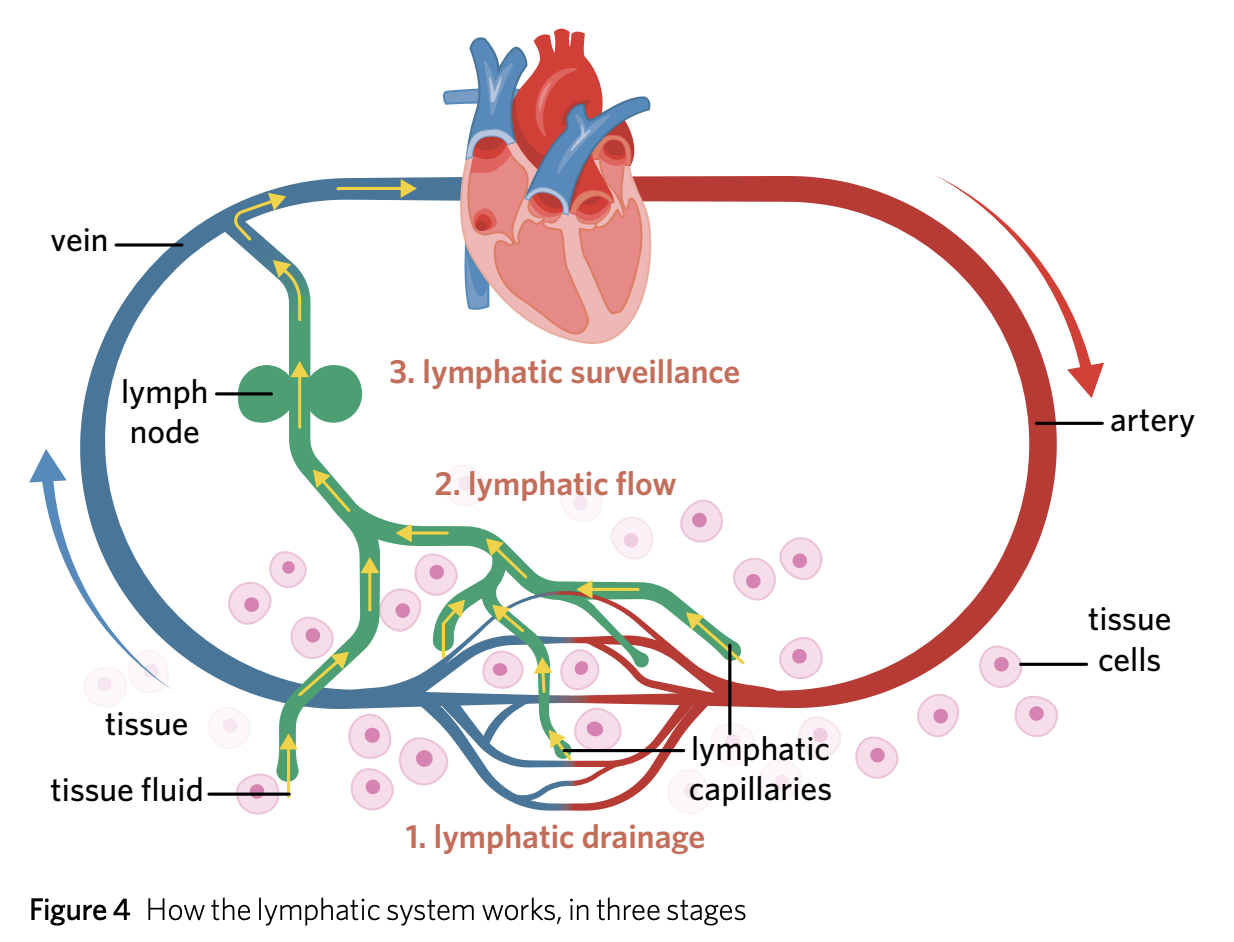
Outline what occurs in the three steps of the lymphatic system
Fluid from blood vessels constantly leak into tissues (more so during inflammation) and lymphatic capillaries collect fluid (lymph) and carry it away through the system
The small capillaries gradually join together to form larger vessels, that rely on surrounding muscle movements to squeeze lymph fluid through the system.
The fluid arrives at the lymph nodes through the afferent lymphatic vessels, and travels through clusters of B and T cells - allowing the APCs/pathogens to meet with a lymphocyte with a matching antigen binding site.
After the adaptive immune system is triggered, antibodies and activated cytotoxic T cells leave the lymph nodes via the efferent lymphatic vessels.
What is Natural Immunity?
Immunity developed without any medical intervention
What is Natural active immuinity?
When a person is infected with a pathogen and their adaptive immune system (3rd line) develops long-lasting immunity (immunological immunity) to the disease. It is ‘active’ due to the body producing antibodies against the pathogen.
What is Natural passive immunity?
When a person becomes immune by obtaining antibodies from another (eg: breastfeeding or through the placenta - the mother’s antibodies are protecting their babies weak adaptive immune system)
What is Artificial Immuinity?
Immunity developed due to medical intervention
What is artificial passive immunity?
A key example is vaccines - this immunity is developed through producing antibodies and memory cells against a pathogen that has been artificially introduced
Explain the importance of vaccines
Vaccines aim to introduce a pathogen to allow you to generate immunity towards the pathogen without getting sick. Normally active immunity is long-lasting as a result of you getting sick first and being exposed to it. Vaccines mimic this but containing a weakened or deactivated (so that it can’t replicate) form of the pathogen. Active immunity is triggered due to the body recognising it as foreign, triggering antibodies and memory cells to be made.
List some types of vaccines
Attenuated
Toxoid
Inactivated
Virus like particles
What is the booster vaccine?
This is given after the first vaccination, where the body first created an immunity to the given pathogen, so the memory cells will recognise the antigen creating a rapid, large immune response. Boosters are needed as memory cells die over time, as this occurs a person’s immunity decreases as well, so they are needed to increase a person’s B and T cells to an adequate level.
What is Artificial passive immuinity?
Immunity developed when antibodies are gained via human intervention - antibodies given this way degrade and eventually none are left , so no memory cells are needed providing short-term immunity.
What is Herd Immuinity?
When enough of a population (95%) is vaccinated against a disease, preventing it from spreading to those who aren’t vaccinated. This is important as some people can’t receive vaccines due to being too young, or having a weakened immune system. So it there aren’t enough people to spread the pathogen, we can eliminate it.
What are non-infectious diseases compared to infectious?
Not all diseases are caused by pathogens, making them non-infectious. Examples include abnormal genes and lifestyle factors. So infectious diseases are those caused by a pathogen, a subset of these can be ‘contagious’ with these being measured in how ‘virulent’ they are (how severe the disease they cause is)
What are emerging diseases?
Diseases that have occured in the past, only affecting particular populations
What are re-emerging diseases?
Diseases that have caused major public concern but then declined, and are currently returning.
What factors cause diseases to emerge or re-emerge?
Increasing populations
Insufficient vaccination of population
Evolution of causative organisms
Globalisation and travel
Increased exposure of humans to animals
What is a disease outbreak?
An outbreak is a sudden/unexpected increase in disease occurence
Define an endemic and pandemic
Endemic - sudden, widespread increase in occurrence in a specific population, location and time
Pandemic - spread to different countries and/or continents
What factors resulted in Indigenous Communities being susceptible to diseases during colonization
Lack of immunity in the Indigenous community (limited exposure)
A lack of knowledge and experience with European disease
The disruption caused by colonisation - food + water access and change
Over 60% of the Indigenous population succumbed to a series of epidemics
Define contagious
A property of a pathogen that means it can be transmitted between organisms
Define virulent/virulence
The potential of a pathogen/disease to cause serious illness or harm
What are the main methods of identifying pathogens?
Physical (visualising a pathogen under microscope to see its structure)
Phenotypic (placing pathogens throgh tests that highlight their type)
Immunological (involves the diagnosis of diseases based on the presence of antibodies/antigens)
Molecule (testing for genetic materials be searching for a signal which highlights that a pathogen is present)
What are the main methods of disease transmission?
Airborne transmission
Droplet transmission
Direct and Indirect physical transmission
Faecal-oral transmission
List 2-3 methods of controlling disease transmission
Prevention (improved hygiene, sterilising surfaces, access to clean water and food, vaccinations)
Screening (routine testing, observation of medication sales)
Quarantine and isolation