Phys Ch. 6 - Contraction of Skeletal Muscle
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
59 Terms
Organization of skeletal muscle:
each muscle fiber = a muscle cell

fiber length and innervation of skeletal muscles:
in most skeletal muscles, each fiber extends the entire length of the muscle
each fiber is usually innervated by only one nerve ending, located near the middle of the fiber
Sarcolemma:
assoc w/ tendons:
thin membrane enclosing skeletal muscle fiber
consists of true cell membrane (plasma membrane) and an outer coat made up of a thin layer of polysaccharide material containing numerous thin collagen fibrils
at each end of the muscle fiber, this surface layer of the sarcolemma fuses with the tendon fiber
the tendon fibers, in turn, collect into bundles to form the muscle tendons that then connect the muscles to the bones
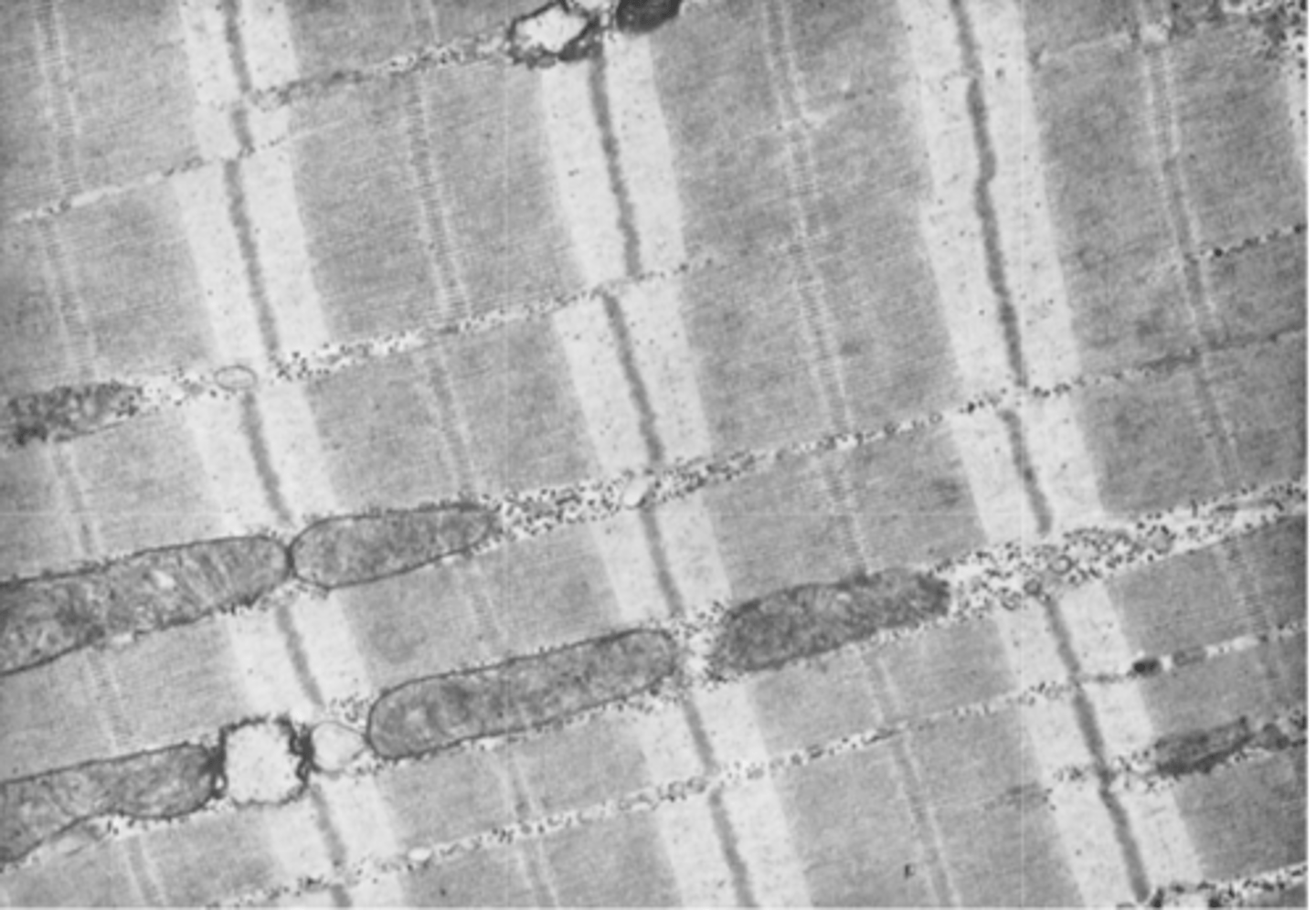
What does a myofibril consist of?
each muscle fiber contains hundreds of myofibrils
Note the mitochondria lying between the myofibrils.
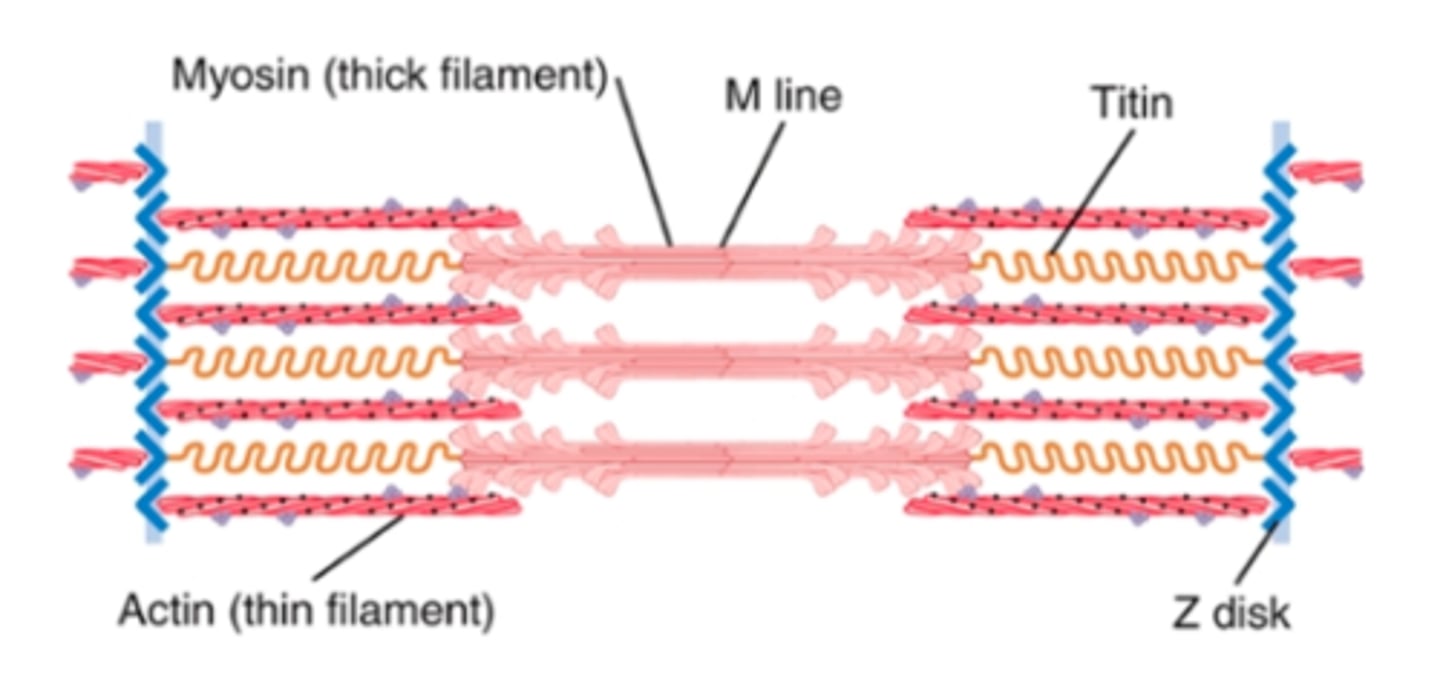
each myofibril contains 1500 adjacent thick myosin filaments and 3000 thin actin filaments
the myosin and actin filaments partially interdigitate and thus cause alternate light and dark bands
Myosin projections = cross-bridges that interact w/ the actin filaments and cause contraction
the entire muscle fiber has light and dark bands, as do the individual myofibrils. These bands give skeletal and cardiac muscle their striated appearance.
I bands:
light bands
contain only actin
(Isotropic to polarized light)

A bands:
dark bands
contain myosin filaments as well as the ends of the actin filaments where they overlap
anisotropic to polarized light

Z disc:
disk where the ends of actin filaments attach
from this disk, these filaments extend in both directions to interdigitate w/ the myosin filaments
composed of filamentous proteins different from actin and myosin
passes crosswise across myofibril and crosswise from myofibril to myofibril, attaching them to one another all the way across the muscle fiber

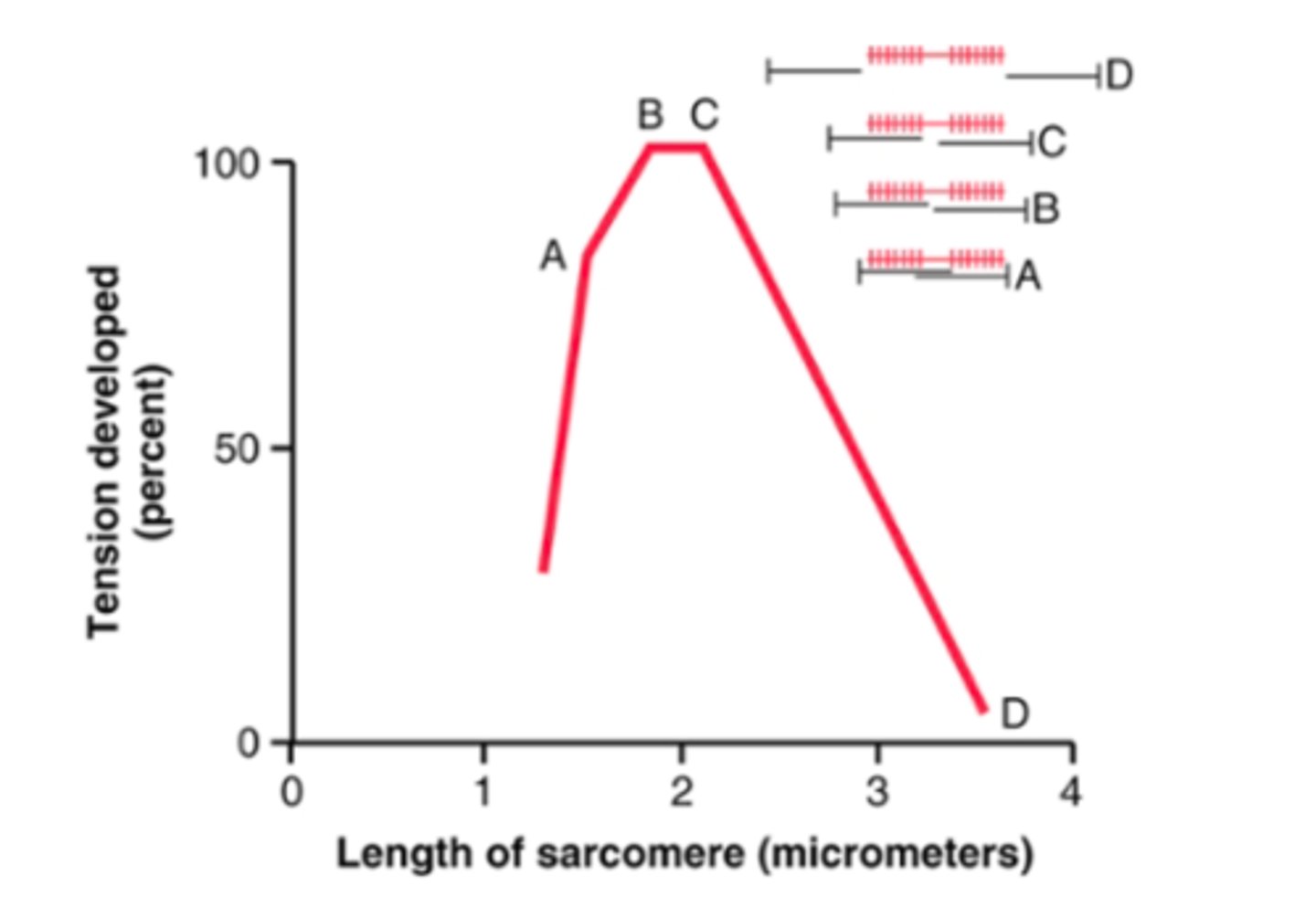
Sarcomere:
portion of myofibril (or of whole muscle fiber) that lies between 2 successive Z disks
when the muscle fiber is contracted, the length of the sarcomere is about 2 micrometers
at this length, the actin filaments completely overlap the myosin filaments, and the tips of the actin filaments are just beginning to overlap one another
at this length, the muscle is capable of generating its greatest force of contraction

Titin filaments:
What is its function?
What makes it unique?
What does it attach to?
filamentous molecules of protein that maintain side-by-side relationship between myosin and actin
one of the largest molecules in the body (MW = 3 mil)
because it is filamentous, it is very springy
acts as freamework that holds the myosin and actin in place so that the contractile machinery of the sarcomere will work
one end = elastic, attached to Z disk- acts as spring and changes length as sarcomere contracts + relaxes
other end = tethers it to myosin thick filament
may also act as a template for initial formation of contractile filaments of the sarcomere (esp myosin filaments)
Sarcoplasm:
intracellular fluid between myofibrils
contains large amounts of K, Mg, phosphate, plus multiple protein enzymes
also present are tremendous # of mitochondria that lie parallel to the myofibrils - supply the contracting myofibrils w/ large amounts of ATP
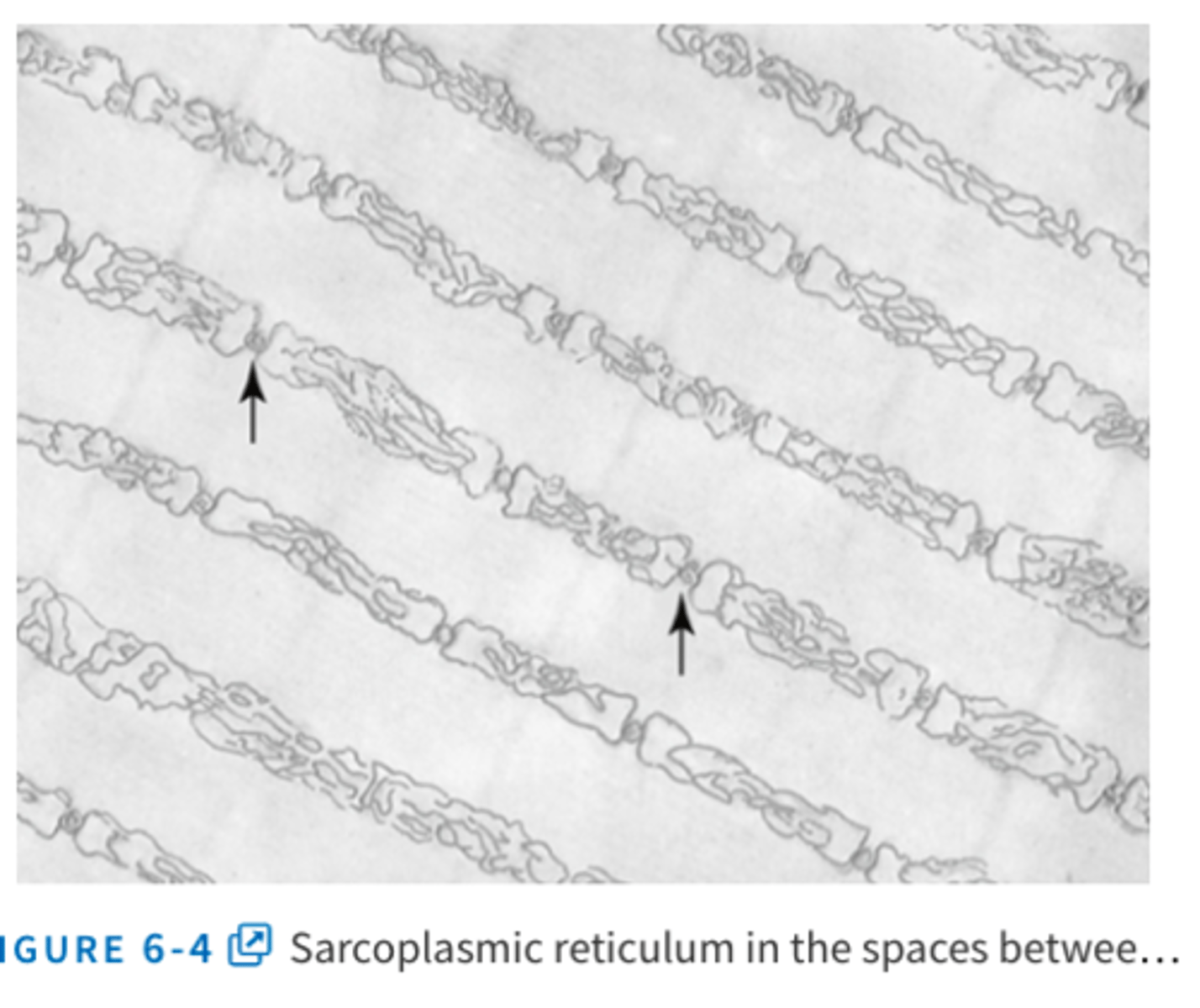
Sarcoplasmic reticulum:
specialized endoplasmic reticulum of skeletal muscle
in the sarcoplasm surrounding the myofibrils of each muscle fiber
special organization important in regulating calcium storage, release, reuptake, and therefore muscle contraction
The rapidly contracting types of muscle fibers have especially extensive sarcoplasmic reticula.
General mechanism of muscle contraction via acetylcholine:
1. An action potential travels along motor nerve to its ending on muscle fiber
2. nerve secretes acetylcholine
3. Acetylcholine acts on local area of muscle fiber membrane to open acetylcholine-gated cation channels through protein molecules in the membrane
4. opening allows large quantities of Na ions to diffuse to interior of muscle fiber membrane; causes local depolarization that in turn leads to opening of voltage-gated sodium channels, which initiates AP at the membrane
5. Action potential travels along muscle fiber membrane in same way AP travels along nerve fiber membranes
6. AP depolarizes the muscle membrane, and much of AP electricity flows through center of muscle fiber. Causes sarcoplasmic reticulum to release Ca ions stored in reticulum
7. Ca ions initiate attractive forces between actin and myosin filaments, causing them to slide alongside each other = contractile process
8. After a fraction of a second, Ca ions are pumped back into SR by Ca membrane pump to remain stored in reticulum until new muscle AP comes along; removal of Ca ions from myofibrils causes muscle contraction to cease
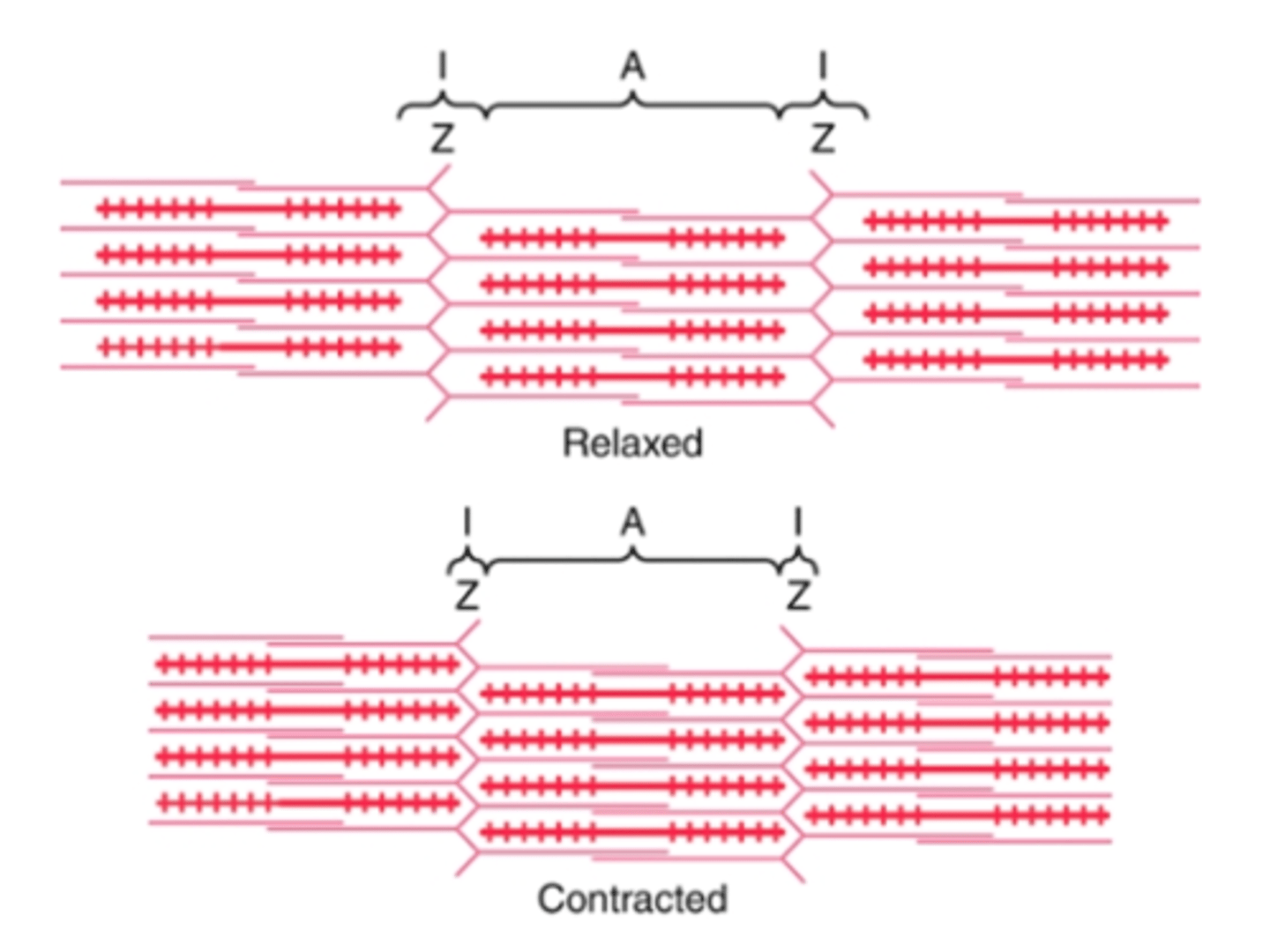
Sliding filament mechanism:
in the relaxed state, the ends of the actin filaments extending from two successive Z disks barely overlap one another
in the contracted state, these actin filaments have been pulled inward among the myosin filaments, so their ends overlap one another to their maximal extent
the Z disks have been pulled by the actin filaments up to to the ends of the myosin filaments
caused by forces generated by interaction of cross-bridges from the myosin filaments with the actin filaments
Characteristics of myosin filaments:
components
structure
twisting arrangement
myosin molecule =
composed of 6 polypeptide chains - 2 heavy chains and 4 light chains
2 heavy chains wrap spirally around each other to form double helix = tail
one end of each these chains is folded bilaterally into a globular polypeptide structure = myosin head
the 4 light chains are part of the myosin head- 2 at each head - help control the function of the head during muscle contraction
the myosin filament is made up of >200 individual myosin molecules
central portion of filament = tails of the myosin molecules bundled together to form body, while many heads of the molecules hang outward to the sides of the body
part of the body of each myosin molecule hangs to the side along with the head, providing an arm that extends the head outward from the body
arm + head = cross-bridge
total length = uniform = 1.6 micrometers
myosin filament twisted so that each successive pair of cross-bridges is axially displaced from previous pair by 120 degrees - twisting ensures cross-bridges extend in all directions around the filament
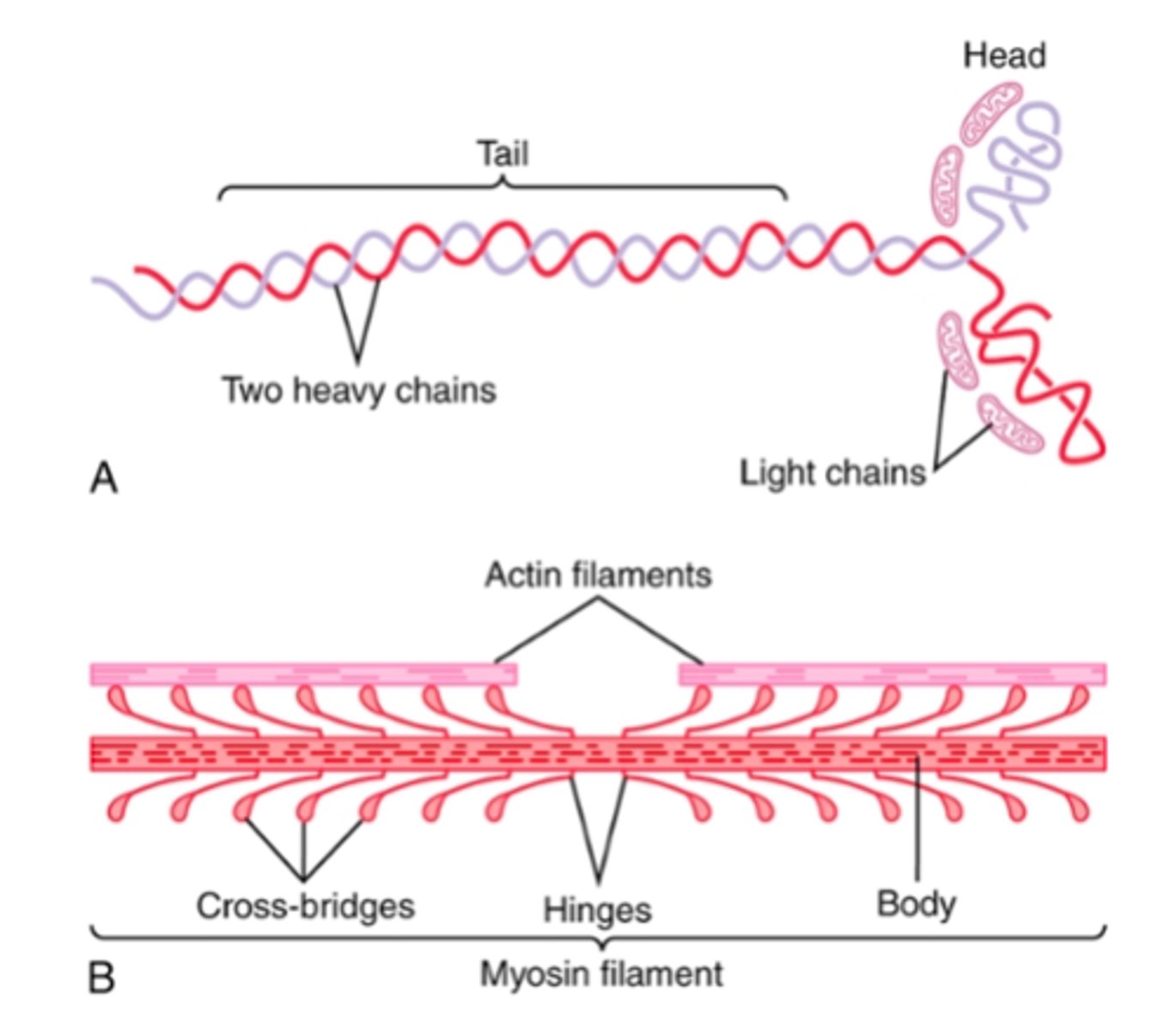
Cross-bridges:
what are they? where are they flexible?
protruding myosin head and arm together
flexible at 2 points (hinges) - one where the arm leaves the body of the myosin filament and the other where the head attaches to the arm
hinged arms allow heads either to be extended far outward from body or brought close to the body; the hinged heads participate in the contraction process
Special function of the myosin head:
acts as ATPase enzyme
allows head to cleave ATP and use the energy derived to energize contraction process
characteristics of actin filaments:
backbone/composition
backbone = double-standed F-actin molecule wound in a helix
each strand of the double F-actin helix is composed of polymerized G-actin molecules
Attached to each one of the G-actin molecules is one molecule of ADP
These ADP molecules are the staggered active sites on the actin filaments with which the cross-bridges of the myosin filaments interact
length = ~1 micrometer
the bases of the actin filaments are inserted strongly into the Z disks; the ends of the filaments protrude in both directions to lie in the spaces between the myosin molecules
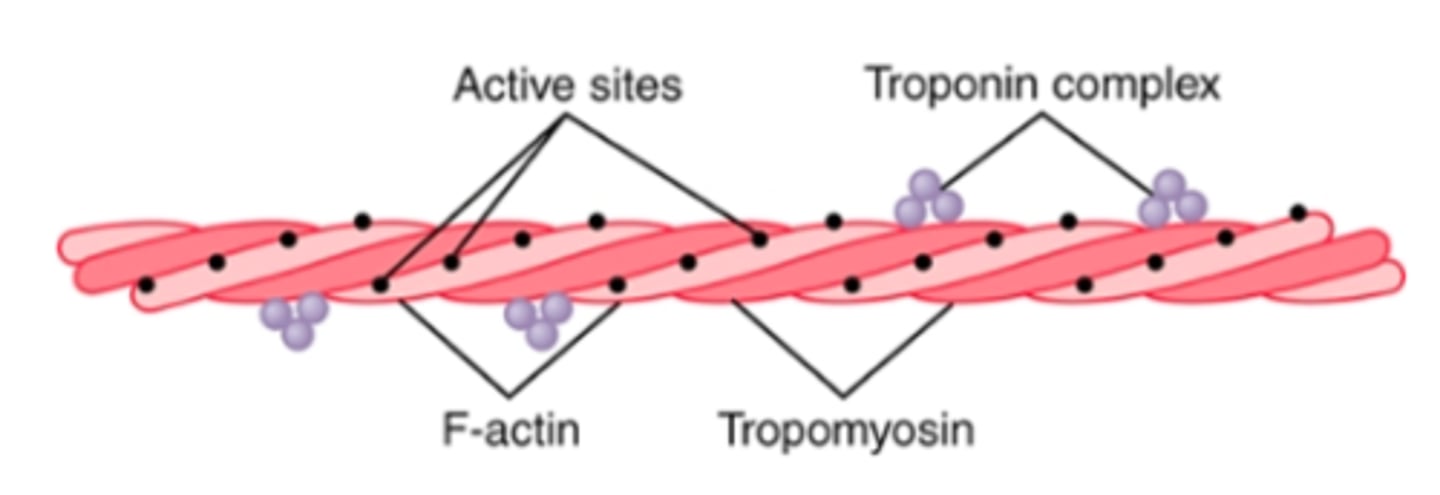
Tropomyosin molecules:
attached to actin filaments
wrapped spirally around sides of F-actin helix
In the resting state, the tropomyosin molecules lie on top of the active sites of the actin strands so that attraction cannot occur between the actin and myosin filaments to cause contraction.
(A pure actin filament without the presence of the troponin-tropomyosin complex (but in the presence of magnesium ions and ATP) binds instantly and strongly with the heads of the myosin molecules.)
Contraction occurs only when an appropriate signal causes a conformation change in tropomyosin that “uncovers” active sites on the actin molecule and initiates contraction
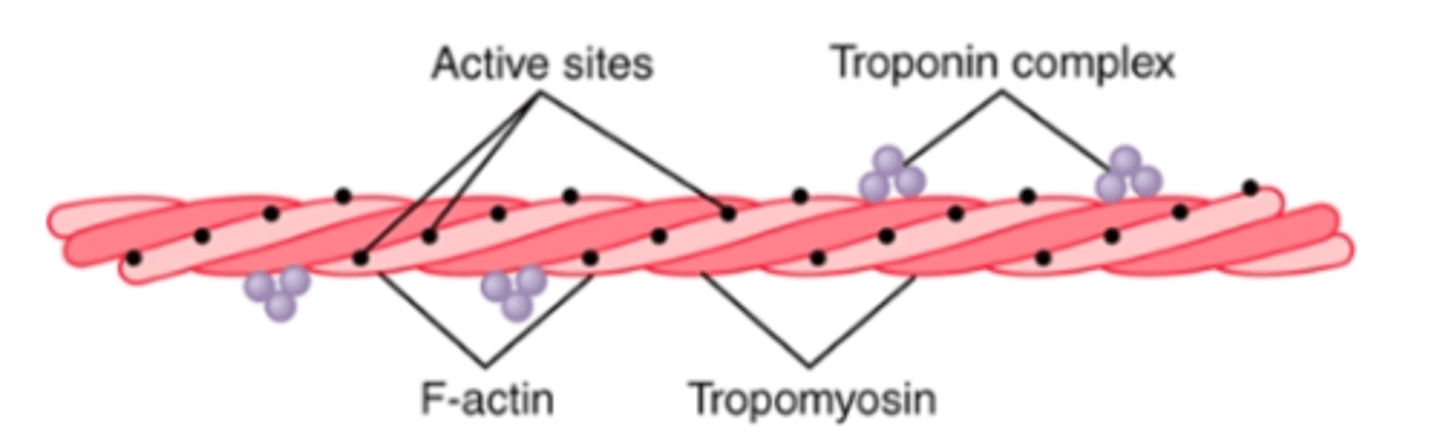
Troponin molecules:
3 subunits
attached intermittently along the sides of tropomyosin - attaches tropomyosin to actin
complexes of 3 loosely bound protein subunits, each of which plays a specific role in controlling muscle contraction
troponin I = strong affinity for actin
troponin T = strong affinity for tropomyosin
troponin C = strong affinity for calcium ions
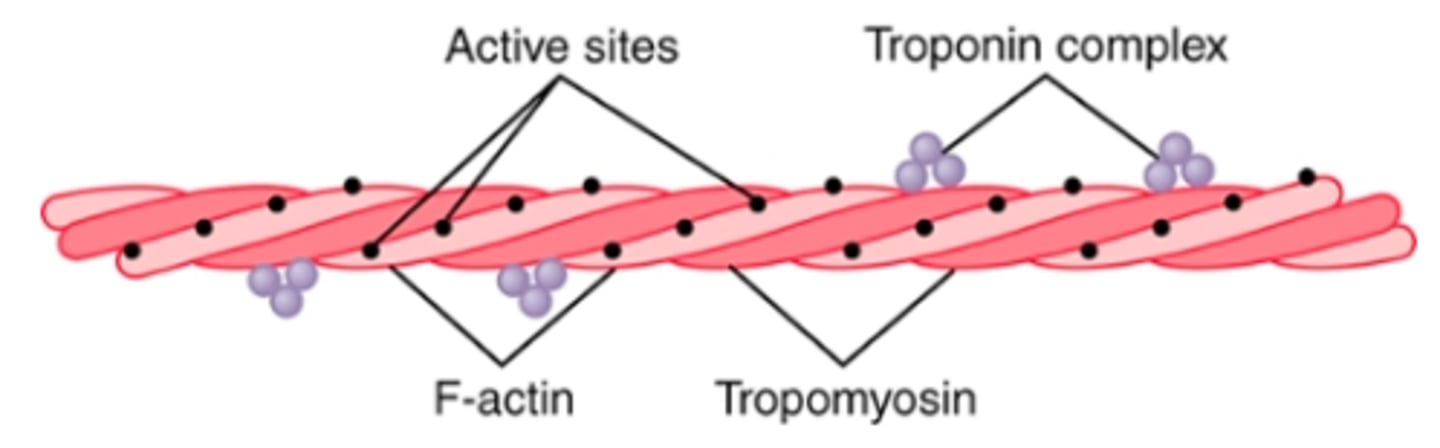
On a molecular level, what initiates the contraction process?
in the presence of large amounts of calcium ions, the inhibitory effect of troponin-tropomyosin on actin filaments is inhibited - when troponin C binds calcium (up to 4 Ca ions), the troponin complex undergoes a conformational change that tugs on tropomyosin molecule and moves it deeper into groove between 2 actin strands, uncovering actin's active sites
the heads of the myosin filaments become attracted to the active sites of the actin filament and initiate contraction
Walk-along (ratchet) theory of contraction:
When a myosin head attaches to an active site, this simultaneously causes profound changes in the intramolecular forces between head and arm of its cross-bridge
the new alignment of forces causes the head to tilt toward the arm and to drag the actin filament along with it
tilt of head = power stroke
immediately after tilting, the head automatically breaks away from the active site and returns to its extended position
It combines with a new active site farther down along the actin filament; the head then tilts again to cause a new power stroke and the actin filaments move another step
thus, the heads of the cross-bridges bend back and forth and step by step, walk along the actin filament, pulling the ends of 2 successive actin filaments toward the center of the myosin filament

What determines force of contraction?
each of the cross-bridges is believed to operate independently of all the others, with each attaching and pulling in a continuous repeated cycle - therefore, the greater the # of cross-bridges in contact with the actin filament at any given time, the greater the force of contraction
amount of actin and myosin overlap determines tension developed by contracting muscle
Fenn effect:
The greater the amount of work performed by the muscle, the greater the amount of ATP that is cleaved.
How does ATP get used up in the muscle contraction process?
1. before contraction begins, heads of cross-bridges bind ATP. ATPase activity of myosin head immediately cleaves ATP but leads ADP+P bound to head
-> in this state, the conformation of the head is such that it extends perpendicularly toward the actin filament but is not yet attached to the actin.
2. When troponin-tropomyosin complex binds w/ calcium ions, active sites on the actin filament are uncovered and myosin heads then bind w/ these sites
3. The energy that activates the power stroke is the energy already stored, like a cocked spring, by the conformational change that occurred in the head when the ATP molecule was cleaved
4. Once the head of the cross-bridge tilts, release of the ADP and phosphate ion that were previously attached to the head is allowed. At the site of release of the ADP, a new molecule of ATP binds. This binding of new ATP causes detachment of the head from the actin.
5. After the head has detached from the actin, the new molecule of ATP is cleaved to begin the next cycle, leading to a new power stroke.
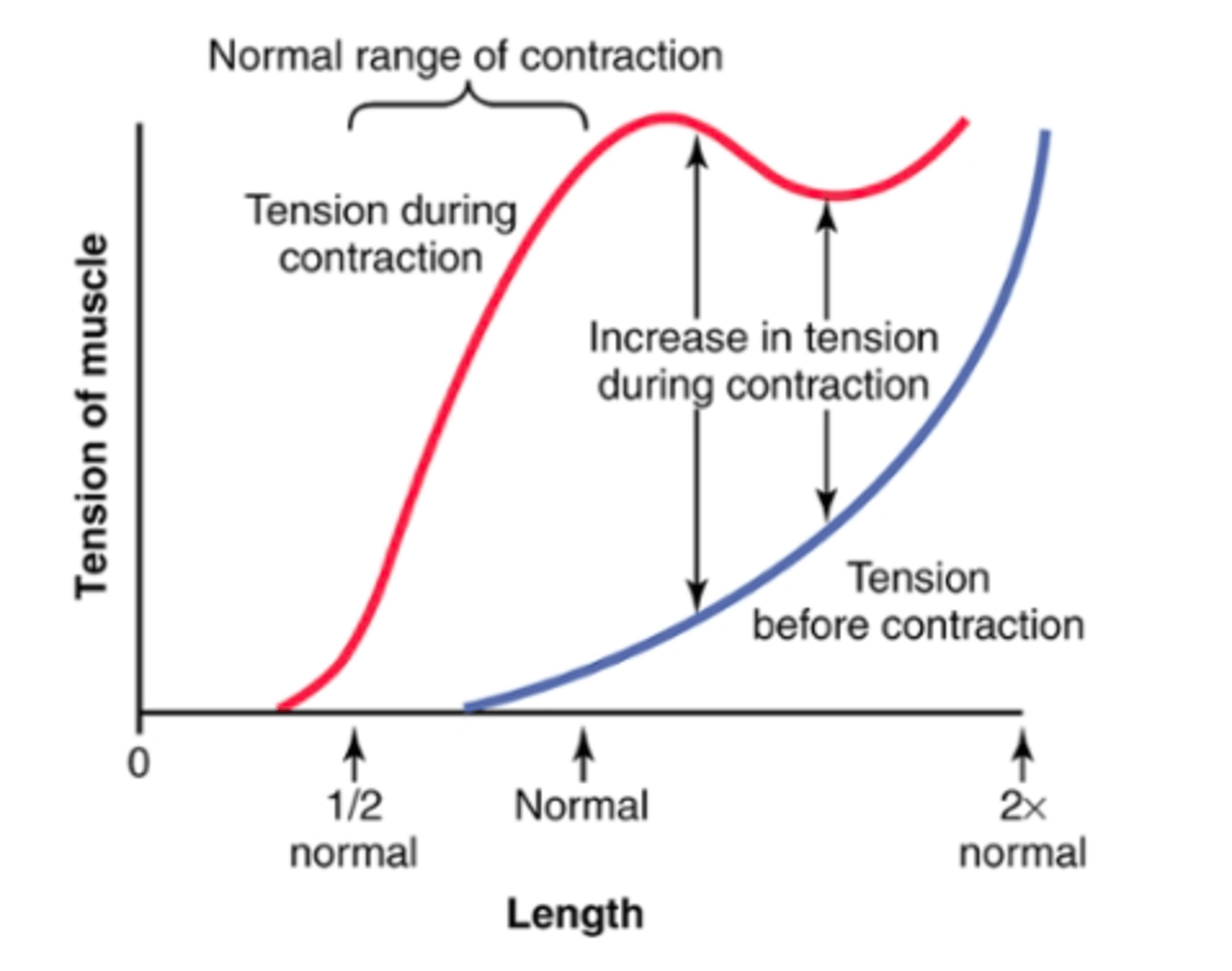
What is the effect of muscle length on force of contraction in the whole intact muscle?
the whole muscle has large amount of CT in it; the sarcomeres in different parts of the muscle do not always contract the same amount - same general form as individual muscle fibers, but different dimensions
when the muscle is at its normal resting length, it contracts on activation w/ the approximate maximum force of contraction
the increase in tension that occurs during contraction (active tension) decreases as the muscle is stretched beyond its normal length
An elongated muscle contracts w/ more force than does a shortened muscle
The graph shows max strength of contraction at full functional muscle length and almost no strength of contraction at half normal length
What is the relationship between velocity of contraction to load?
A skeletal muscle contracts rapidly when it contracts against no load to a state of full contraction (0.1 s)
When loads are applied, the velocity of contraction decreases progressively as the load increases
When the load has been increased to equal the max force the muscle can exert, the velocity of contraction becomes zero, and no contraction results, despite activation of muscle fiber
A load on a contracting muscle is a reverse force that opposes the contractile force caused by muscle contraction (therefore, the net force available to cause velocity of shortening is correspondingly reduced)

Work output during muscle contraction:
When a muscle contracts against a load, it performs work
to perform work means energy is transferred from muscle to external load to lift an object to greater height or overcome resistance to movement
W = L x D
L = load
D = distance of movement against load
What is energy needed for during muscle contraction?
Most of the energy required for muscle contraction is used to trigger the walk-along mechanism whereby the cross-bridges pull the actin filaments, but small amounts are required for the following: (1) pumping calcium ions from the sarcoplasm into the sarcoplasmic reticulum after the contraction is over; and (2) pumping sodium and potassium ions through the muscle fiber membrane to maintain an appropriate ionic environment for the propagation of muscle fiber action potentials.
3 sources of energy for ADP rephosphorylation during muscle contraction
1. phosphocreatine - carries high-energy phosphate bond similar to bonds of ATP
-> slightly higher amount of free energy than that of each ATP bond
-> total amount of phosphocreatine in the muscle fiber is small
2. Glycolysis - Rapid enzymatic breakdown of the glycogen to pyruvic acid and lactic acid liberates energy that is used to convert ADP to ATP
-> can occur in the absence of oxygen, so muscle contraction can be sustained even when O2 delivery from blood is unavailable
-> rate of ATP formation by glycolysis is 2.5x as rapid as ATP formation in response to cellular foodstuffs reacting w/ oxygen; so many end products of glycolysis accumulate in the muscle cells that glycolysis also loses its capability to sustain maximum muscle contraction after about 1 minute.
3. Oxidative metabolism - combining oxygen w/ end products of glycolysis and w/ various other foodstuffs to liberate ATP
-> More than 95% of all energy used by the muscles for sustained long-term contraction is derived from oxidative metabolism
-> carbohydrates, fats, proteins
-> For extremely long-term maximal muscle activity—over a period of many hours—the greatest proportion of energy comes from fats but, for periods of 2 to 4 hours, as much as one half of the energy can come from stored carbohydrates.
Efficiency of muscle contraction:
efficiency = % of energy input that is converted into work instead of heat
low efficiency of muscle - less than 25%
-> about 1/2 of energy in foodstuffs is lost during the formation of ATP and only some of the energy in ATP itself can later be converted into work
How can muscle achieve maximum efficiency?
only when the muscle contracts at a moderate velocity (~30% of max velocity)
if the muscle contracts slowly or w/o any movement, small amounts of maintenance heat are released during contraction, even though little or no work is performed, thereby decreasing the conversion efficiency to as little as zero
If contraction is too rapid, much of the energy is used to overcome viscous friction w/i the muscle itself, and this too reduces the efficiency of contraction
Eliciting single muscle twitches:
demonstrates features of muscle contraction
done by electrical excitation of the nerve to a muscle or by passing a short electrical stimulus through the muscle itself, giving rise to a single sudden contraction lasting a fraction of a second
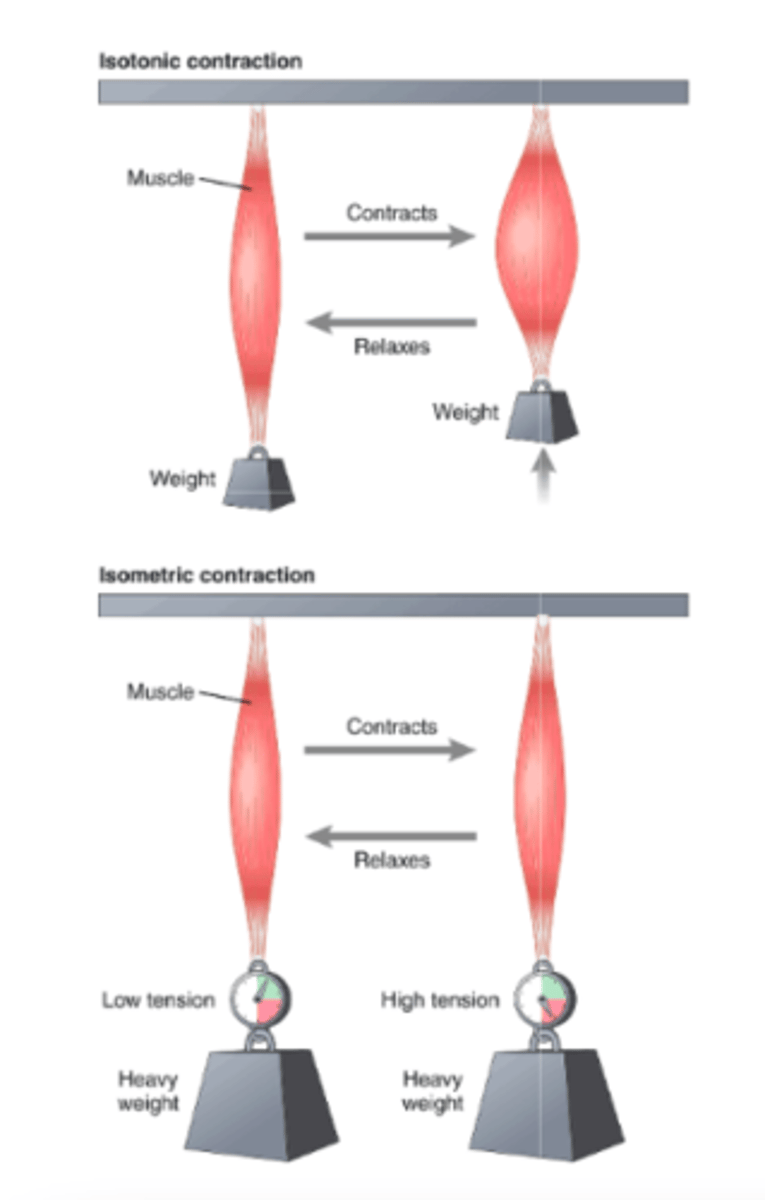
Isometric vs Isotonic contractions:
when does each occur in terms of load?
Isometric: muscle does not shorten during contraction
-> occurs when the load is greater than the force of the muscle contraction; the muscle creates tension when it contracts
-> often used when comparing functional characteristics of different muscle types: records changes in force of muscle contraction independent of load inertia
Isotonic: muscle shortens but tension on the muscle remains constant throughout the contraction
-> occurs when the force of the muscle contraction is greater than the load
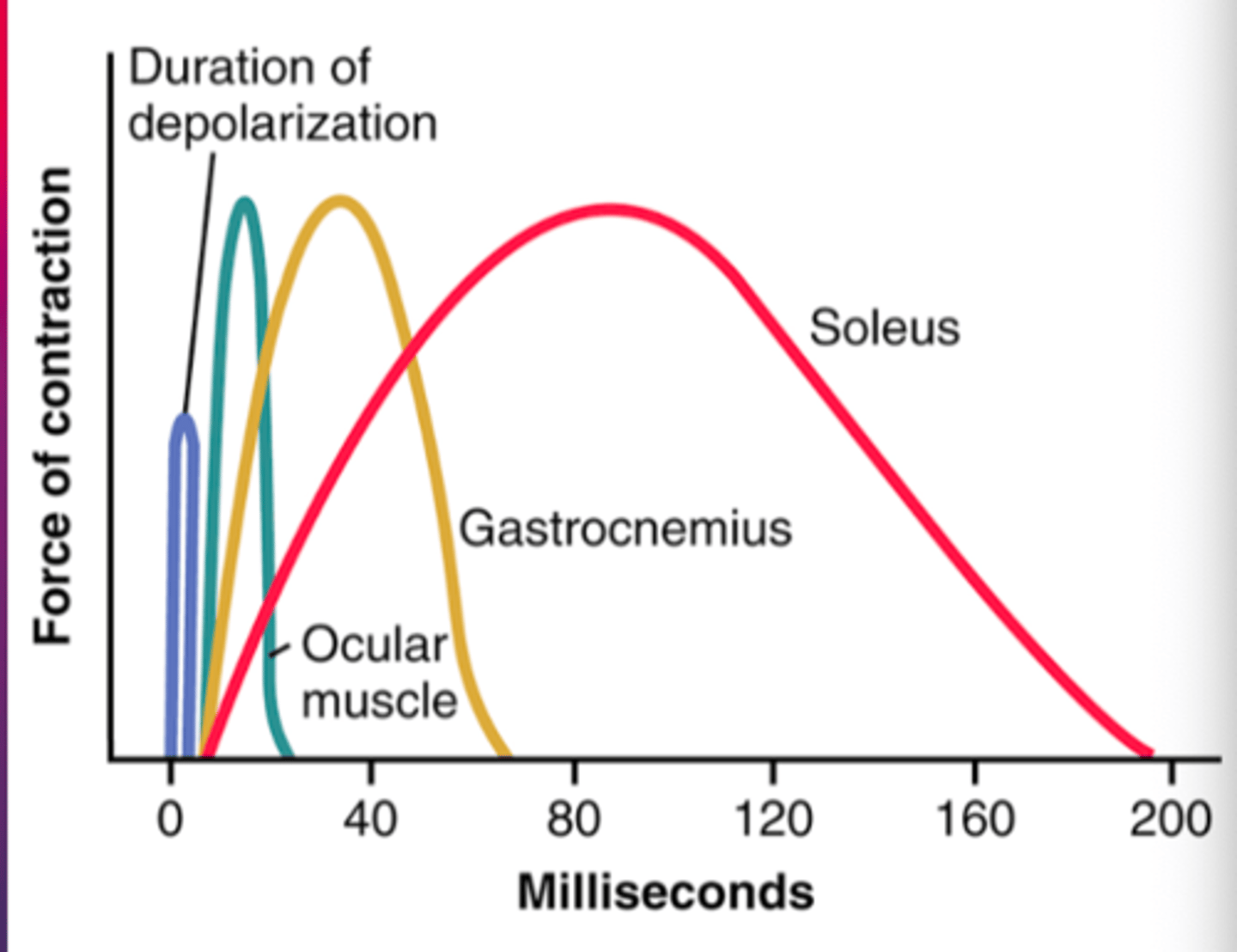
Duration of isometric contractions for different types of mammalian skeletal muscles:
-shows a latent period between action potential (depolarization) and muscle contraction
Ocular movements must be extremely rapid to maintain fixation of the eyes on specific objects to provide accuracy of vision
gastrocnemius muscle must contract moderately rapidly to provide sufficient velocity of limb movement for running/jumping
soleus muscle is concerned principally w/ slow contraction for continual long-term support of body against gravity
Fast vs slow muscle fibers:
fast fibers: muscles that react rapidly (ex. anterior tibialis = mainly fast fibers)
slow fibers: respond slowly but w/ prolonged contraction (ex. soleus)
Type 1 slow fibers- 5 characteristics:
red muscle
1. smaller than fast fibers
2. innervated by smaller nerve fibers
3. have more extensive BV system and more capillaries to supply extra amounts of oxygen
4. greatly increased # of mitochondria to support high levels of oxidative metabolism
5. contain large amounts of myoglobin - stores oxygen until needed, which greatly speeds oxygen transport to the mitochondria
Type II Fast Fibers- 5 characteristics:
White muscle
1. Large for great strength of contraction
2. extensive sarcoplasmic reticulum for rapid release of calcium ions to initiate contraction
3. large amounts of glycolytic enzymes for rapid release of energy
4. less extensive blood supply because oxidative metabolism is of secondary importance
5. fewer mitochondria because oxidative metabolism is secondary
(deficit of myoglobin in fast muscle gives it the name white muscle)
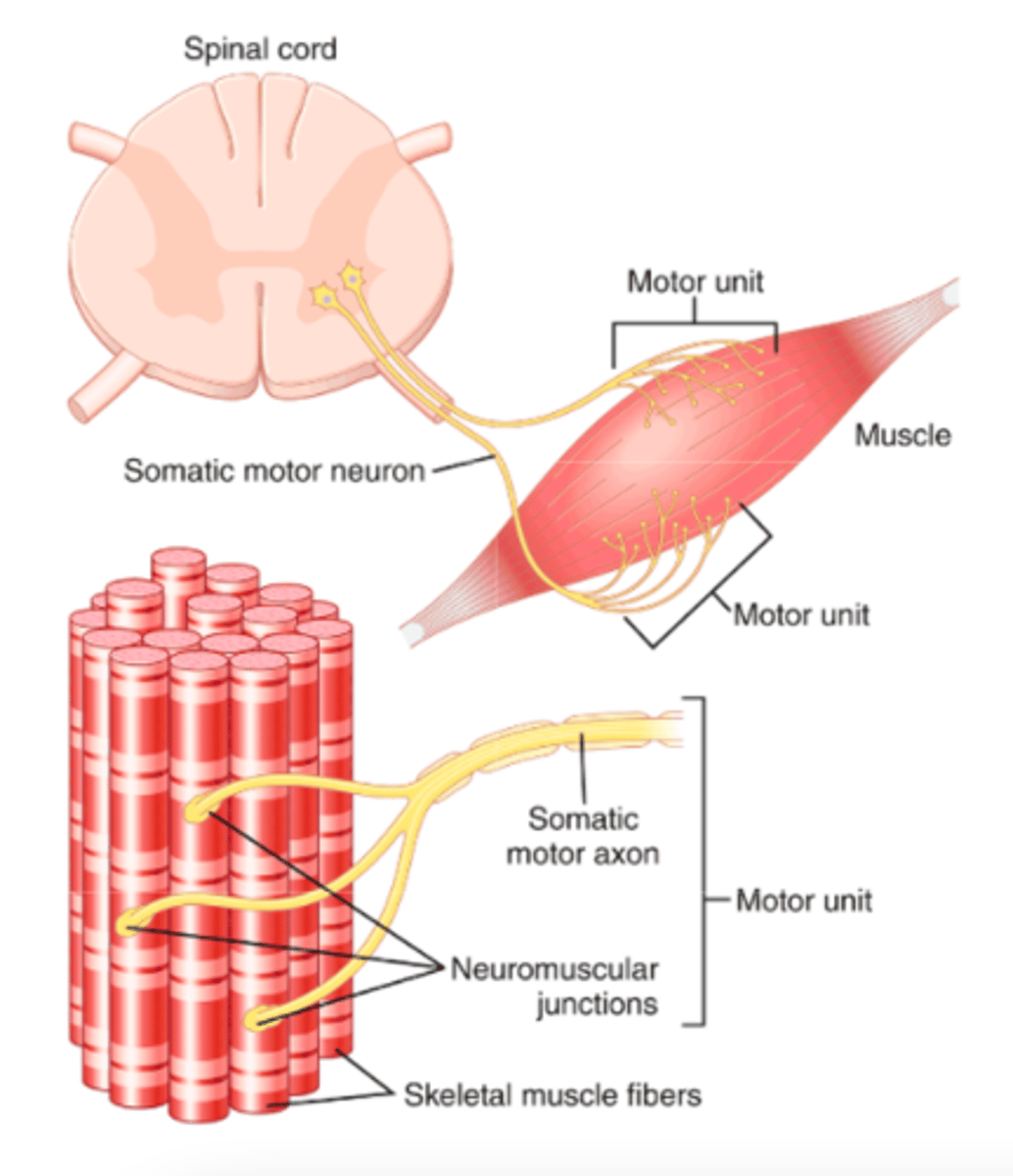
Motor unit:
all the muscle fibers innervated by a single nerve fiber
An entire muscle may receive input from hundreds of different motor neurons
In general, small muscles that react rapidly and whose control must be exact have more nerve fibers for fewer muscle fibers (e.g., as few as two or three muscle fibers per motor unit in some of the laryngeal muscles). Conversely, large muscles that do not require fine control, such as the soleus muscle, may have several hundred muscle fibers in a motor unit.
the muscle fibers in each motor unit are not all bunched together - they overlap other muscle units in microbundles (3-15 fibers) - this interdigitation allows the separate motor units to contract in support of one another rather than entirely as individual segments
Force summation:
in what 2 ways can this occur?
the adding together of individual twitch contractions to increase the intensity of overall muscle contraction
occurs by:
1. increasing # of motor units contracting simultaneously (multiple fiber summation)
2. by increasing the freq of contraction (frequency summation - tetanization)
Size principle:
When the central nervous system sends a weak signal to contract a muscle, the smaller motor units of the muscle may be stimulated in preference to the larger motor units. Then, as the strength of the signal increases, larger and larger motor units begin to be excited
important because it allows the gradations of muscle force during weak contraction to occur in small steps, whereas the steps become progressively greater when larger amounts of force are required
occurs because smaller motor units are driven by small motor nerve fibers, and the small motoneurons in the spinal cord are more excitable than the larger ones
Multiple fiber summation:
size principle = important feature
different motor units are driven asynchronously by the spinal cord; as a result, contraction alternates among motor units one after the other, thus providing smooth contraction, even at low freq of nerve signals
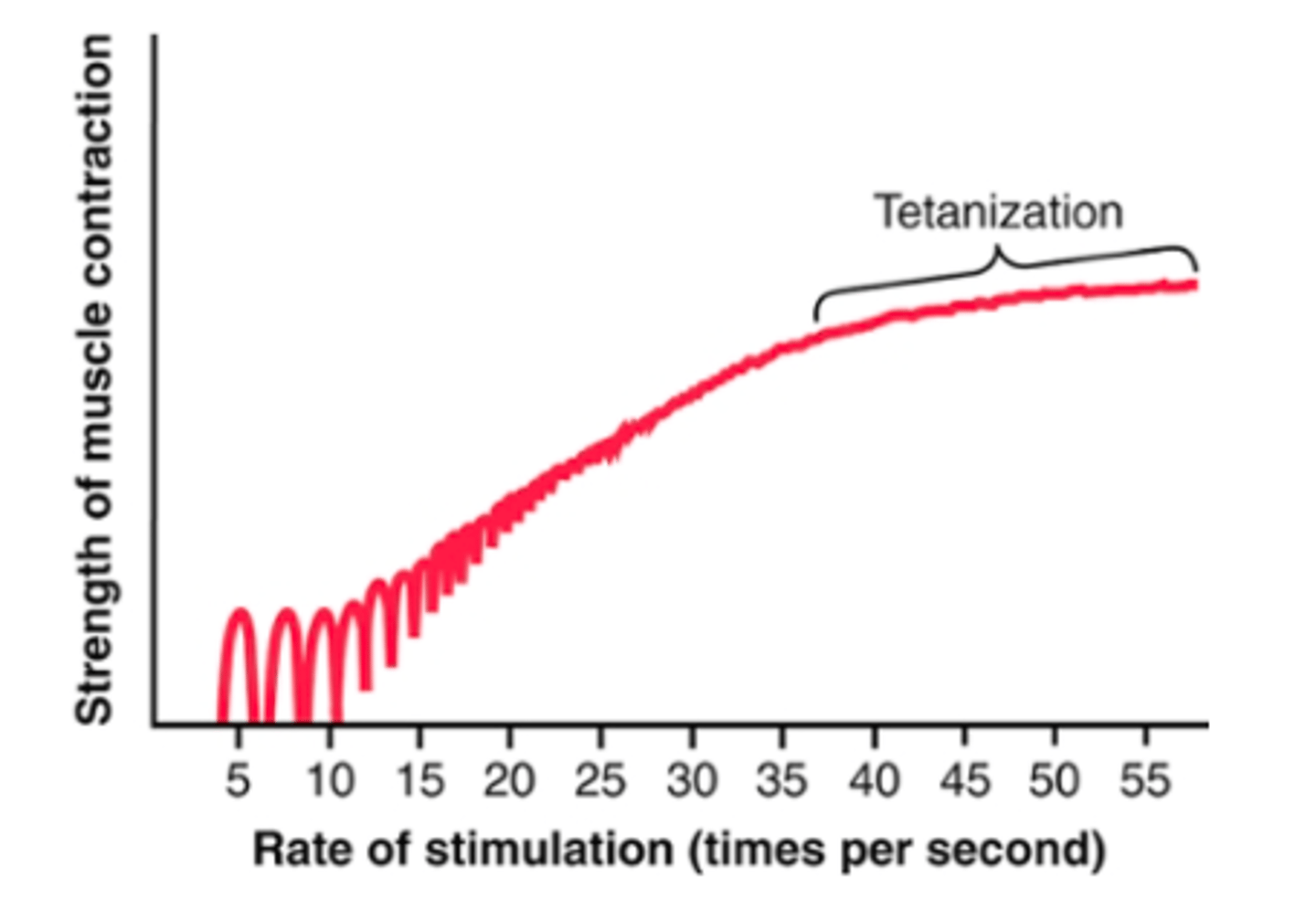
Frequency summation/tetanization:
as freq of individual twitch contractions increases, there comes a point when each new contraction occurs before the preceding one is over
as a result, the second contraction is added partially to the first, and thus the total strength of contraction rises progressively w/ increasing freq
When the frequency reaches a critical level, the successive contractions eventually become so rapid that they fuse together, and the whole muscle contraction appears to be completely smooth and continuous
the strength of contraction reaches its maximum, so any additional increase in frequency beyond that point has no further effect in increasing contractile force
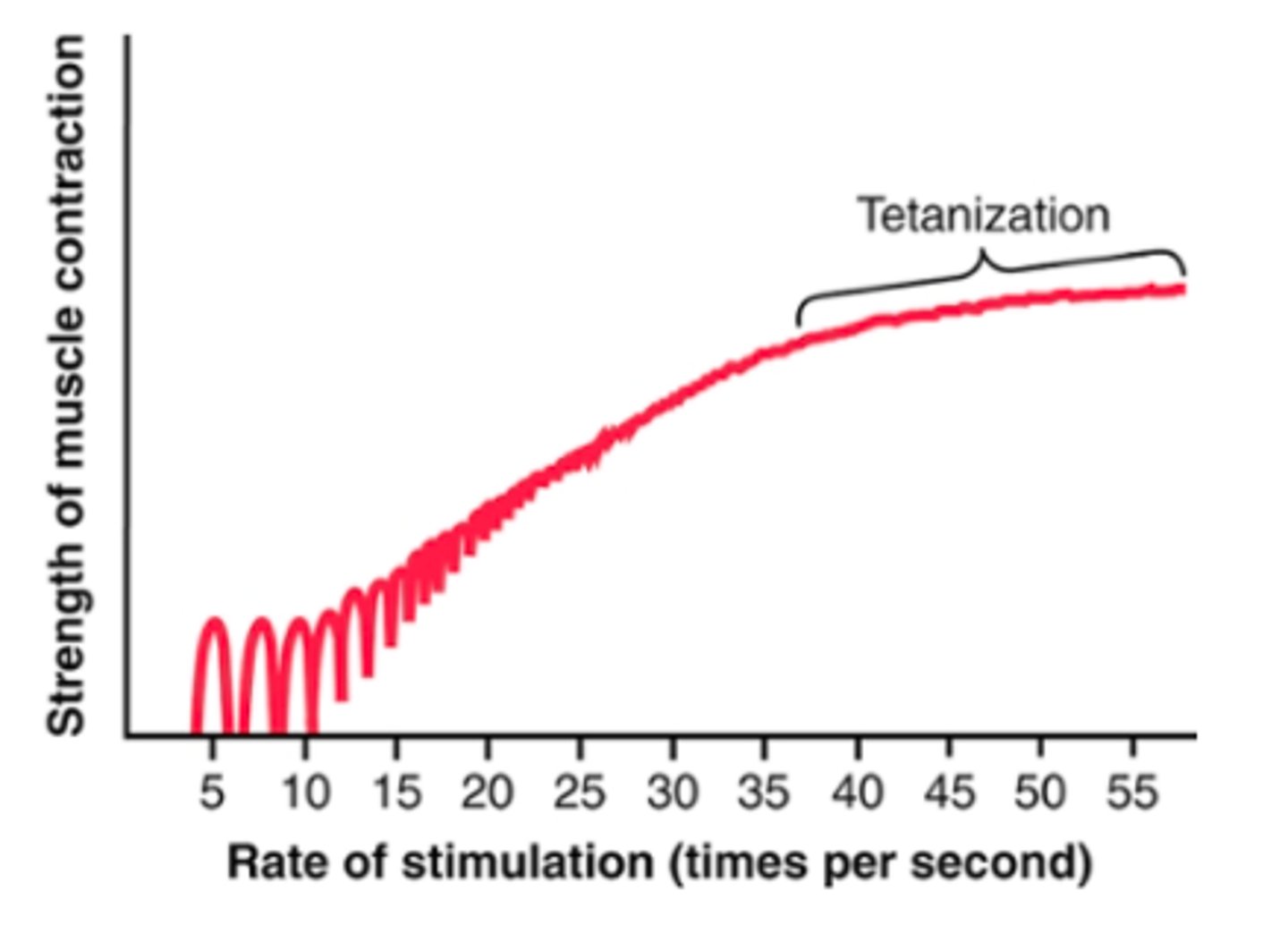
Tetany;
enough calcium ions are maintained in the muscle sarcoplasm, even between action potentials, so that a full contractile state is sustained w/o allowing any relaxation between APs
The staircase effect (Treppe)
when a muscle begins to contract after a long period of rest, its initial strength of contraction may be as little as one-half its strength 10 to 50 muscle twitches later. That is, the strength of contraction increases to a plateau
cause not fully known
believed to be caused primarily by increasing calcium ions in the cytosol because of release of more and more ions from the sarcoplasmic reticulum w/ each successive muscle AP and failure of sarcoplasm to recapture the ions immediately
Muscle tone:
= a certain amount of tautness remaining even when a muscle is at rest
results entirely from a low rate of nerve impulses coming from the spinal cord
-> controlled partly by signals transmitted from the brain to the appropriate spinal cord anterior motoneurons and partly by signals that originate in muscle spindles located in the muscle
Muscle fatigue:
muscle fatigue increases in almost direct proportion to rate of depletion of muscle glycogen
fatigue results mainly from the inability of the contractile and metabolic processes of the muscle fibers to continue supplying the same work output
transmission of nerve signal through the neuromuscular junction can diminish some amount after intense prolonged muscle activity, further diminishing muscle contraction
Interruption of blood flow through a contracting muscle leads to almost complete muscle fatigue within 1 or 2 minutes because of the loss of nutrient supply, especially the loss of oxygen.
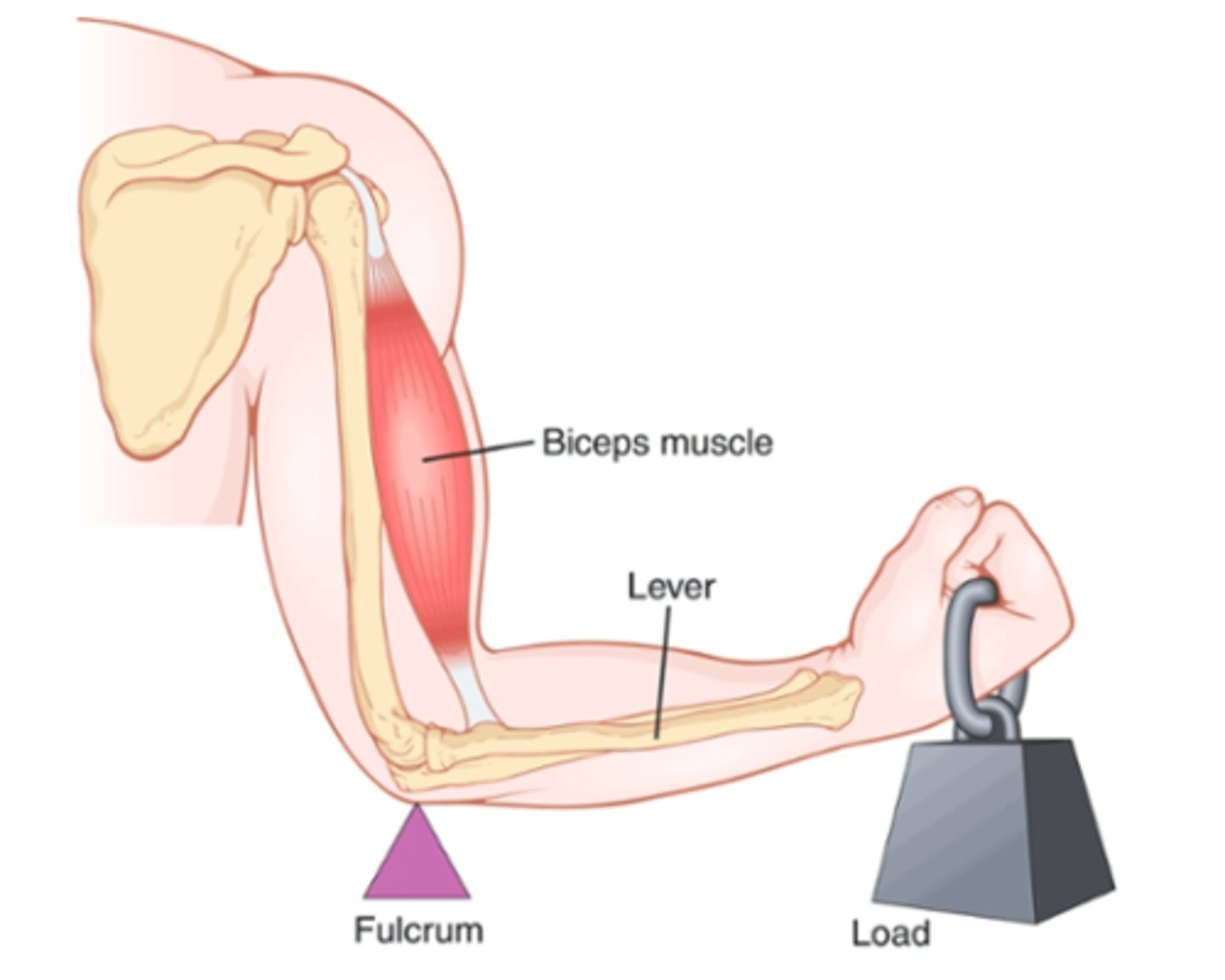
Lever systems:
Muscles operate by applying tension to their points of insertion into bones, and the bones in turn form various types of lever systems
depends on knowledge of:
- point of muscle insertion
-distance from fulcrum of leve
- length of lever arm
-position of lever
The study of different types of muscles, lever systems, and their movements = kinesiology
Agonist and antagonist muscles- coactivation:
Virtually all body movements are caused by simultaneous contraction of agonist and antagonist muscles on opposite sides of joints. (coactivation)
controlled by motor control centers of brain and spinal cord
Recall that an elongated muscle contracts with more force than does a shortened muscle - Therefore, the elongated muscle on one side of a joint can contract with far greater force than the shorter muscle on the opposite side
As an arm or leg moves toward its midposition, the strength of the longer muscle decreases, but the strength of the shorter muscle increases until the two strengths equal each other. At this point, movement of the arm or leg stops.
Thus, by varying the ratios of the degree of activation of the agonist and antagonist muscles, the nervous system directs the positioning of the arm or leg.
How long does muscle remodelling take?
often quite rapid - occurring w/i a few weeks
Muscle hypertrophy:
The increase of the total mass of a muscle is called muscle hypertrophy
Virtually all muscle hypertrophy results from an increase in the number of actin and myosin filaments in each muscle fiber, causing enlargement of the individual muscle fibers (fiber hypertrophy)
occurs to a much greater extent when the muscle is loaded during the contractile process. Only a few strong contractions each day are required to cause significant hypertrophy within 6 to 10 weeks.
Some of the myofibrils have been observed to split within hypertrophying muscle to form new myofibrils, but the importance of this process in the usual enlargement of skeletal muscle is still unknown.
the enzyme systems that provide energy also increase, especially the enzymes for glycolysis, allowing for a rapid supply of energy during short-term forceful muscle contraction
Muscle atrophy;
what system accounts for much of the protein degradation?
When the total mass decreases, the process is called muscle atrophy.
when a muscle remains unused for many weeks, the rate of degradation of contractile proteins is more rapid than the rate of replacement
ATP-dependent ubiquitin proteasome pathway = accounts for much of protein degradation in muscle atrophy
ubiquitin labels cells for proteasomal degradation
Adjustment of muscle length;
type of hypertrophy that occurs when muscles are stretched greater than normal length
causes new sarcomeres to be added at the ends of muscle fibers, where they attach to the tendons
rapid - several per minute
Conversely, when a muscle continually remains shortened to less than its normal length, sarcomeres at the ends of the muscle fibers can actually disappear
Hyperplasia of muscle fibers:
Under rare conditions of extreme muscle force generation, the actual number of muscle fibers has been observed to increase (but only by a few percent), in addition to the fiber hypertrophy process. This increase in fiber number is called fiber hyperplasia
mechanism = linear splitting of previously enlarged fibers
muscle denervation:
tendency of fibrous tissue:
atrophy begins almost immediately
If the nerve supply to the muscle grows back rapidly, full return of function can occur in as little as 3 months but, from then onward, the capability of functional return becomes less and less, with no further return of function after 1 to 2 years.
In the final stage of denervation atrophy, most of the muscle fibers are destroyed and replaced by fibrous and fatty tissue. The fibers that do remain are composed of a long cell membrane with a lineup of muscle cell nuclei but with few or no contractile properties and little or no capability of regenerating myofibrils if a nerve does regrow.
fibrous tissue has a tendency to continue shortening for many months (contracture) - PT important to keep atrophying muscles from developing debilitating and disfiguring contractures= daily stretching of muscles or use of appliances that keep muscles stretched
Recovery of muscle contraction in poliomyelitis:
When some but not all nerve fibers to a muscle are destroyed, as occurs in poliomyelitis, the remaining nerve fibers branch off to form new axons that then innervate many of the paralyzed muscle fibers
results in large motor units = macromotor units
The formation of large motor units decreases the fineness of control one has over the muscles but allows the muscles to regain varying degrees of strength.
Rigor mortis:
several hours after death, all of the muscles of the body go into a state of contracture
the muscles contract and become rigid, even w/o APs
results from loss of all the ATP, which is required to cause separation of cross-bridges from actin filaments during the relaxation process
The muscles remain in rigor until the muscle proteins deteriorate about 15 to 25 hours later, which presumably results from autolysis caused by enzymes released from lysosomes
occurs more rapidly at higher temps
Muscle dystrophy:
include several inherited disorders that cause progressive weakness and degeneration of muscle fibers - replaced by fatty tissue and collagen
Symptoms of DMD include muscle weakness that begins in early childhood and rapidly progresses, so that the patient is usually in wheelchairs by age 12 years and often dies of respiratory failure before age 30 years
Duchenne muscular dystrophy (DMD):
affects only males (X-linked recessive trait)
caused by mutation of gene that encodes for dystrophin
dystrophin = links actins to proteins in the muscle cell membrane
dystrophin and assoc proteins form an interface between intracellular contractile apparatus and extracellular connective matrix
lack of dystrophin causes cell membrane destabilization and activation of multiple pathophysiological processes, including altered intracellular calcium handling and impaired membrane repair after injury.
abnormal dystrophin causes increase in memrbane permeability to calcium, thus allowing extracellular calcium ions to neter the muscle fiber and initiate chnages in intracellular enzymes that ultimately lead to proteolysis and muscle fiber breakdown
Becker muscular dystrophy (BMD)
milder form of DMD
caused by mutation of gene that encodes dystrophin but has a later onset and longer survival