Basics of Insulin & glucose
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
Too much glucose =
hyperglycemia (aka high blood sugar)
Too little glucose =
hypoglycemia (too little blood sugar)
If we have too little of a hormone we give?
a synthetic version of the hormone or a drug that increases the stimulation of the organ to produce more endogenous hormones
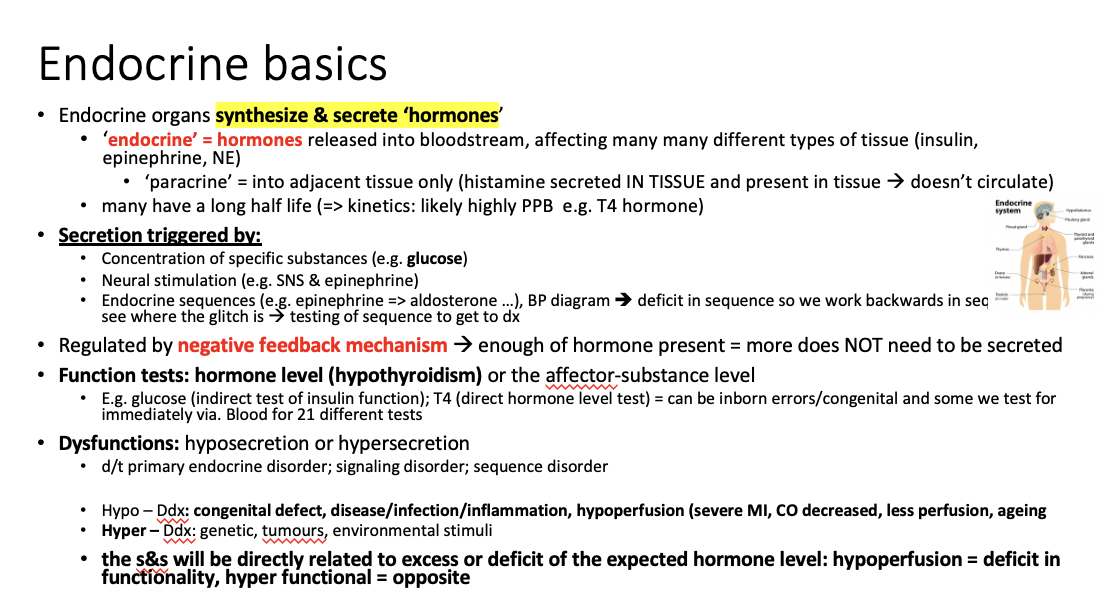
Endocrine organs __________& __________hormones
synthesize and secrete
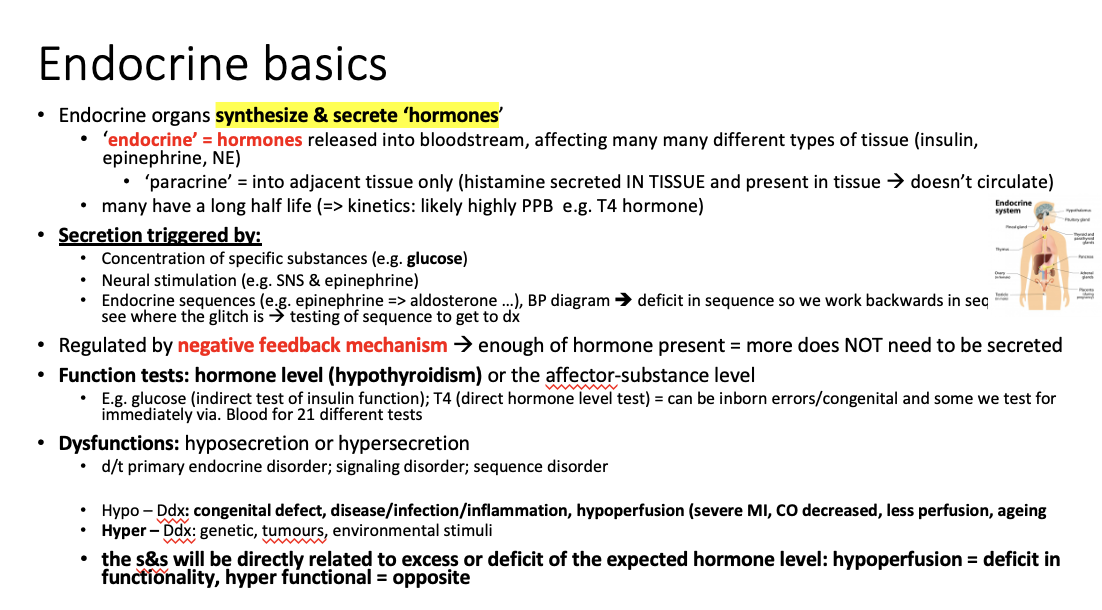
Endocrine means:
hormones released into the bloodstream affecting many different types of tissue
(insulin, epinephrine, NE are all examples of hormones that affect different tissues and organs)
Paracrine means:
hormones that are released into adjacent (neighbouring) tissues only
What are examples of paracrine hormones?
histamine ==> secreted IN tissues and present in tissues
Histamine doesn’t circulate, it stays a local hormone
Endocrine hormones typically have a _____half life d/t kinetics
long ==> likely highly PPB (plasma protein bound)
What’s an example of a hormone with a long ½ life?
T4 = the thyroid hormone
What triggers secretion of hormoned?
concentration of specific substances (ex: high glucose causes the pancreas to release insulin)
neural stimulation via. SNS ==> epinephrine
Endocrine sequences (epinephrine ==> aldosterone); such as the BP sequences where something is in deficit so we work backwards in sequence to see where the glitch is
How do we sometime get a diagnosis of what hormone is “glitching”?
by working/testing the endocrine sequences to see where it’s going wrong
How does NE trigger aldosterone release?
SNS activation: A drop in blood pressure or blood volume causes increased sympathetic nerve activity, leading to the release of NE.
Renin release: NE stimulates beta-1 adrenergic receptors on the juxtaglomerular cells in the kidneys, prompting the release of renin into the bloodstream.
RAAS system end product is aldosterone which induces salt absorption where water follows and raise the BP that way
What mechanism regulates the endocrine system?
Mostly negative feedback:
we have too much of something, we turn it off
we have too little of something, we increase the production
What substance tests insulin function?
Glucose
How do we test the functions of endocrine organs to see if they’re secreting hormones properly?
by testing the level of substance it produces or measuring the hormone levels
Ex: test insulin by checking glucose ==> indirect test
test thyroid hormone levels by checking the T4 hormone ==> direct test
How do we test for congenital endocrine errors?
Via. blood test which is sent for 21 different tests before the baby is even born
What are the dysfunctions of the endocrine system?
hyposecretion & hypersecretion
d/t primary endocrine disorder; signaling disorder; sequence disorder
What are some causes for hyposecretion of a hormone?
congenital defects
disease/infection/inflammation
hypoperfusion (severe MI, CO decreased, aging)
What are some causes for hypersecretion of a hormone?
genetics
tumors
environmental stimuli
The s&s will be directly related to excess or deficit of the expected hormone level:
hypoperfusion = deficit in _________________
hyper functional = opposite ==> too efficient
functionality
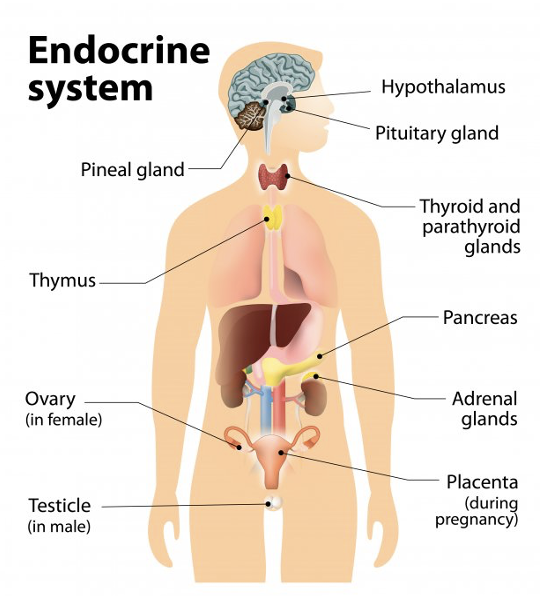
What are some of the glands of the endocrine system?
hypothalamus ==> anterior and posterior pituitary glands
pineal gland ==> sleep hormone
Thyroid and parathyroid
thymus
Pancreas
ovary
Adrenal glands
Placenta
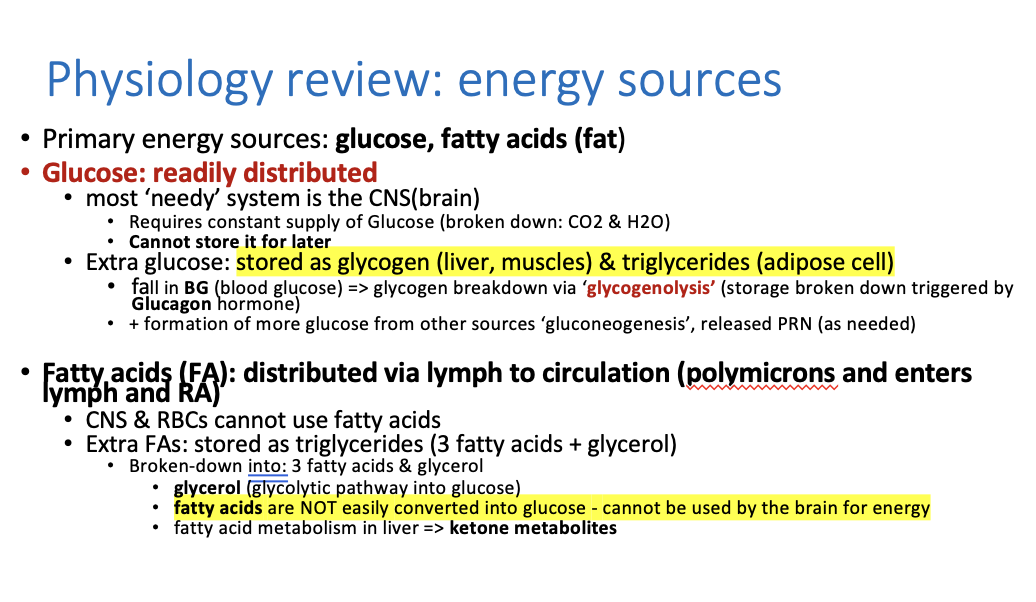
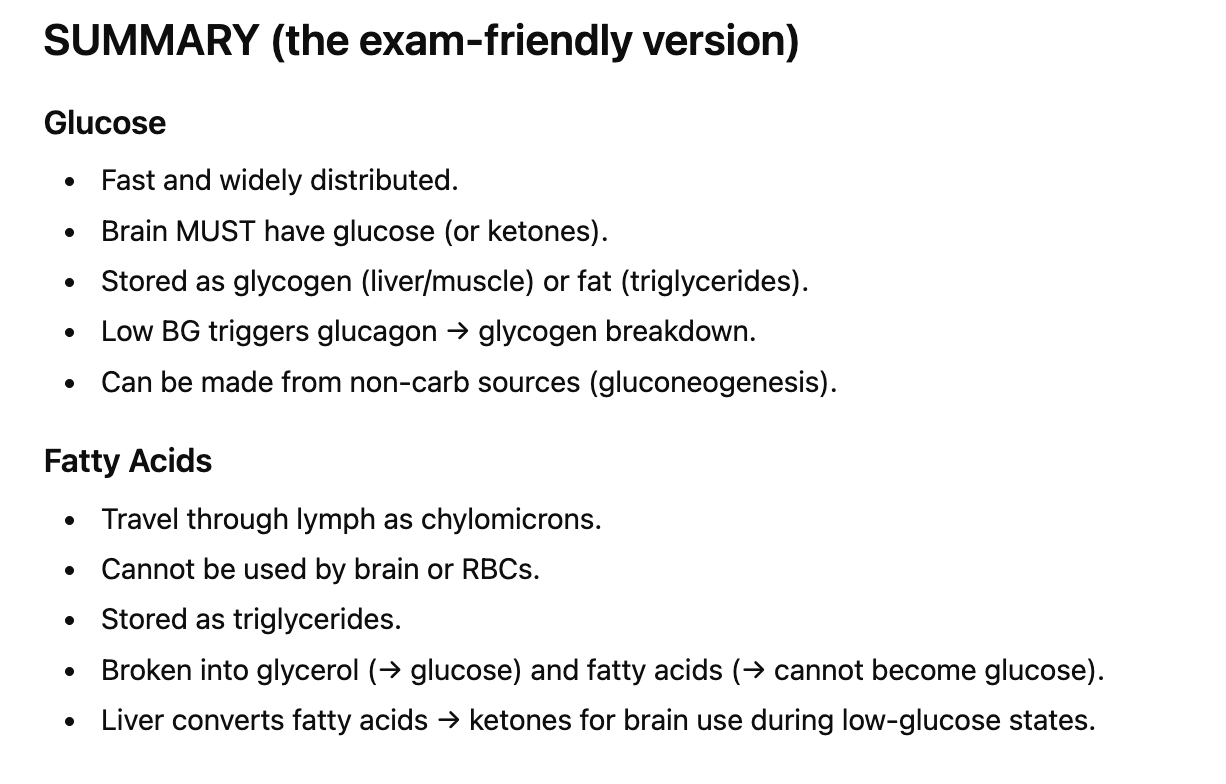
What are the 2 main primary energy sources for the body?
glucose, fatty acids (fat)
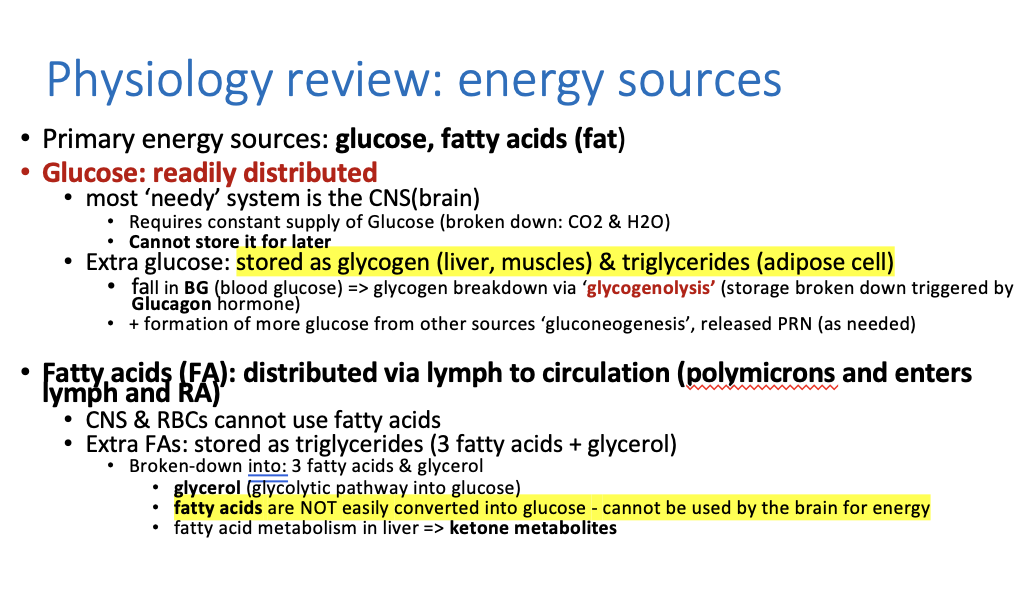
Glucose is readily distributed and most needed by the _______
CNS ==> brain
it requires a constant supply of glucose
this is then broken down into CO2 and H20
What does the brain use to survive if glucose isn’s available?
It uses ketones
you CANNOT store glucose for later, true or false?
False!!, you CAN store extra glucose
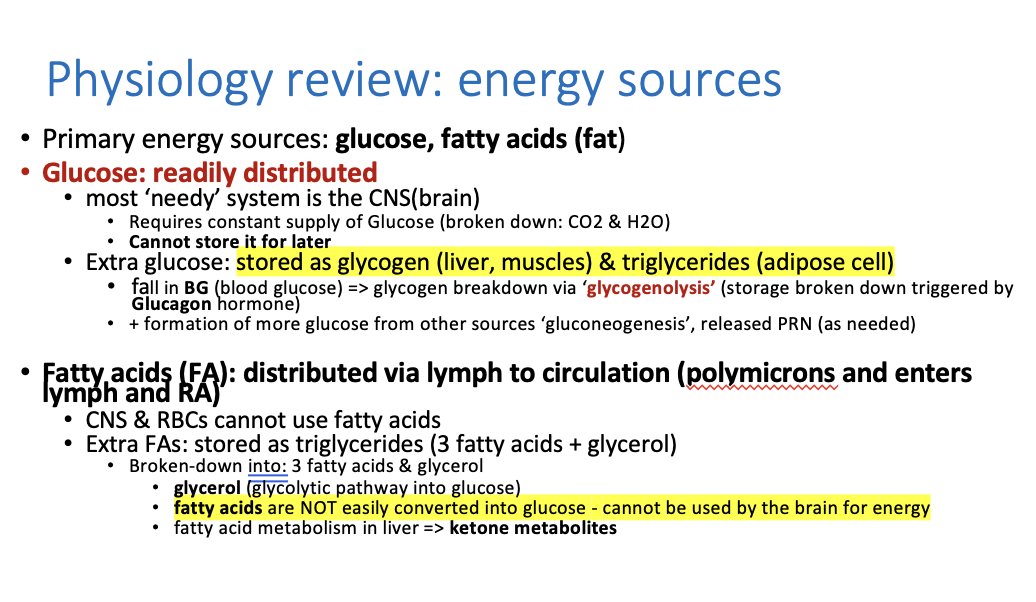
what happens with the extra glucose?
it turns into glycogen stored in the liver and muscles and as triglycerides (in adipose/fat tissue).
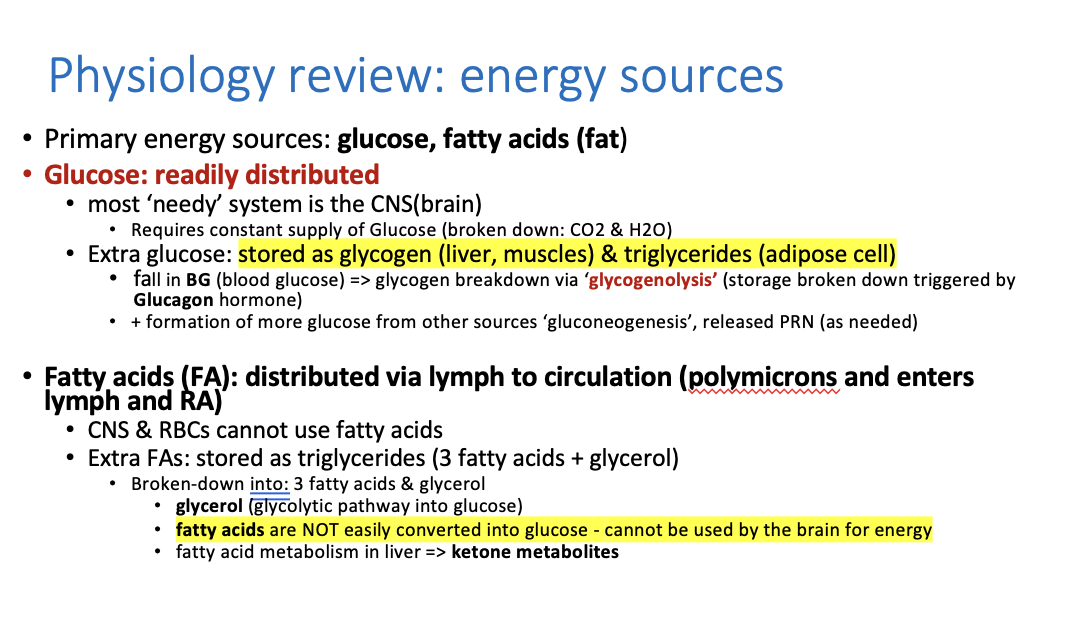
Extra glucose is turned into:
A. Glycogen (short-term storage)
Stored in liver and muscles.
When blood sugar drops → body breaks down glycogen via glycogenolysis (triggered by glucagon).
B. Triglycerides (long-term fat storage)
Stored in adipose (fat) tissue.
If glucose is low for a long time:
Body makes new glucose from non-carbs through gluconeogenesis (proteins, glycerol, lactate, etc.).
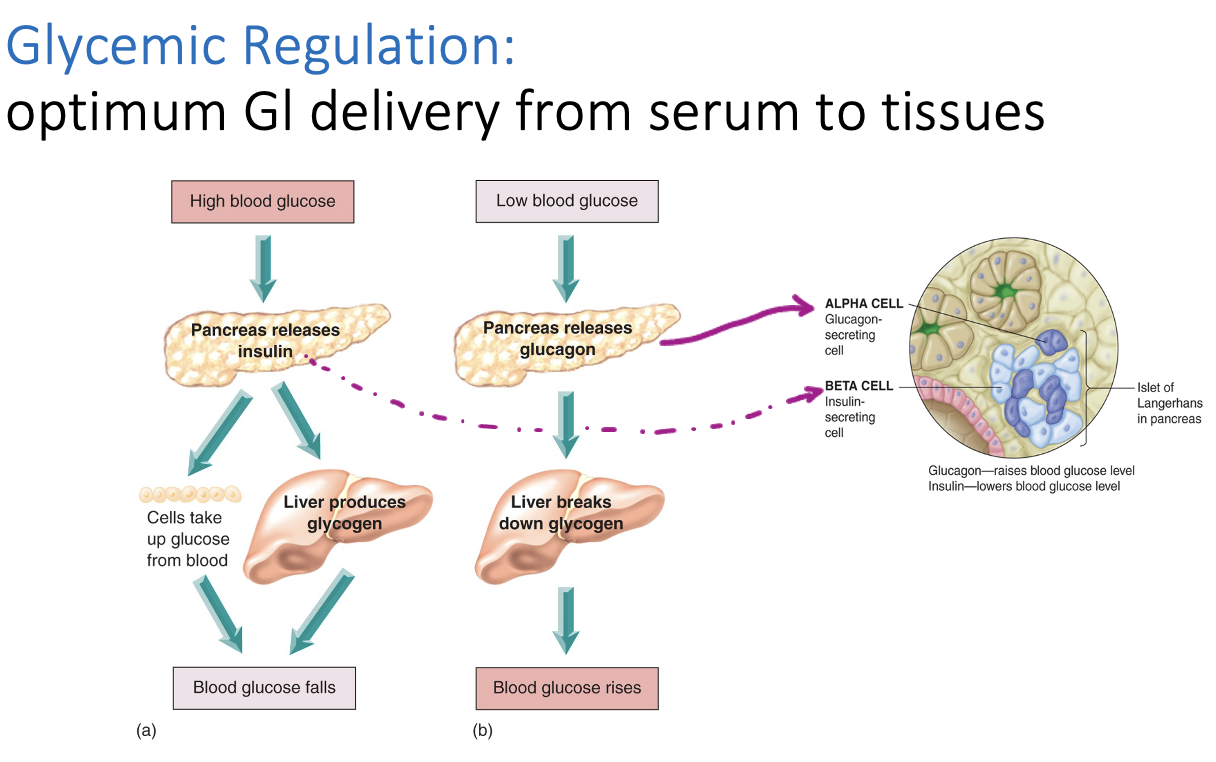
What happens when there’s a drop/fall in blood glucose?
Glycogen gets broken down via. “glycogenolysis” into glucose again
What triggers the breakdown of glycogen into glucose again?
The hormone glucagon, it stimulates the body to break down glycogen
What is gluconeogenesis?
Formation of more glucose from other sources that’s released as needed
What happens to fatty acids after they’re digested in the small intestine?
They’re distributed via lymph as chylomicrons into circulation and travels to the right atrium
_______ and _________can’t use fatty acids
CNS & Red blood cells can’t use fatty acids
hence why we don’t store fat in the brain
What happens when the body breaks down triglycerides?
Extra fat/FA is stored as triglycerides and can be broken down into 3 fatty acids + glycerol
Fatty acids are NOT easily converted into glucose - cannot be used by the ___________ for energy
brain
What does the body do when glucose is low, aka. when someone is fasting?
When glucose is low (fasting, starvation, low-carb diet):
Liver breaks fatty acids into ketone bodies
**Ketones can cross into the brain and be used for energy
This is what happens in ketosis.
What provides glucose movement into cells and out of circulation?
Insulin
Summary:
Glucose and fatty acids are the main sources of energy
Glucose gets turned into glycogen or fat
Fat is turned into triglycerides
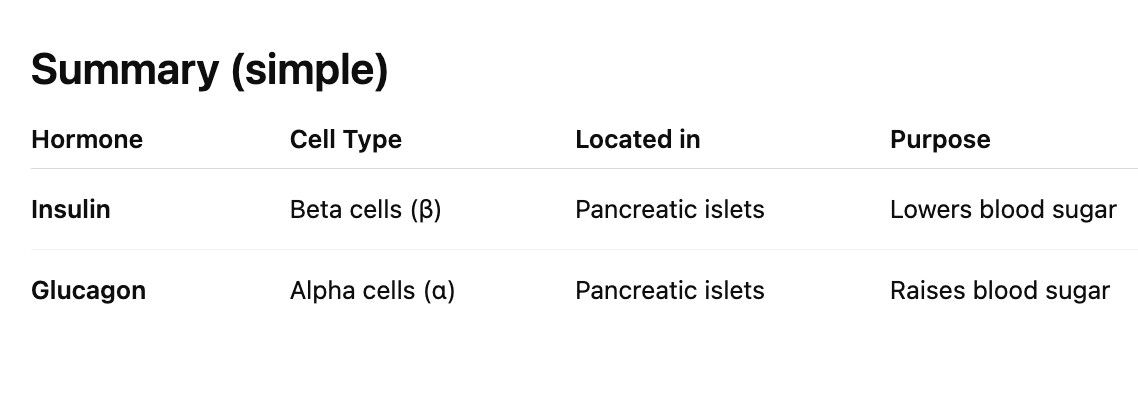
What is insulin?
A pancreatic hormone produced by the beta cells (β-cells) in the islets of Langerhans.
Released when blood glucose is high (like after eating).
What are the main job of insulin?
1. Helps glucose enter cells
👉 “Glucose’ cellular uptake”
Insulin acts like a key that unlocks cells so glucose can enter and be used for energy.
Insulin also tells the body to __________energy and not break it down
store
It increases:
Glycogen synthesis (stores glucose in liver & muscle)
Triglyceride synthesis (stores fat in adipose tissue)
Protein synthesis (builds muscle & tissues)
Insulin prevents:
Glycogen breakdown
Fat breakdown
Protein breakdown
Because the body wants to use glucose first, not burn stored energy
Insulin helps ___________also enter cells, not just glucose
amino acids enter cells
→ Supports protein building
→ Helps triglycerides enter fat cells for storage
Insulin = anabolic hormone (“builds & stores”).
3 actions of insulin?
glucose celular uptake
promotes storage formations > glycogen synthesis, triglyceride synthesis and protein synthesis. > insulin stores glycogen, triglycerides and protein
Amino acid cellular uptake
Where is Glucagon (hormone) synthesized/made?
in the alpha cells
It is the opposite of insulin.
Released when:
Blood sugar is LOW
Between meals
During hypoglycemia
Where does insulin and glucagon come from?
Insulin and glucagon come from specific cells in the pancreas
Beta (sweet) cells create insulin
Alpha cells create glucagon
Function: raise blood glucose by releasing stored energy.
What does glucagon do?
Promotes breakdown of stores to release glucose:
glycogenolysis (glycogen breakdown)
lipolysis (triglyceride breakdown)
gluconeogenesis (amino acid conversion into glucose)
What triggers glucagon release?
Glucagon is triggered by low plasma glucose levels (low glucose in blood)
(between meals; hypoglycemia) => leads to mobilizing stores to release more glucose into blood and replenish blood glucose for cellular use
What is glycogen?
stacks of glucose
once we run out of glycogen, we start to breakdown other things like protein and blood glucose rises
What is the normal glucose range?
4-8 mmol/L = feeling great
***we often like to see it at 5 in diabetic patients, has to be in range at all times
High blood glucose vs. low blood glucose
blood sugar regulation
Cells have to uptake glucose via. insulin
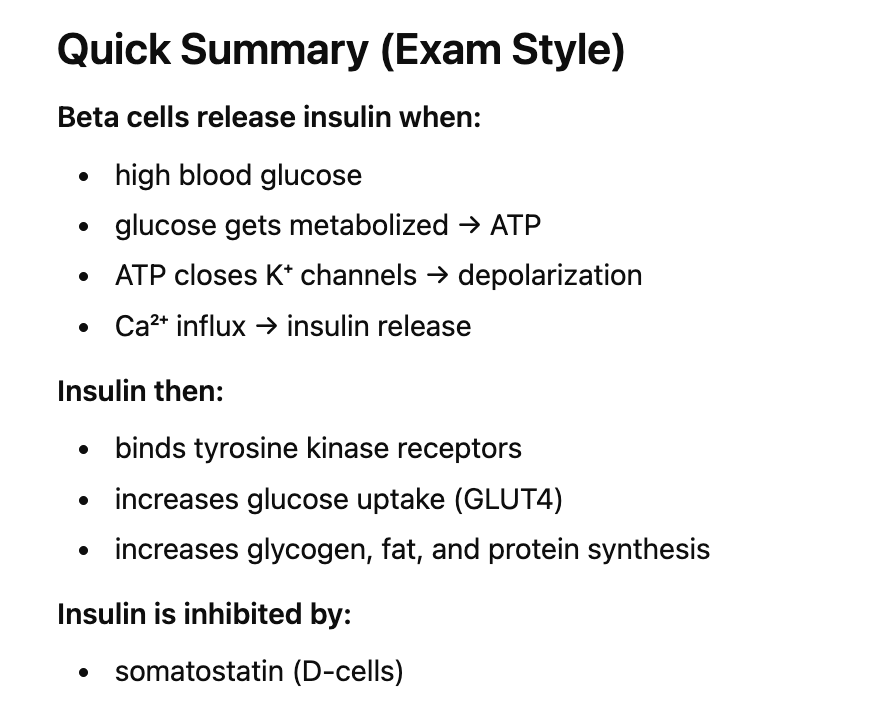
What triggers insulin synthesis in the beta cells?
stimulant is high serum glucose
so high glucose in blood triggers insulin synthesis and secretion
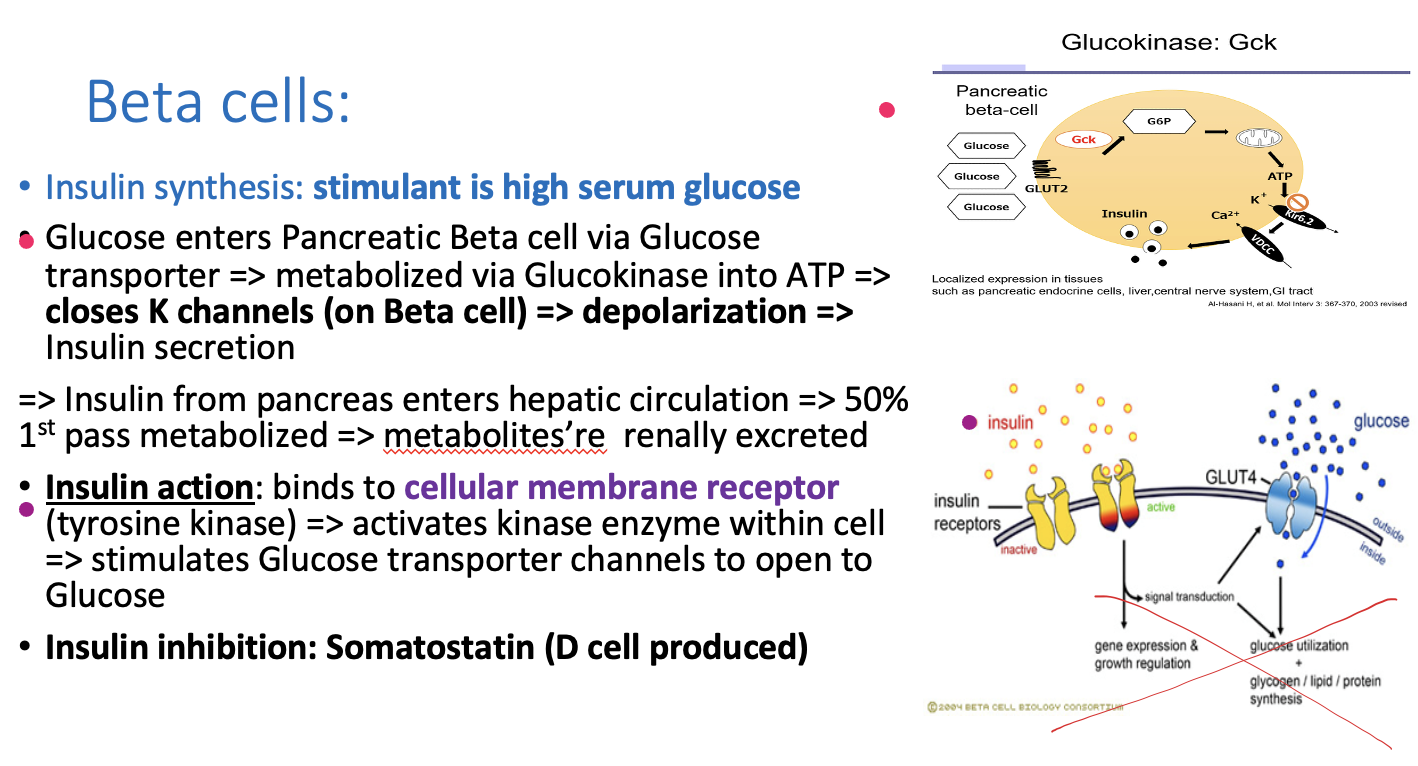
How does glucose enter pancreatic beta cells?
Glucose enters beta cells through glucose transporter
The glucose is then metabolized via. Glucokinase into ATP
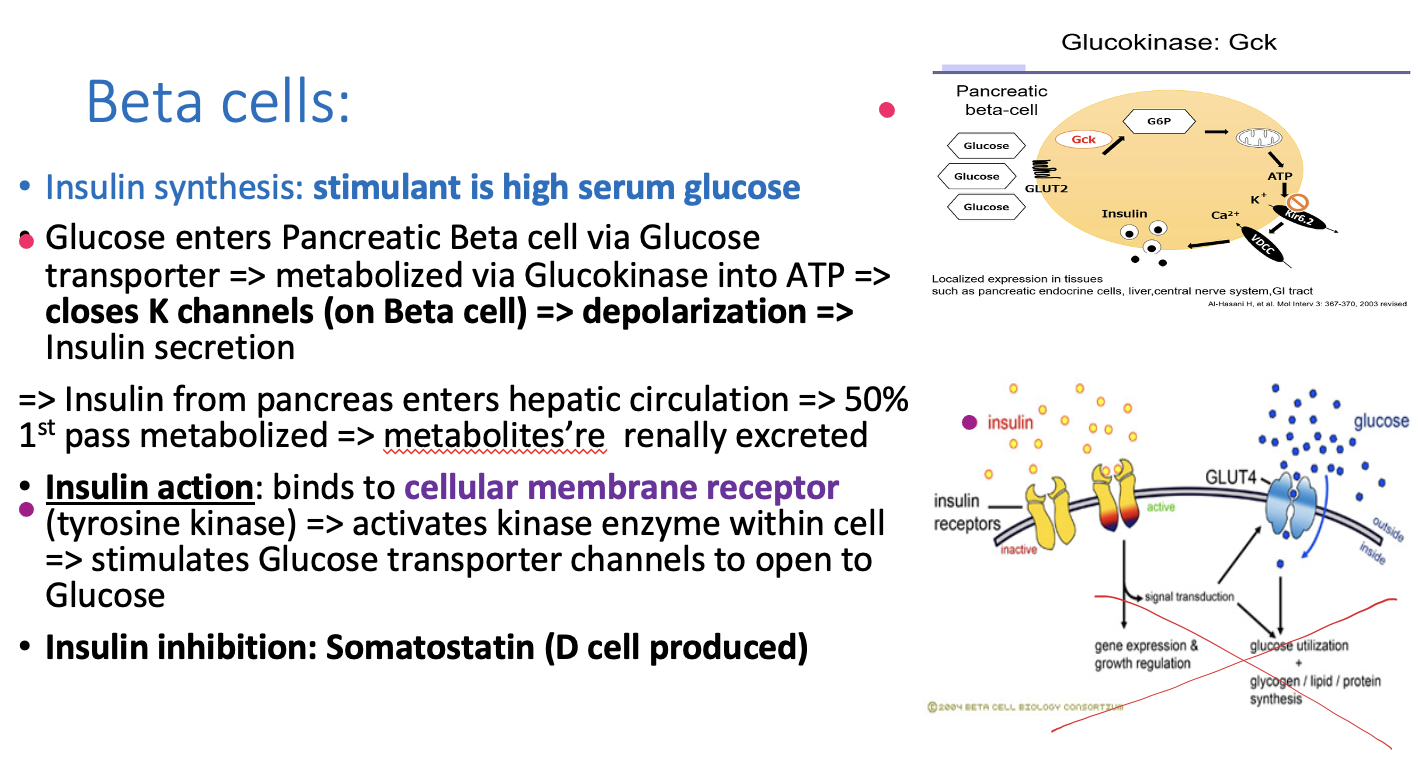
How is insulin released?
Step 1: Glucose (substance) enters beta cells via. glucose transporter
Step 2: Glucose is metabolized via. Glucokinase (enzyme) into G6P
G6P produces ATP
Step 3: ATP closes K⁺ channels, potassium cannot leave cell
Step 4: Cell depolarizes because cell is positive due to K+
Step 5: insulin is secreted
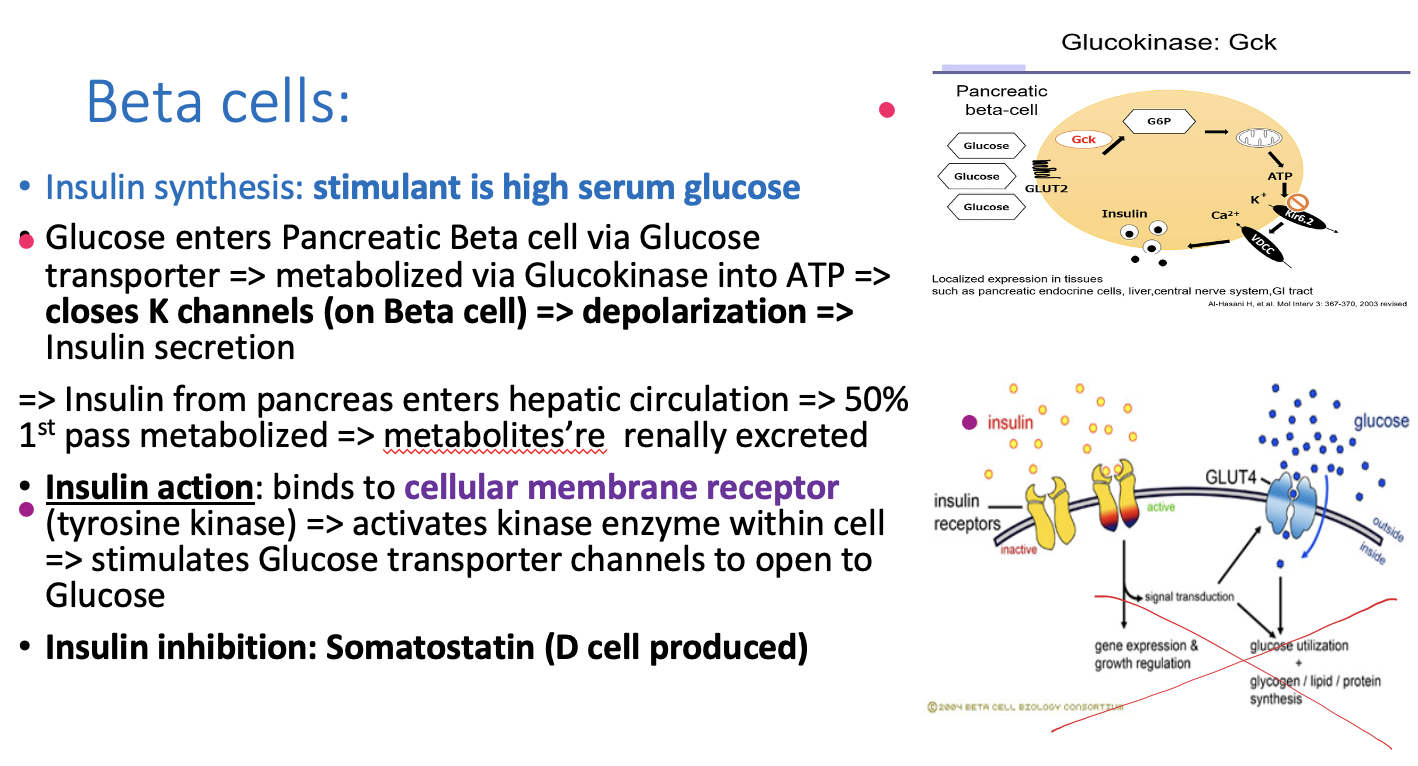
What happens after to insulin after it’s released from pancreas?
insulin from pancreas enters hepatic circulation (insulin goes to liver, 50% is metabolized)
insulin metabolites are renally excreted after metabolization and
insulin goes into bloodstream
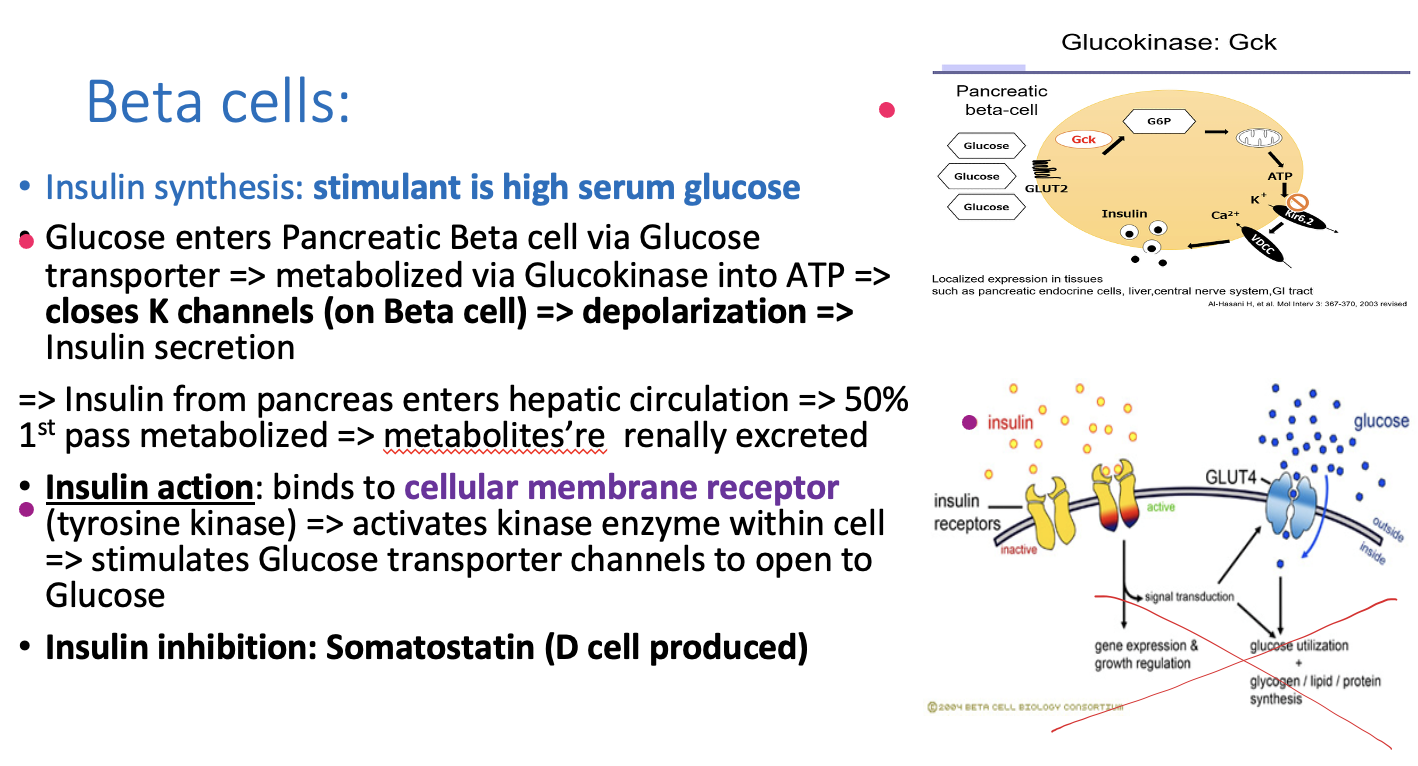
What is insulin’s action after it’s released into systemic circualtion ?
insulin binds to cell membrane receptor called tyrosine kinase
> activates kinase enzyme within cell > ==> stimulates glucose transported channels to open to Glucose and take in glucose
Insulin binds to tyrosine kinase ==> Opens up another glucose channel and trickle into that cells
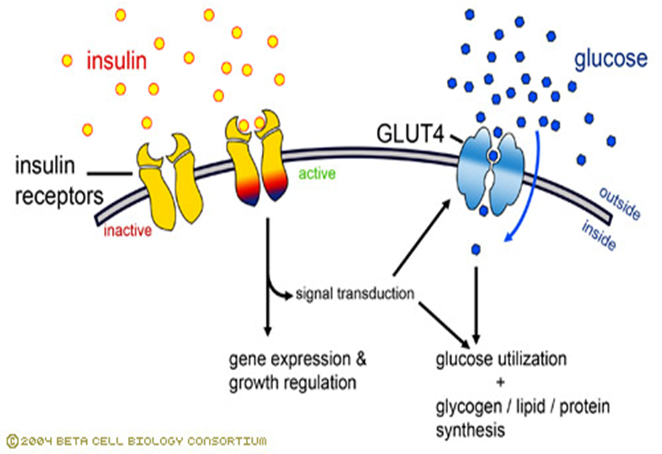
What inhibits Insulin?
Somatostatin (D cell produced)
Absence of glucose shuts down __________
insulin
What’s a lab value that can be a precurssor to diabetes?
Hemoglobin A1C and steroids both can cause diabetes
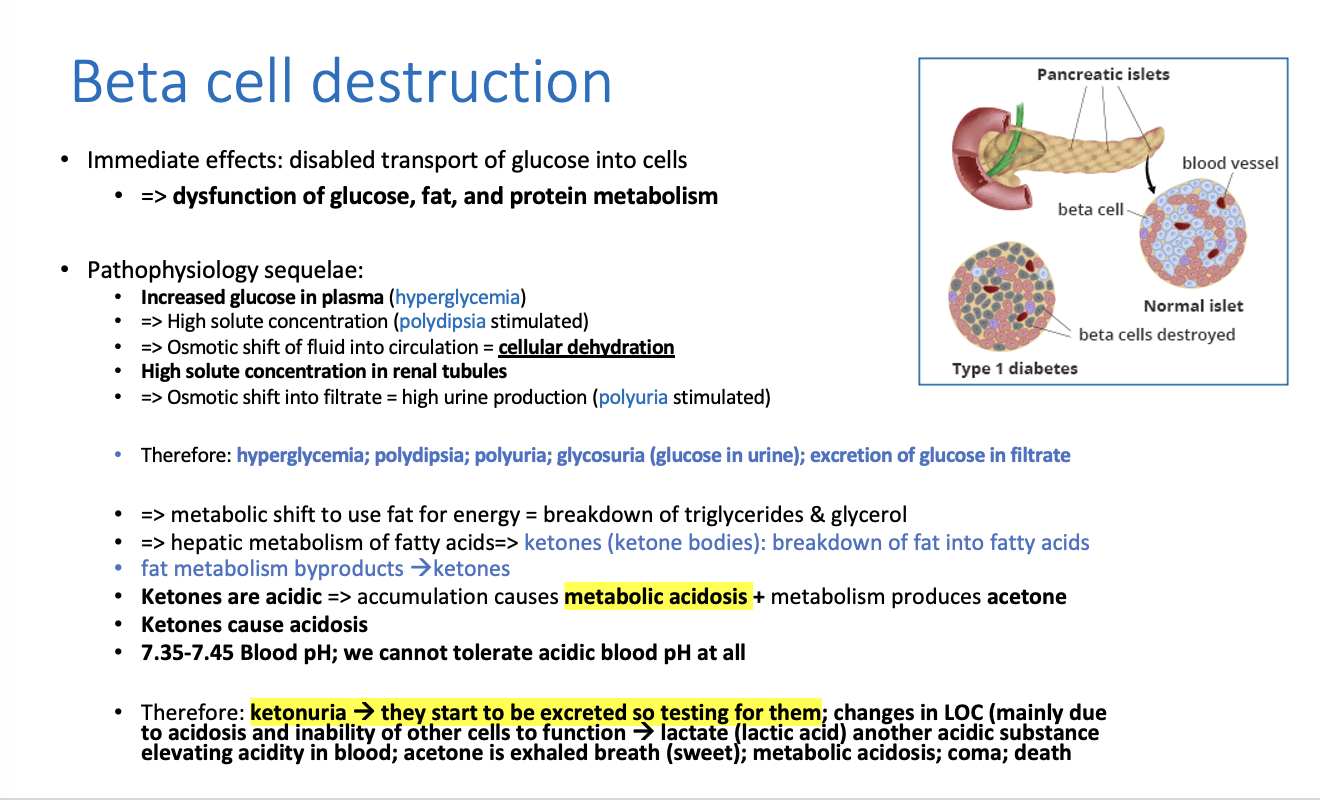
What happens if the beta cells are destroyed (immediate effect)?
beta cells being destroyed means disabled transport of glucose into cells, because without beta cells you don’t have insulin and you need insulin
==> dysfunction of glucose, fat, & protein metabolism
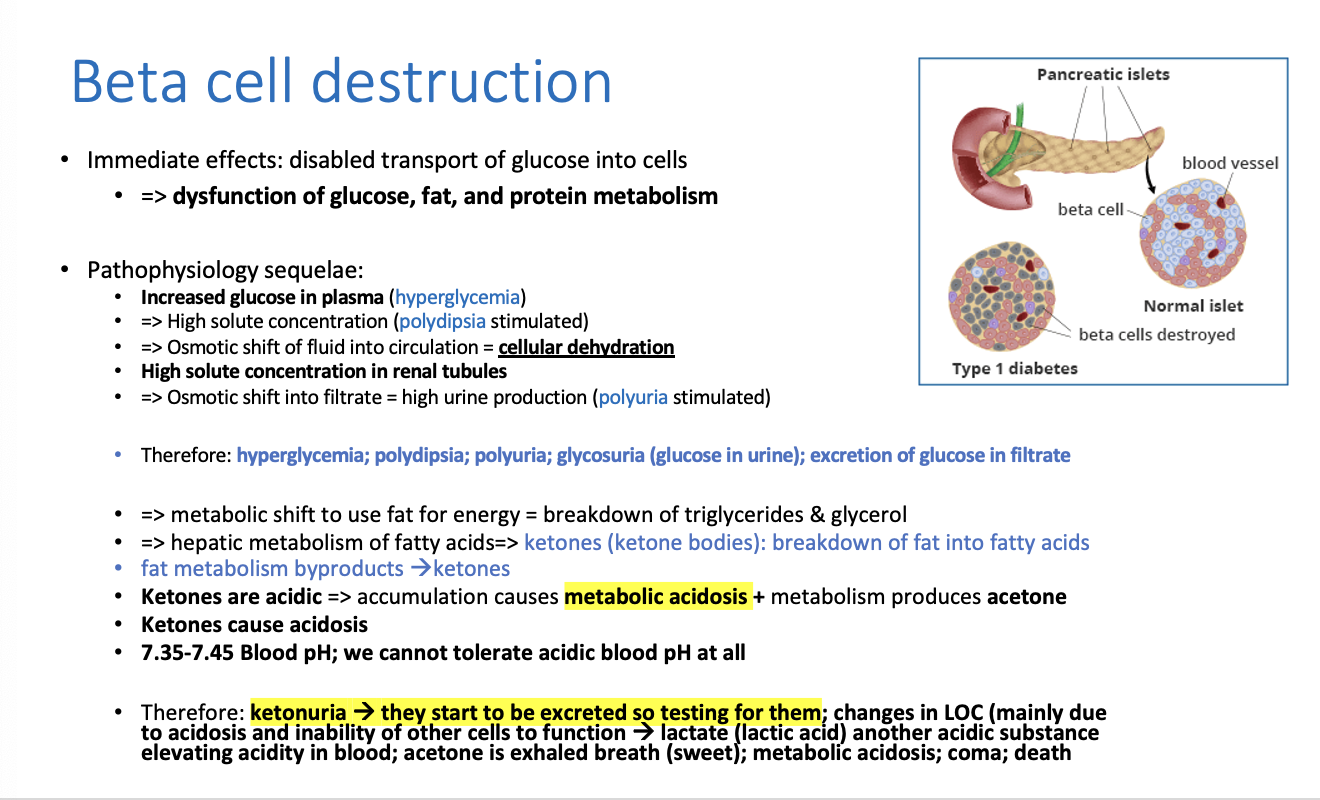
What is the results of beta cell destruction/side effects?
hyperglycemia (because glucose stays in blood without insulin)
High solute (glucose) concentration (polydipsia ==> excessive thirst occurs), so low water and high solute = cells become dehydrated
Osmotic shift of fluid into circulation = cellular dehydration
Polyuria (excessive urination): Osmotic shift into filtrate = high urine production (polyuria stimulated)
Triad of Side effects d/t hyperglycemia
So the classic triad appears:
Hyperglycemia
✔ Polydipsia
Polyuria
Glycosuria —> glucose in urine and filtrate
With high glucose in blood, it leads to:
Breakdown of triglycerides and fats because the CELLs cannot use glucose despite in being in bloodstream ==> leads to ketones as a byproduct
a metabolic shift to use fat for energy = so breakdown of triglycerides and glycerol
> hepatic (liver) metabolism of fatty acids > ketones (ketone bodies are produced) because of fat metabolism
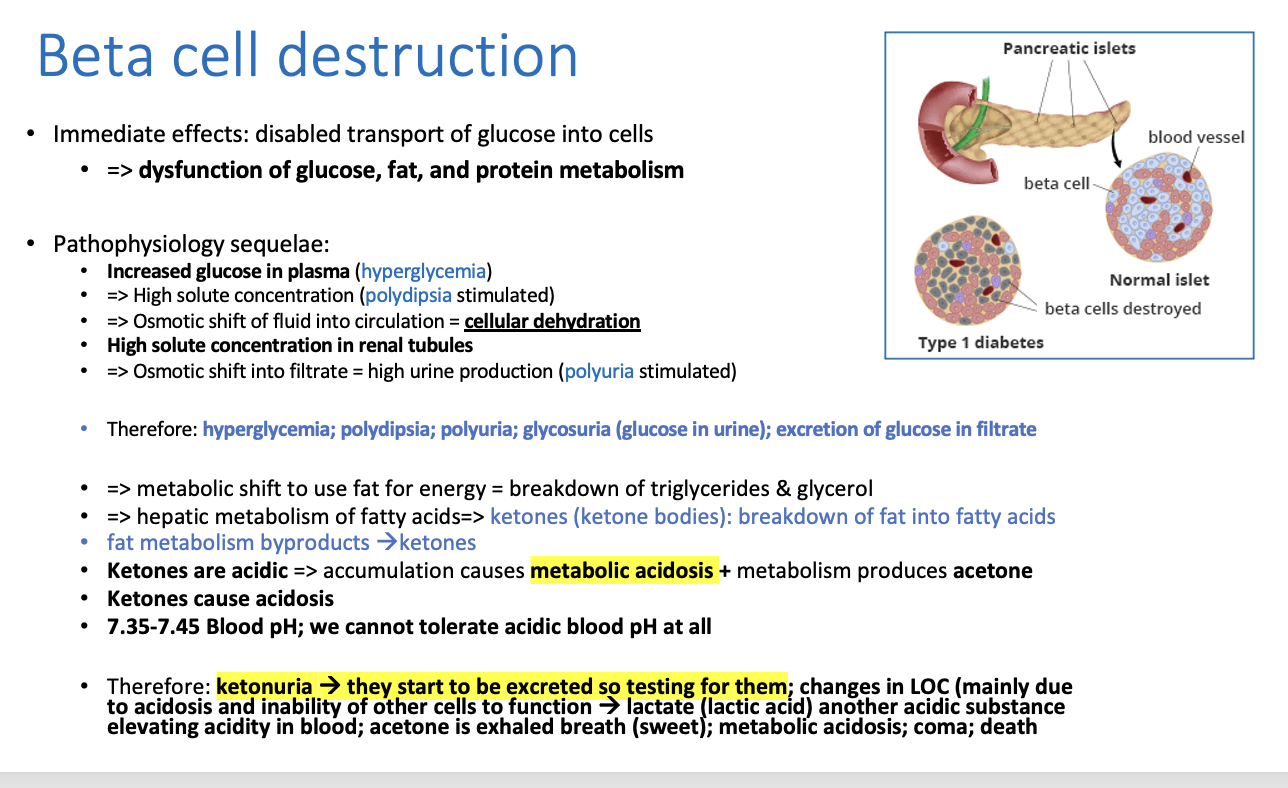
fat metabolism byproducts:
KETONES —> acidic
ketones accumulate and cause metabolic acidosis (DKA)
As ketones accumulate:
Blood becomes acidic
Blood pH drops (below normal 7.35–7.45)
Acetone is volatile → sweet, fruity breath.
What does acetone as a byproduct of DKA cause?
Acetone is volatile → sweet, fruity breath.
Ketones in urine =
ketonuria ==> they start to be excreted so we test for them
What are side effects of DKA?
changes in LOC (due to acidosis and inability of other cells to function)
lactate —> lactic acid —> elevates blood acidity
acetone is exhaled in breath
coma
death
When osmotic pressure is called oncotic pressure, its because _________is the influencer
protein
What is the disease name where beta cells are destroyed?
Type I diabetes
Ketone bodies metabolism
Liver
Makes ketones
From fatty acids
Low glucose trigger
What are the consequences of reduced glucose uptake?
glucose is low and we don’t have energy, therefore:
Fat breakdown == ketones
Fat stores are depleted so then: proteolysis (muscle wasting)
Lipolysis ==> fatty acid breakdown
liver metabolism of fatty acids (fatty acid oxidation) ==> ketones and ketonuria
Depletion of fat stores ==> proteolysis (smooth muscle then gets broken down and functionality decreases = severe effects of weight loss & muscle wasting)
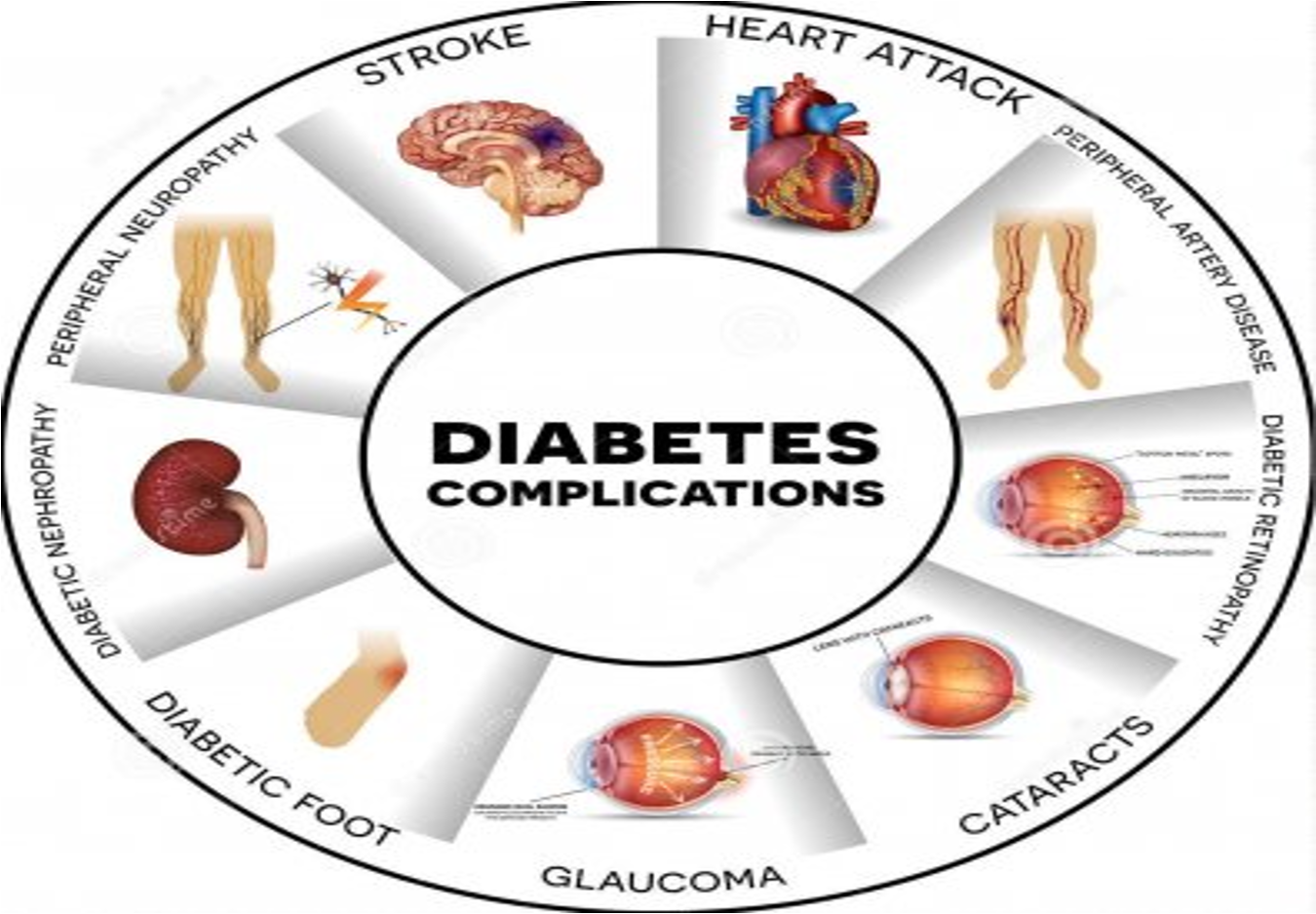
What altered cell functions are seen with reduced glucose reuptake?
insulin resistance ==> in cells that actually need it because they have decreased functionality, so they got used to not having insulin
Altered cellular repair
endothelial dysfunction and decreased angiogenesis (no new blood vessels)
increased ROSS > inflammatory response (oxidative particles hurt the cells)> risk for clotting
organ injury ==> organs will suffer first
Why won’t the cells respond to insulin when we first administer it?
We won’t see immediate results because cells aren’t used to the insulin so when we administer insulin we have to wait a bit to see
What is our #1 priority even before giving insulin?
Restoring normal hydration because the cells are dehydrated d/t high solute concentration
so rehydrate the cells in order for them to respond to insulin
**-Dehydration and depleted energy led to complete dysfunction of cells