ECHO 3 : Valvular Stenosis
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
what can cause valvular stenosis?
congenitall abnormal valve
post inflammatory
age related
which valve does rheumatic disease affect first?
mitral
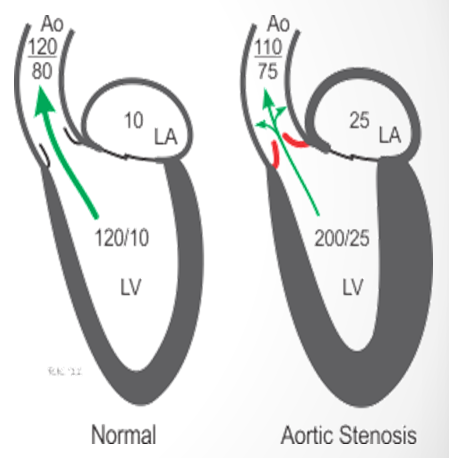
valvular stenosis results in
pressure overload
what is the ventricular vs atrial responsce to pressure overload?
ventricular → hypertrophy
atrial → dilatation
how does a narrowed orifice affect velocity?
smaller the opening, the greater the velocity of the jet
what occurs as a result of aortic stenosis?
concentric left ventricular hypertrophy
(LV must generate higher pressure to move blood through. It does this by thickening muscular walls EQUALLY aka concentric)
what are the symptoms of severe AS?
fatigue
decreased exercise tolerance
chest pain
difficulty breathing on exertion
aortic sclerosis is common in
adults older than 65 (25% have it)
what is ao sclerosis?
focal areas of increased echogenicity without significant obstruction
in ao stenosis what kind of data is recommended to provide functional valve area
doppler data
what accounts for most cases of severe AS in adults younger than 70?
bicuspid aortic valve (accounts for 2/3 of those cases)
what is raphes?
lines present where the valve does not open (typically in larger leaflet) so when closed valve looks trileaflet
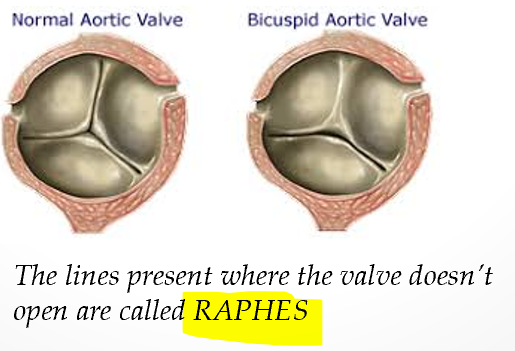
should bicuspid ao valve be diagnosed in diastole or systole?
systole because in diastole when it is closed the raphe may make it appear trileaflet
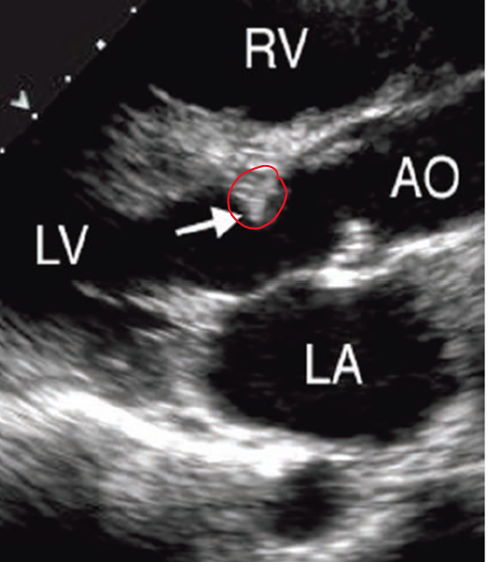
what does a bicuspid valve look like in PSAX?
in systole only 2 leaflets “open”
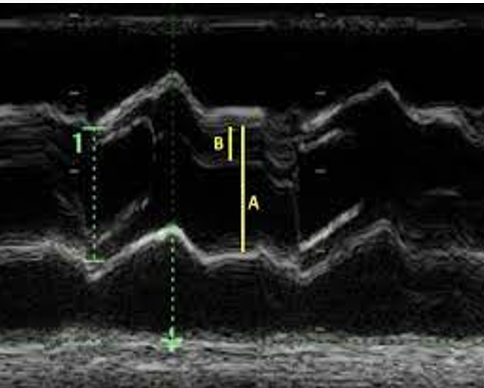
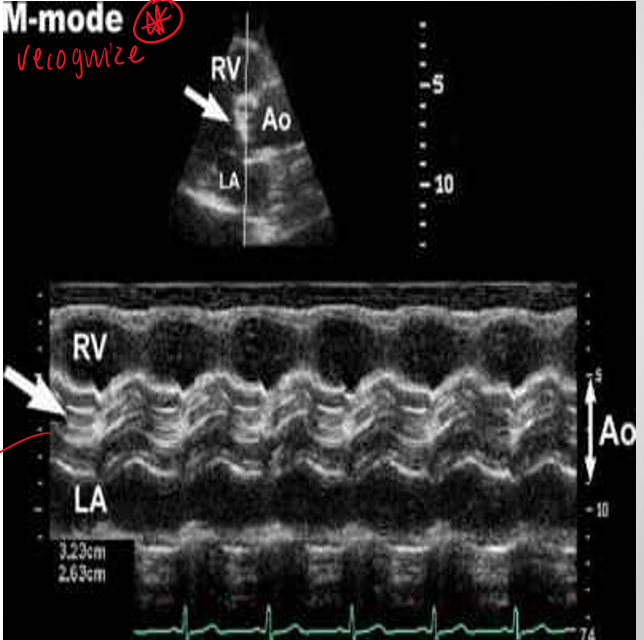
what does bicuspid ao valve appear like on m mode? **
eccentric line closure
bicuspid AO valve is associated with
dilatation of aortic sinuses and ascending aorta
coarctation of aorta
aneurysm
aortic dissection

what is the most comon bicuspid AV valve
larger anterior leaflet with opening along anterolateral posterior closure line
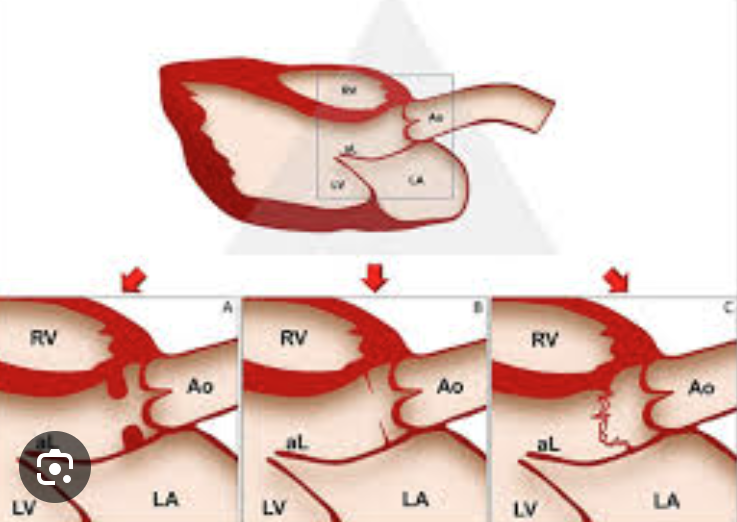
what does rheumatic aortic stenosis typically present with
increased echogenicity along leaflet edges
commisural fusion
systolic doming of aortic leaflets
rheumatic disease is more likely when ao disease occurs
concurrently with typical rheumatic mitral changes
when does rheumatic heart disease occur?
typically starts in childhood acutely and is followed by lifelong progressive valvular damage
bicuspid ao valve is what type of stenosis?
congenital
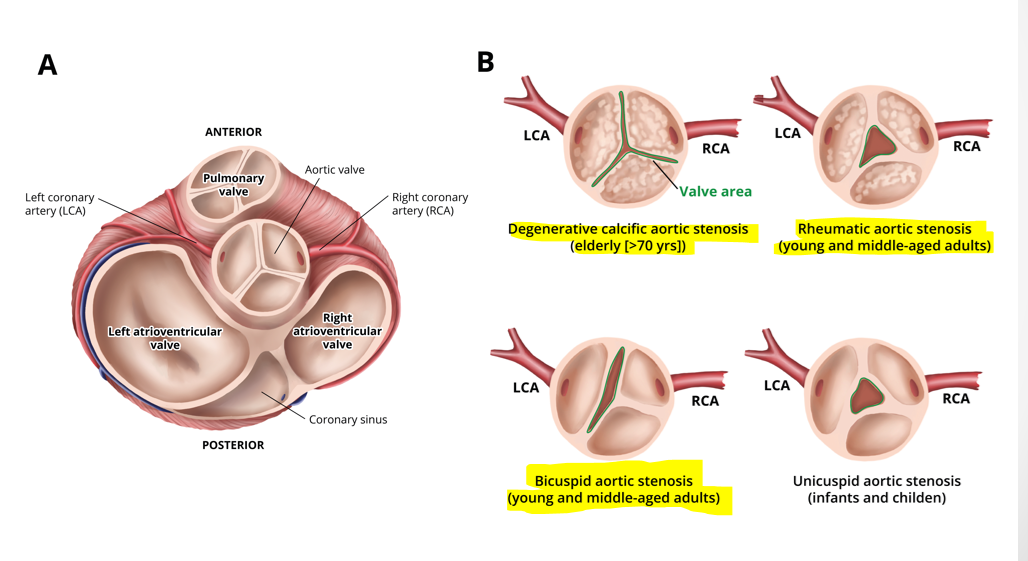
what are differential diagnosis for aortic stenosis? *
fixed subvalvular obstruction (subaortic membrane or muscular subaortic stenosis)
dynamic subaortic obstruction (hypertrophic cardiomyopathy)
supravalvular stenosis
what causes ao stenosis?
degenerative calcific aortic stenosis (elderly >70)
bicuspid aortic stenosis (young/middle aged)
rheumatic aortic stenosis (young/middle aged)
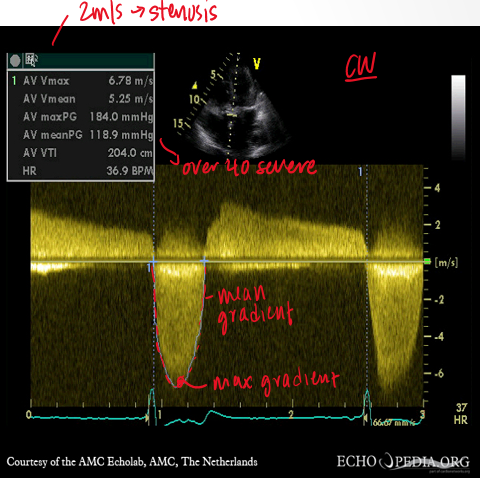
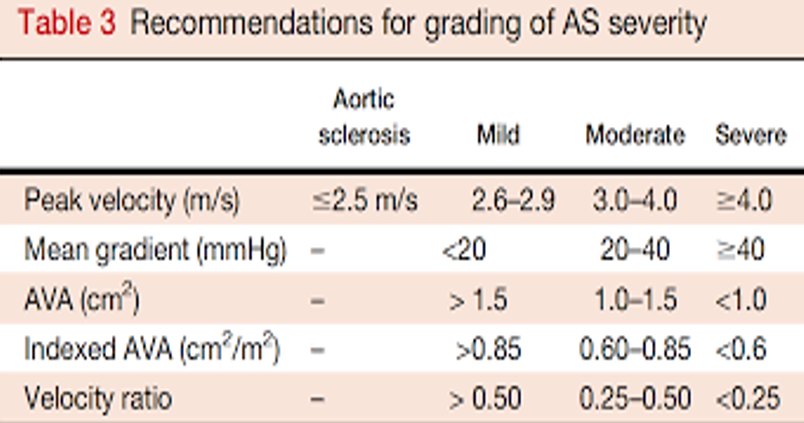
what are the main measurements to quantify severity of ao stenosis?
max ao jet velocity
mean transao pressure gradient
continuity equation valve area
what doppler is used to measure ao stenosis?
CW bc of high velocities (3-6m/s)
how is mean transo pressure gradient calculated?
by tracing the velocity curve and avering instantaneous gradients over systolic ejection period
how is the continuity equation measured for ao stenosis?
LVOT
LVOT VTI
AO jet VTI
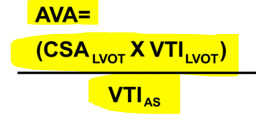
why is LVOT measurement important in continuity equation?
to calc CSA(LVOT) you need to square LVOT so small differences in diameter measurements can make significant differences in area calculations
why is pedoff probe used in ao stenosis? what views?
smaller footprint and better sensitivity for doppler
apical 5CH
suprasternal
right parasternal
what are potential pitfalls in measuring ao stenosis?
poor doppler beam alignment
inaccurate LVOT dimension
beat to beat variability (AF,PVCs)
grading for AS severity
what are additional measurements used for ao stenosis?
planimetry
ao cusp separation
what is planimetry in ao stenosis?
tracing ao valve border to get an area

what planimetry measurement should raise concern for ao stenosis?
<2cm²
what cusp separation measurement should raise suspicious for ao stenosis?
</= 1.5cm
why is velocity ratio used in ao stenosis? (dont focus on)
to reduce error from LVOT diameter by removing CSA from continuity equation (Vlvot / Vav)
smaller velocity ratio indicates
stenosis
(closer to 1 → absence of valve stenosis)
what will you see with low flow aortic stenosis? (dont focus on)
ao velocity less than 4 m/s
valve area less than 1cm
presence of LV dysfunction less than 50% (reduced EF)
how is low flow ao stenosis evaluated? (dont focus on)
degree of valve calcification
dobutamine stress echo
what is a subaortic stenosis?
fixed stenosis and considered NON VALVULAR (valve could be completely normal)
hockey stick valve appearance is specific to**
mitral valve
what is used to evaluate severity of mitral stenosis?
3d/2d planimetry
mean gradient
pressure half time
rheumatic disease almost always affects - and nearly always the cause of -
mitral valve
mitral stenosis
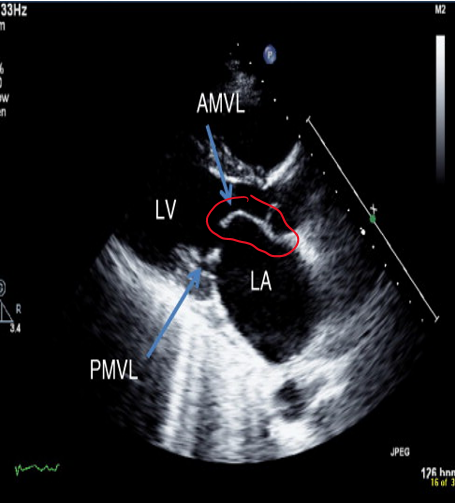
mitral stenosis is characterized by
commisural fusion → bowing or doming of leaflets in diastole → hockey stick appearance of AMVL
what do you need to evaluate as a result of mitral vavle obstruction?
LA size
LA thrombus
estimate pulmonary pressures
RV size and systolic function
how does mitral annular calcification affect stenosis?
calcific stenosis rare in mitral valve
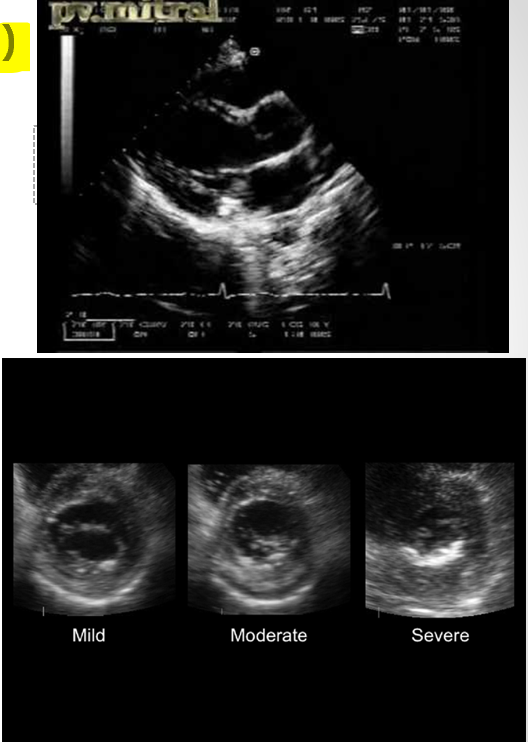
what does this represent?
planimetry of MV in diastole
in what window are pressure gradients measured?
apical window
how is pressure gradient measured in mitral valve stenosis?**
CW/PW of mitral inflow through mitral leaflets and then trace
how does the analysis package calcualte pressure gradients?
averages the instantaneous gradients over the diastolic filling period suing bernoulli equation
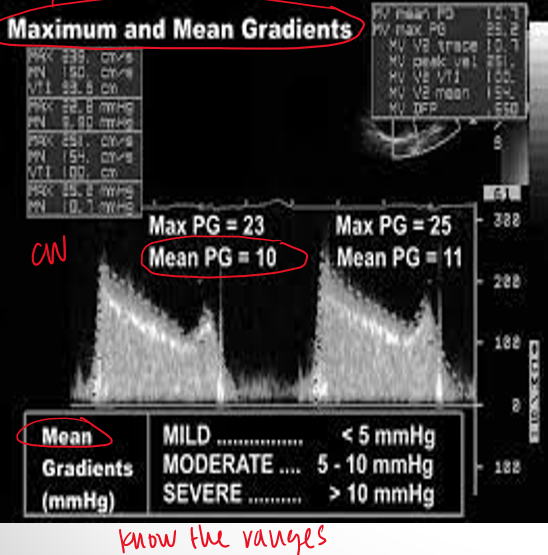
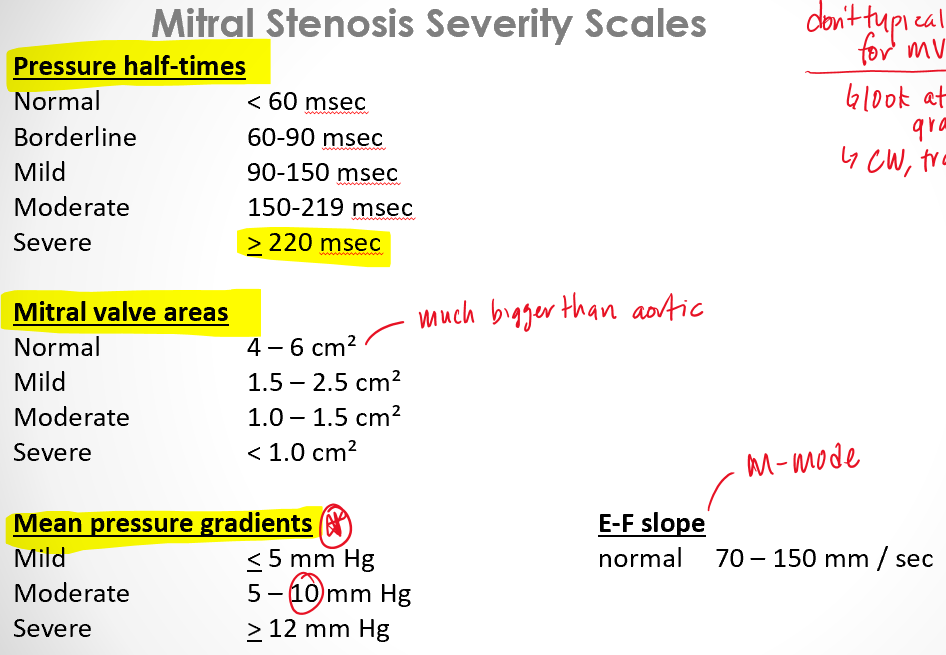
what is the range for mild, moderate, and severe stenosis with regarding mean gradients of mitral valve?**
mild : <5mmHg
moderate : 5-10mmHg
severe : >10mmHg
what is pressure half time? and how is it measured?**
time it takes for pressure to go down by half
trace waveform
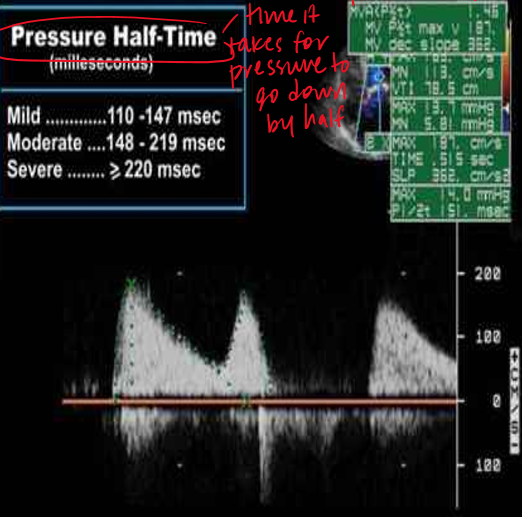
what is considered severe pressure half time for mitral stenosis? mild?
severe : >220
mild : 100
what are common reasons for an increase in pressure gradients across mitral valve?
DOE (dyspnea on exertion)
conditions that increase cardiac output
tachycardia (shortens diastole → interferes with LA emptying)
what is the pressure half time formula?
MVA = 220/PHT
how is PASP measured?
TR jet + RAP estimation
what is normal IVC measurement
2.1
how do we calculate RAP?
normal IVC size and collapses 50%+ = 3
dilated IVC size and does not collapse 50%+ = 15
everything else = 8
what is parachute mitral valve
cause of stenosis
both valves attached to the same pap muscle
what is a secondary measurement for evaluate mitral stenosis?
MVA continuity equation : CSA (mv) = [CSA(lvot) x VTI(lvot)] / VTI(mv)
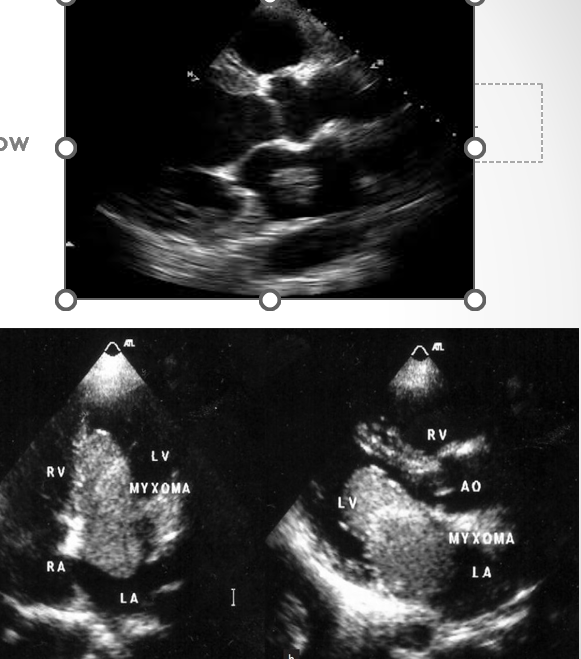
what is a myxoma?
non rheumatic form of mitral stenosis where tumor prolapses into mitral valve funnel in diastole and produces inflow obstruction
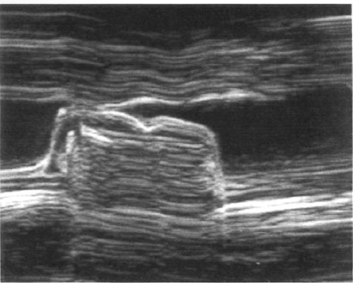
what is characteristic finding in mitral stenosis m mode?
decreased E/F slope
mitral annular calcification (MAC) is most commonly observed in which leaflet?
posterior leaflet
what is very commonly seen in MAC?
calcium deposits
large mitral calcifications can produce
moderate to severe mitral regurg (rarely stenosis)
how does calcification compare in MAC vs rheumatic mitral stenosis?
MAC : calcification at the basal portion of leaflets
rheumatic mitral stenosis : tips/free edges are thickest portion of the leaflets
severe MV pressure half time
>/= to 220 msec
normal MV pressure half time
<60 msec
what is normal mitral valve area?
4-6cm²
what is considered severe MV area?
<1cm²
mitral stenosis severity scales
tricuspid valve stenosis is usually due to
rhuematic tricuspid valve involvement in patients with mitral stenossi
pulmonic stenosis is usually caused by
congenital heart disease
review qs
what is the most common cause of ao stenosis?
age related calcification
review qs
what is the most common cause of congenital ao stenosis?
bicuspid ao valve
review qs
what is bicuspid ao valve associated with
dilatation of ao
coarctation
aneurysm
ao dissection
review q
how do we assess ao stenosis?
max velocity
mean pressure gradient
continuity equation
review qs
what is the most common cause of mitral stenosis? other causes?
rheumatic fever
age related, tumor
review qs
what valve does rheumatic fever affect first?
mv → ao → tv
review qs
what are the two ways to assess mitral stenosis and MVA? which is most accurate?
mean pressure gradient (most accurate)
pressure half time (PHT )
planimetry