Rabies in Equids + Other Neuro Diseases
1/34
Earn XP
Description and Tags
Module 23, Week 1
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
35 Terms
What is myeloencephaitis and encephalitis
Encephalitis is inflammation only of the brain, while myeloencephalitis (or more commonly encephalomyelitis) means inflammation of both the brain (encephalo-) and spinal cord
List some of the viral causes of myeloencephalitis or encephalitis
EHV1 (MOST LIKELY IN THE UK)
Rabies
Arboviruses :
Flaviviruses (WNV, JE)
Togaviruses (alphaviruses); WEE, EEE, VEE
Borna virus
Hendra virus
Arboviruses (most commonly WNV and WEE/EEE/VEE)
How do most of them spread? Are they typically zoonotic?
most spread between mosquitos and birds, with horses (and humans) typically “dead end” hosts
most are SERIOUS zoonoses
Viral Encephalitides
Typical clinical signs?
Many can be subclinical
Mentation: hyper-excitability or lethargy (profound), comatose
Behavior : head pressing, self mutilation, compulsive walking
Gait derangements : ataxia, paresis, paralysis, muscle fasiculations (twitching) in WNV
Other: circling, blindness, deafness, recumbency, fever
Equine Rabies
What are 3 ways of spread (epidemiology)
skunks, raccoons, and red fox most common in USA
dogs, cats, and other horses may also spread to horse via infected saliva in bite wounds
small carnivores (opossum, or pole cat) and bats may be more important cause of sprfead to equids in other counties. mules/donkeys naturally inquisitive = get bit
Equine Rabies
What kind of virus is it?
Neurotropic rhabdovirus (Lyssavirus)
Equine Rabies
Describe the pathogenesis
Virus multiplies in myocytes at bite site and infects peripheral nerces via nerve endings/NMJs
Progresses along PN via axoplasmic flow to spinal and dorsal root ganglia
rapid multiplication in CNS (brain and spinal cord, sympathetic trunk): spreads in CSF and subsequent spread to blood
Equine Rabies
Does rabies initially spread within the blood or lymph node?
No! theres no initial spread within the blood or lymph node. it multiplies in neurones, perikaryons of neurons and accumulates in nucleocapsid (negri body formation). there is then an increase in cellularity in CSF ocne reaches (now detectable by PCR). THEN it spreads to salivary glands, secretions, bloood
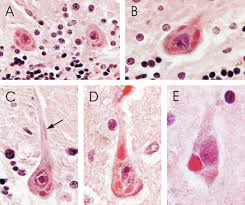
What are these? Why are they important
Negri bodies
They are pathognomic (specifically diagnostic) for rabies virus infections
Equine Rabies
What is the incubation period?
Depends on site of bite, viral strain, and inoculum dose, ranging from 9 days to 1 year
There is also variable retention time of virus in myocytes, direct entry of virus to neural tissue allows for short IP
Equine Rabies
Clinical signs? Early vs Late
Very variable in horse!!
Early signs: hyperesthesia (physical sensitivity, especially of skin), ataxia, behavior change, anorexia, paresis, colic
Late signs: cerebral signs, with rapid progression and deterioration usual over 48 hr
furious form = aggression, self mutilation, photophobia, hyperesthesia
Equine Rabies
Summary to describe the clinical progression
Range of Clinical signs:
Change in behavior, dysphagia, ataxia
Apparent colic pain or limb pain
Later clinical progression:
Usually rapid increase in ataxia/paresis
Self mutilation and aggression common
Further clinical progression
Progress progression to recompense, often with multiple' ‘bucking’ attempts to stand
Aggression may remain present
Equine Rabies
How do we diagnose?
Often on clinical signs, especially self mutilation
Recumbent paralytic form animals may continue to eat, drink with slower progression
Usual progression to death within 48 hours of initial onset
Lab diagnosis
Immuno fluorescent antibody test on fresh brain tissue very quick
Make sure you use the correct PPE
Histopathology would reveal non-suppurative encephalomyelitis
Negri bodies pathognomic for rabies
Equine Rabies
Treatment
No progressive treatment, euthanize with appropriate PPE
Equine Rabies
How should we prevent?
Vaccinate in high risk areas
Inactivated vaccine given IM annually and high risk areas
Stray, dog control, minimize exposure to bats
Do not vaccinate horses that have had immediate contact with suspect case!
EHV-1
What is it? What can it cause?
EHV-1 (Equine Herpes Virus) is a ubiquitous disease (80% of ALL horses latently infected): causes mild respiratory disease in young horses, abortion storms, chorioretinopathy and myeloencephalopathy (EHM = Equine Herpes Myeloencephalopathy)
EHV-1 Myeloencephalopathy (EHM)
What is EHM?
Rarest manifestation of disease: may be pyrexic, with respiratory signs, and herd mates or individuals with neuro signs
EHV-1 Myeloencephalopathy (EHM)
Clinical signs
Symmetric ataxia (typically affect Hind limbs first)
Urinary/fecal retention, recumbency
CN signs common, especially V, VII, VIII, XII
Multifocal Neuro signs with variable forebrain disease (dullness, low head carriage, inability to rise, central vision loss)
May be preceded by URT signs, pyrexia, inappetence, lethargy
** typically see symmetric ataxia, reduced tail tone, and struggle to urinate/defecate FIRST
EHV-1 Myeloencephalopathy (EHM)
How to diagnose
Hx, CS, evidence in herd
Recent travel, competition, or mixing?
Multicentric lesions predominantly affecting cauda equina (bundle of nerves at very bottom of spinal cord), but cranial nerve deficits can also be present
CSF: xanthochromia, PCR
Serology
Viral Isolation: PCR,, culture (nasopharyngeal swab or blood)
necropsy
EHV-1 Myeloencephalopathy (EHM)
Treatment options
Anti inflammatories: NSAIDS, corticosteroids (controversial, but useful for 2-3 days)
Supportive tx: position/slings, antimicrobials, urinary cath/rectal evacuation
Possibly anti-virals
Quarantine, hygiene measures
EHV-1 Myeloencephalopathy (EHM)
Prognosis and prevention
Related to disease, severity, and response to treatment
Recumbent horses = poor/grave
Prevention and control = difficult
Vaccination = controversial, does not prevent, but will increase herd immunity and decrease shedding period
Herd management = keep young stock and older broodmares in separate areas, consider vaccination of all stock
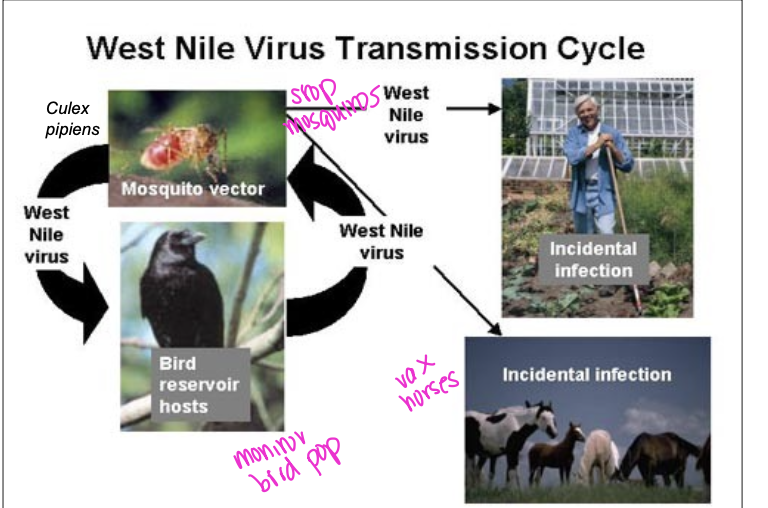
West Nile Virus (WNV)
What type of virus is it? What are the hosts? zoonotic?
Flavivirus
Hosts: birds, humans, horses, other mammals
humans/horses = dead end hosts
ZOONOTIC
West Nile Virus (WNV)
What 2 things can amplify the virus and are involved in the virus cycle?
birds and mosquitos
West Nile Virus (WNV)
What is the Transmission cycle (pic)
West Nile Virus (WNV)
Clinical signs
ataxia, paresis
Muscle fasciculations - twitching
Hyperesthesia
Behavioral changes
Cranial nerve deficits: CNVII, XII, IX
Recumbency
West Nile Virus (WNV)
Diagnosis
Clinical signs
Laboratory techniques:
IgM ELISA after two weeks
IgG species- specific ELISA
Nested RT-PCR on EDTA blood or brain tissue
brain immunohistopchemistry
West Nile Virus (WNV)
How can we prevent?
Vector control!!! - reduce mosquitos
Vaccination - most US horses are vaxxed
Alpha Viruses
What are they? Where are they endemic to? Zoonotic?
Eastern/Western/Venezuelan encephalitis viruses
endemic to the americas
zoonotic!!
high fatality rate in horses
Alpha Viruses (WEE/EEE/VEE)
Main amplifying host? Vector? Dead end hosts?
amplifying = birds
vectors = mosquitos
dead end hosts = horses and humans (with the exception of VEE, cause horses develop marked viremia bc the horse is the primary reservoir and perpetuates infection with horse/mosquito cycle!)
Alpha Viruses (WEE/EEE/VEE)
Clinical signs
Wide range: asymptomatic or severe CNS signs
initial viremia = fever, lethargy stiffness
behavioral changes
blindness, CN deficits
ataxia, paresis
recumbency, seizures, coma
Death: EEE > VEE > WEE
Alpha Viruses (WEE/EEE/VEE)
Diagnosis
CS and epidemiology suggestive
virus detection/isolation
serology
main research aim to improve vaccine efficiency so as to require fewer doses to establish effective immune response
NOTIFIABLE DISEASE
Hendra Virus: Australia
Risk factors?
Food trees
Bat birthing season
Breed (Thoroughbreds)
>8yo
Pasture housing
Pregnancy
Hendra Virus: Australia
Clinical signs? Diagnosis?
Pyrexia
severe pneumonia
Frothy nasal discharge
icterus
Recumbency
Death
Dx: CS, virus isolation, serology, PCR, hisptopathology, zoonotic, caution w necropsy
Borna Virus
there is a slide on this but its a lot of random shit and not in the UK or the US
Main ways to prevent infection of these viral diseases
reduce exposure to vectors
vaccination