Anatomy of the Gastrointestinal system
1/146
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
147 Terms
What are the three accessory organs to the GI tract?
Liver
Gall bladder
Pancreas
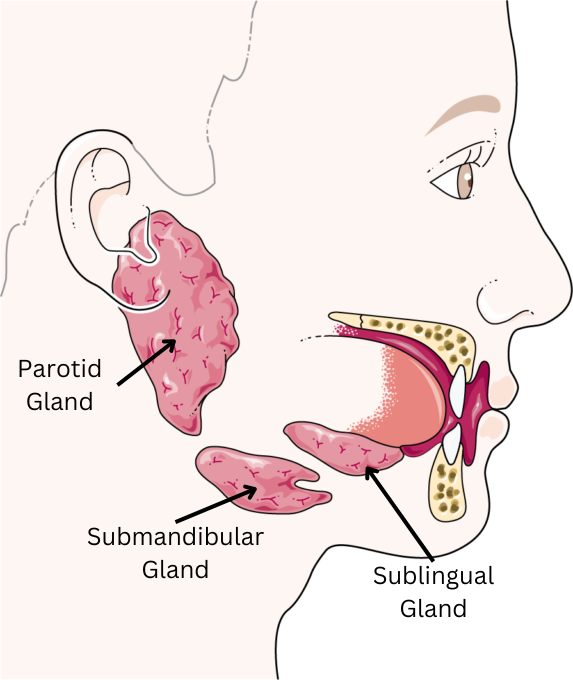
What are the three main salivary glands?
Parotid
Submandibular
Sublingual
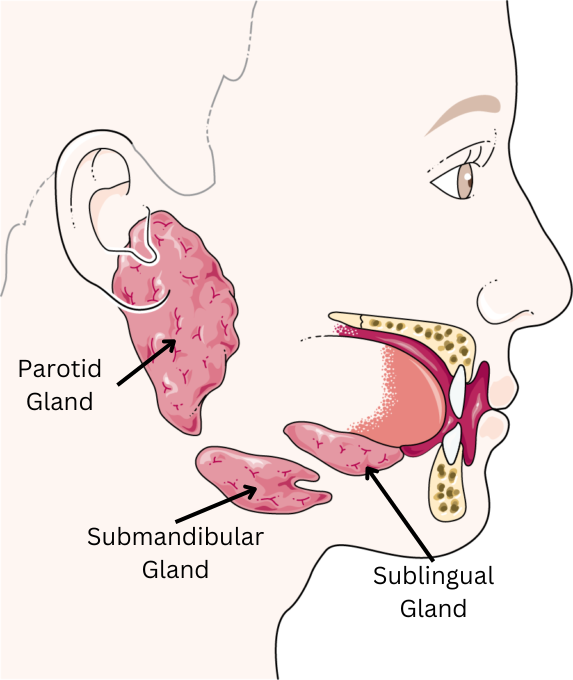
What types of saliva do the Submandibular, Parotid and Sublingual salivary glands secrete?
Submandibular - Both serous and mucus saliva
Parotid - Serous saliva
Sublingual - Mucous saliva
Where in the saliva glands is saliva produced?
The acini
How is saliva initially produced in the saliva glands?
Via active filtration of ions from the blood.
Has a similar composition to extracellular fluid
Where is the composition of saliva modified?
In the ducts of the saliva glands.
Modification makes it appropriate for requirements.
How does parasympathetic stimulation of the saliva glands affect saliva composition/volume?
Parasympathetic simulation produces a large volume of watery saliva.
How does sympathetic stimulation of the saliva glands affect saliva composition/volume?
Sympathetic simulation produces a small volume of mucous saliva.
List some functions of saliva.
Lubrication (due to mucin content)
Digestion (due to presence of α-amylase)
Protection of oral mucosa
Antibacterial (due to antimicrobial thiocyanate)
Speech
Absorption in the mouth
Why is food broken down into smaller pieces by our teeth?
To increase surface area for action of digestive enzymes.
What are the muscles of the tongue and cheeks called?
Buccinator muscles.
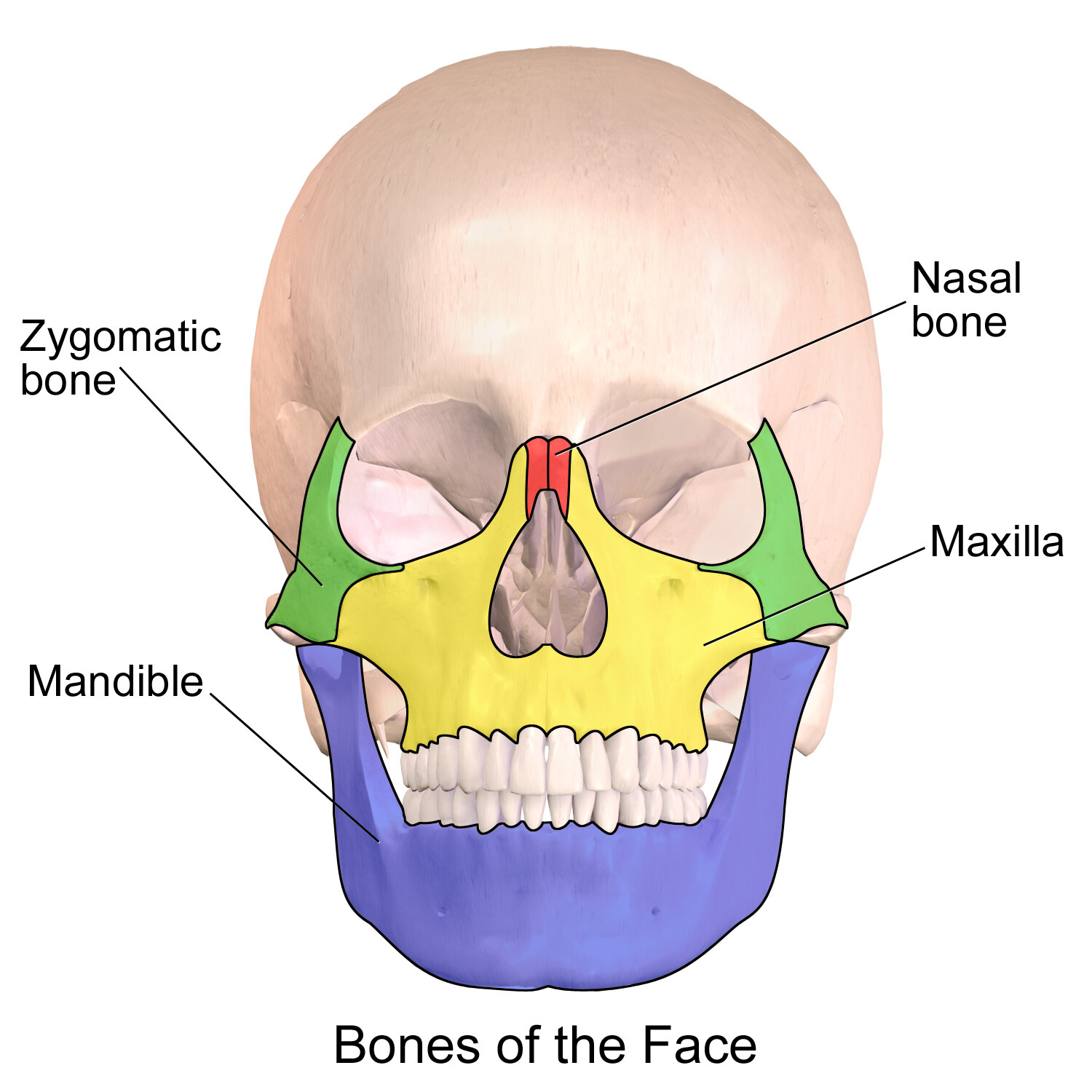
What is the lower jaw bone called?
Mandible
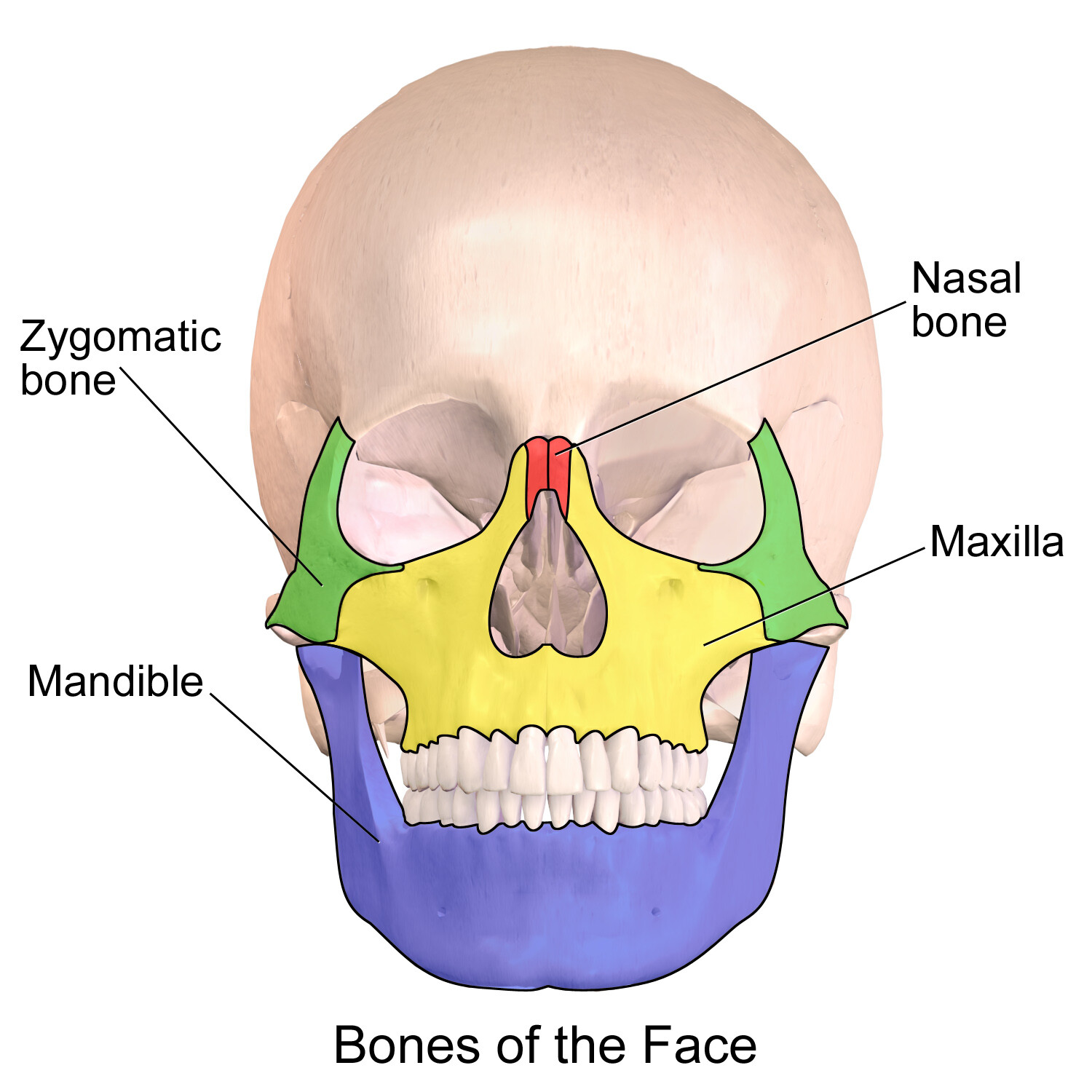
What is the upper jaw bone called?
Maxilla
What is the joint which moves when mastication (chewing) occurs?
The Temporomandibular Joint (TMJ)
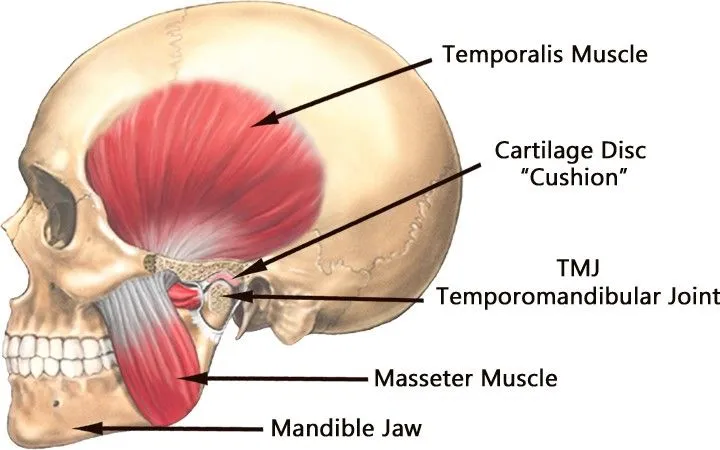
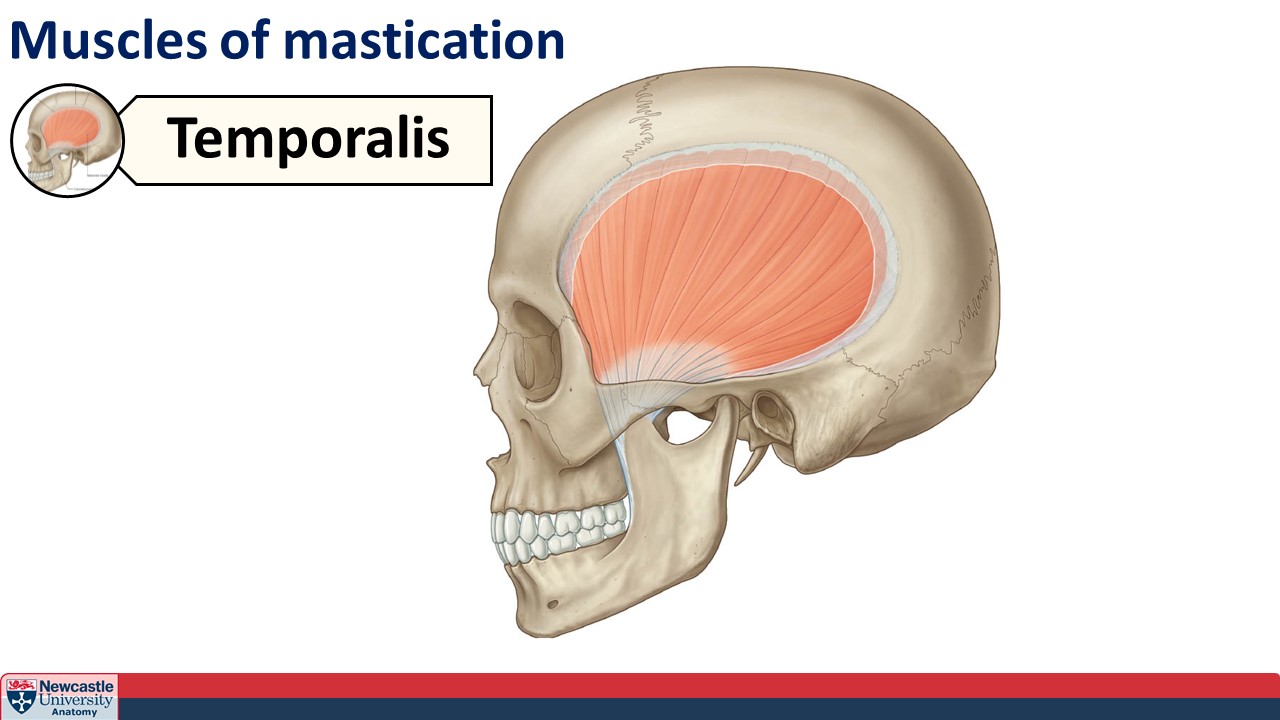
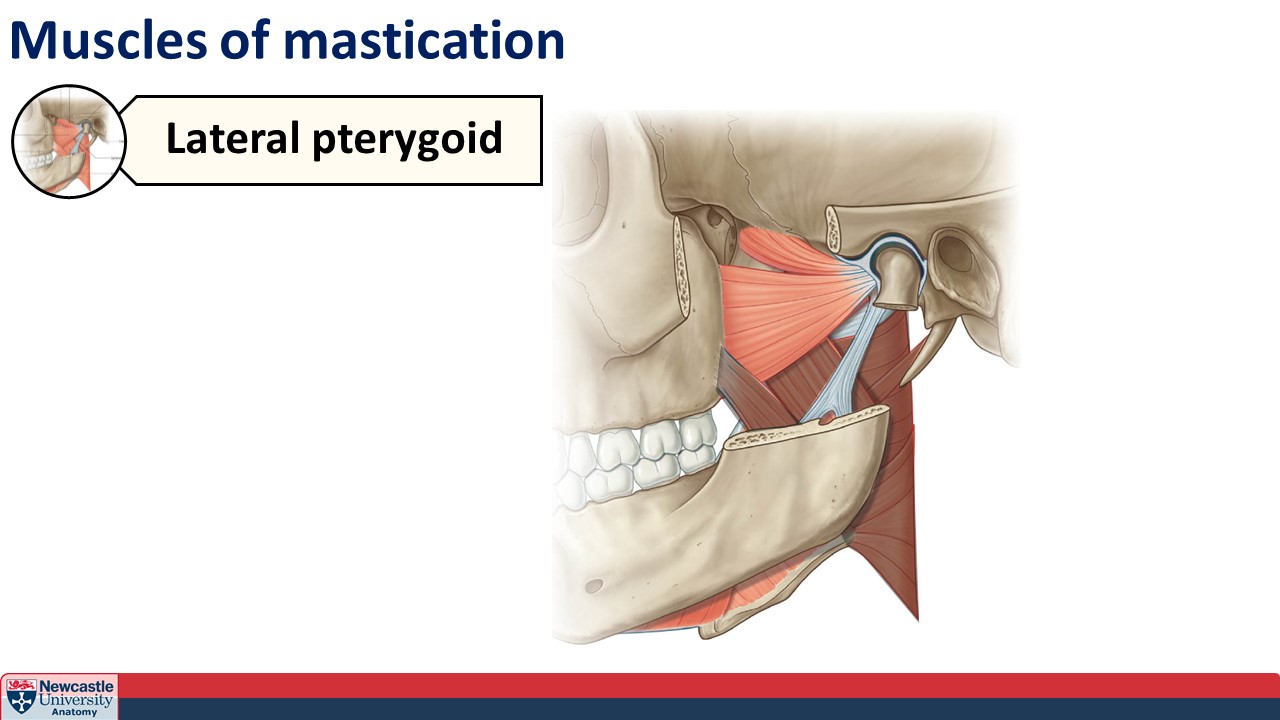
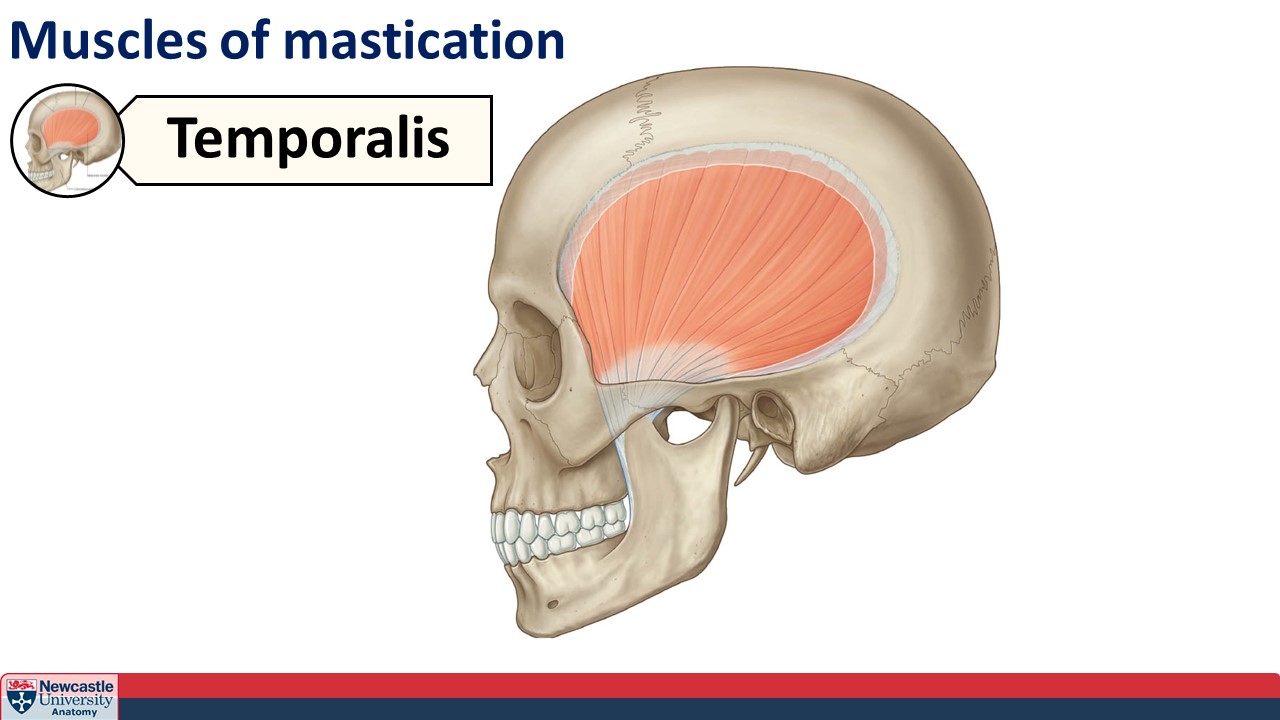
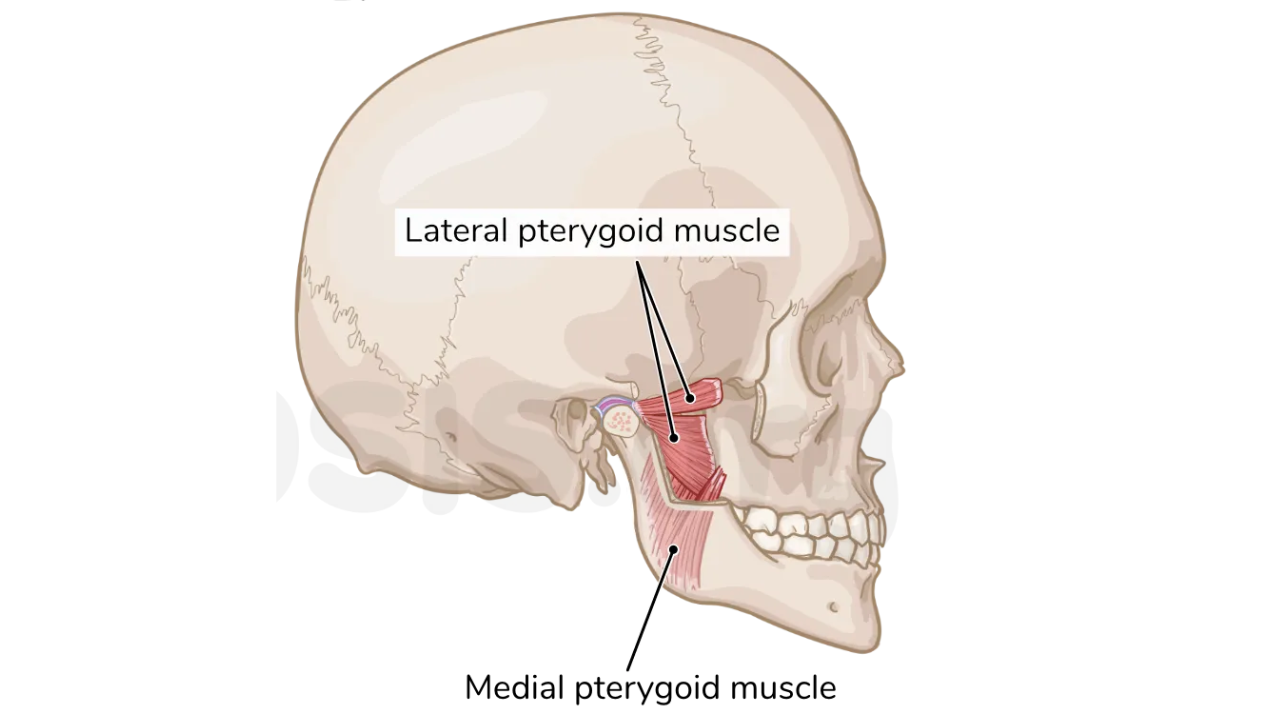
What are the four muscles of mastication called?
Temporalis
Masseter
Lateral pterygoid
Medial pterygoid
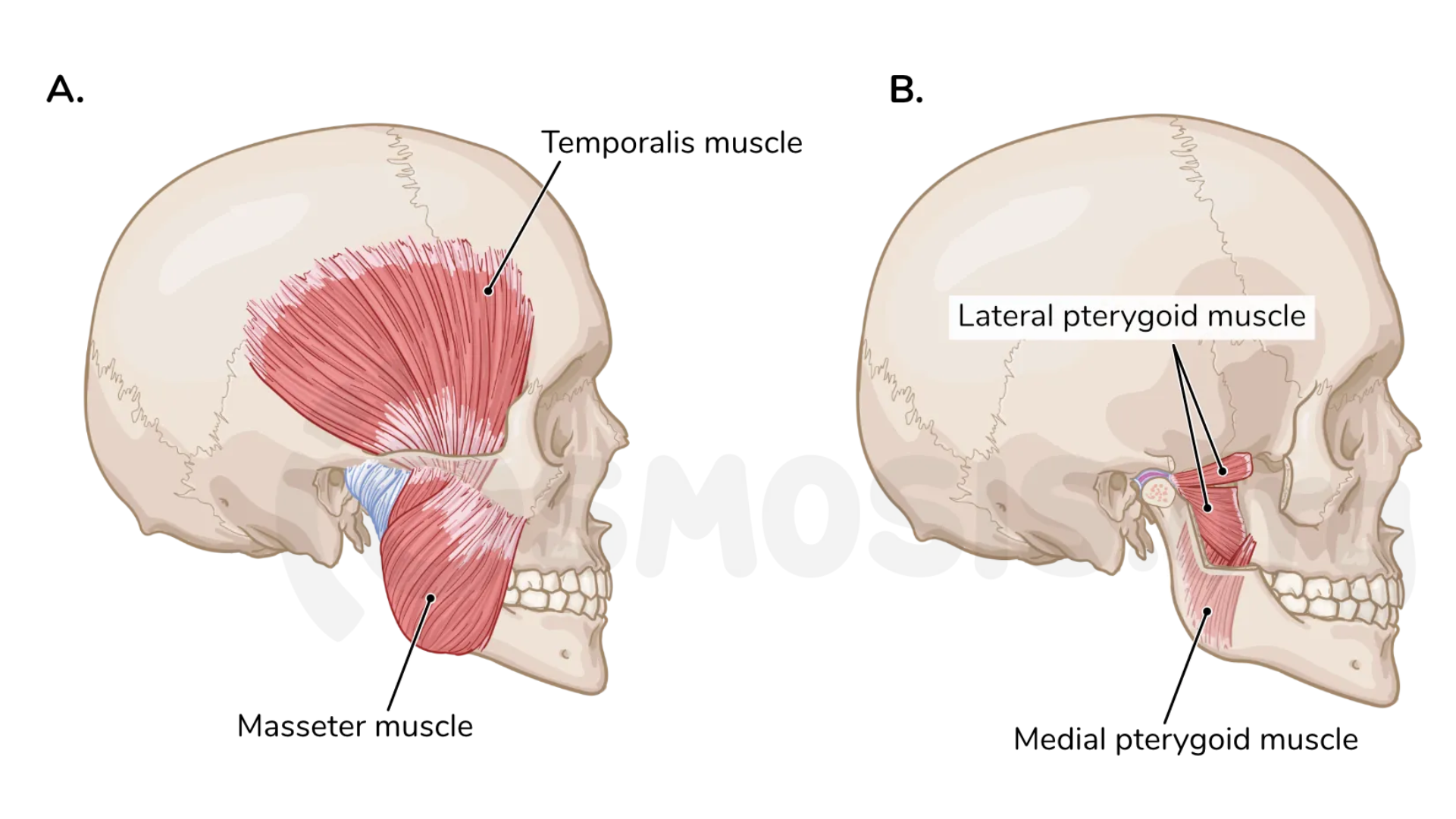
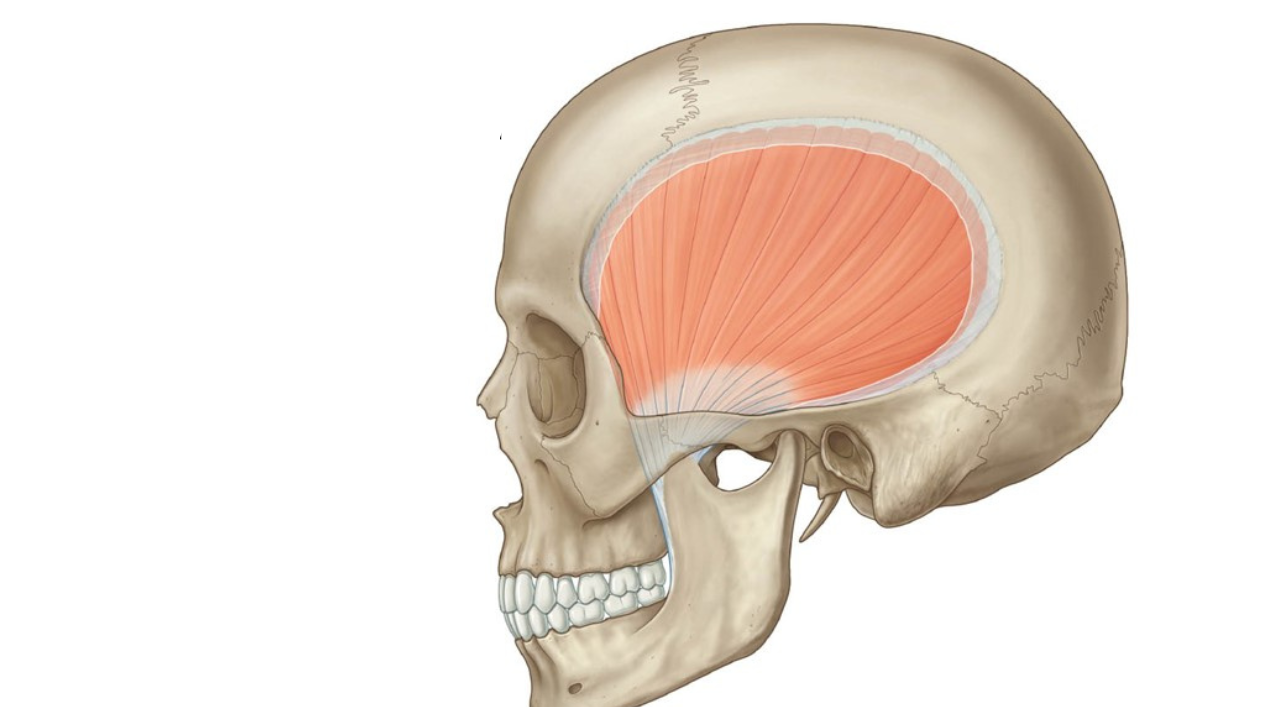
What muscle is this?
Temporalis muscle
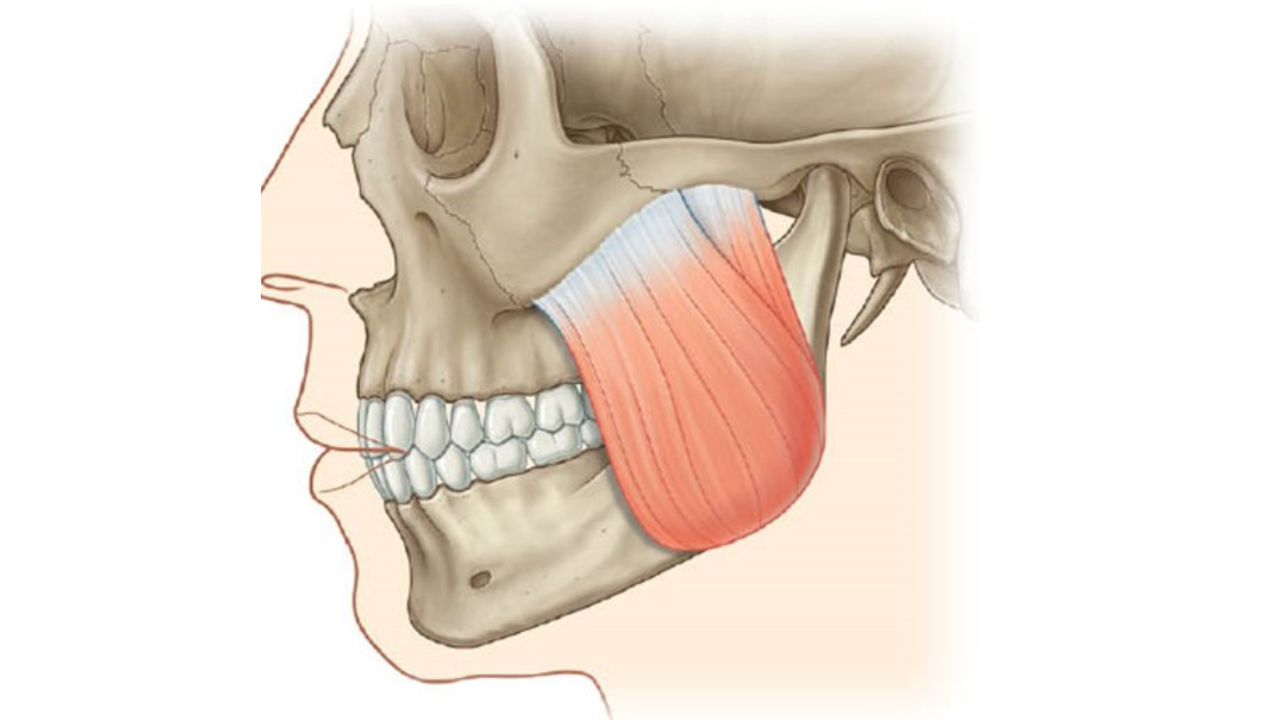
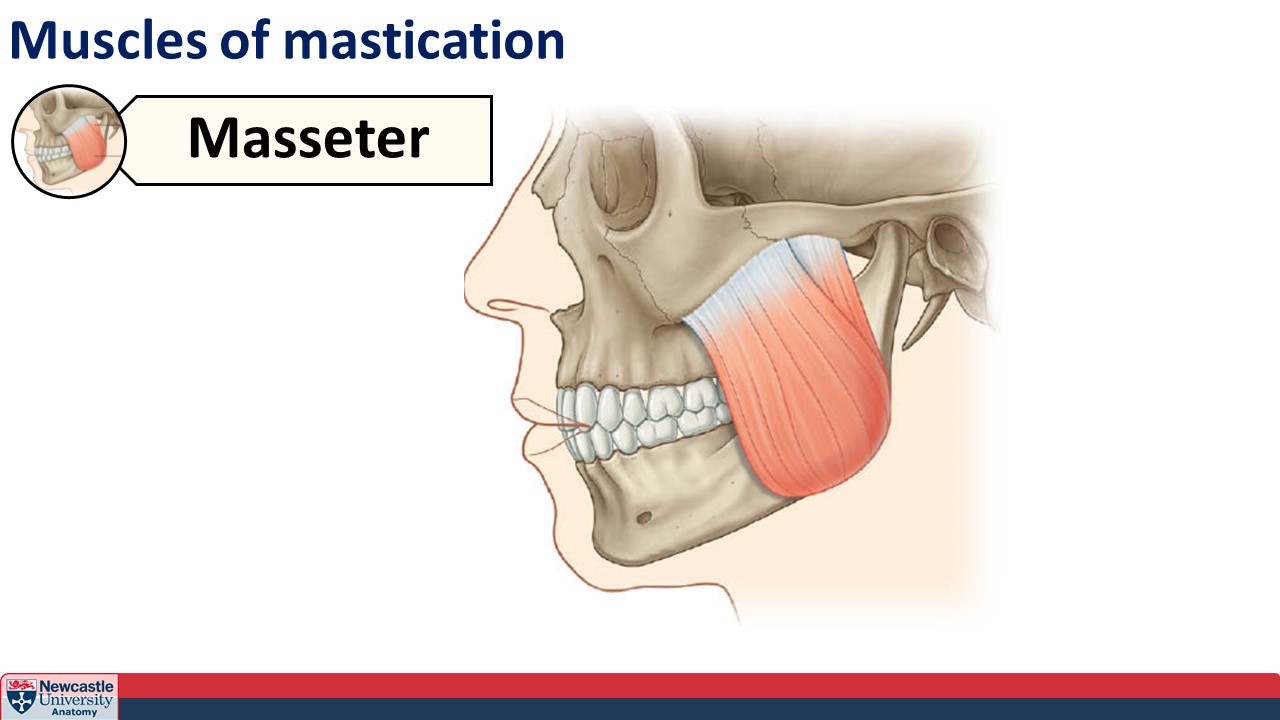
What muscle is this?
Masseter muscle
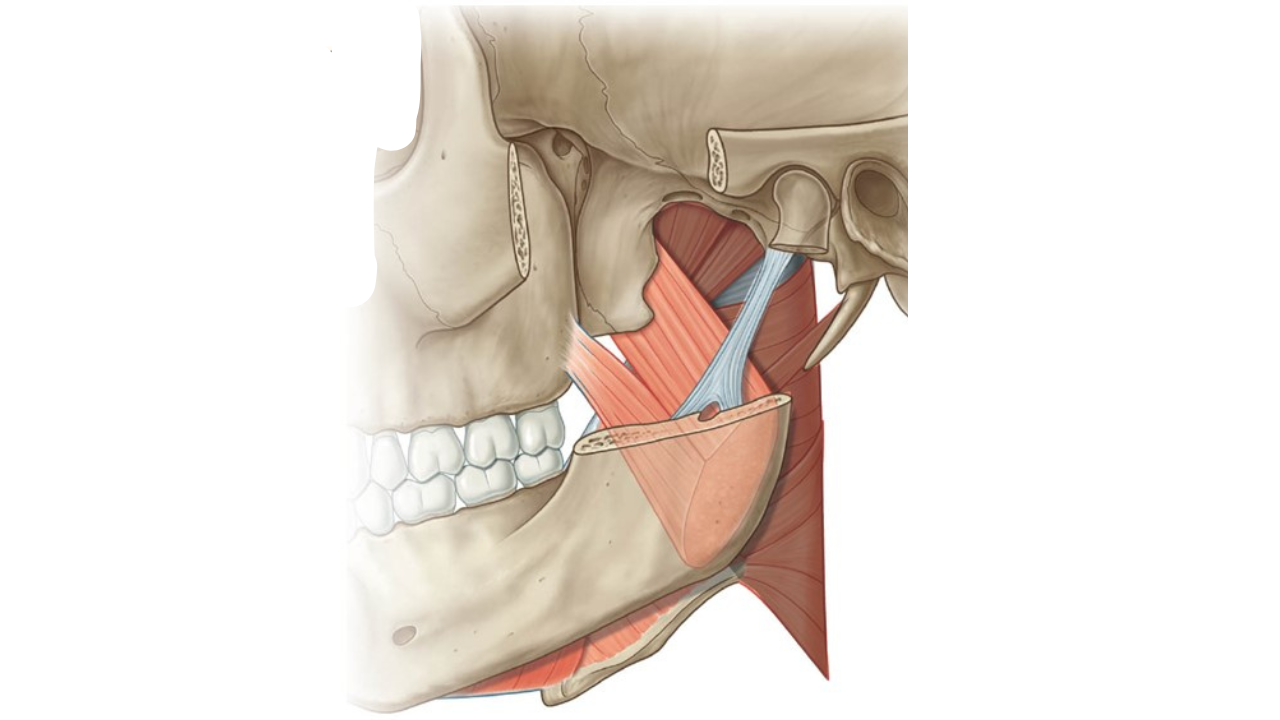
What muscle is this?
Medial pterygoid
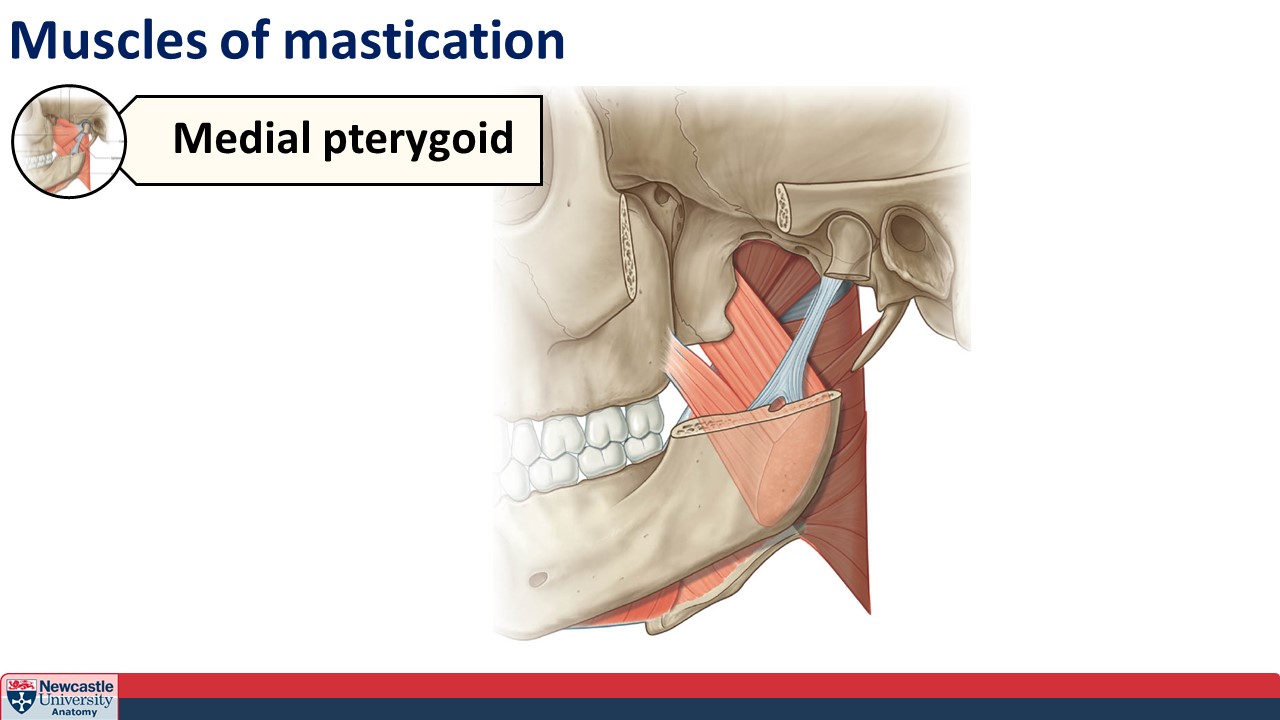
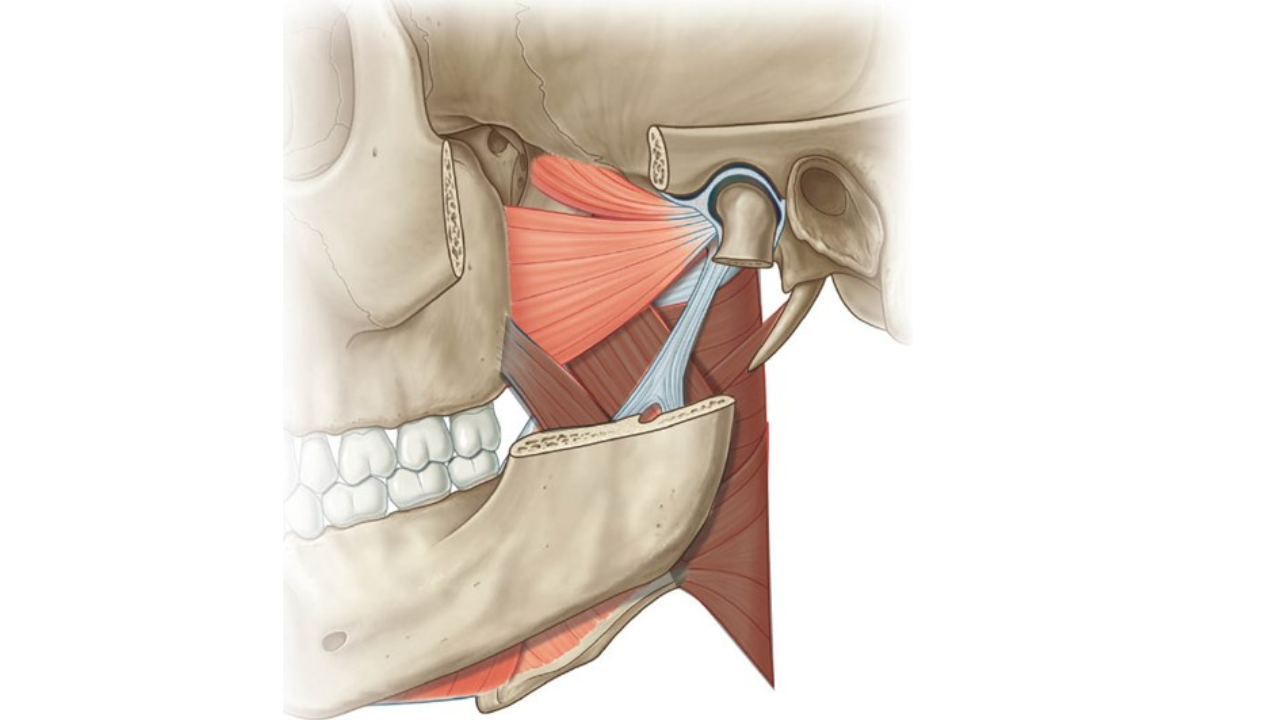
What muscle is this?
Lateral pterygoid
Which of the four muscles of mastication are the major effector?
Temporalis muscle
Which muscles of mastication are responsible for lateral/side-to-side movement?
Medial and lateral pterygoids
What two stages can swallowing be divided into?
Pharyngeal stage and Oesophageal stage.
How is the swallow reflex triggered?
Food is voluntarily swallowed and the tongue pushes the bolus (food) posteriorly
Food contacts the back of the pharynx and the swallow reflex is triggered.
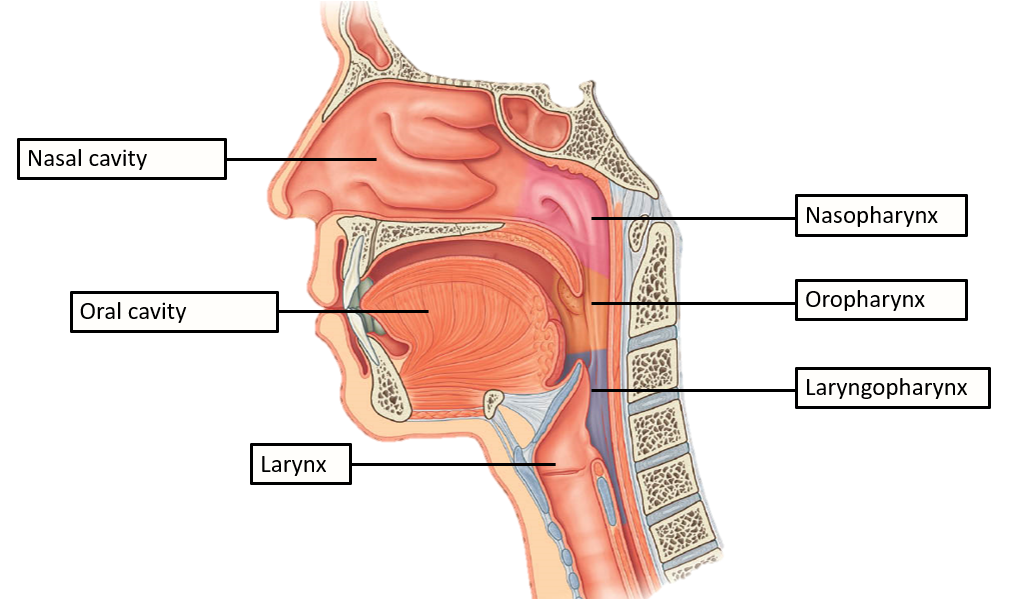
How is food prevented from entering the trachea?
Following the swallow reflex, the larynx is elevated and moves the epiglottis over the trachea
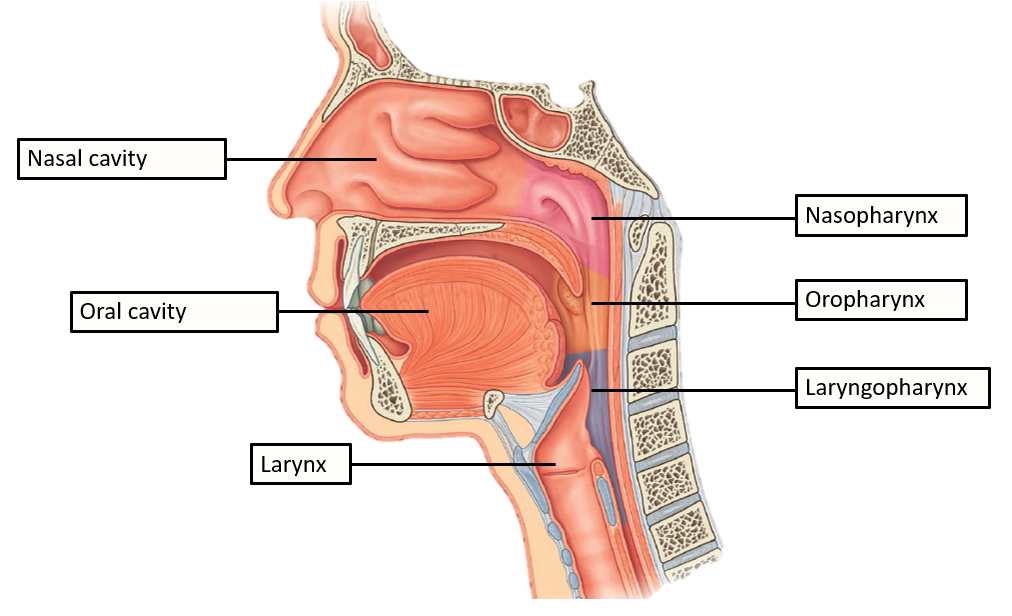
Which muscles move the larynx in order to close off the trachea?
Suprahyoid muscles.
At the junction between the oesophagus and stomach, there is an anatomical sphincter to prevent reflux of stomach contents
True or False.
False.
There is no anatomical sphincter at the junction. Instead there are bands of muscle from the diaphragm (lower oesophageal sphincter) which increase tension produced by the oesophageal wall.
This is also referred to as a physiological/functional sphincter rather than an anatomical sphincter.
What type of epithelium lines the oesophagus?
Stratified squamous epithelium.
What is a hiatus hernia?
The upper part of the stomach squeezes through a gap between the oesophagus and diaphragm (hiatus).
This is usually asymptomatic and only presents when it causes reflux of stomach contents.
Where does the stomach lie?
Just below the diaphragm, to the left of the abdominal cavity.
What does the stomach open into?
Opens into the duodenum (proximal part of small intestine)
What is the name of the orifice where the stomach opens into the duodenum?
Pyloric orifice
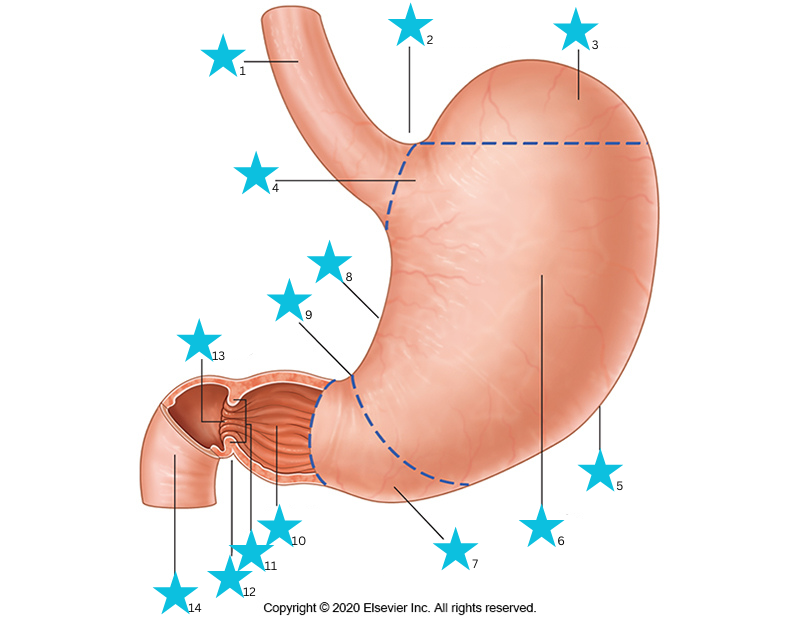
What are the different structures of the stomach shown in the image?
1) Abdominal oesophagus
2) Cardial notch
3) Fundus
4) Cardia
5) Greater curvature
6) Body
7) Pyloric antrum
8.) Lesser curvature
9) Angular incisure
10) Pyloric canal
11) Pyloric sphincter
12) Pyloric constriction
13) Pyloric orifice
14) Duodenum
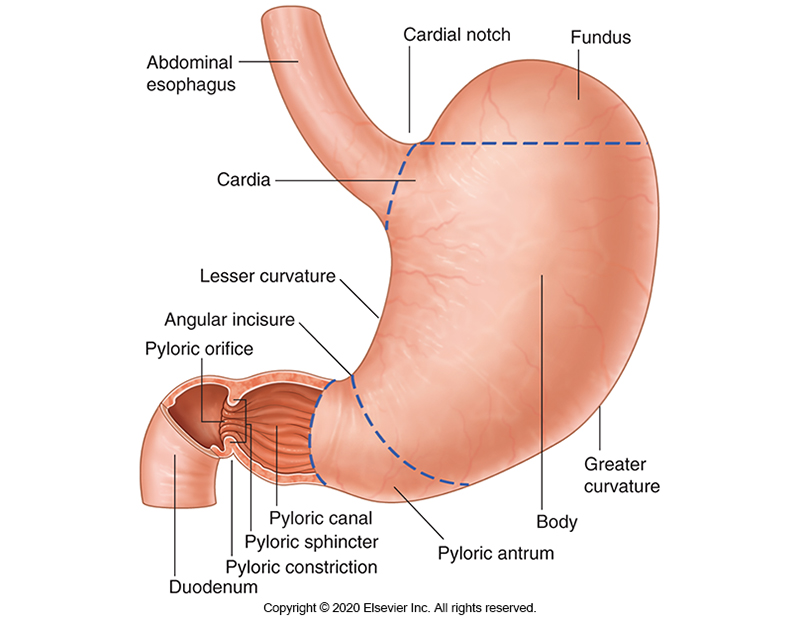
Which parts of the stomach secrete acid?
Fundus and body
What cell type secretes acid in the stomach?
Parietal cells.
What cell type secretes pepsin precursor, pepsinogen?
Peptic cells (Also called Chief cells)
Which part of the stomach secretes endocrine molecules which control gastric secretion and gastric motility?
The antrum
What three molecules are secreted by the antrum in order to control gastric secretions/motility?
Gastrin
Histamine
Somatostatin
What type of epithelium lines the stomach?
Columnar epithelia which contain tight junctions between cells to prevent tissue damage from acid secretions
In addition to circular and longitudinal layers of smooth muscle, the stomach also contains ______ layer of smooth muscle which allows _______ of the stomach.
Oblique (sloping) layer of smooth muscle which allows distension of the stomach.
What are the three parts of the small intestine?
Duodenum
Jejunum
Ileum
The duodenum can be further divided into four parts. What are these parts?
Superior duodenum
Descending duodenum
Horizontal duodenum
Ascending duodenum
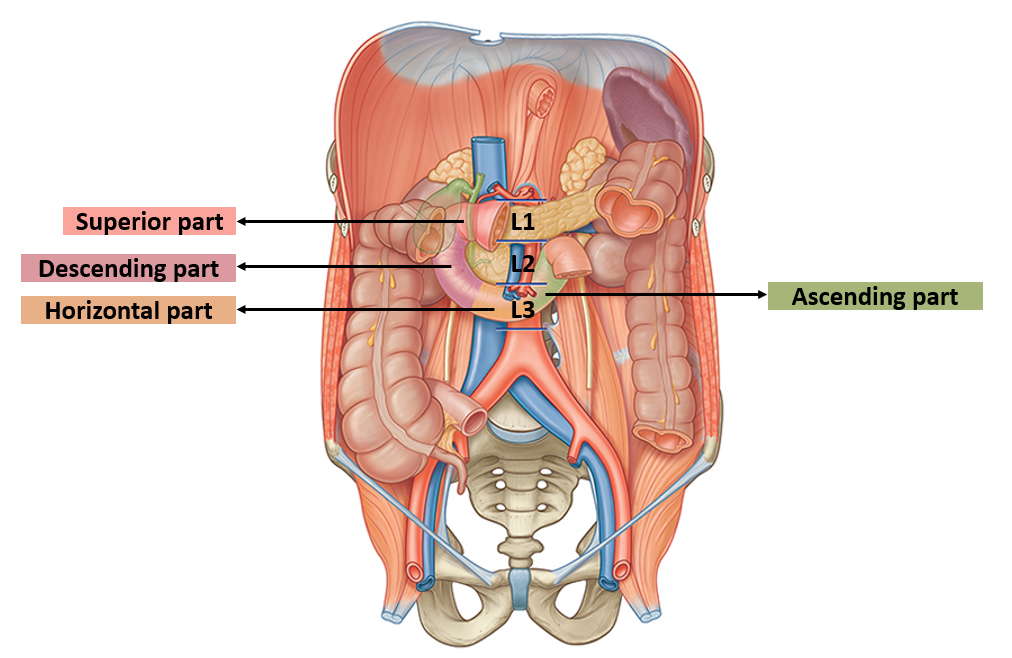
Where does the superior duodenum travel and at what level?
Travels slightly superiorly and posteriorly at the level of L1
Where does the descending duodenum travel and at what level?
Travels inferiorly over part of the kidney at level of L3
Where does the horizontal duodenum travel and at what level?
Travels medially to the left and crosses the aorta at the level of L3
Where does the ascending duodenum travel and at what level?
Travels superiorly on the left of the aorta at the level of L2
It then becomes the jejunum.
Which part of the duodenum receives further digestive secretions?
The descending duodenum.
Receives from the liver/gallbladder and pancreas.
How does the descending duodenum receive digestive secretions from the liver/gallbladder and pancreas?
Liver/gallbladder - Via the common bile duct
Pancreas - Via the main pancreatic duct
What vertebral level does the jejunum begin?
L2 vertebrae
The jejunum becomes the ileum at an anatomically indistinct junction.
True or False?
True.
They ‘join’ at an anatomically, indistinct junction.
How are the jejunum and ileum anchored to the posterior body wall?
They are anchored by the mesentery.
What parts of the small intestine are the main sites of absorption?
Jejunum and Ileum
What is the major function of the large intestine?
Absorption of water and ions (some nutrients absorbed in the proximal colon)
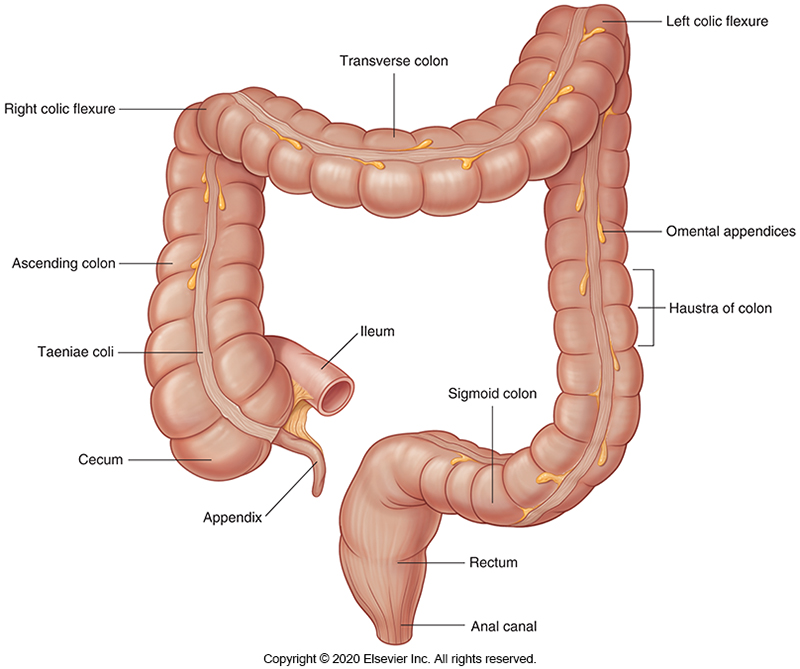
What are the three bands of longitudinal smooth muscle in the large intestine known as?
Taeniae coli.
What parts can the large intestine be divided into?
Caecum
Colon
Ascending colon
Transverse colon
Descending colon
Sigmoid colon
Rectum
Anal canal
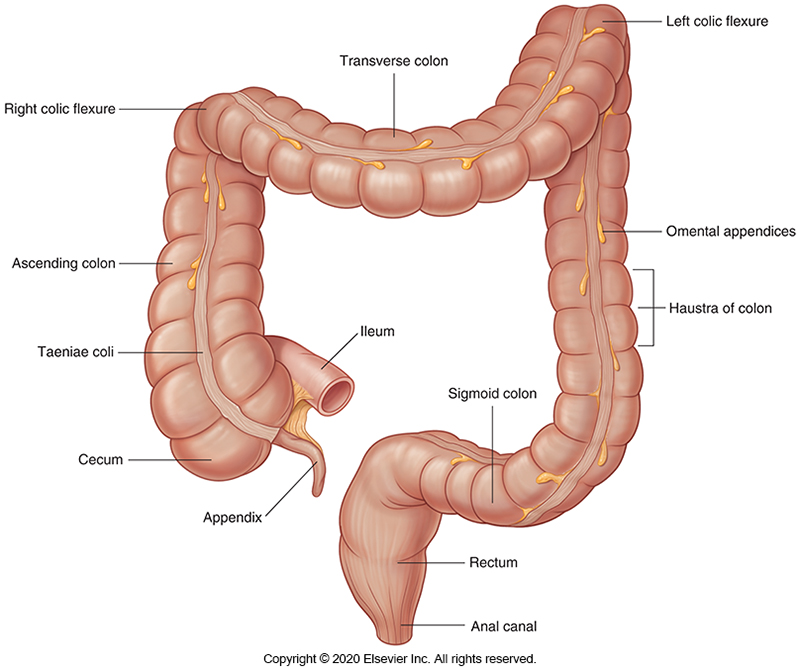
What is the caecum and where does it begin?
First section of the large intestine. Pouch of the large intestine and contains the vermiform appendix.
Begins at the ileocecal junction (connection between Ileum and Caecum)
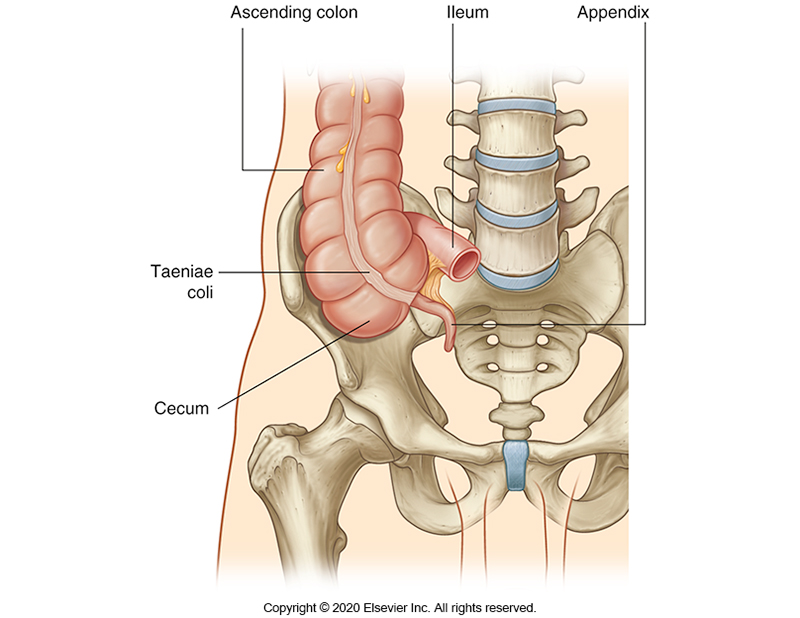
Where does the ascending colon travel?
Superiorly from the right lower to right upper quadrant
Then forms a 90° bend to the left and into the transverse colon.
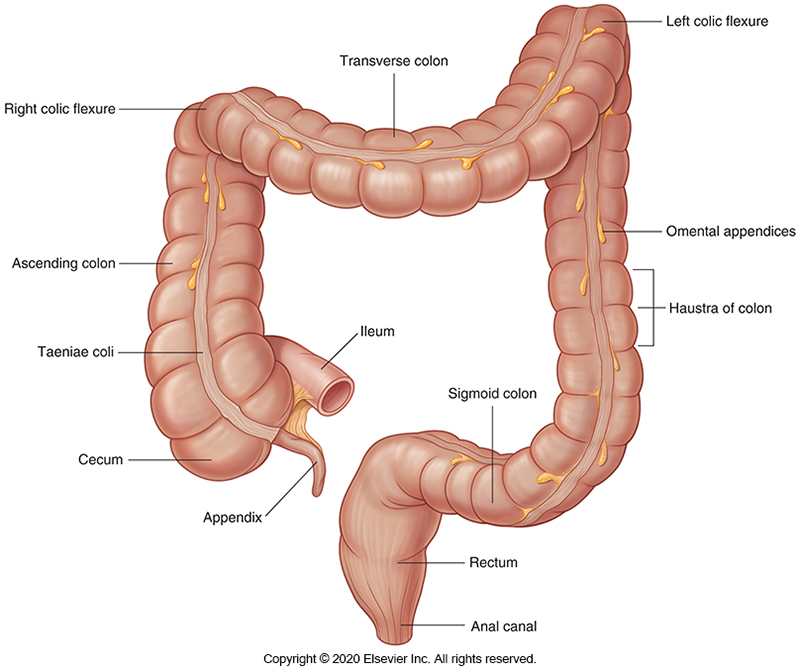
What is the 90° bend between the ascending and transverse colon called?
Right colic flexure.
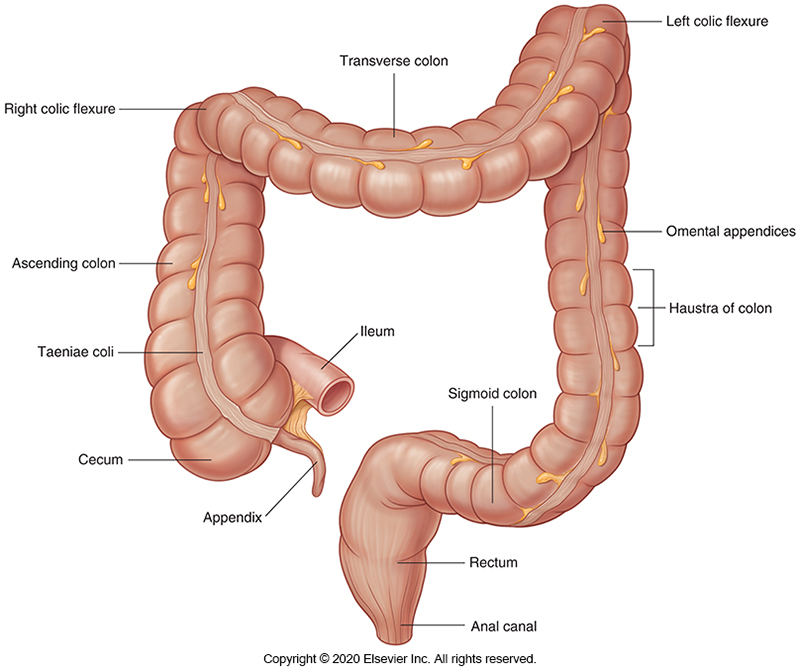
Where does the transverse colon travel?
From right upper to left upper quadrant
Then forms a 90° bend down and into the descending colon.
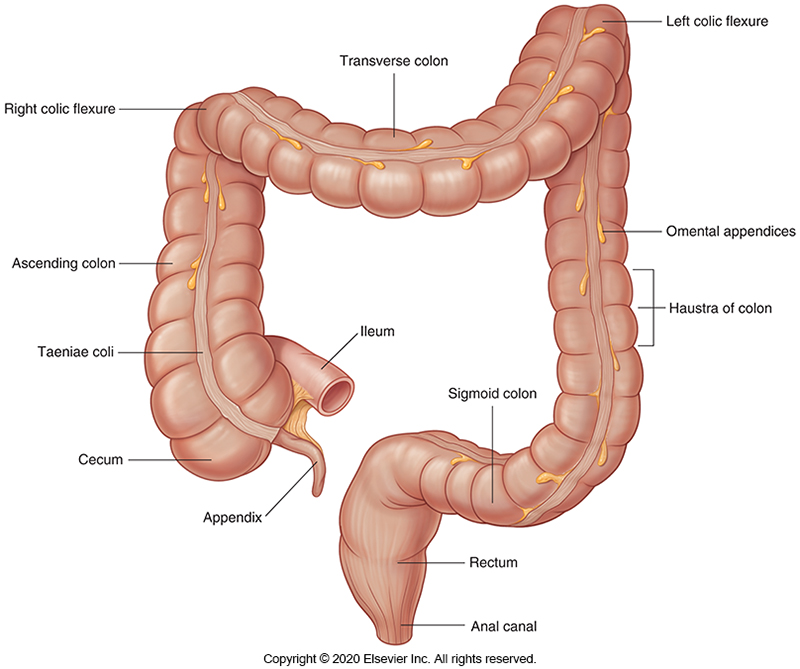
What is the 90° bend between the transverse and descending colon called?
Left colic flexure
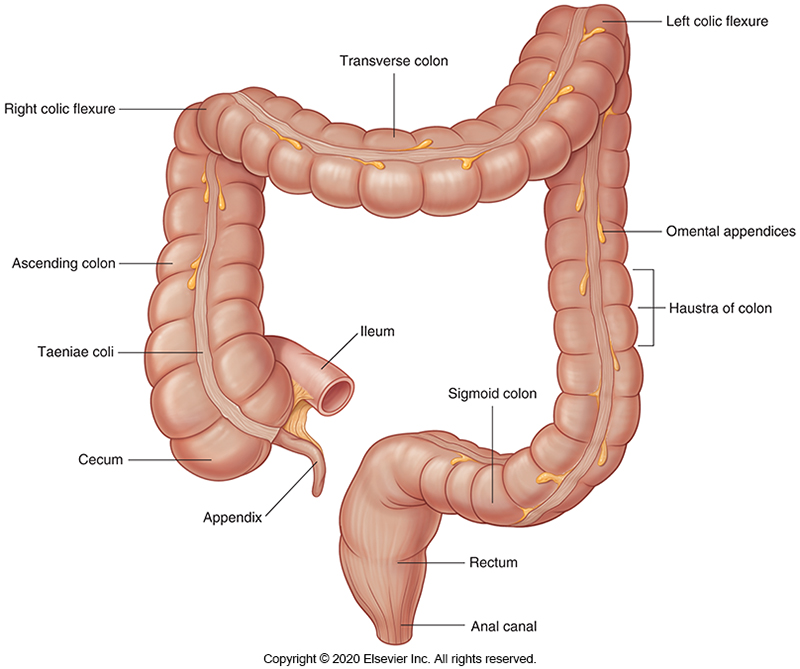
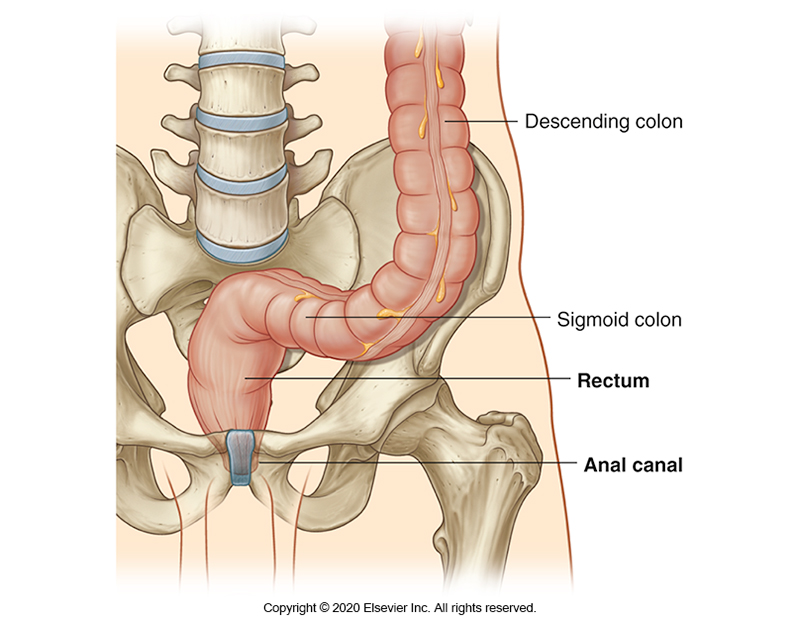
Where does the descending colon travel?
From the left upper to left lower quadrant.
Then becomes the sigmoid colon (S-shaped)
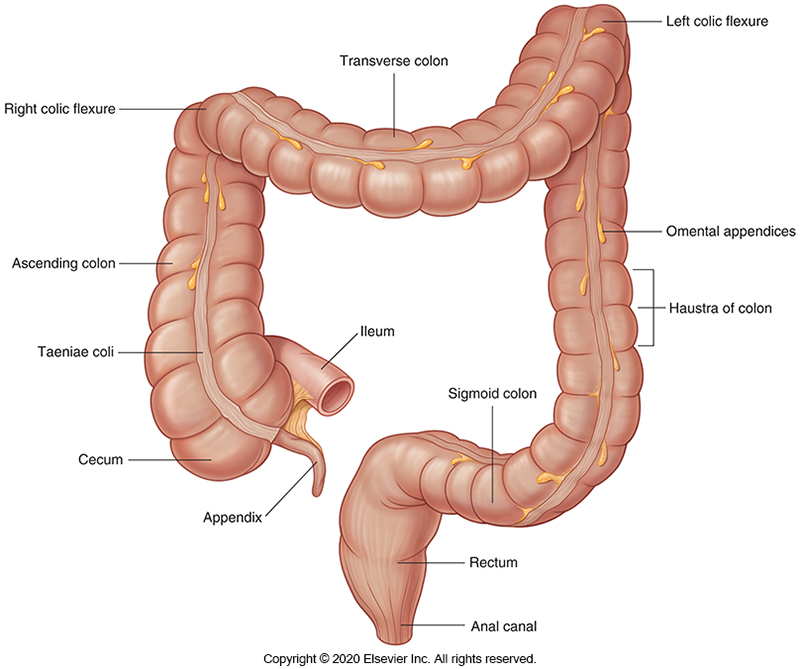
What does the sigmoid colon connect?
The descending colon with the rectum.
Where do the rectum and anal canal sit?
Within the pelvic cavity, posterior to the:
Vagina in females
Prostate in males.
What are some of the livers many functions?
Glucose storage
Protein, lipoprotein and cholesterol synthesis
Digestion: Production of bile and bile salts
Storage of fat soluble vitamins
Toxin and drug metabolism/excretion
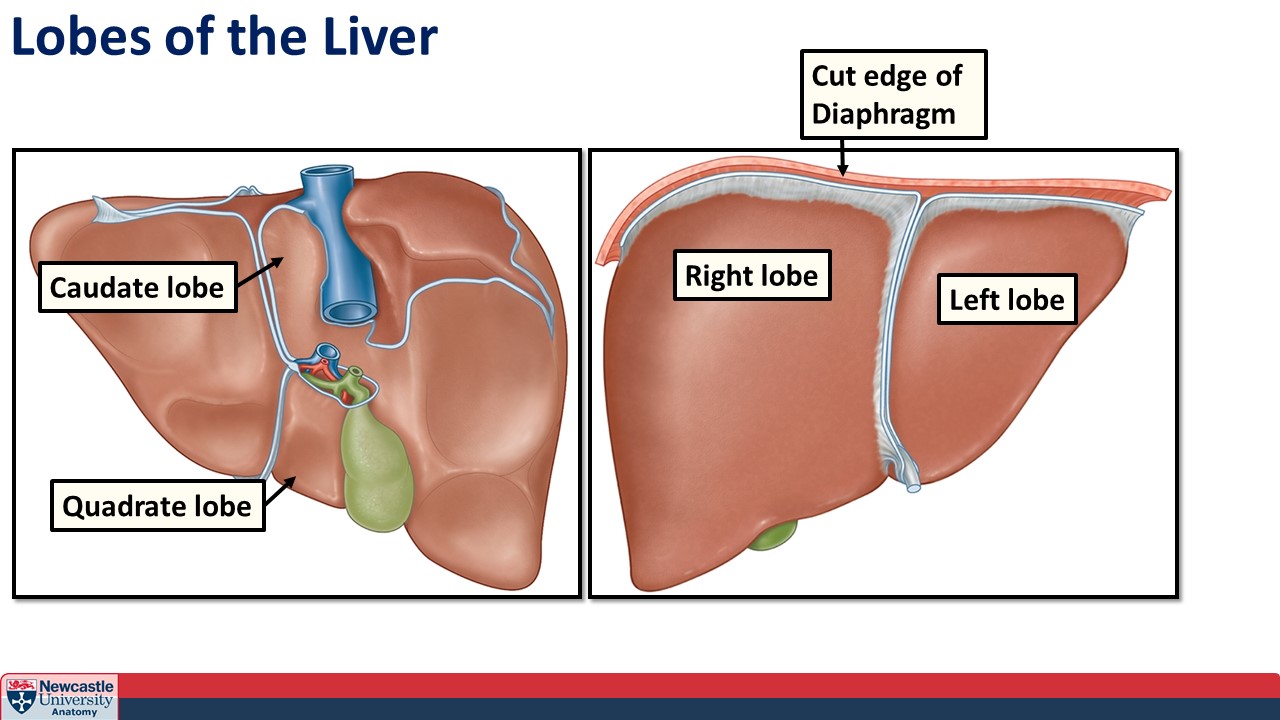
How many lobes does the liver have?
Four lobes
Right
Left
Caudate
Quadrate
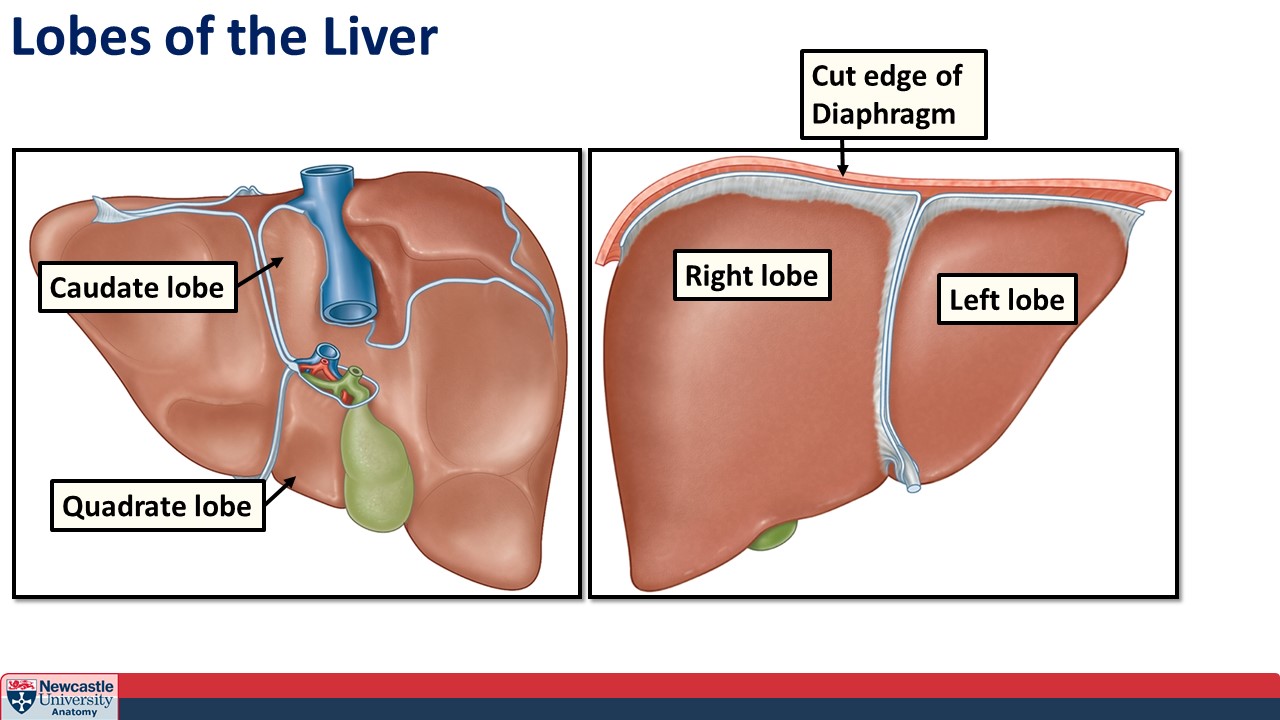
What are the four lobes of the liver?
Right lobe
Left lobe
Caudate lobe
Quadrate lobe
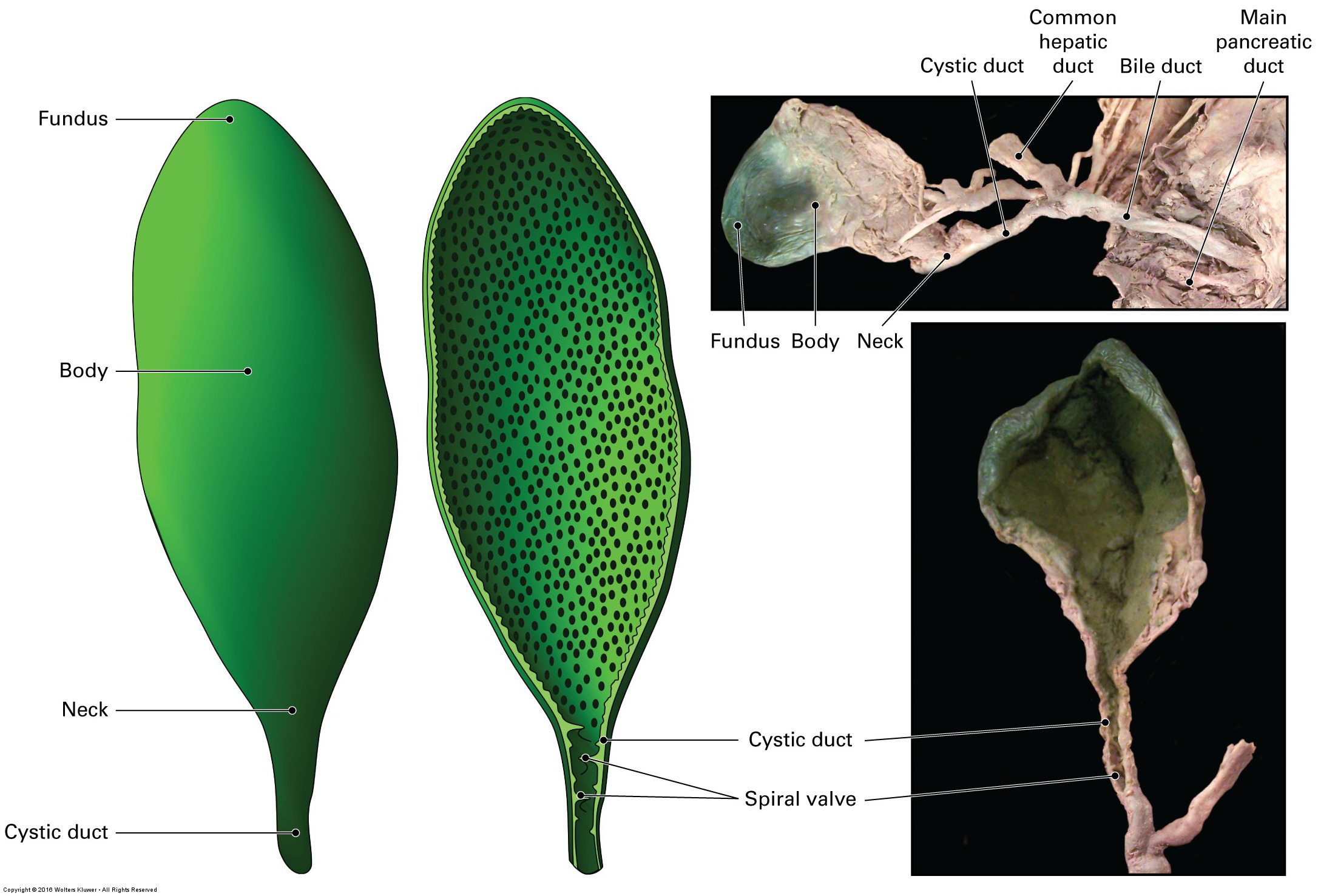
What is the gallbladder?
Fluid filled sac which stores and concentrates bile.
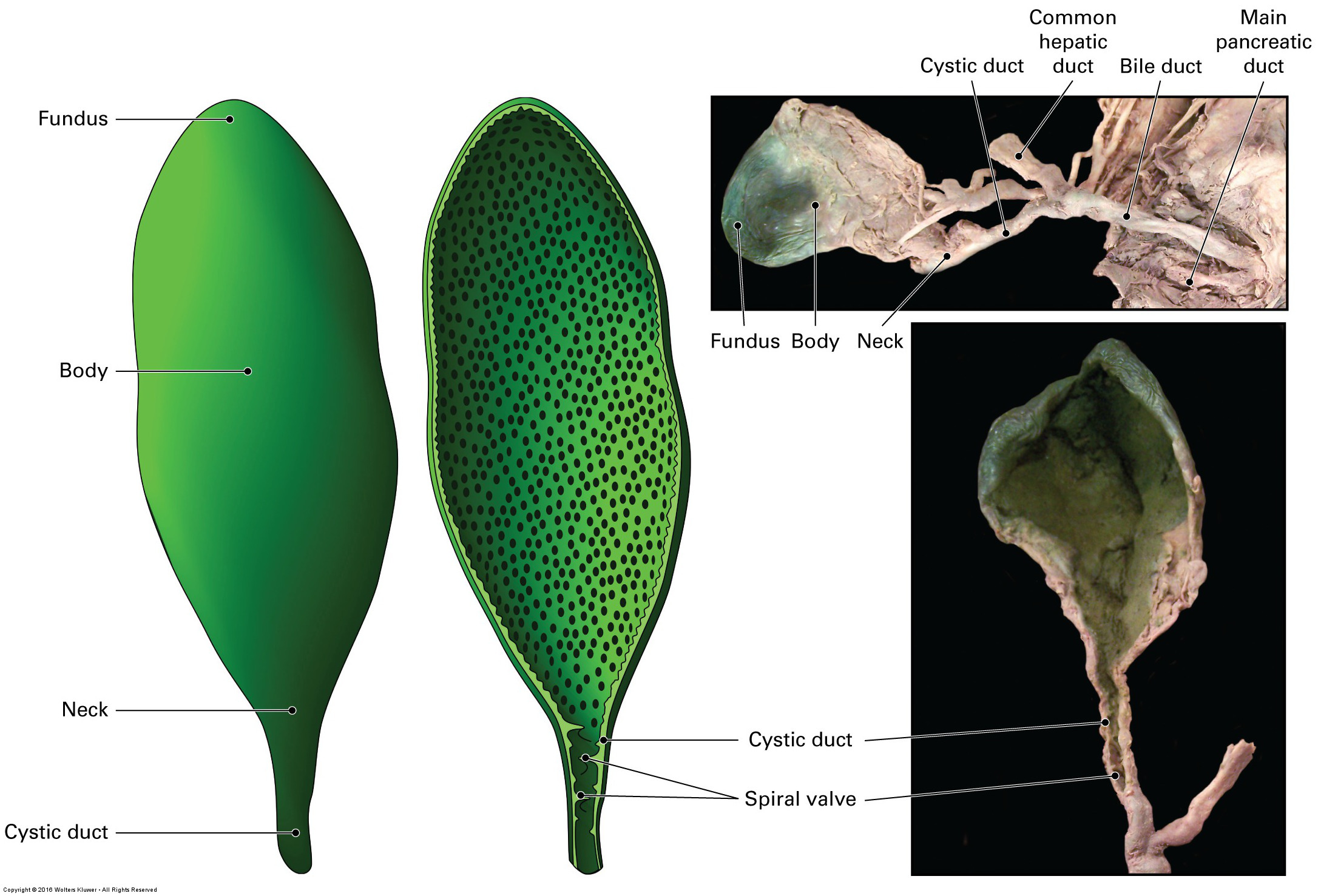
What three parts make up the gallbladder?
Fundus
Body
Neck
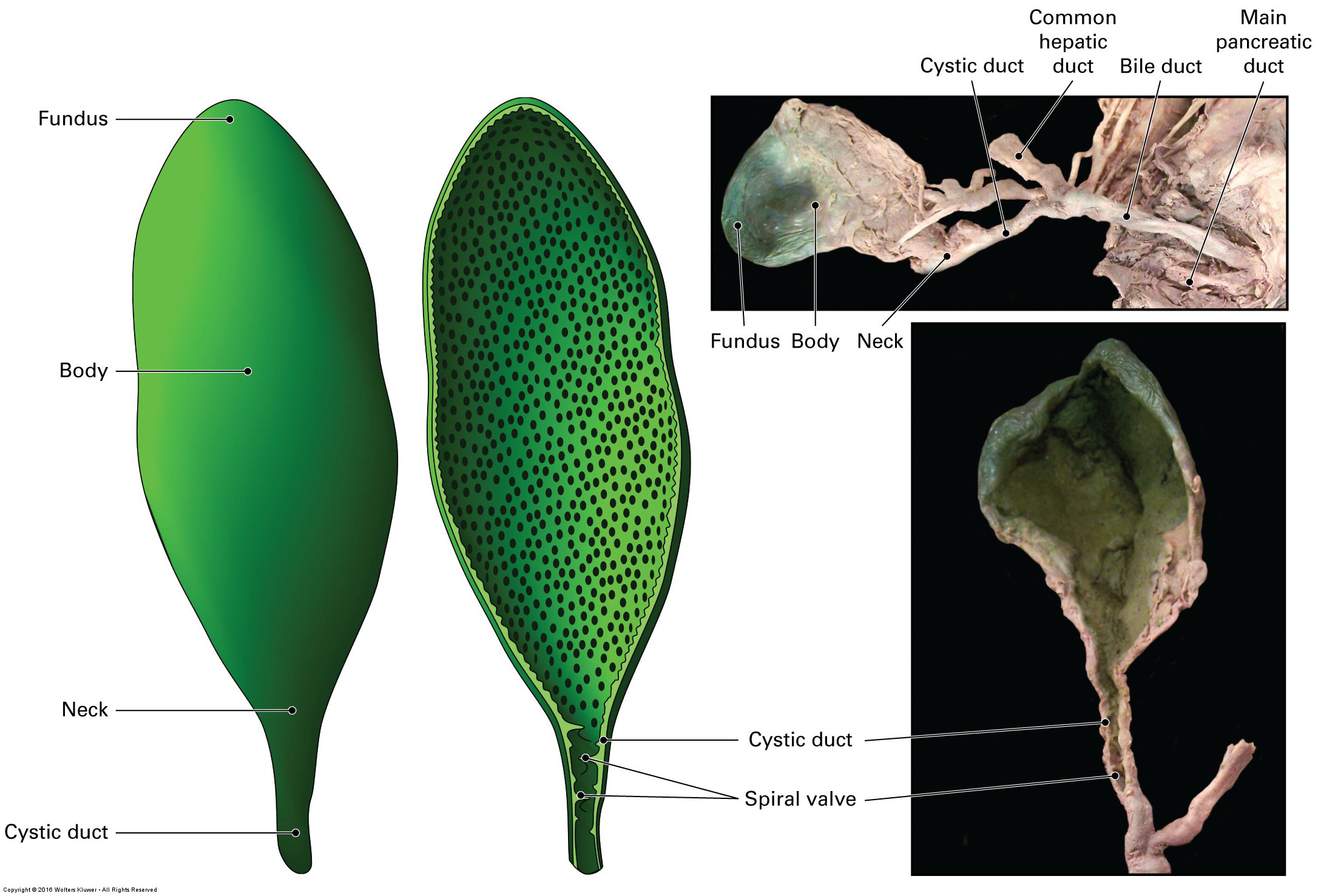
Where does the neck of the gallbladder lead to?
Into the cystic duct which transports bile to and from the gallbladder.
What are some of the roles of bile?
Produces an alkaline pH to decrease acidity of gastric contents released from the stomach
Decreasing pH also facilitates emulsion of fats by bile salts
Toxic waste products from the liver may also be excreted by the kidneys in the bile
What cell type produces bile?
Hepatocytes found in the liver.
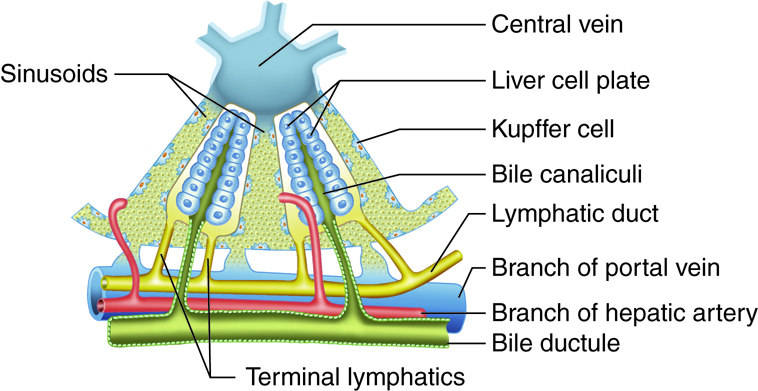
What are sinusoids in the liver?
Structure which runs between layers of hepatocytes in allow close contact between hepatocytes and portal blood supply
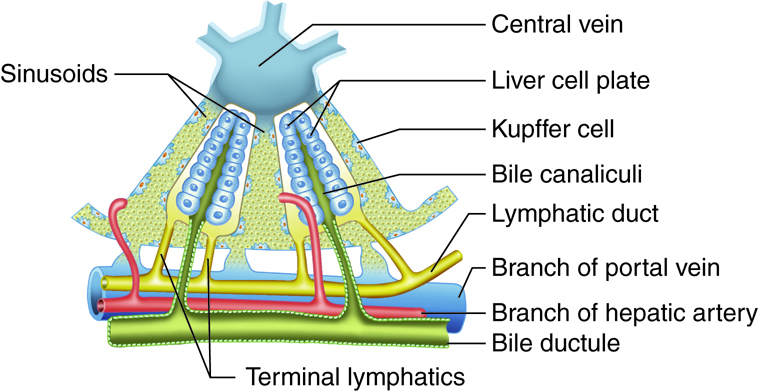
How is bile collected from the hepatocytes?
Products of hepatocyte function are removed via small channels found between cells called canaliculi.
Canaliculi then drain into bile ducts.
Bile ducts → Right/Left Hepatic ducts → Common hepatic duct → Common bile duct
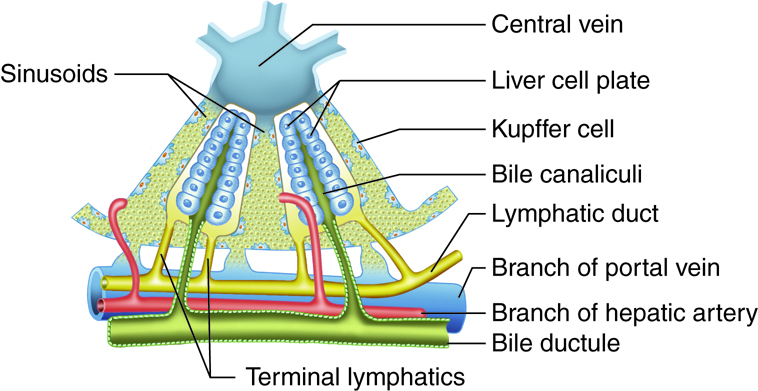
What does the unity of the common hepatic duct and the cystic duct form?
The unity forms the common bile duct.
Where does the main pancreatic duct join the common bile duct?
They join at the hepatopancreatic ampulla which opens into the duodenum.
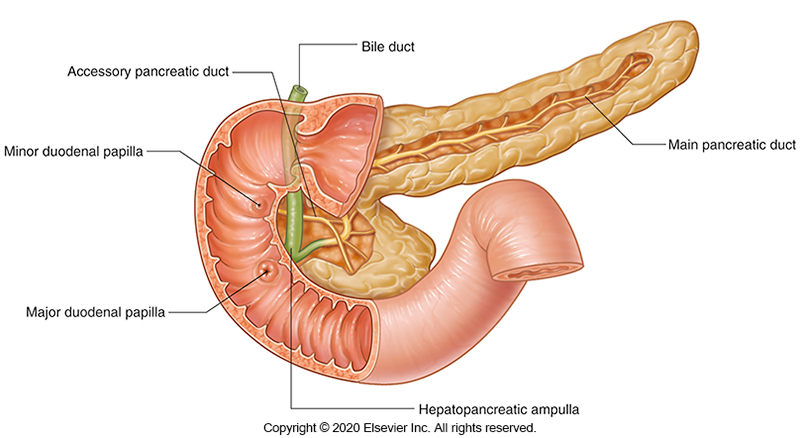
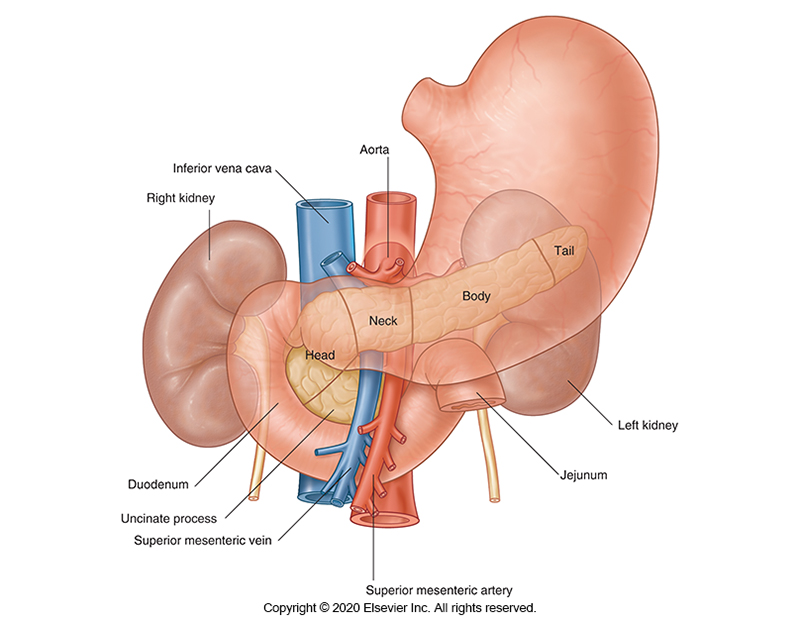
Where does the pancreas sit?
Lies horizontally across the posterior abdominal wall.
Sits posterior to the stomach.
What are the five regions which make up the pancreas?
Uncinate process
Head
Neck
Body
Tail
______ tissues of the pancreas release pancreatic juice.
Exocrine tissues.
What are the two components of pancreatic juice?
Alkaline secretion
High bicarbonate and low enzyme content
Helps neutralise acidic gastric contents
Enzyme rich secretion
Contains major digestive enzymes
Enzymes secreted as pre-enzymes which are activated in the gut
Why are digestive enzymes secreted by the pancreas released as pre-enzymes?
Pre-enzymes become activated in the gut.
This prevents the enzymes from digesting the pancreas.
Sympathetic stimulation of the pancreas causes ________
Decreased secretions
Parasympathetic stimulation of the pancreas causes ________
Increased secretions
How are exocrine glands similar to salivary glands?
Both contain acinus and ducts.
Pancreatic enzymes are secreted in the acinus and modified in the ducts
What controls entry of bile and pancreatic juice into the descending duodenum?
The Hepatopancreatic Sphincter (of Oddi)
What is the Peritoneum?
Layer of connective tissue which covers the walls and viscera of the abdomen.
What is the purpose of the peritoneum?
Acts to anchor floppy abdominal organs to the posterior body wall.
This prevents them from squashing each other or moving too much when we jump
Also carries blood supply to organs.
What is the greater omentum?
A major reflection or ‘flap’ of the peritoneum which covers the abdominal contents.
This is the first structure visible if you were to remove the anterior abdominal wall.
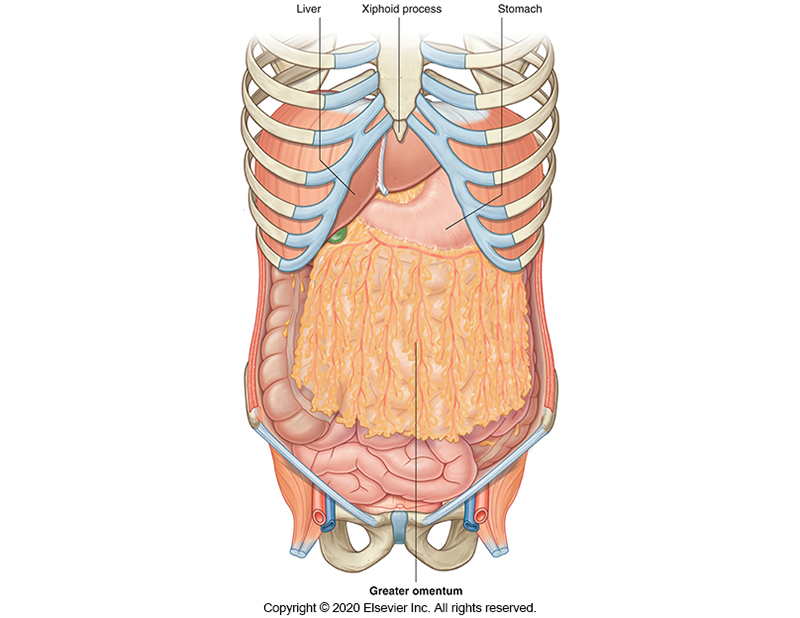
What is the mesentery?
A major reflection or ‘flap’ of the peritoneum which originates from the posterior abdominal wall.
It surrounds the majority of the small intestines.
What is the peritoneal cavity?
The continuous space around all the abdominal organs as a result of the peritoneum ‘vacuum packing’ the abdominal organs
What are the six classifications of epithelium found in the GI tract?
Squamous
Simple Squamous
Stratified Squamous
Cuboidal
Simple Cuboidal
Stratified Cuboidal
Columnar
Simple Columnar
Stratified Columnar
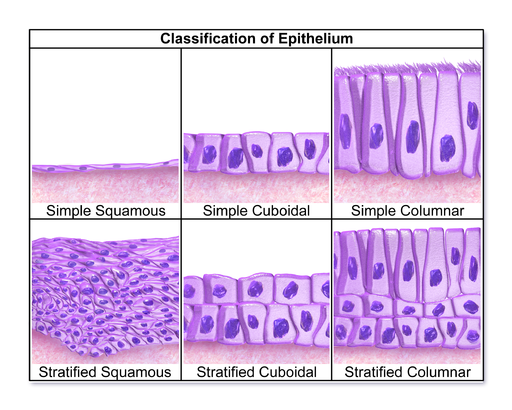
How thick is a simple epithelial layer?
1 cell thick
How thick is a stratified epithelial layer?
>1 cell thick
What is a pseudostratified epithelial layer?
A 1 layer thick epithelium which pretends to be 2 layers thick
What shape are squamous cells?
Flat cells.
What shape are columnar cells?
Column-like cells.
Long and thin
What shape are cuboidal cells?
Square shaped (cubes)
What four layers make up the wall of the digestive tract?
Mucosa
Submucosa
Muscularis externa
Serosa
The mucosa layer of the digestive tract can be further divided into three component layers. What are they?
Epithelium
Thin layer of cells which line the lumen
Lamina propria
Layer of loose connective tissue
Muscularis mucosa
Thin layer of smooth muscle cells which cause localised contractions of the mucosa
What is the submucosa of the digestive tract wall?
Layer of dense connective tissue which contains the submucosal plexus which is a component of the enteric nervous system
What is the enteric nervous system?
Branch of the autonomic nervous system which is entirely separate from the sympathetic and parasympathetic systems.
Can operate independently of the CNS
What two major plexi make up the enteric nervous system?
Myenteric and submucosal plexi
Old names: Meissner’s and Auerbach’s plexi