Local Anesthesia Unit 2 Review
1/155
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
156 Terms
What are the areas anesthetized by the IANB? (5)
1. mandibular teeth to the midline (cross innervation to incisors)
2. Body of the mandible (inferior aspect of ramus)
3. Buccal mucoperiosteum (central incisors posterior to M1)
4. Anterior 1/3 of tongue & floor of mouth (via lingual branch)
5. Lingual mucoperiosteum (via lingual branch)
After bone is contacted at an IANB, how much of the cartridge should you inject & when? (2)
1/2 cartridge (0.9 mL) slowly inject! after aspiration!
1/4 cartridge (0.45 mL) while removing the needle
How long can it take for an IANB to begin showing clinical effects on a patient?
5-10 minutes until patient may begin to feel numb (gravity)
Which of the following is a complication of an IANB due to the injection of the facial nerve near the parotid gland?
A. trismus
B. bell's palsy
C. numb lips
D. inability to speak
B. Bell's Palsy (temporary paralysis of half of the face, drooping eyes, lips, cheeks, resembling a stroke, etc)
Sometimes patients can experience trismus due to an accidental injection into a muscle. Which muscle is most commonly pierced? Where is the needle located to pierce this muscle?
Most common muscle = medial pterygoid
The needle is inserted below the mandibular foramen
Which structures are numbed via the long buccal nerve block?
buccal/some of lingual soft tissue only (adjacent to the mandibular molars)
Which structures are numbed via the mental nerve block? (3)
buccal soft tissues lying anterior to the mental foramen, soft tissues of the lower lip, soft tissues of the chin
Should you anesthetize with a mental block if you are performing an IANB? Why or why not?
NO!!! Because then you cannot assess success of the IANB initially because the mental block numbs the lips quickly
How much of a cartridge do you use in total for an IANB?
1/2 (0.9 mL) (+ 1/4 when removing the needle)
2 multiple choice options
How much of a cartridge do you use in total for a lingual nerve block?
1/4 (0.45 mL)
2 multiple choice options
How much of a cartridge do you use for a long buccal nerve block?
1/4 (0.45 mL)
What is the current standard of care for an aspirating dental syringe?
permits the ability for aspirating blood to help determine if the tip of the needle is located intravascularly
T/F: a prototypical dental syringe does NOT have to be aspirating
FALSE, it should be able to aspirate!! also: breech-loading, metallic, and be able to hold a cartridge
The weakest part of a needle is the _____.
hub
A higher gauge means a needle has a ______ diameter.
smaller (smaller lumen, more precise but also weaker needle bc it's thin)
A _______ gauge means a needle has a smaller diameter.
higher
Which gauge of needle is most commonly used for a mandibular block vs maxillary infiltration?
mandibular = 27-gauge long
maxillary = 30 gauge short
Select the needle gauge with the smallest diameter:
A. 20 (pink)
B. 25 (red)
C. 27 (yellow)
D. 30 (blue)
D. 30
3 multiple choice options
Which needle gauge is more prone to deflection?
A. 20 (pink)
B. 25 (red)
C. 27 (yellow)
D. 30 (blue)
D. 30 (blue)
What is the function of sodium metabisulfite in the anesthetic cartridge solution?
A preservative for the vasopressor (epinephrine)
What is the function of sodium chloride in the anesthetic cartridge solution?
makes the solution isotonic
What is the function of distilled water in the anesthetic cartridge solution?
helps dilute the solution & adds additional fluid volume
How do you convert % (percent) concentration of a local anesthetic to mg/mL? (hint: multiplication)
multiply the percent by 10
ex: 0.5%= 5 mg/mL; 2% = 20 mg/mL, etc
How do you calculate the number of milligrams (mg) of an anesthetic solution based on the cartridge volume (1.8 mL) and concentration (mg/mL)?
1. Multiply the concentration (%) by 10 to convert to mg/mL
2. Multiply the mg by 1.8
(concentration x volume = mg)
Jose is receiving an injection of 2% lidocaine plain. How many milligrams are distributed if the entire cartridge is used?
36 mg
explanation: 2x10 = 20 mg/mL x 1.8 mL = 36 mg of lidocaine
Brittany is receiving an injection of 0.5% lidocaine plain. How many milligrams are distributed if half of the cartridge is used?
4.5 mg of lidocaine
0.5x10 = 5 mg/mL x 0.9 mL = 4.5 mg of lidocaine
How do you convert a vasopressor ratio (g/mL) to mg/mL?
1. multiply the grams by 1000
2. divide the new ratio to find the number of mg in 1 mL
You finally got Taylor Swift as a patient! Moving to New York was worth it. Taylor needs a 2% lidocaine with 1:100,000 epinephrine injection for her restoration for #9 because she chipped it on a microphone :(. What is the concentration of the vasopressor in the solution?
1 g: 100,000 mL
1 g x 1000 = 1000 mg
1000 mg/100,000 mL = 0.01 mg/mL
How do you convert the concentration of a vasopressor (mg/mL) to the mg of vasopressor in the solution?
Multiply the concentration by 1.8 mL (total volume of cartridge)
Taylor loved your work on her #9 restoration. She sends Bella Hadid to you for veneers and needs an injection of lidocaine with 1:200,000 epinephrine. How many mg of epinephrine are in a 1:200,000 ratio for a 1.8 mL cartridge?
0.009 mg epinephrine
explanation:
1 g = 1000 mg
1000/200,000 = 0.005 mg/mL
0.005 mg/mL x 1.8 mL = 0.009 mg epinephrine
What color is lidocaine 2% with 1:100,000 epinephrine?
RED (cuz loving him was red and you used this on Taylor!!!)
What are the two types of maximum recommended doses (MRDs)?
1. weight-based (based on patient's weight)
2. absolute MRD (based on general max dose)
When should the weight-based maximum recommended dose (MRD) be used?
Every time, unless the weight-based MRD exceeds the absolute MRD!! aka use the lowest, safest MRD.
What is the absolute MRD for lidocaine with epinephrine?
500 mg
What is the weight-based (kg) MRD for lidocaine with epinephrine? (mg/kg)
7 (6.6) mg/kg
What is the weight-based (lbs) MRD for lidocaine with epinephrine? (mg/lb)
3 (3.2-3.6) mg/lb
What is the absolute MRD for lidocaine without epinephrine?
300 mg
What is the weight-based (kg) MRD for lidocaine without epinephrine? (mg/kg)
5 (4.4) mg/kg
What is the weight-based (lbs) MRD for lidocaine without epinephrine?(mg/lb)
2 mg/lb
How do you convert pounds to kilograms and vice versa?
pounds to kg:
multiply lbs by 0.45
divide lbs by 2.2
kg to pounds:
multiply kg x 2.2
How do you calculate the maximum number of cartridges based on the MRD?
MRD (mg) divided by # mg/cartridge
Theo James weighs 90 kg and is receiving lidocaine with epinephrine. What is his MRD? What is the maximum number of cartridges you can use?
7 x 90= 630 but absolute is 500!!! so you have to use 500!!!
500 mg/36 mg= 13.86 cartridges
Snoop Dogg weighs 120 pounds and is receiving lidocaine without epinephrine? What is his MRD? What is the maximum number of cartridges you can use?
2x120 = 240 mg (max is 300, safer to use 240)
240 mg/36 mg= ~6.67 cartridges
Your 12 year old patient, Little Miss Pink weighs 50 kg and is receiving lidocaine with epinephrine. What is her MRD? What is the maximum number of cartridges you can use?
50x7 = 350 (absolute is 500, safer to use 350)
350/36 = 9.7 cartridges
Which of the following local anesthetics is NOT available in the US?
A. bupivacaine
B. mepivacaine
C. procaine
D. articaine
C. procaine (novocaine)
For which type of patient is 3% mepivacaine plain commonly used?
For patients that are contraindicated for vasoconstrictors (cardiac patients or hypertensive patients)
OR pediatric patients for general dentists (DO NOT OVERDOSE!! common with this drug!)
What other drug can be used for patients with contraindication for vasopressors in their local anesthetic?
Prilocaine (citanest)
Which of the following conditions are contraindicated for prilocaine?
A. idiopathic or congenital methemoglobinemia
B. sickle cell anemia/anemia in general
C. hypoxia
D. All of the above
D. all of the above
If a successful IANB is performed, but the patient is still sensing pain on their mandibular molars, what other nerve could be innervating these structures that may not have been anesthetized via the IAN block?
A. incisal nerve
B. greater palatine nerve
C. lingual nerve
D. mylohyoid nerve
D. mylohyoid (solution; a higher IANB will also block the mylohyoid nerve)
For which types of injections is articaine NOT recommended for?
Regional, mandibular blocks: specifically, IAN/lingual blocks (persistent paresthesia)
Which of the following anesthetics are typically NOT recommended for an IAN or lingual nerve block due to persistent paresthesia? Select all that apply.
A. bupivacaine
B. prilocaine
C. mepivacaine
D. articaine
B & D (prilocaine 4% & articaine 4%) & lidocaine from the readings is barely bad for paresthesia
Place the anesthetics in order based on onset speed:
(fastest) mepivacaine, articaine, lidocaine, prilocaine, bupivacaine, procaine (slowest)
Meep! Arti Lied to Priscilla But Pros (don't care)
1 multiple choice option
A ____ (higher/lower) pKa has a slower onset.
higher pka = slower onset
A lower pKa has a _____ onset.
faster onset; lower pKa = faster onset
Which of the local anesthetics has a lowest vasodilation?
mepivacaine (remember it's common to use mepivacaine plain 3% for patients who cannot receive a vasoconstrictor)
T/F: the PDL injection does NOT pass through the actual PDL fibers
TRUE!! goes in the spaces around the PDL fibers in the periapical tissue/interseptal bone
Which of the following are considered modified intraosseus injections? Select all that apply.
A. PDL injection
B. Intraseptal injection
C. Mental nerve block
D. all of the above
A & B (PDL & intraseptal)
How many teeth are anesthetized by an intraosseous injection?
literally only one tooth (distal)
How is an intraosseous injection technique performed? (3 main steps)
1. push the perforator through the soft tissues until bone is contacted
2. activate the slow speed handpiece penetrating bone with a "pecking" motion until resistance is lost (~2 seconds)
3. hold the guide sleeve in place until the drill is withdrawn (remains until you are sure you have achieved adequate anesthesia)
Why do you use a pecking potion when performing an intraosseous technique?
to avoid overheating the bone, high pressure is not needed to deliver the anesthetic into cancellous (spongy) bone
T/F: a 2% lidocaine with 1:100,000 epinephrine poses a risk for ASA I-II patients with an intraosseous injection.
FALSE!! Vasoconstrictors are not contraindicated when using an intraosseous injection for ASA I-II patients (can still increase HR)
Intraosseous injection techniques should be avoided in patients with mixed (deciduous + adult) dentition due to possible ____ ____ damage.
tooth bud
Intrapulpal injections are most commonly used on ______ ______.
mandibular molars (not exclusively)
T/F: intrapulpal injections are associated with brief pain by the patient
TRUE! Intense, instantaneous pain is usually felt briefly by the patient
Which of the following injection types deem it to be appropriate to retrieve the needle if it is bended due to easier retrieving?
A. intrapulpal
B. IANB
C. PDL
D. lingual
A, C
T/F: once you bend a needle once, you may as well just bend it again
FALSE!! not ideal to ever bend the needle but if you do, only bend it once to prevent breakage
What are the 4 main branches of the V2 nerve?
ASA (anterior superior alveolar n), MSA (middle superior alveolar), PSA (posterior superior alveolar), greater palatine nerve
Which structures are anesthetized by a V2 Maxillary Nerve Block? (4)
1. pulpal nerves of all teeth on ipsilateral side of injection
2. buccal periodontium and bone on side of injection
3. soft tissue & bone of the hard/soft palates medial to midline
4. skin of lower eyelid, side of nose, cheek, and upper lip
What are the two alternative approaches to a Maxillary V2 nerve block?
high tuberosity & greater palatine approaches
What is the target of the High Tuberosity (PSA) approach for a V2 injection?
maxillary nerve as it passes through the pterygopalatine fossa
other steps: 25 or 27-long gauge, should NOT contact bone, use 30 mm of needle depth, use entire cartridge (1.8 mL)!!
What is the target of the Greater Palatine Approach for a V2 injection?
V2 as it passes through the pterygopalatine fossa, access through the greater palatine canal
other steps: use a 27-long gauge, perform greater palatine block first, insert depth of ~30 mm
What should you do if you encounter a bony obstruction during a Greater Palatine Approach for V2 injection?
5-15% of patients have the obstruction in their nasopalatine canal, so you will rotate the needle and do NOT force it! if unable to pass the needle through, inject slowly or abort mission
Which of the following complications occurs from a Greater Palatine Approach into the orbit?
A. optic nerve anesthesia, causing loss of vision
B. block of 6th cranial nerve, causing diplopia (abducens)
C. periorbital swelling or proptosis
D. retrobulbar hemorrhage, causing corneal anesthesia
E. all of the above
E. all of the above
T/F: a Gow-Gates block is used as a supplemental mandibular injection.
true
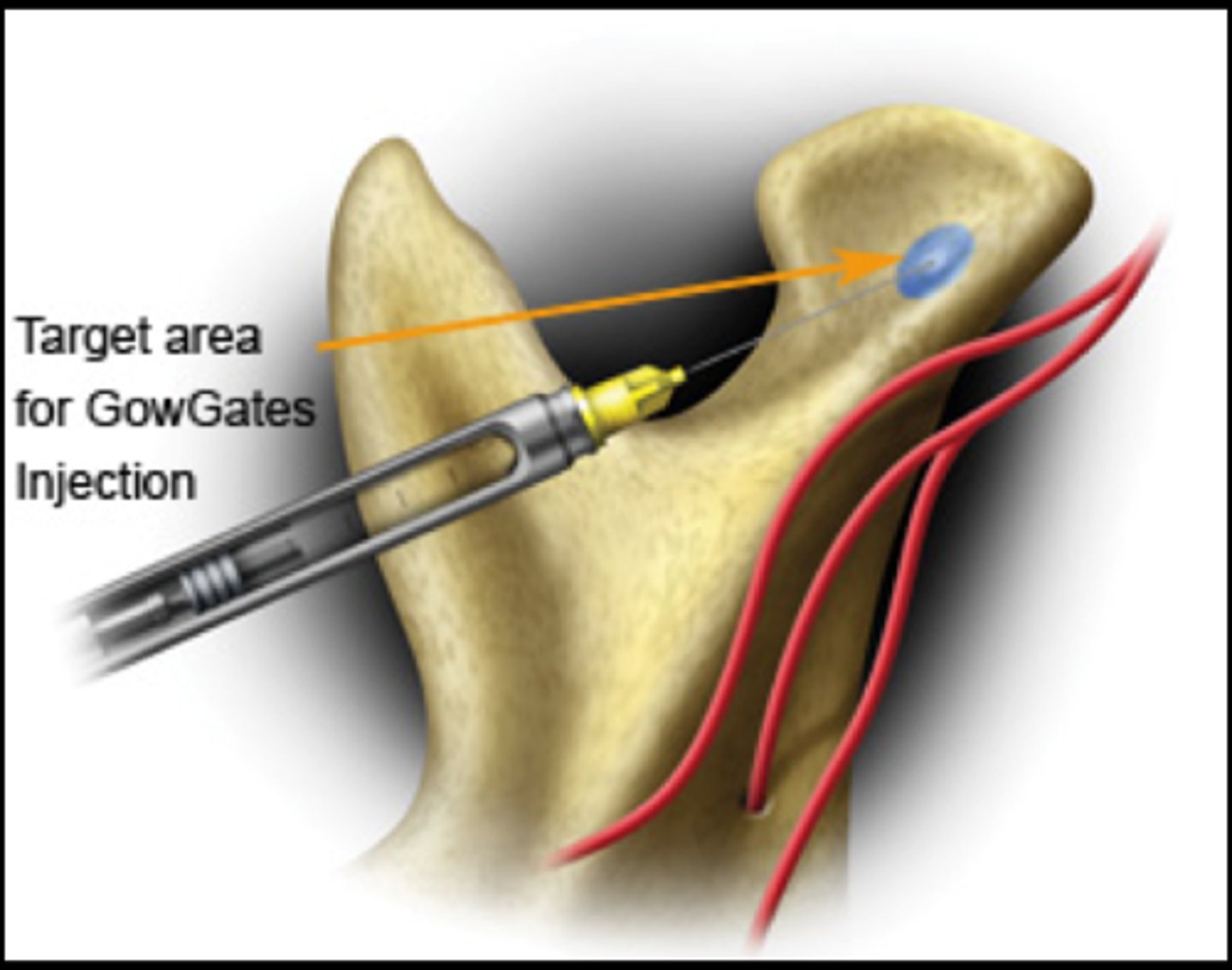
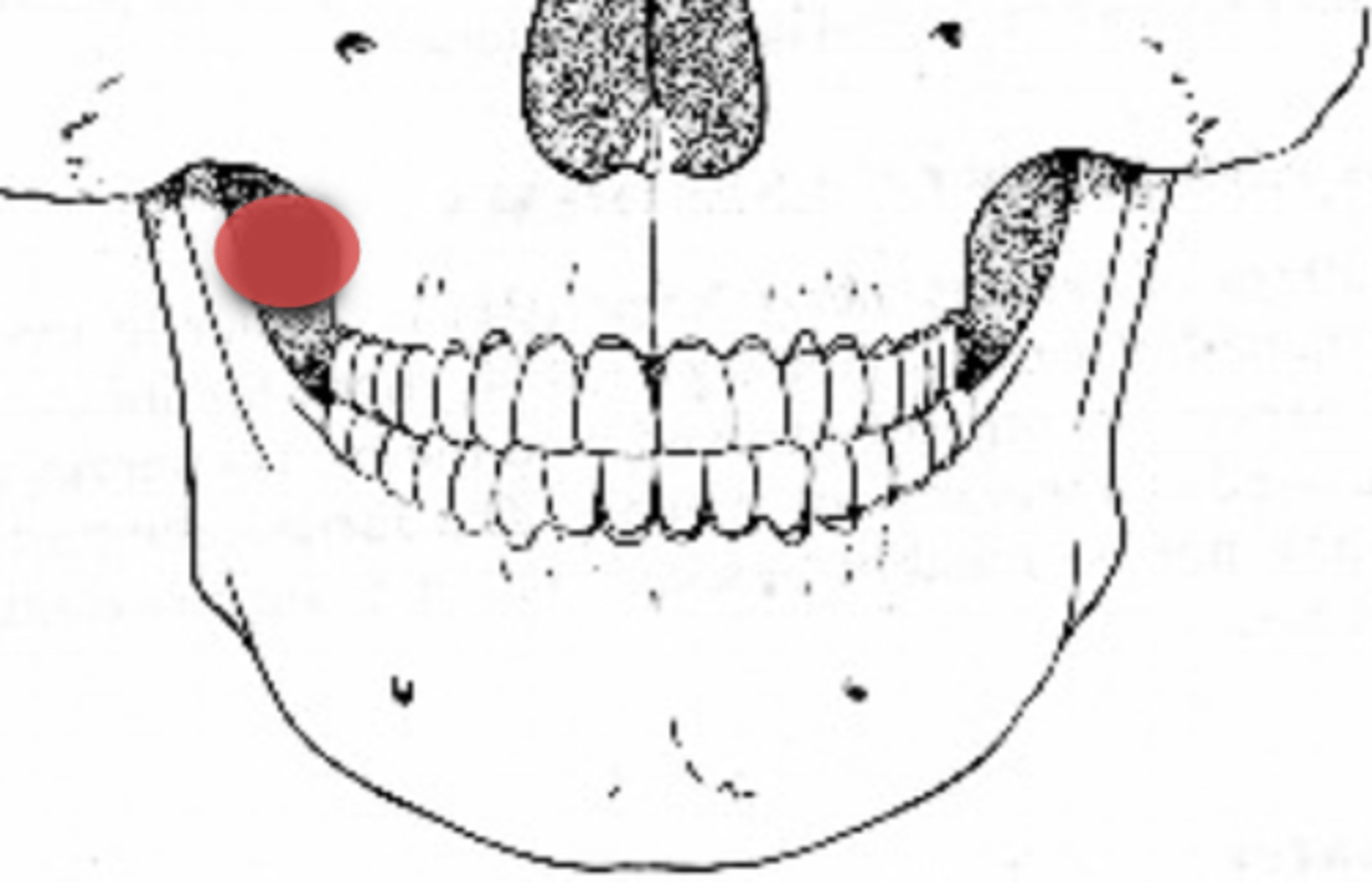
What is the target of the Gow-Gates block?
medial aspect of the condyle, higher than the IANB before the CN V3 branches (higher than lingual, long buccal, & IAN)
The _____ block's target is between Gow-Gates & IANB.
Akinosi
When would you use an Akinosi block in patients?
When a patient cannot open maximally (trismus) because the approach doesn't require the patient to open their mouth
What should you do if a patient experiences persistent anesthesia or paresthesia? (protocol for patient, chart/records/follow up/referral)
Patient --> reassure them, speak with them in person, have them follow up initially with you
Chart/Records --> record initial findings & determine degree/extent
Follow Up --> every 2 months for 1 year (6 times a year), If it does not subside/resolve, consider referring to an OMFS or neurologist
____ ______ usually involves part of the distribution and puts a patient at risk for self injury (burning or biting)
persistent anesthesia
______ alters a patient's sensation (hyperesthesia or dysesthesia) and is often more bothersome than complete numbness in an area
paresthesia
What are causes of paresthesia/persistent anesthesia? (2)
trauma from the needle, causing an "electric shock sensation" OR a local anesthetic solution that may be neurotoxic
_____ is the restricted ability to maximally open
trismus
a hematoma is bleeding into ______ spaces and stops once pressure _____.
extravascular (outside the vessels); equalizes (apply direct pressure for 2+ minutes)
Hematomas are often caused by the nicking of a blood vessel in which two injection types?
PSA (posterior superior alveolar n) & IAN block
During facial nerve paralysis, it is important to evaluate the patient's ____ & ____ responses to rule out a CVA/stroke.
sensory & motor
During facial nerve paralysis, it is important to evaluate the patient's sensory & motor responses to rule out a _____.
CVA/stroke
How can you prevent a soft tissue injury in patients?
remind patients/parents for patients to not chew or bit their lip & avoid hot foods/liquids until their sensations return... common for children or special needs pts to bite their lips or tongue with anesthesia
What is the most common adverse drug reaction?
Overdose reaction (~99% by some estimates)
Statement 1: A vasoconstrictor in an LA can help prevent overdose
Statement 2: Injecting LA directly into a blood vessel decreases the risk for an overdose
Statement 1 is true, statement 2 is false (it increases the risk)
With a local anesthetic, it is common for overdosing to cause _____ effects
CNS (CNS depression S/S)
WIth a vasopressor, it is common for overdosing to cause _____ effects.
cardiovascular effects (tachycardia, high BP, etc)
If a patient is having a severe overdose reaction, what should you do first?
A. reassure & monitor patient
B. provide basic life support until help arrives
C. call 911/activate EMS
D. cause emesis (throwing up) so they can get it out of their system
C. call 911/EMS and then provide basic life support until help arrives
When is the onset of an immune complex allergy? Which antibody type is it mediated by?
A. IgE, immediate
B. IgG, 6-8 hours
C. IgM, 3-4
D. none of the above
B. IgG, 6-8 hours
Which allergy reaction is most common from ester local anesthetics due to PABA?
delayed hypersensitivity (type 4)
Statement 1: a patient cannot be allergic to epinephrine
Statement 2: a patient can be allergic to metabisulfite, amides, and esters
both are true (esters from PABA, amides extremely rare, metabisulfite for vasoconstrictor preservation)
Metabisulfites are ______ used to preserve vasoconstrictors.
antioxidants (oxidation turns it rusty and red so don't use any LA that isn't clear)
What should you do if a patient has a true allergy and you need to prepare for accidental exposure?
find your epipen or epinephrine vial
Type IV allergy reactions are also called _____ _____ reactions
delayed hypersensitivity
How should you manage a patient with a type IV allergy?
avoid the offending agent & perform palliative care (ABX?)
What should you document after administering a local anesthetic? Select all that apply.
A. total dose of all drugs administered
B. techniques/blocks/injection types used
C. record individual agents if multiple are used
D. patient's response to anesthesia
A, B, C, D