PTE 731: exam 3
1/279
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
280 Terms
according to the notes, what is the definition of a red flag noted during a neurological screen?
any alterations in mental status, sensations, reflexes, balance, and movement/strength
emergent referrals
immediate medical attention needed
non-emergent referrals
urgent but not life-threatening
what are the ascending motor tracts?
dorsal column-medial lemniscus tract and anterolateral spinothalamic tracts
what are the descending motor tracts?
lateral corticospinal and ventral corticospinal tracts
what is the primary responsibility of the lateral corticospinal tract?
controlling contralateral fine motor movements of the limbs, particularly the distal muscles
crucial for skilled, precise voluntary movements
what is the primary responsibility of the anterior corticospinal tract?
controlling bilateral gross motor movements of the trunk and proximal musculature
crucial for movements for posture and balance
the _____ tract is responsible for deep touch, proprioception, and vibratory sensations.
DCML
the ___ tract is responsible for pain and temperature sensations.
ALS
how would a therapist determine if a spinal cord injury is incomplete?
if there is an odd presentation, where right/left and UE/LE examinations don’t match
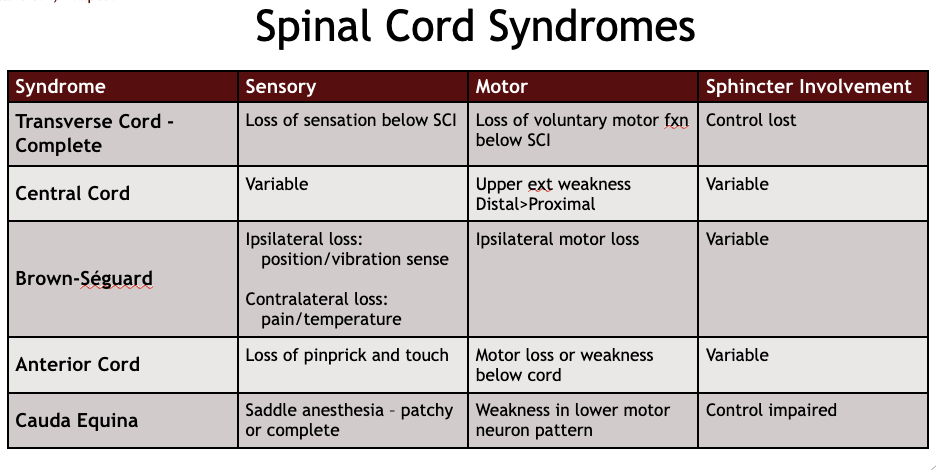
spinal cord syndromes chart
what are the two most common characteristics seen with a central cord lesion?
most common incomplete spinal cord injury
most commonly in cervical and thoracic spinal levels
a SCI patient presents with dysfunction and weakness in his upper extremities, specifically in his hands, along with using descriptors like tingling and burning for his pain in those regions. upon further questioning, he admits to peeing often (bladder dysfunction) and feeling like his bladder is always full (urinary retention). which spinal cord lesion should the therapist suspect?
central cord
T or F: central spinal cord lesions often present bilateral symptoms but the symptoms can be asymmetric.
T
extreme and forceful head movement into _________ can result in a central cord spinal lesion.
hyperextension
what are some examples of underlying pre-existing pathologies associated with central cord lesions?
spondylosis
atlantoaxial instability
tethered cord
spinal abscess
syringomyelia
a patient presents with UE and LE motor loss to one side. the therapist performs other tests to rule out a stroke and discovers the patient cannot perceive pain on the contralateral UE and LE. however the patient experiences little to no sensation on the same side as the motor loss. what should the therapist conclude?
brown-sequard spinal cord lesion
describe a brown-sequard lesion.
transverse hemi-section of the spinal cord is affected
list some possible traumatic and non-traumatic incidents that could lead to a brown-sequard lesion.
traumatic: stab or gunshot wound, fracture
non-traumatic: tumor, disc herniation, radiation
when performing the adult neurological exam, a SCI patient fails the pain/temp tests and the light touch tests, but experiences no problems with the proprioception tests. she also exhibits bilateral motor lost below T10. what spinal cord lesion should the therapist conclude?
anterior cord
extreme and forceful head movement into _________ can result in an anterior cord spinal lesion.
hyperflexion
list some direct and indirect incidents that could lead to an anterior spinal cord lesion.
direct: crush injury, burst fracture, gunshot or stab wound
indirect: occlusion, ischemia, or hypo-perfusion of the anterior spinal artery
a SCI patient complains of uncontrollable bowel and bladder movements along with increasing weakness in bilateral LEs. upon further inspection, the patient states he cannot feel sensations around his crotch region. which spinal cord lesion should the therapist suspect?
cauda equina
a cauda equina diagnosis should result in a 911 call. what five characteristics should a therapist be “on the look out for”?
bilateral neurogenic sciatica
reduced perineal sensation
loss of anal tone
altered bladder function leading to painless retention
loss of sexual function
list some examples of clinical signs and symptoms of a neurological impairment.
confusion
depression/irritability
drowsiness/lethargy
dizziness/light-headedness
loss of consciousness
vision or speech changes
no positive changes in gross motor exam →
no further testing required (like sensory function)
according to the notes, what are the seven steps of the neurological exam?
mental and emotional status
cranial nerves
sensory function
motor function
reflexes
neural tension
vision
what is Marcus Gunn Pupil?
occurs when there is damage to the optic nerve or severe retinal disease on one side; characterized by an abnormal response to light when performing the swinging flashlight test
aka: relative afferent pupillary defect (RAPD)
describe the clinical presentation of Horner’s Syndrome.
ptosis (drooping eyelid), miosis (constricting pupil), and anhidrosis (lack of sweating on face)
what is the purpose of performing neural tension testing?
to assess whether the nerves are being stretched, compressed, or irritated during certain movements and to pinpoint the area where
vision makes up ___ of cortex making it one of the most important senses.
50%
saccades
fast, voluntary eye movements used to shift the eyes’ focus from one object to another
why might a therapist perform a saccadic visual test?
to gain insight into the function of the CNS, particularly the brain’s eye movement control centers that affect eye movement coordination, attention, and gaze control
describe the saccadic testing procedure.
the patient is asked to alternate gaze between two stationary objects placed horizontally or vertically 12-18 inches apart
the examiner observes how quickly and accurately the eyes move from one target to the other
what aspects of eye movement does the saccadiac procedure test?
accuracy, speed, corrective movements, hypermetria or hypometria
which diseases can display abnormal saccadic function?
Parkinson’s disease, Multiple Sclerosis, stroke, or TBI
what is the difference in clinical significance between delayed saccades or multiple corrective movements found during the testing?
delayed: neurological conditions affecting the frontal eye fields or brainstem pathways
multiple corrections: dysfunctions in cerebellar or brainstem regions
what is the vestibular ocular reflex (VOR)?
an involuntary reflex that keeps vision stable by making the eyes move in the opposite direction of head movement to keep focus on a target
vital for maintaining clear vision while moving and preventing the world from appearing blurry or bouncing
what is the purpose of the VOR testing?
assess the function of the vestibular system (balance) and its interaction with the ocular system
describe the VOR head-thrust test.
patient is asked to focus on a stationary target
examiner moves patient’s head rapidly and unpredictably to one side and then the other
eyes should remain fixed on the target during head movements if the VOR is functioning properly
positive if patient’s eyes move off target
describe the dynamic visual acuity test.
patient is asked to read a line of letters from an eye chart
test repeated while the patient’s head is moved side to side by the examiner
positive if reduce visual acuity occurs
what is the smooth pursuit system?
a set of neurological circuits that allow the eyes to smoothly follow a moving object, keeping its image stabilized on the fovea for clear vision
what is the purpose of smooth pursuit testing?
evaluates and assesses the integrity of the visual tracking system via eyes’ ability to smoothly track a moving object
critical for maintaining visual focus during slow, controlled movements
which disorders may produce an impaired smooth pursuit system?
cerebellar disorders, Parkinson’s disease, multiple sclerosis, concussion, and/or TBI
what is eye convergence?
the simultaneous inward movement of both eyes towards an object to ensure the object remains in focus on both retinas
allows for clear, single vision at close distances
what is the procedure for testing the eye convergence system?
patient is asked to focus on a small object held at arms length in front of the face
the object is slowly moved toward the patient’s nose
the patient is instructed to follow the object with both eyes until he or she experiences double vision or can no longer maintain focus
list the convergence insufficiency symptoms.
eye strain
headaches
double vision or blurred vision
difficulty concentrating
the central nervous system is responsible for…
controlling bodily functions and is the center for behavioral and intellectual abilities
why do CNS drugs need to modify the activity of neurons to treat specific disorders or alter the general level of CNS arousal?
CNS drugs alter neurotransmitters so they can traverse the blood brain barrier to exert their effects on the CNS
what’s the difference between white mater and grey mater:
white mater: consists of myelinated axons of neurons (tracts) that ascend or descend between the brain and spinal cord
grey mater: area of synaptic connections between various neurons
cerebrum
composed of frontal, temporal, parietal, and occipital lobes; highest order of conscious function and integration
drugs affect on the cerebrum:
indirectly, except epilepsy and Alzheimer’s drugs
basal ganglia
group of specific areas located deep within the cerebral hemispheres; primarly involved in control of motor activities
drugs affect on the basal ganglia:
target BG movement disorders
diencephalon
area enclosing the third ventricle (thalamus and hypothalamus)
thalamus: relays sensations and hypothalamus: controls hormones
drugs affect on the diencephalon:
influence body functions and sensations
mesencephalon and brainstem
midbrain, pons, medulla
drugs affect on the mesencephalon and brainstem:
impact alertness and arousal
cerebellum
plans and coordinates motor activity; maintains balance and posture
drugs affect on the cerebellum:
do not target actually! but if there is toxicity in the system, individual will demonstrate unwanted movements
limbic system
cortical: amygdala, hippocampus, cingulate gyrus; hypothalamus, mammillary bodies, and septum pellucidum; controls emotional and behavioral activity
drugs affect on the limbic system:
target motivation, aggression, sexual activity, instinctive responses, anxiety, and psychosis
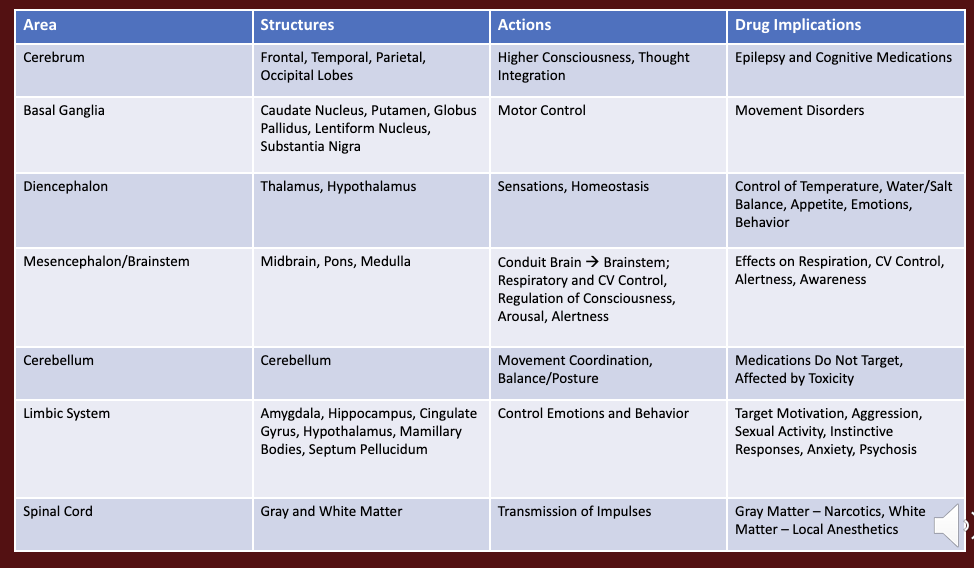
drug and brain region chart
why is the drug treatment complexity higher/more challenging in the central nervous system than the peripheral?
complex structure and function of CNS
blood-brain barrier limits drug entry
neurotransmitters interact with multiple receptor subtypes
neurons are plastic and adaptable
what is the blood brain barrier?
a highly selective membrane, comprised of tight endothelial junctions and astrocytic end-feet, that separates the blood circulating in the brain from the brain tissue
protects the CNS from toxins and maintains a stable environment
by which two mechanisms can a drug enter the blood brain barrier?
1) must be lipid soluble or 2) via carrier-mediated transport
list the four neurotransmitters discussed in class.
biogenic amines
amino acids
neuropeptides
acetylcholine
what substances are associated with the neurotransmitter biogenic amines?
dopamine, norepinephrine, and serotonin
what substances are associated with the neurotransmitter amino acids?
glutamate/aspartate, GABA, and glycine
what substances are associated with the neurotransmitter neuropeptides?
substance P and endorphins/enkephalains
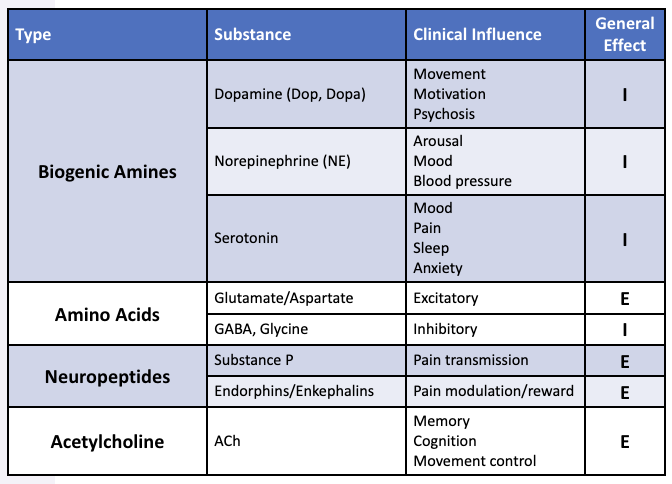
neurotransmitter chart
T or F: biogenic amines and neuropeptides required g-protein linked receptors to act on cells.
T
amino acids and acetylcholine require ___ ________ to act on cells.
ion channels
__________ neurotransmitters increase the likelihood that the postsynaptic neuron will fire an action potential by causing a depolarization of the postsynaptic membrane.
excitatory
________ neurotransmitters decrease the likelihood of postsynaptic firing by causing a hyper-polarization of the postsynaptic neuron.
inhibitory
what are the nine steps of a synaptic transmission?
action potential
neurotransmitter synthesis
neurotransmitter storage
neurotransmitter release
neurotransmitter reuptake
neurotransmitter degradation
postsynaptic receptors
presynaptic autoreceptors
membrane effects
action potential
initiates neurotransmitter release
neurotransmitter synthesis
blockading synthesis will eventually deplete the presynaptic terminal and impair transmission
neurotransmitter storage
impairing storage decreases synapses ability to transmit for extended periods
neurotransmitter release
increasing/decreasing neurotransmitter release modulates synaptic activity
neurotransmitter reuptake
movement of the transmitter molecule back into the presynaptic terminal thus terminating activity and allowing reuse
neurotransmitter degradation
enzymatic breakdown of released transmitter can terminate synaptic activity
postsynaptic receptor
antagonists can block the postsynaptic receptor, decreasing synaptic transmission (improvement can happen too)
presynaptic autoreceptors
serve as a method of negative feedback in controlling neurotransmitters release
membrane effects
alteration of membrane organization and fluidity modulate activity
T or F: presynaptic autoreceptors are always inhibitory
T!
what may occur following presynaptic drug actions?
increase or block NT synthesis
alter storage/package
facilitate or inhibit NT release
block NT reuptake
inhibit NT metabolism
what may occur following postsynaptic drug actions?
direct receptor agonists mimic NT
receptor antagonists block NT
contribute to up or down regulation
central nervous system drugs act on:
pre and post synaptic neurons
central nervous system drugs act by:
altering impulse propagation
altering NT synthesis, storage, release, reuptake, and degradation
altering NT binding and stimulation of post-synaptic surface receptors
T or F: a single neuron influences and is influenced by multiple other neurons.
T
what’s the difference between divergence and convergence
divergence: one neuron → multiple
convergence: multiple neurons → one
what are the drug effects that make up sedative-hypnotic and anti-anxiety drugs?
sedative: calming, reduces anxiety
hypnotic: induces sleep
anxiolytic: relieves anxiety without heavy sedation
___________ is the issue leading to pathophysiology issues like insomnia and anxiety.
hyper-arousal
what are the goals for using sedative-hypnotic to treat insomnia?
hasten sleep onset
lengthen time asleep
improve time in restful sleep
sedative-hypnotic drugs usually target the ______ and _______.
midbrain and brainstem
what are some risks seen when taking sedative-hypnotic drugs?
daytime sedation, confusion, delirium, falls, and dependency
T or F: sedative-hypnotic drugs are amongst the most commonly used and abused drugs worldwide.
T
describe the pharmacokinetics of sedative-hypnotic drugs.
lipophilic: readily absorbed, large Vd, and readily cross the blood-brain barrier
site of action: GABA-A or B receptors
termination of activity: liver metabolism
elimination: renal
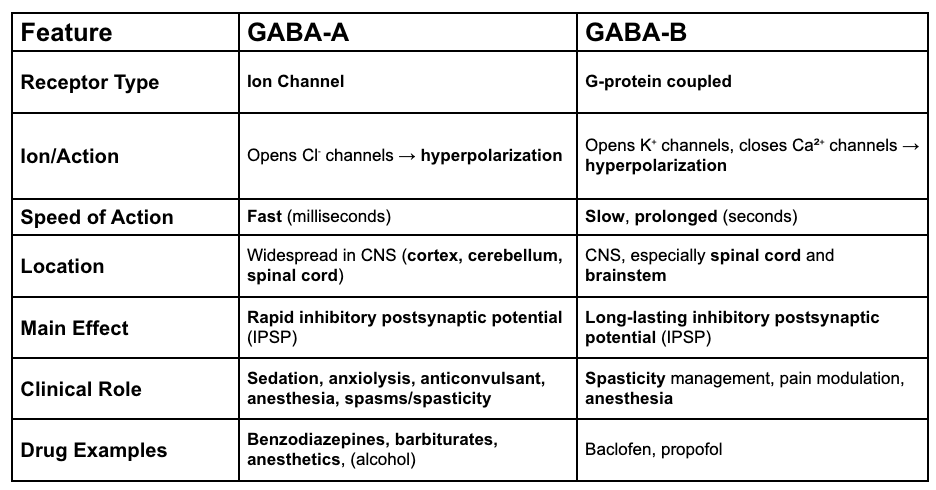
GABA A vs GABA B chart