respiration - compliance, FRC and respiratory volumes, resistance, and ventilation, work and breathing strategies
1/175
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
176 Terms
what counterbalances the surface tension's collapsing force on the lung?
the surfactant
what counterbalances the lung's elastic recoil's collapsing force on the lung?
the expanding force of the chest wall through its fluid attachment to the lung
why is the lung tissue elastic?
it has a connective tissue network composed of elastin fibers which form a meshwork throughout the lung and this tissue lays around and holds the alveoli together
--> fibers are in a pattern such that it can expand and recoil in the same manner each and every time an expanding force is applied to it
what is the minimal lung volume?
the lowest volume the lung will relax to in the absence of an extrinsic (either extrinsic or collapsing) force
in the lung, the change in pressure is _________ to the chain in volume
proportional
--> expressed in total lung capacity (TLC) and pressure required to expand the lung
what is total lung capacity?
TLC- the maximal volume of gas the lung can hold when inflated to its maximal volume
(usually a percentage, such that at residual volume TLC is ~10%)
what is residual volume?
the volume of air in the lung after maximal active expiration
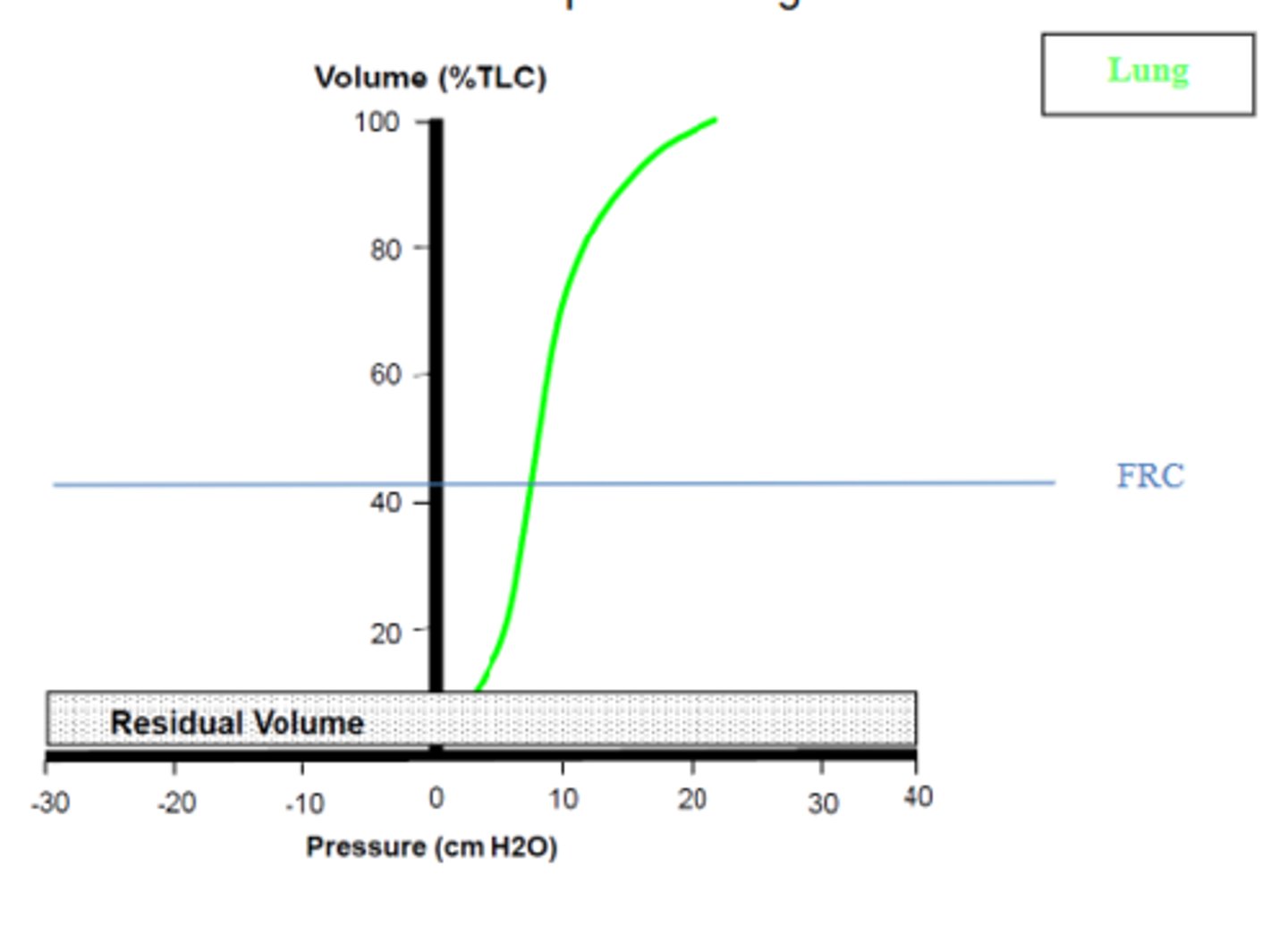
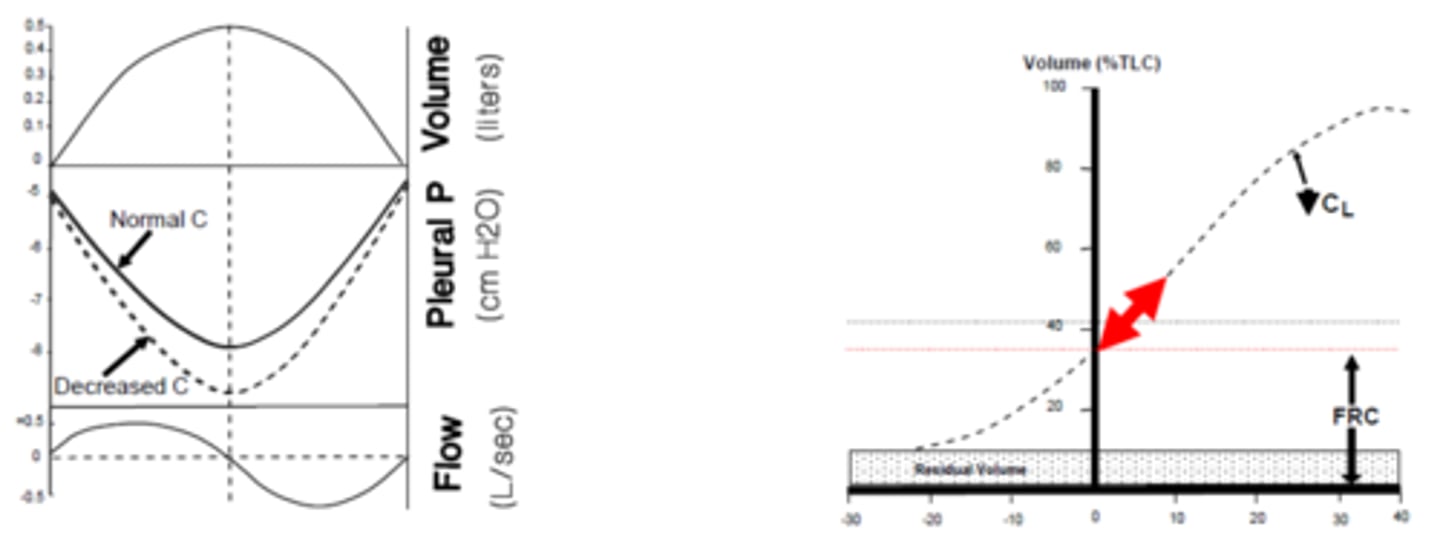
what is the pressure-volume relationship of the lung?
straightest part (30-40% TLC) -> lung is most compliant (requires the least change in pressure, easiest to inflate)
the "s" parts (10-40% TLC) and >70% TLC --> lung is least compliant
this slope is the compliance of the lung, Cₗ (change in volume of lung/change in alveolar pressure)
in volumes <100% TLC, when there is a pressure change, does the volume change as well ?
yes- when there is a pressure change there will be a volume change, due to the lung's compliance
a dog has a tidal volume, Vₜ of 400 ml and a pleural pressure, Pₚₗ that went from -5 cmH₂O at rest to -20 cmH₂O at the end of it's inspiration. what is the lung's compliance?
C = ΔV/ ΔP (ml/cmH₂O)
C = 400 ml/15 cmH₂O
C= 26.66 ml/cmH₂O
if a dog's tidal volume increases from Vₜ of 400 ml to 500 ml but it's change in Pₚₗ, 10 cmH₂O (from -5 to 15 cmH₂O) remains the same, is the lung exhibiting a greater or lesser compliance?
C = ΔV/ ΔP (ml/cmH₂O)
C = 400 ml/10 cmH₂O
C = 40 cmH₂O
C = 500 ml/10 cmH₂O
C = 50 cmH₂O
the lung is exhibiting a greater compliance, because it was able to expand even more without affecting its Pₚₗ
when is the largest pressure change required in inflation/deflation of the lung?
between residual volume and FRC (10%-40% TLC) and,
at volumes >70% TLC
--> these are where the lung is the least compliant
i.e. where pressure-volume relationship is A-shape
when during inflation/deflation is the lung the most compliant?
between 30%-70% TLC
--> is easiest to inflate the lung, requires the least amount of change in pressure
(this includes FRC @ ~40% TLC)
the net compliance of the lung is the combination of the major collapsing forces of the lung: ________ and _________
surface tension and elastic recoil
what is the normal compliance of a lung?
0.2 L/cmH₂O
the greater the compliance, the ________________ the lung complies to a distending force
easier
stiffening the lung _________ its compliance
decreases
--> necessitating greater expanding forces to inflate the lung
what is fibrosis? how does it affect compliance?
condition where connective tissue in lung produces an abnormally high [collagen fibers] which stiffen the lung and overpower the elasticity of the elastin fibers
--> results in decreased lung compliance
what is emphysema? how does it affect compliance?
condition where tissue damage occurs in some alveoli, causing them to collapse and form very large air pockets and r5eults in increased volume
--> results in increased lung compliance
why does the chest wall want to expand outward?
due to its own elastic recoil which is at a larger volume than usual
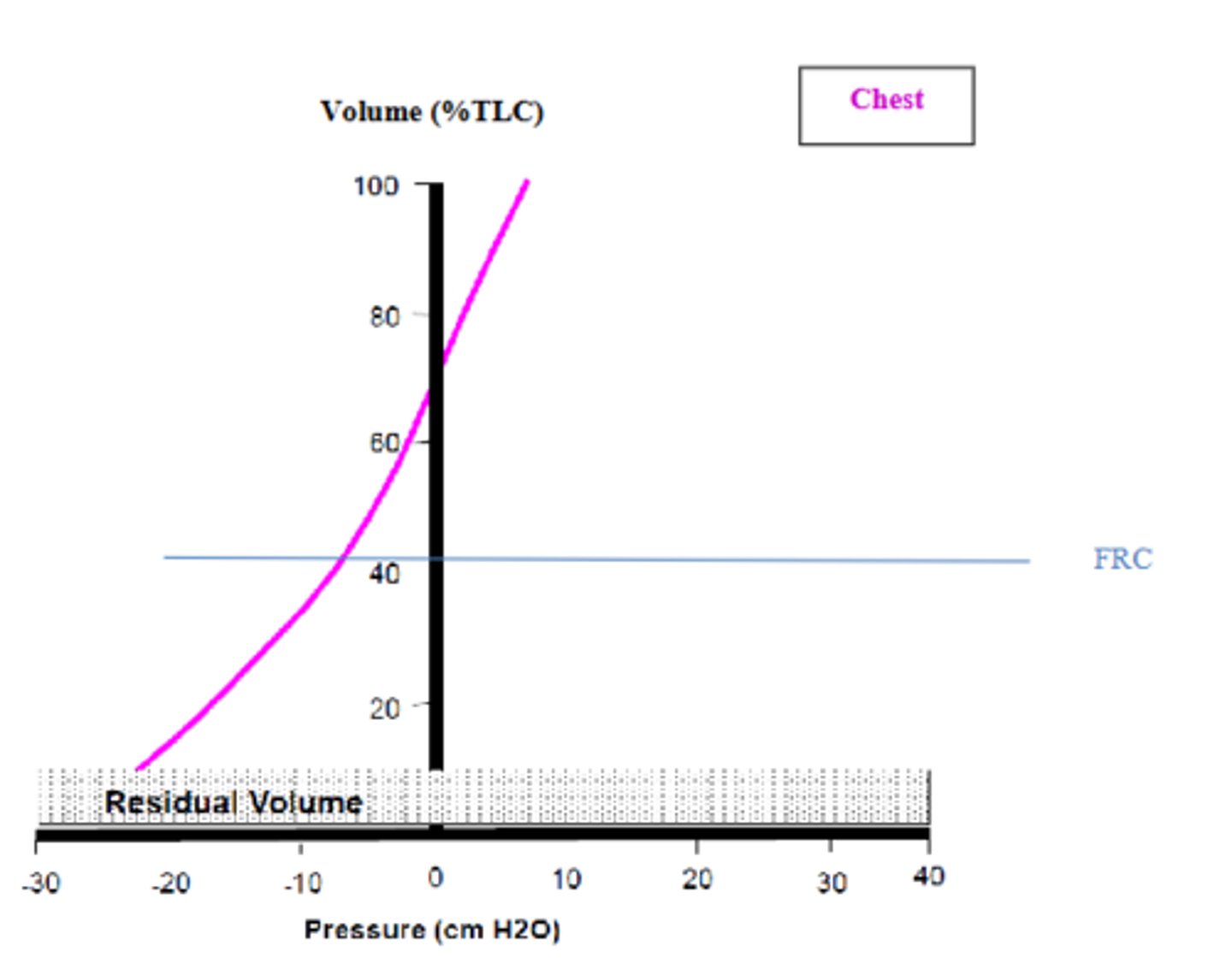
what is the pressure-volume relationship in the chest wall?
the chest's natural rest position is ~70% TLC (P=0 cmH₂O)
--> straightens at + above FRC (>40% TLC), such that negative pressure is required to deflate the chest wall volume below FRC (and has lower compliance below FRC)
slope is the compliance of the chest wall, C꜀ᵥᵥ (change in volume of chest wall/ change in transthoracic pressure)
what is the airway pressure, Pₐᵥᵥ?
the pressure measured in a respiratory system pressure-volume curve, which is dependent on the elastic forces of both the chest wall and lungs
at low lung volumes, airway pressure is very _________; at high lung volumes, airway pressure is very __________
low lung volume, Pₐᵥᵥ -> very negative
high lung volume, Pₐᵥᵥ -> very positive
what is required to expand the respiratory system (chest+lung) above FRC?
active inspiratory muscle contractions
--> deflation back down to FRC is passive
what is required to collapse the respiratory system (chest+lung) below FRC?
active expiratory muscle contractions
--> inflation back up to FRC is passive
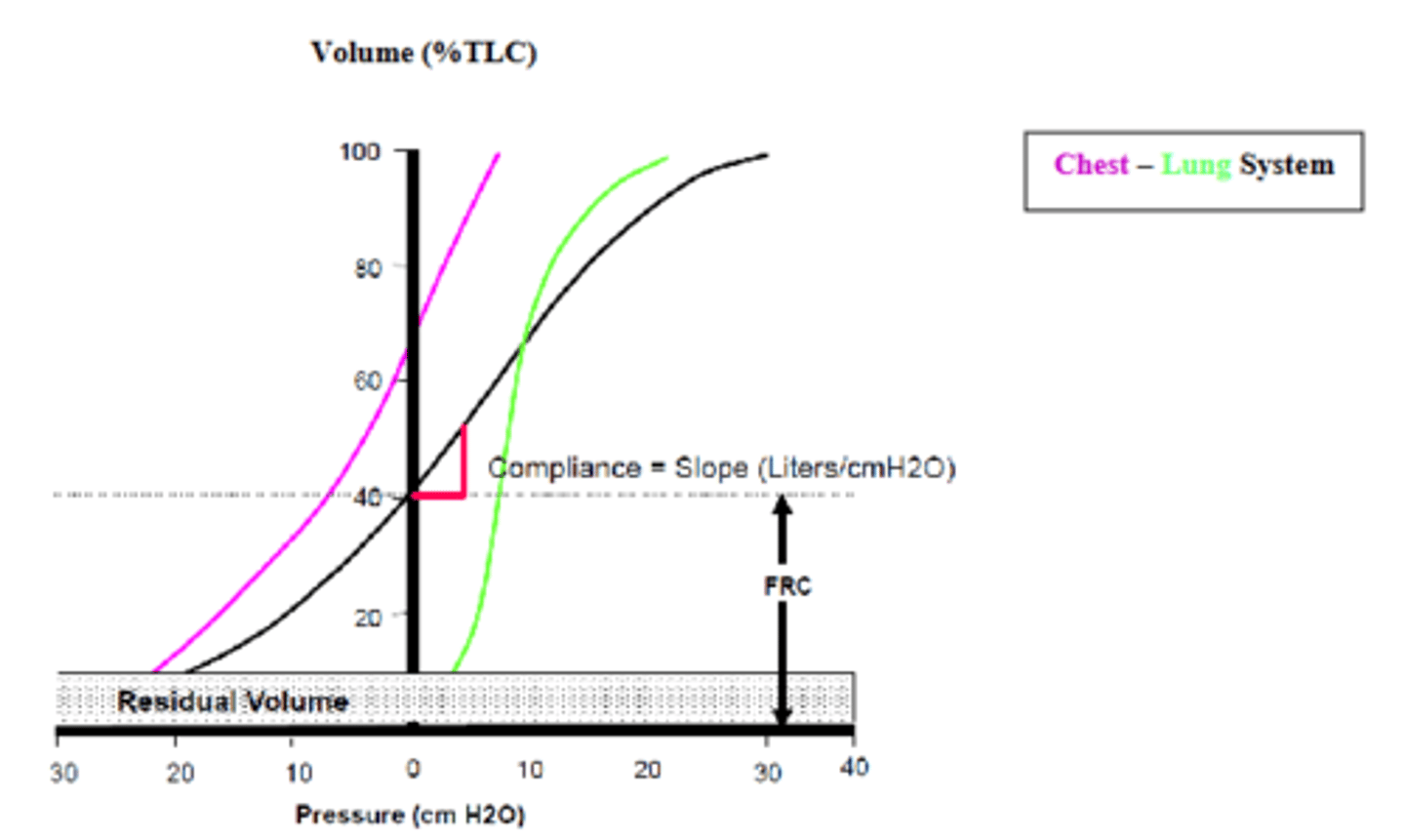
what is the total compliance of the chest-lung (respiratory) system, Cᵣ?
the slope of the pressure-volume curve
--> the ratio of the change in volume over the change in airway pressure (dependent on elastic forces of both chest wall + lungs)
compliance is a major factor determining tidal volume Vₜ and assoc. pleural pressure Pₚₗ
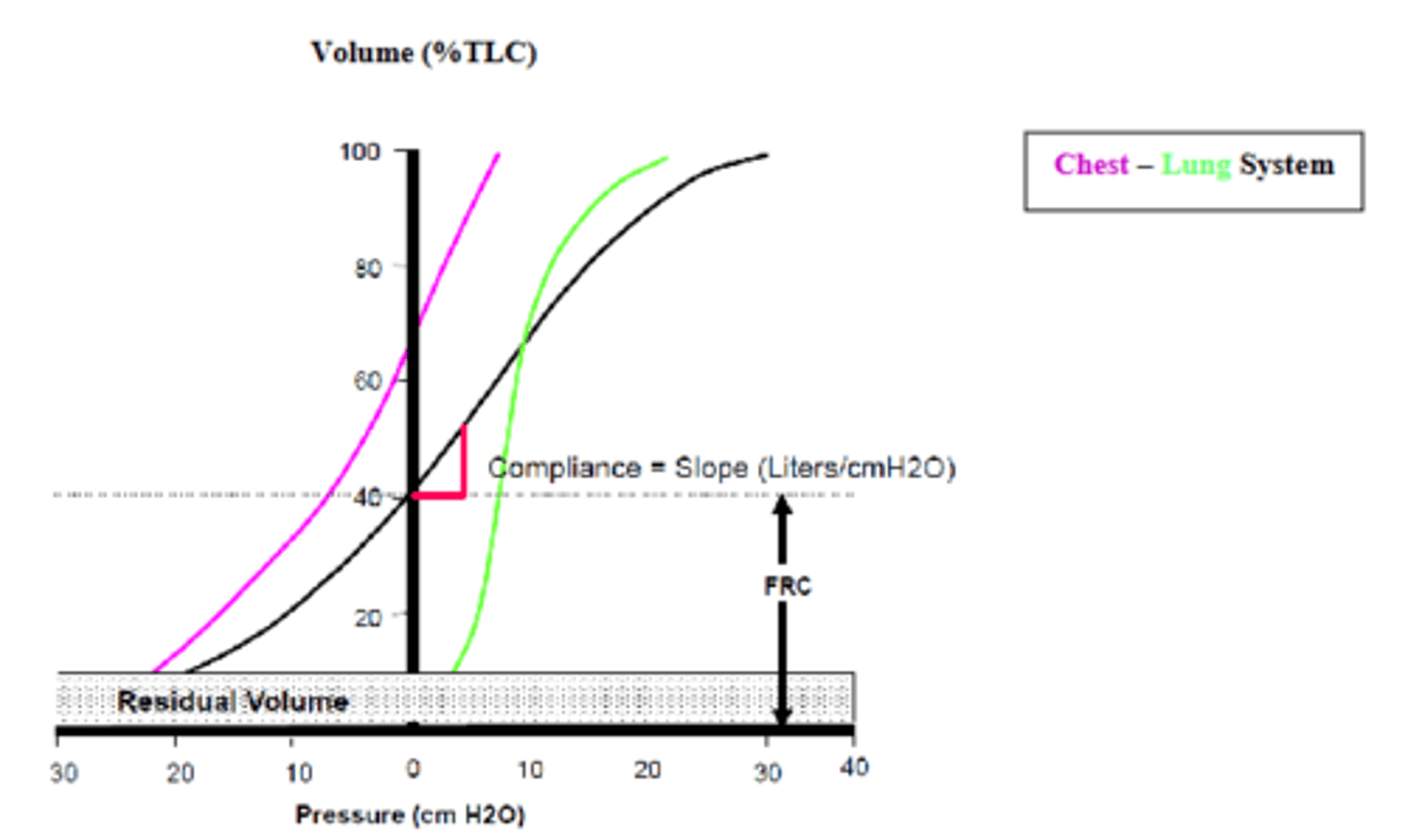
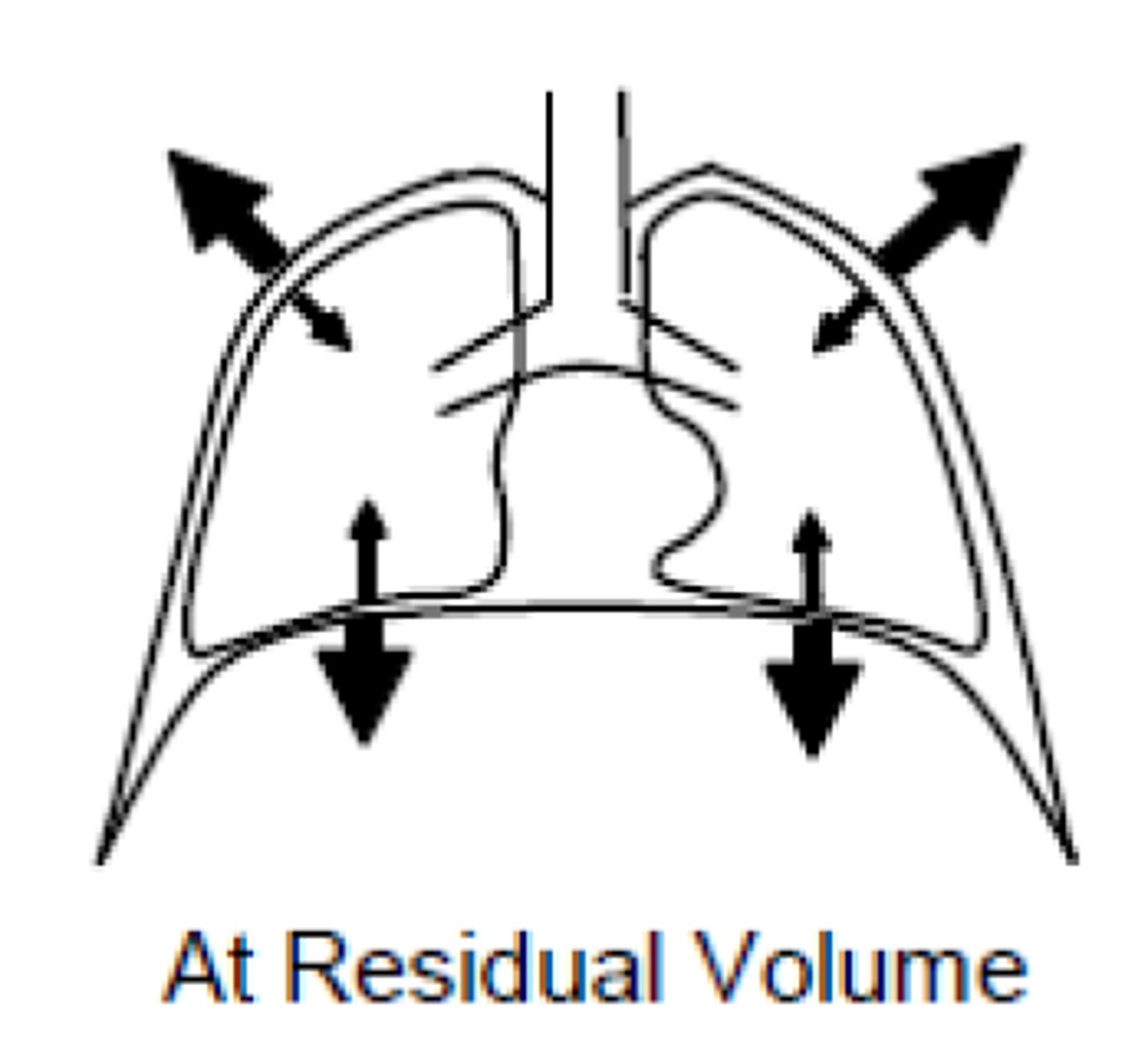
at residual volume what is the net expanding/collapsing force?
the net expanding force is exclusively due to the elastic recoil of the chest wall
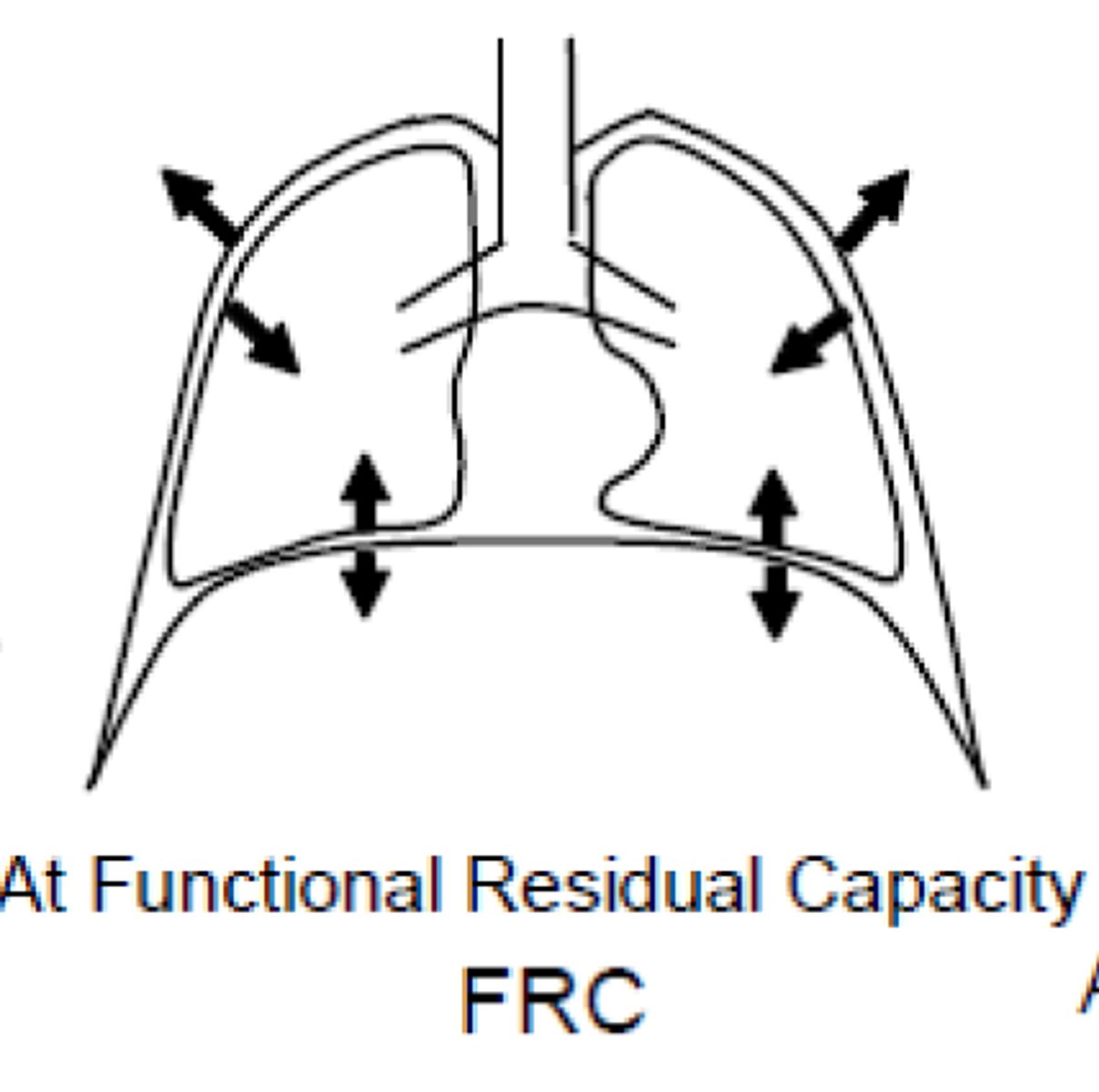
at FRC what is the net expanding/collapsing force?
the net expanding and collapsing forces are equal
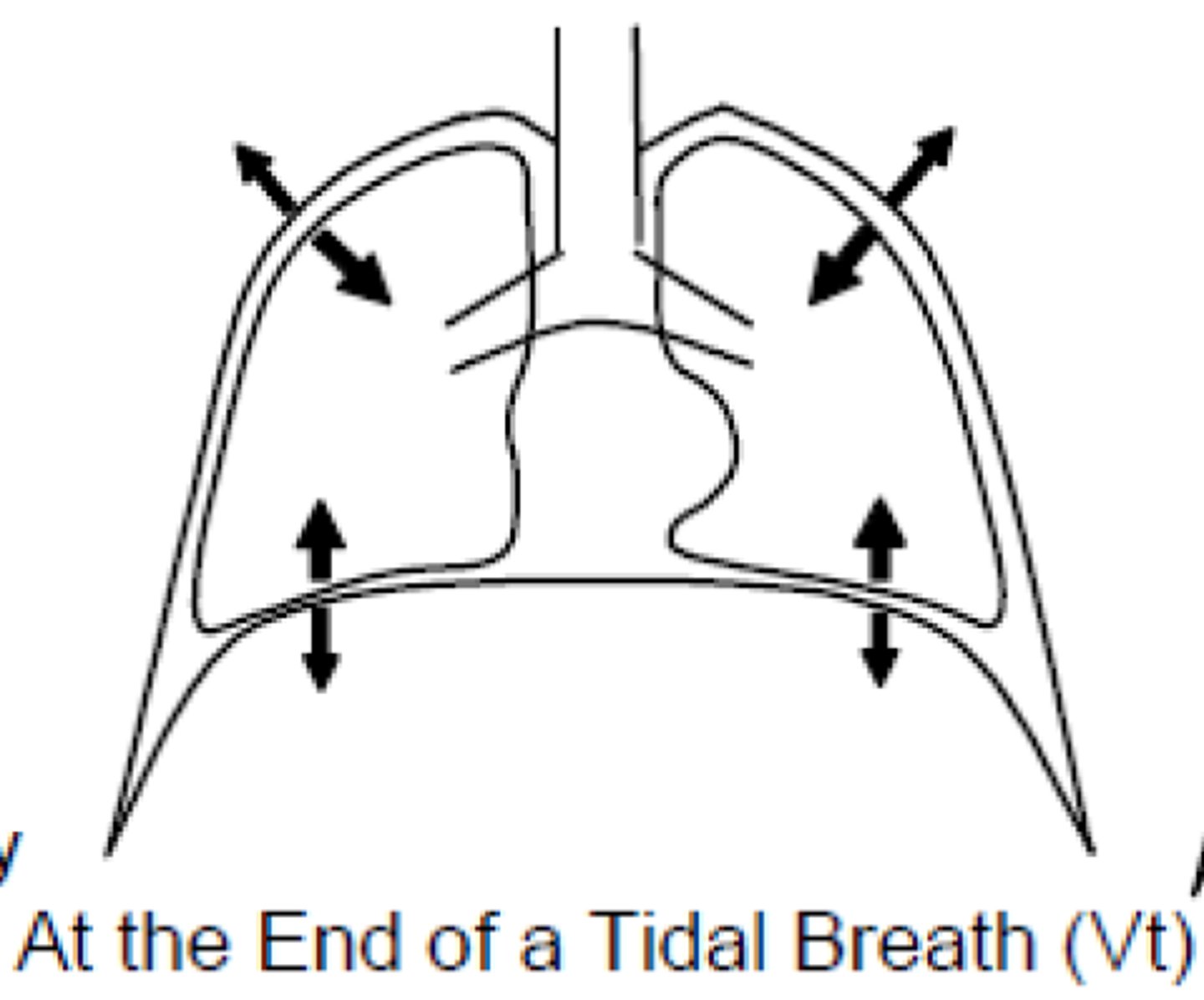
at the end of the a tidal breath, what are the expanding/collapsing forces?
the collapsing force of the lung is greater than the expanding force of the chest wall
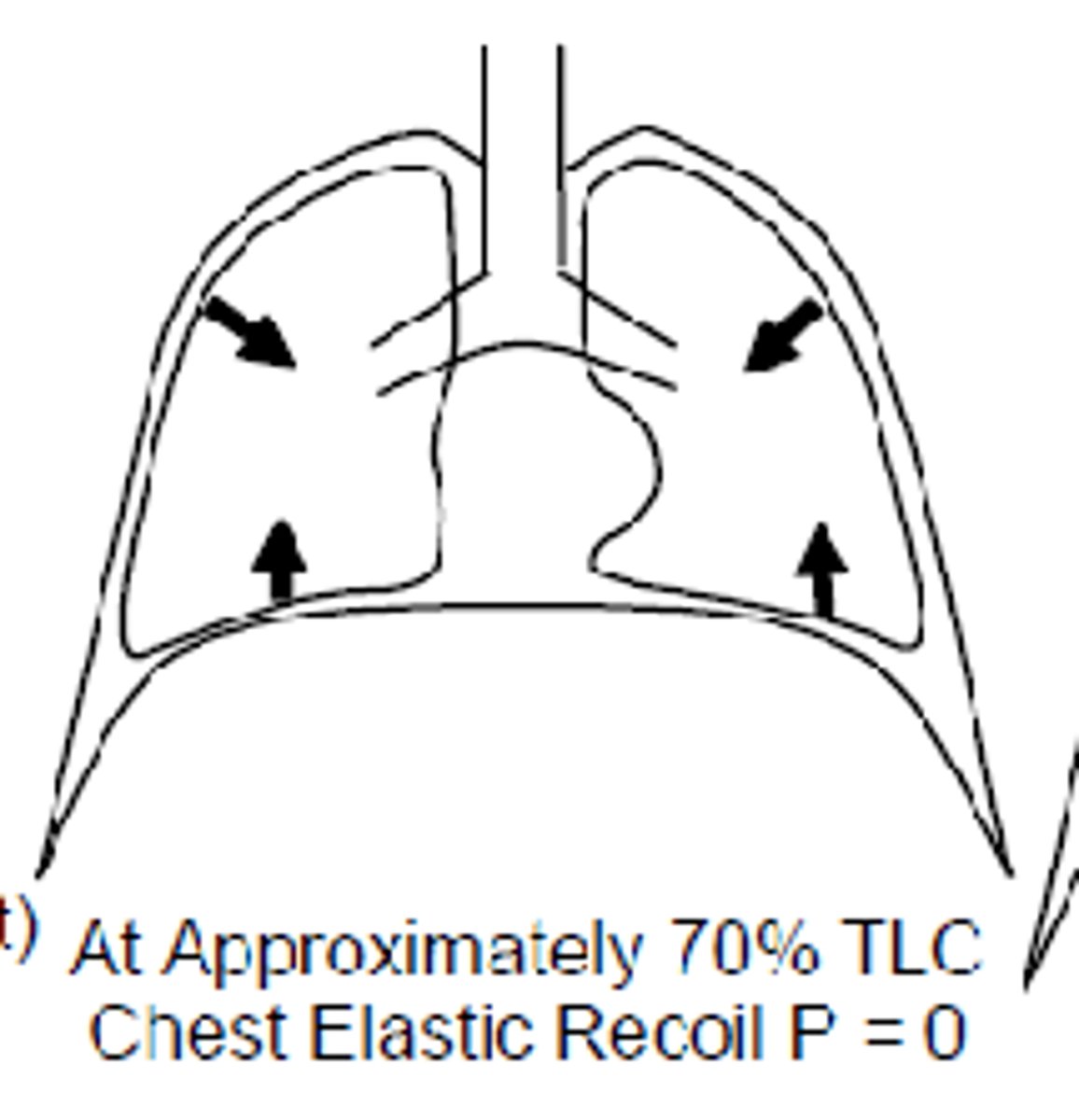
at 70% TLC, what is the net expanding/collapsing force?
there is a net collapsing force almost exclusively due to the lung
--> bc @ 70% TLC the chest wall would be in its rest position if not assoc. w the lung
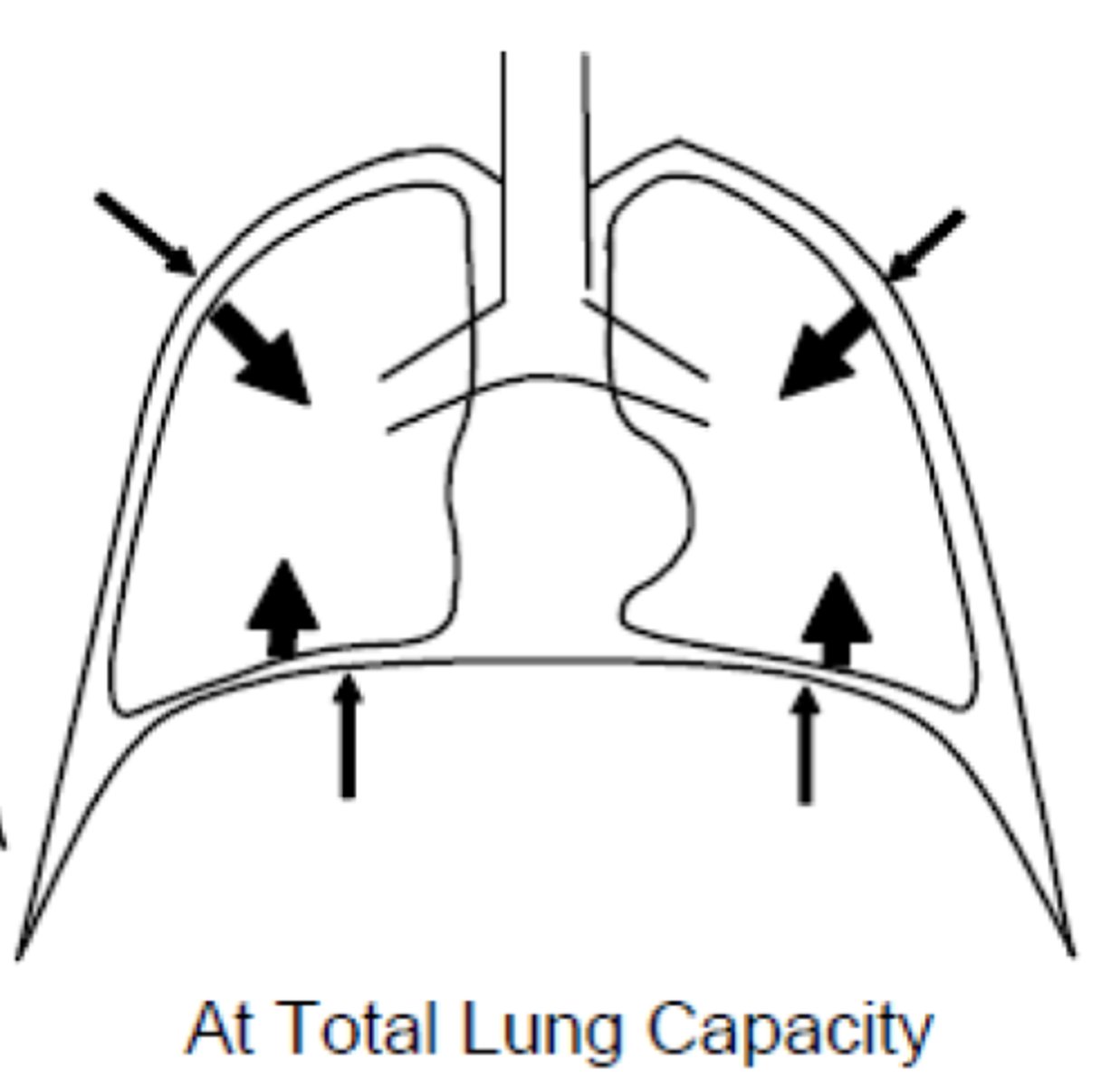
at 100% TLC, what is the net expanding/collapsing force?
there is a net collapsing force mostly due to the lung, but also the chest wall bc it has excessed its resting recoil volume
--> both chest wall & lung want to collapse
where should lung compliance be calculated on pressure-volume urve?
on the linear portion, approx. 40-70% TLC
how do you calculate lung compliance?
measure the change in volume (tidal volume, Vₜ) and divide by the change in pressure when airflow is zero (prior to inflation and at the very end of inflation)
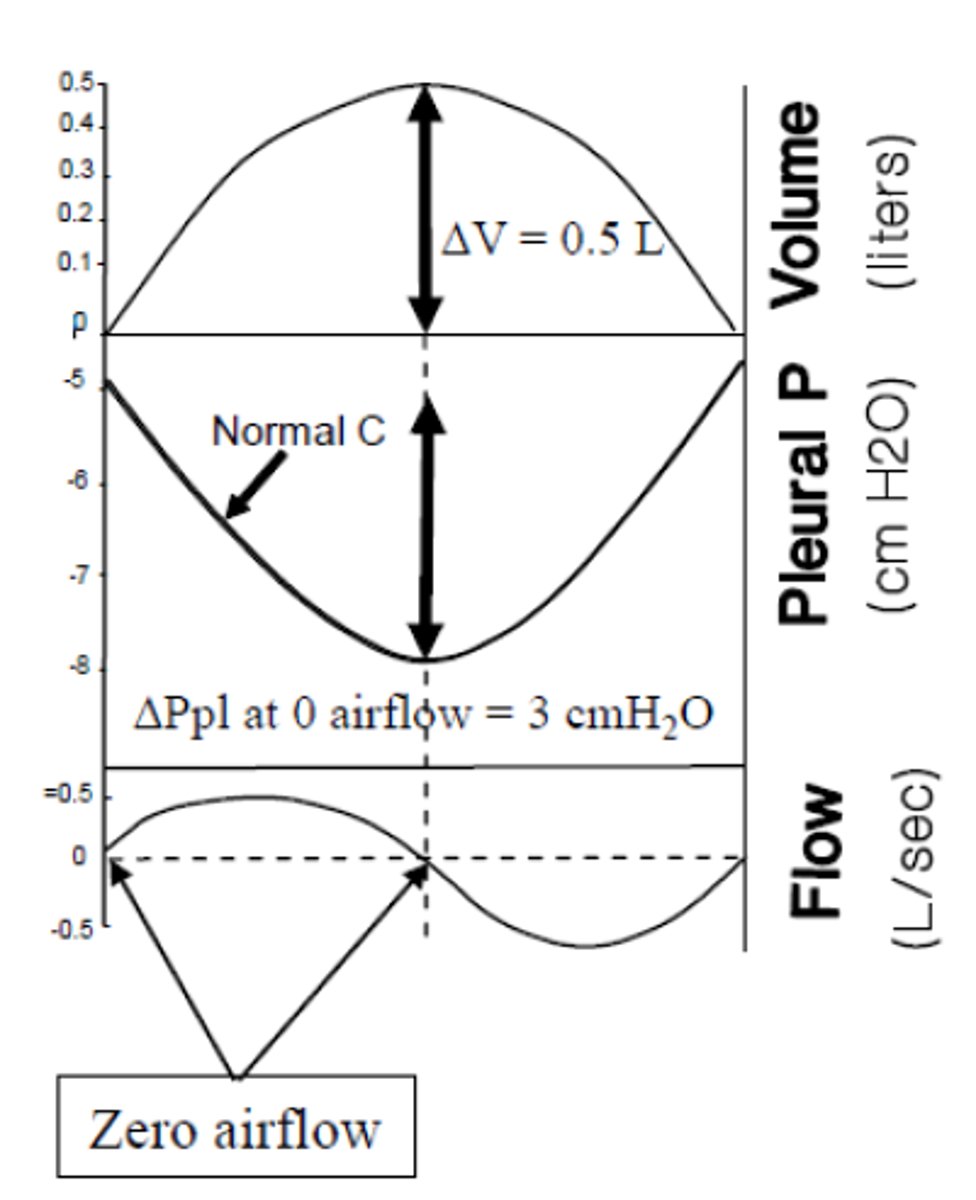
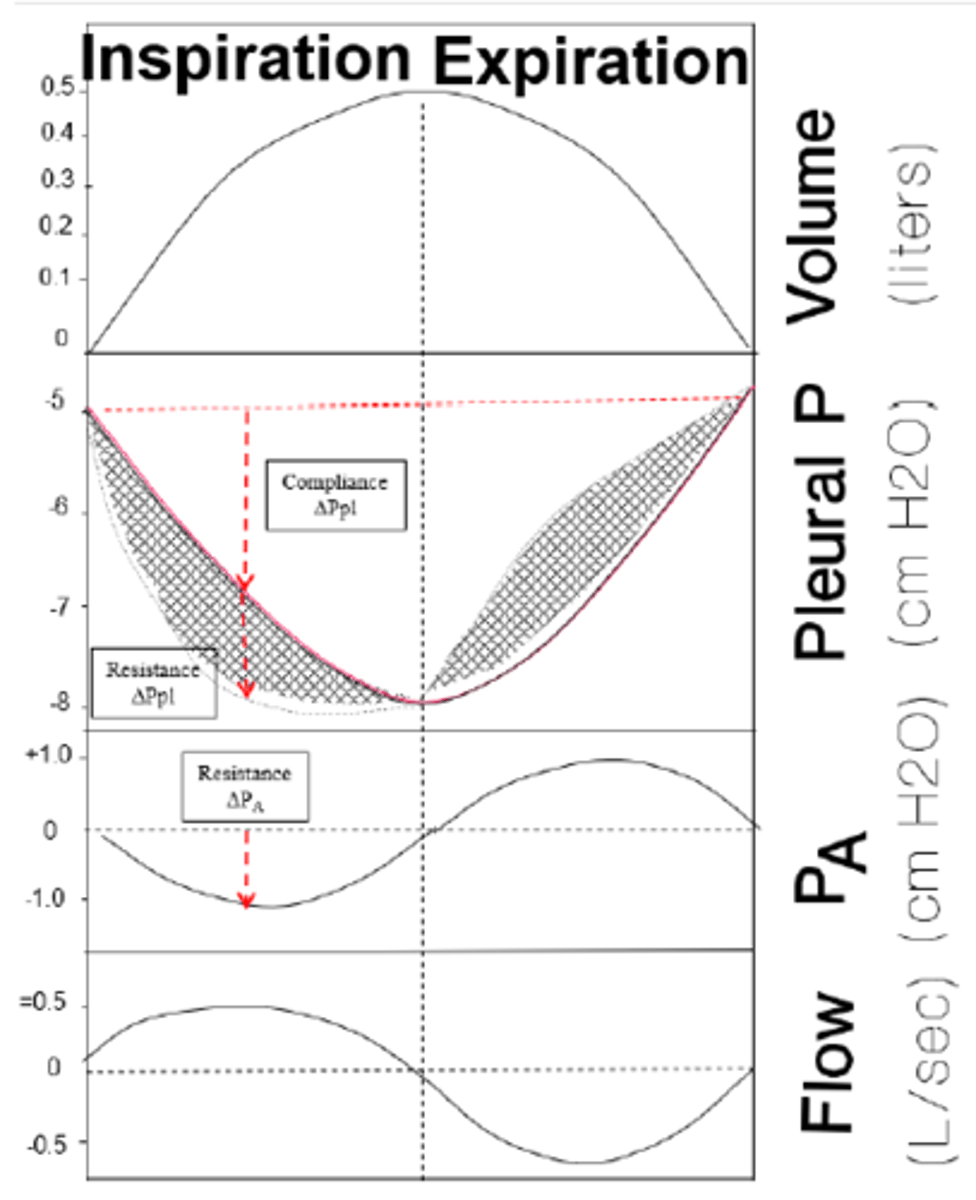
the pleural pressure, Pₚₗ measured during the breathing cycle results in a curve that represents the force necessary to do what two things?
1) overcome the elastic properties of the respiratory system
2) change the lung volume
when a lung becomes looser and more elastic, what happens to its compliance?
it has increased compliance
--> and thus a weaker collapsing force than a typical lung, so the expanding force of the chest wall overcomes the lung's collapsing forces so FRC increases as well
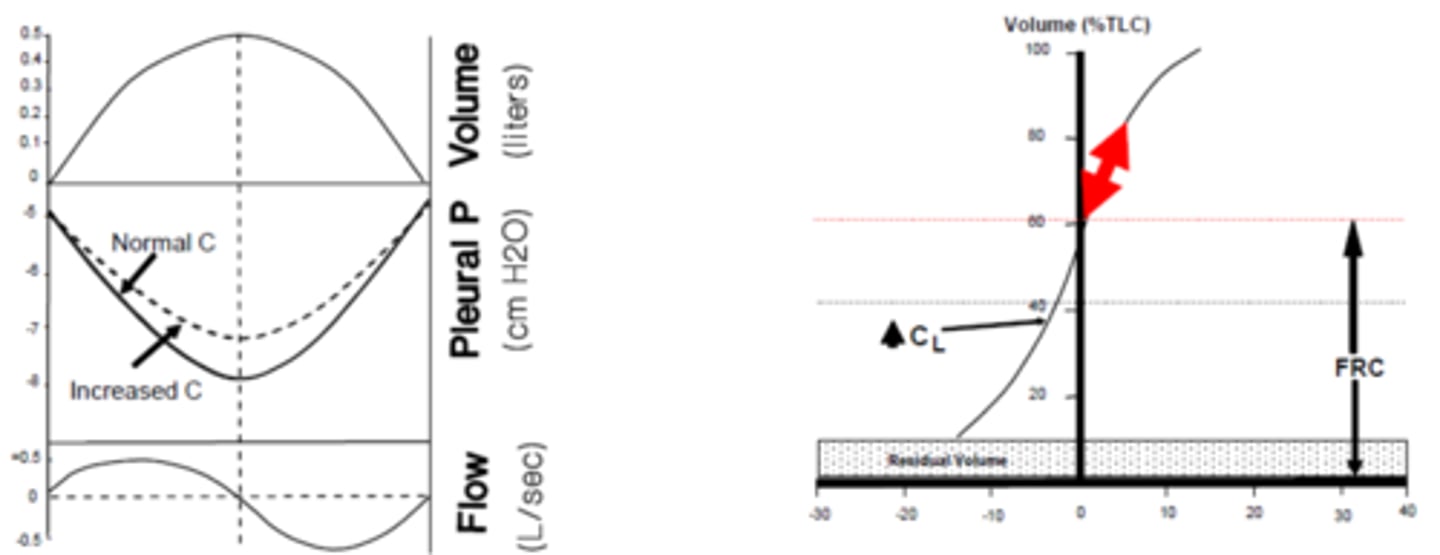
since FRC increases w/ increased lung compliance, what are the ramifications?
-less pressure is required to achieve the same volume change
-it is difficult to increase lung volume (FRC is @ a higher lung volume)
-at higher FRC, diaphragm is at a mechanical disadvantage bc inspiration occurs above FRC, when there is already more volume in the lungs and its contraction does not lift rib cage as effectively
emphysema is a classic example of a condition in which lung compliance _________
increases
--> large air sacs form in lungs as a result of tissue damage
--> diaphragm contraction upon inflation does not lift the rib cage as effectively (lost advantage of flattening from a dome shape)
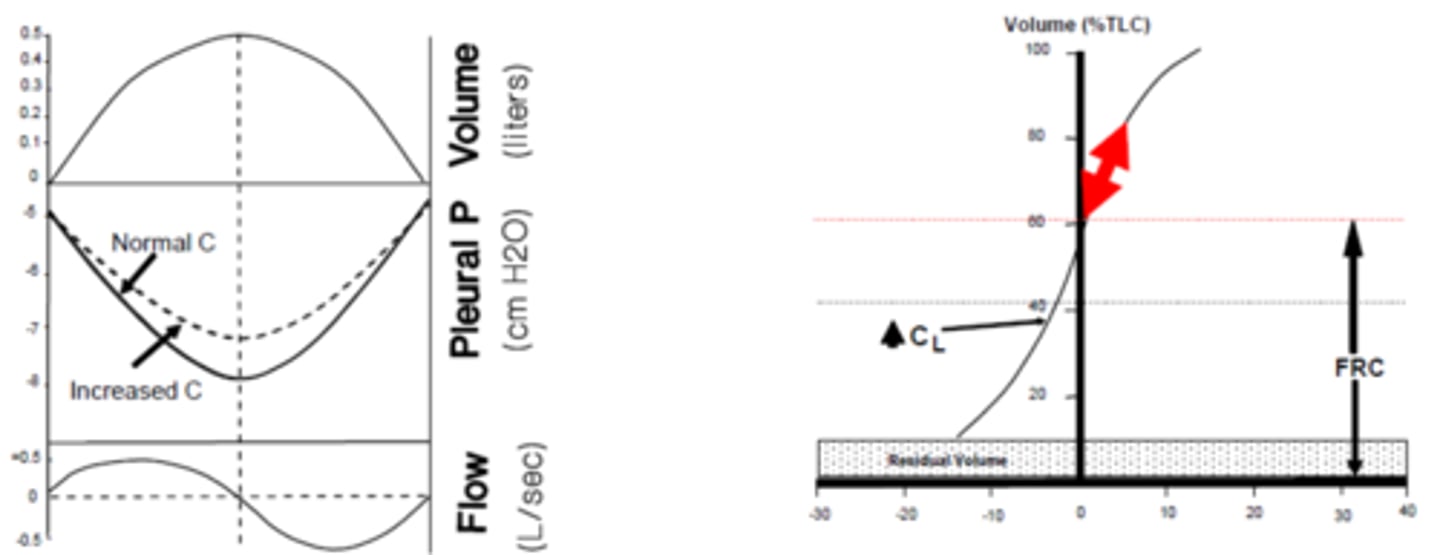
when a lung becomes stiffer and less elastic, what happens to its copliance?
it has decreased compliance
--> it has a stronger collapsing force than a typical lung, which pulls the chest wall down to a lower volume before FRC is reached (decrease in FRC)
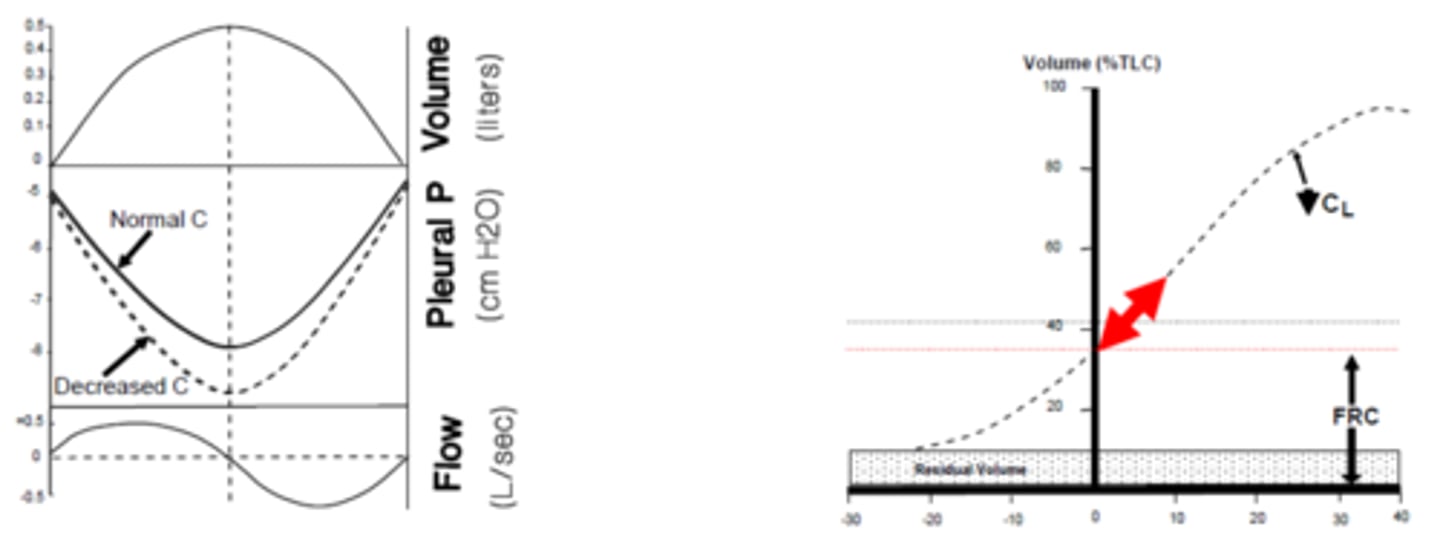
since FRC decreases w/ decreased lung compliance, what are the ramifications?
-greater pressure is required to achieve the same volume change (respiratory pump must use more force & energy)
-FRC is lowered so functional residual volume is lessened as well
i.e. fibrosis (unable to fully treat unless a lung transplant; just make animal comfortable)
fibrosis is a classic example of a condition in which the lung compliance is _________
decreased
--> inc. production of collage fibers in lung tissue decrease overall elasticity of the tissue
what is FRC?
the functional residual capacity
--> the air volume of the lung at rest when expanding and collapsing forces of respiratory system are equal and alveolar pressure is equal to barometric pressure
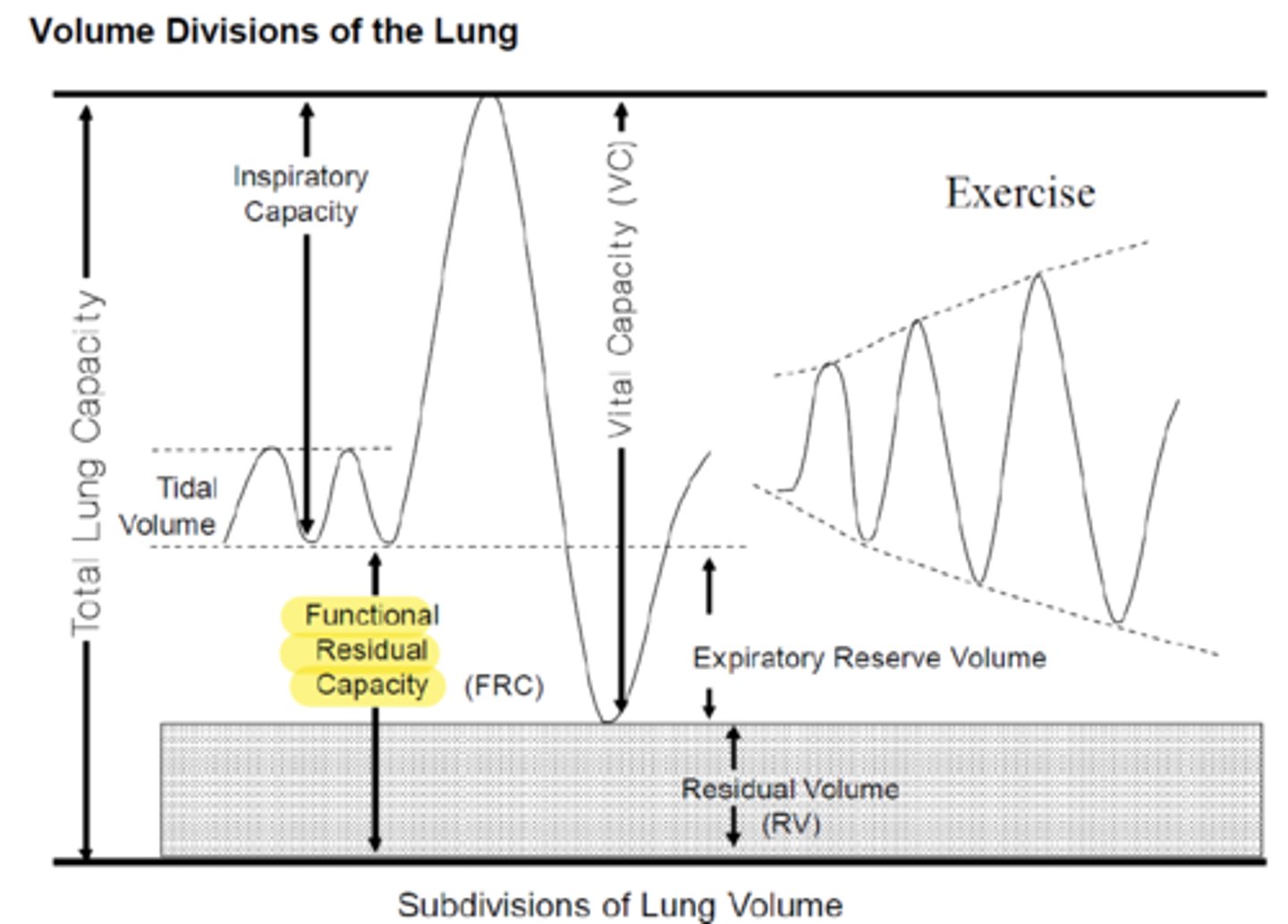
what is RV?
the residual volume
--> the volume of air remaining in the lungs after maximal active expiration
RV = FRC-ERV
(residual volume = functional residual capacity - expiratory reserve volume)
RV = TLC- VC
(residual volume = total lung capacity - vital capacity)
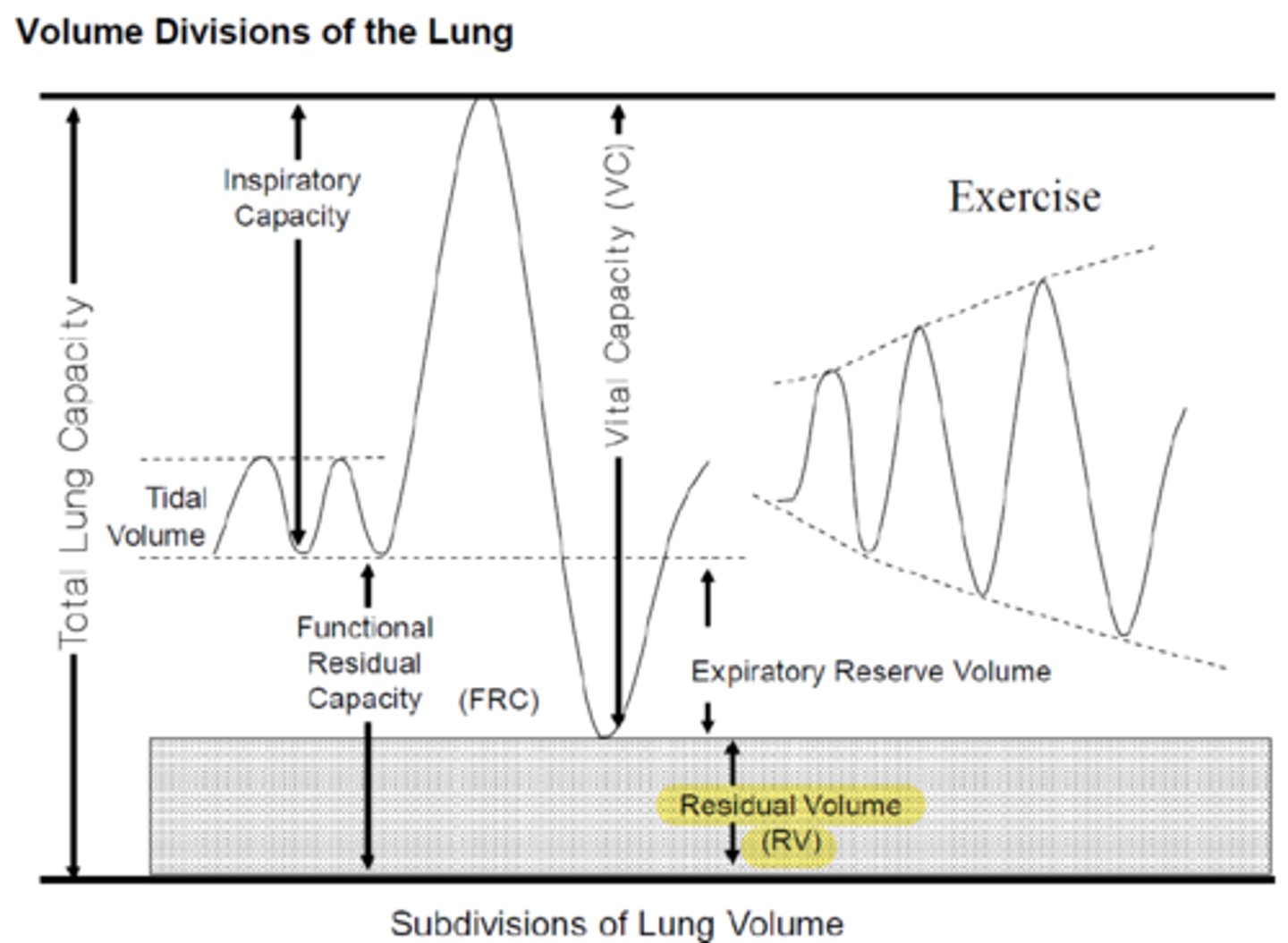
what is ERV?
expiratory reserve volume
--> the volume of air that can be forcibly exhaled
ERV= FRC-RV
(expiratory reserve volume = functional residual capacity - residual volume)
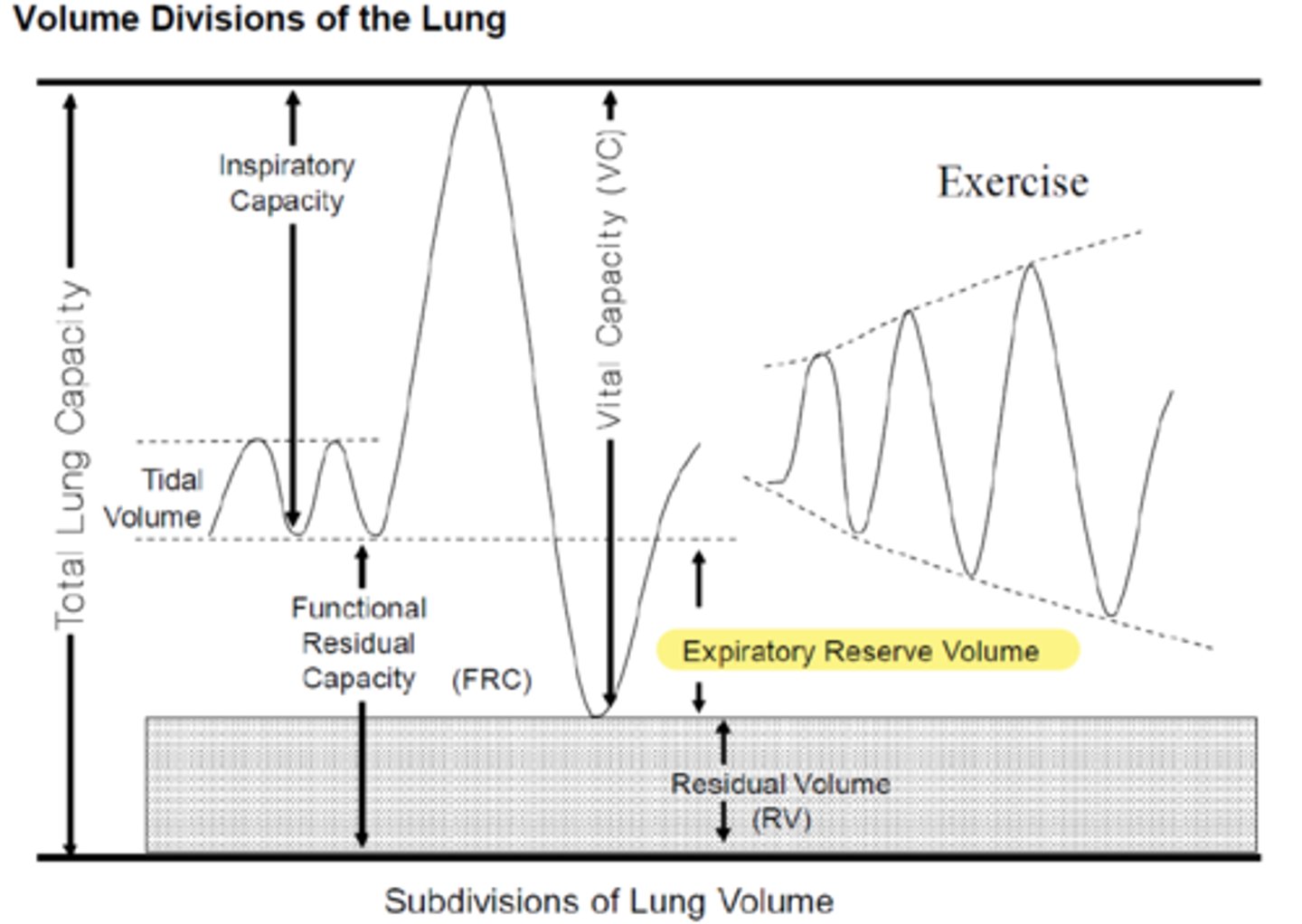
what does FRC = RV + ERV mean?
the functional residual capacity FRC is the sum of the residual volume RV and the expiratory reserve volume ERV
what is IC?
inspiratory capacity
--> the maximum volume of air inhaled from FRC to TLC
IC = VC - ERV
(inspiratory capacity = vital capacity - functional residual capacity)
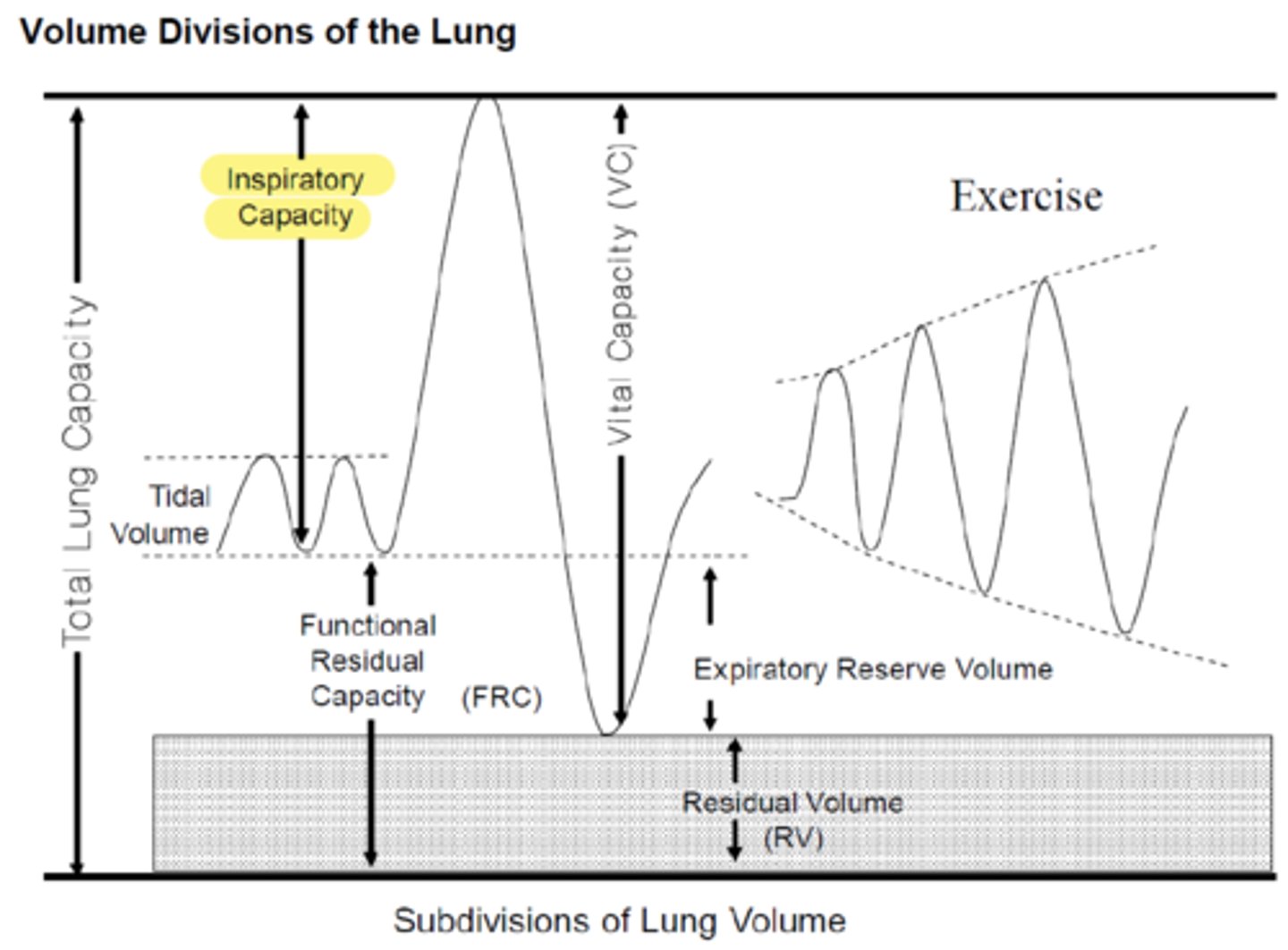
what is VC?
vital capacity
--> the air volume of the lung from residual volume to maximal volume; the maximum amount of air that can be moved in and out of the lungs
VC = IC + ERV
(vital capacity = inspiratory capacity + expiratory reserve volume)
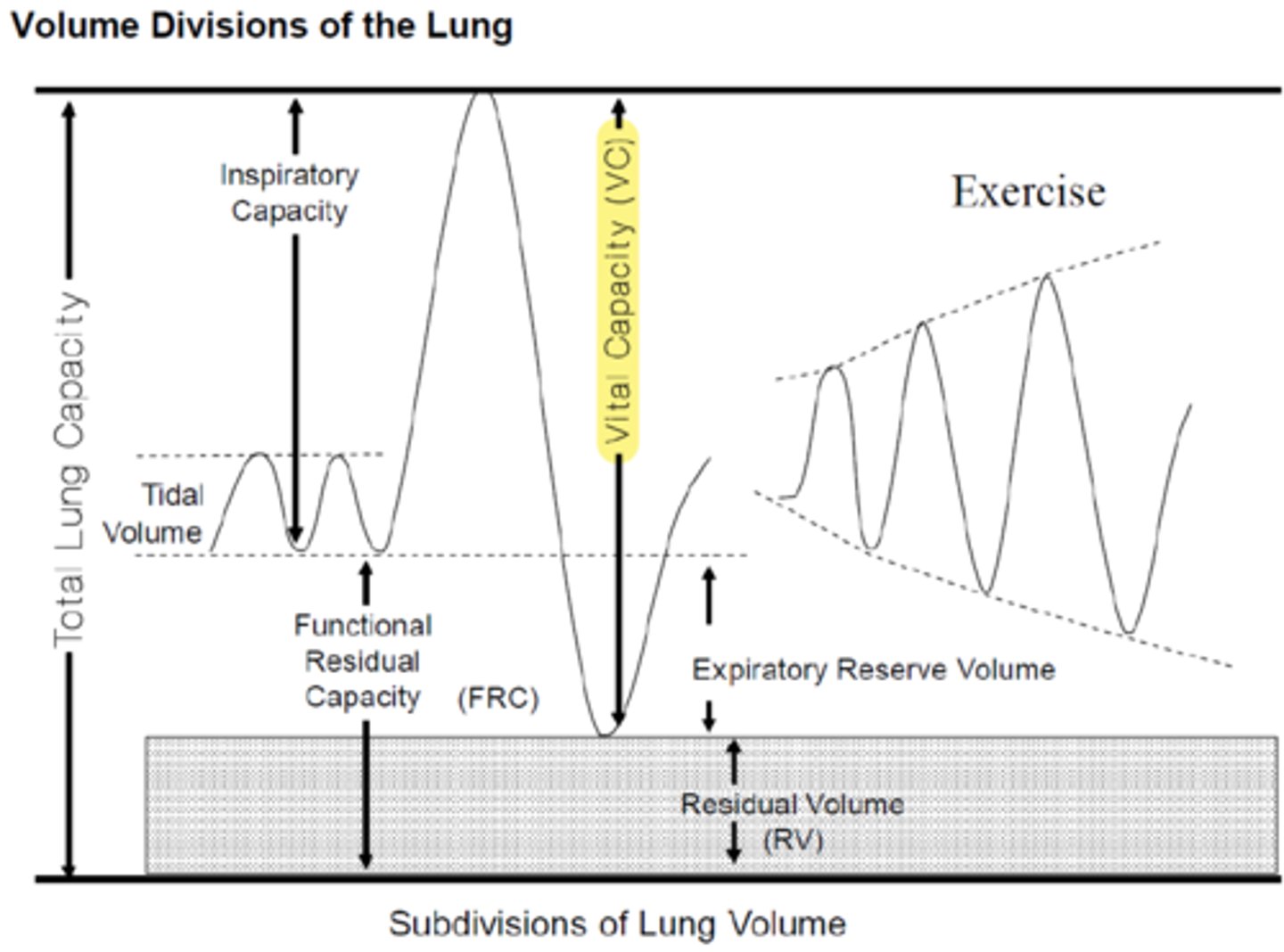
how does TLC differ from VC?
TLC -> measures air volume from minimal (completely empty) to maximal (completely full), but it is functionally impossible to deflate a healthy lung all the way to completely empty b/c the rib cage only compresses so far (may be possible in severe pneumothorax)
whereas in VC, it measures the air volume from residual volume to max
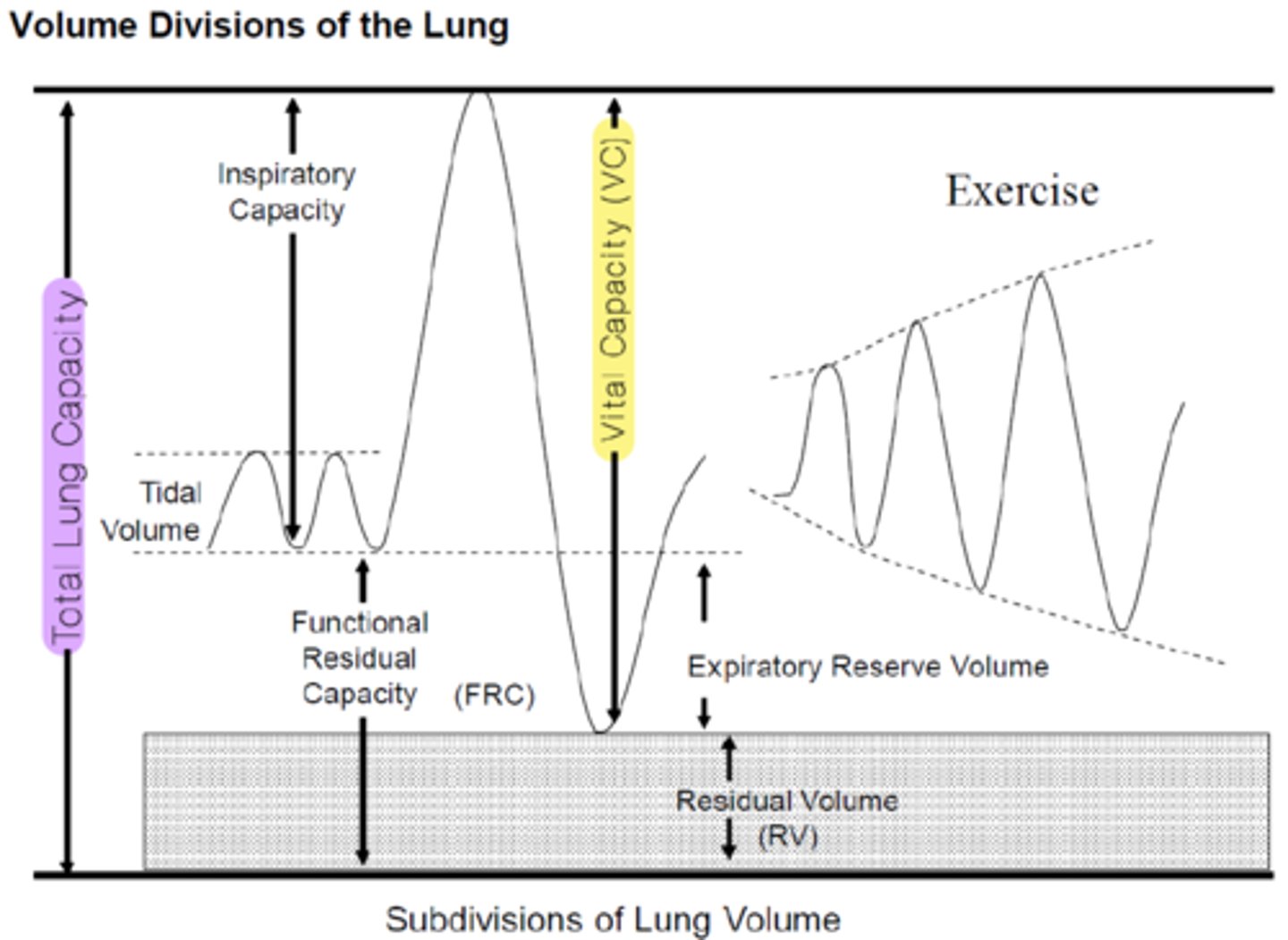
if a lung has decreased compliance, how are the other parameters affected? (IC, VC, FRC, ERV, RV)?
stiffer lung can not expand as much as a healthy lung, so IC & VC are reduced
stiffer lung exerts a stronger collapsing force so FRC, ERV, and RV are decreased
the total lung capacity decreases as well
if a lung has increased compliance, how are the other parameters affected? (IC, VC, FRC, ERV, RV)?
a stretchable lung exerts a weaker collapsing force, so FRC, ERV, and RV are increased
a stretchable lung inflates from a higher volume FRC, so IC and VC are reduced
what is the lung's rest positoin?
at minimal volume
(this is lower than residual volume, as minimal volume can only be reached if there is no expanding force of the chest... the "deflated balloon")
what is the chest wall's rest position?
at ~70% TLC
(if there is no lung collapsing forces, the chest wall would be at this position)
lung compliance is the slope of the _______ pressure-volume curve, whereas chest wall compliance is the slope of the ________ pressure-volume curve
lung compliance -> lung (alveolar) pressure-volume
chest wall compliance -> transthoracic pressure-volume
end compliance, FRC and respiratory volumes...... start resistance, and ventilation,
------
gas exchange only occurs at one place in the lungs- where?
the alveoli
--> bc there is a thin membrane that allows for gas exchange; there are no cartilaginous rings or smooth muscle b/w the alveoli and capillaries like there are in the bronchus/bronchioles
what is resistance?
the opposition to air flow; affects the rate of airflow
--> can be elastic resistance due to moving lung tissue and be related to 1) compliance and 2) tendency of lung to collapse when lung volume is increased above FRC
--> can be airway resistance due to properties of the tubes which oppose movement of air through them
the airway resistance is dependent on what 5 parameters?
1) the rate of airflow
2) the driving pressure
3) the diameter of the tube
4) the length of the tube
5) the viscosity (or density) of the gas
what is Poiseuille's law?
V̇ = [π(P₁ -P₂)r⁴]/[8ηl]
where:
V̇ = airflow
(P₁ -P₂)= pressure gradient
r = diameter of the tube
η = viscosity
l = length of tube
how is resistance, R measured?
R = (P₁ -P₂)/V̇ = 8ηl/πr⁴
where:
V̇ = airflow
(P₁ -P₂)= pressure gradient
r = diameter of the tube
η = viscosity
l = length of tube
compared to the cardiovascular system, what parameter of resistance is not as important for the respiratory system?
the viscosity/density
--> respiratory is gas, CV is blood which can vary its properties
when airflow is high there is a ______ resistance or a ______ pressure difference
a low resistance or a high pressure difference
i.e. in Poiseuille's law, V̇ = [π(P₁ -P₂)r⁴]/[8ηl], the nominator is greater
![<p>a low resistance or a high pressure difference</p><p>i.e. in Poiseuille's law, V̇ = [π(P₁ -P₂)r⁴]/[8ηl], the nominator is greater</p>](https://knowt-user-attachments.s3.amazonaws.com/14b444f7-c35e-4600-8d1b-c88c8218d4d3.jpg)
airflow decreases as radius __________
decreases
i.e in Poiseuille's law, V̇ = [π(P₁ -P₂)r⁴]/[8ηl], the nominator decreases
what is cross-sectional area?
the area of the opening within an airway passage
πr²
the greater the cross-sectional area, the _______ the airflow and the ______ the Rₐᵥᵥ
greater the airflow and the lower the Rₐᵥᵥ (airway resistance)
where is the major airway resistance?
in the proximal, large airways
--> bc although they have a larger diameter, they have a smaller total cross-sectional area compared to the smaller airways down the respiratory tree
in the distal airways, the diameter of the tubes are getting smaller. how is the airflow affected?
although the diameter of individual tubes is decreasing and each individual tube resistance increases, the total cross-sectional area (of all the tubes) is increasing so there is a lower total resistance
--> airflow is lower
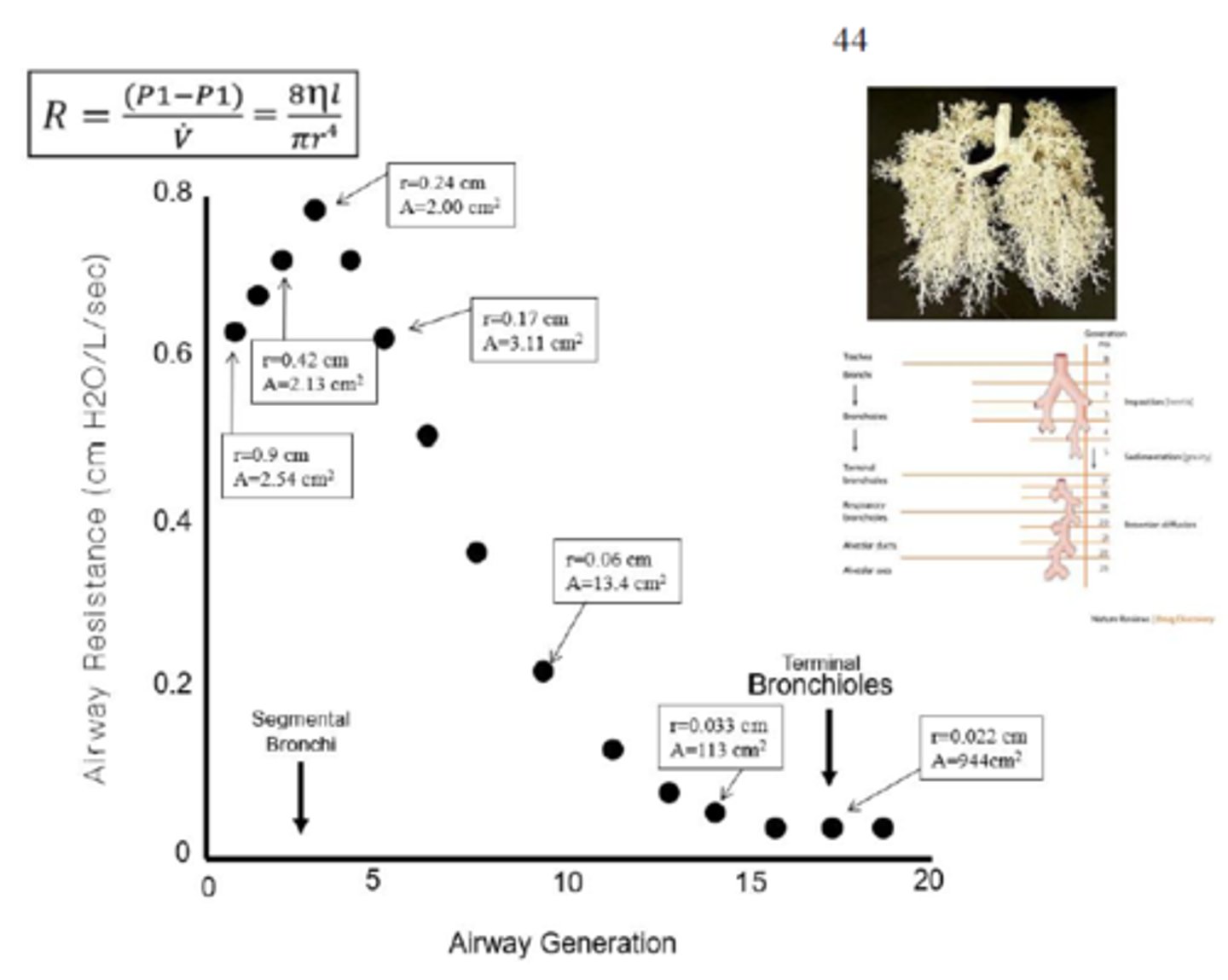
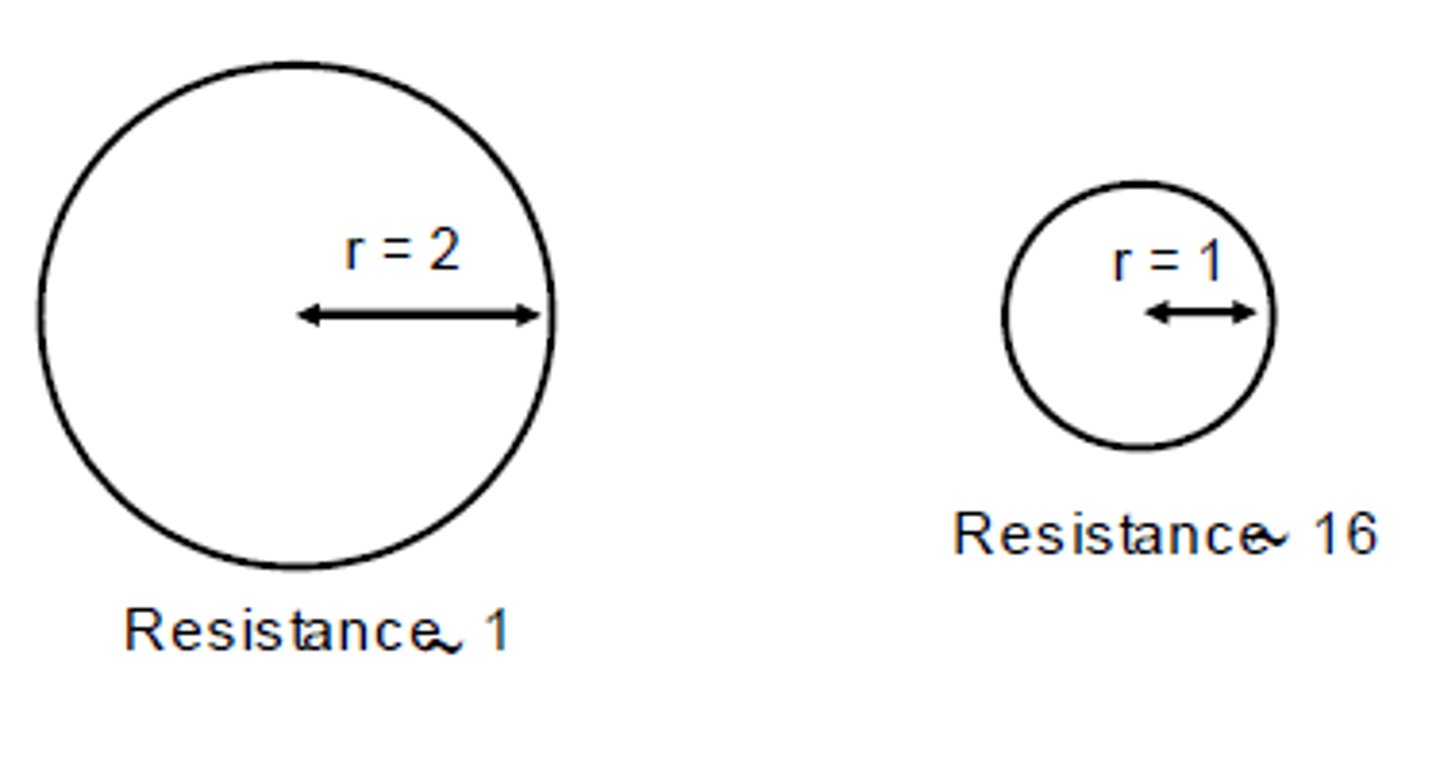
the smaller the diameter of the tube, the _____ the airway resistance of that tube
greater
b/c in R = 8ηl/πr⁴, smaller denominator
i.e. breathing through a straw vs breathing through a pipe
the more viscous and dense a material is, the _______ resistance it will meet travelling through a tube
greater
R = 8ηl/πr⁴, greater nominator
(this is bc of increased friction b/w molecules of material & molecules of tube)
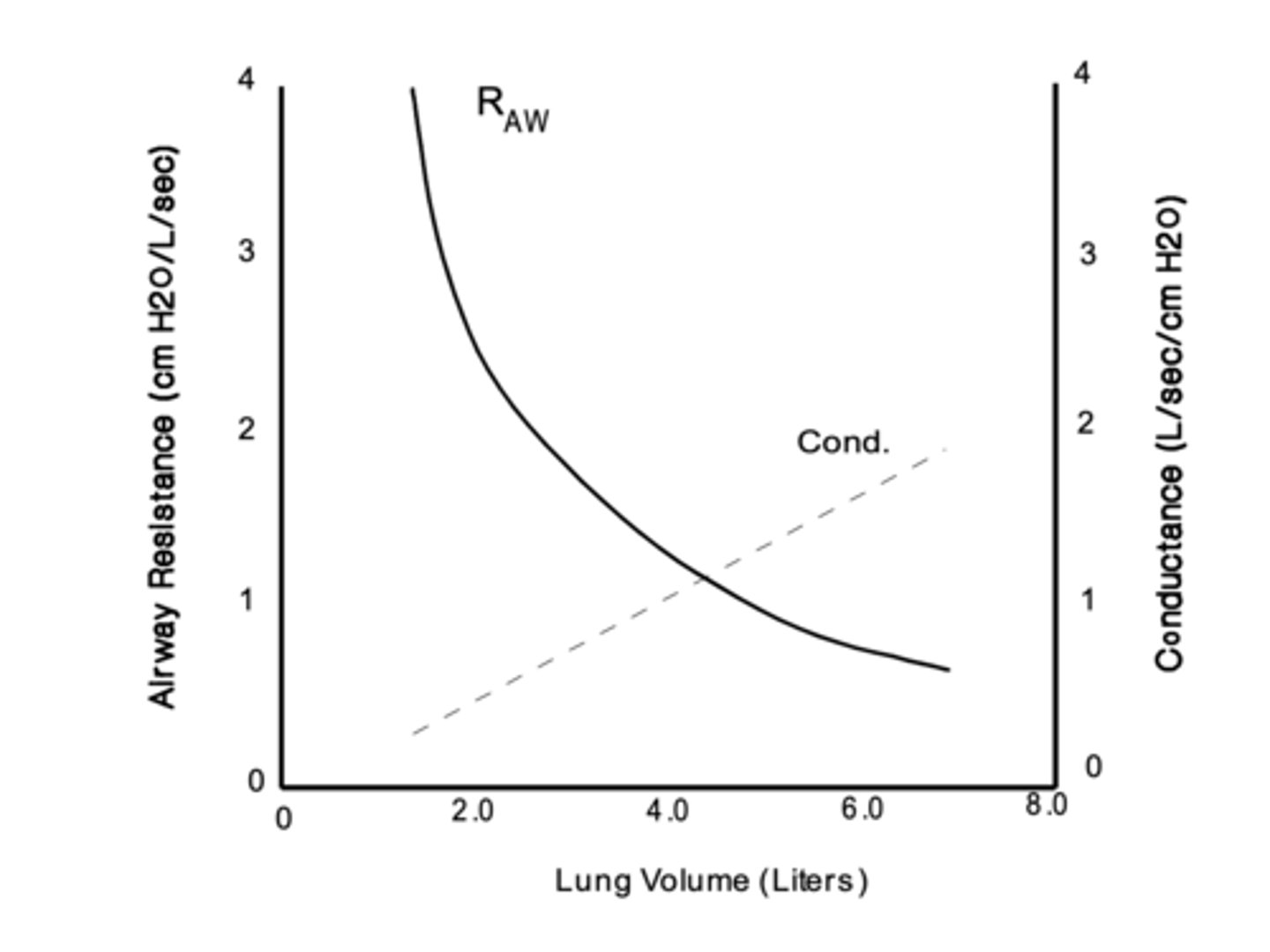
total airway resistance varies w/ changing lung volume. so, as lung volume increases, what happens?
radii of the individual bronchioles increase so tube resistance and total airway resistance both decrease w/ increasing lung volume
overcoming airway resistance requires a sufficient driving force, a pressure gradient. such that air flow is high (air flows easily) when airway resistance is _________ and there is a __________ pressure gradient
when airway resistance is low and there is a strong pressure gradient (P₁ -P₂)
what is laminar airflow?
laminar airflow occurs when no obstacles are in the path of the air molecules and they move in relatively straight "sheets" of air
--> in small, distal airways w/ minimal branching and air velocity in slower
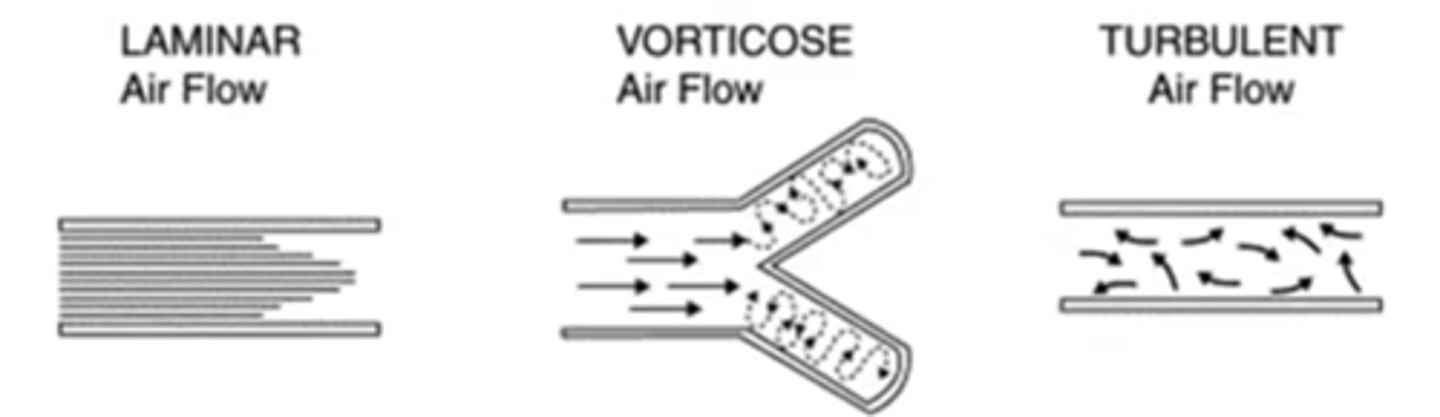
what is turbulence?
occurs when air molecules collide w/ obstacles
--> obstacles are branch points and inner walls of airway tubes, causing air molecules to change direction
--> eddies & currents are created resulting in turbulent travel
when does laminar flow become turbulent flow?
if the airflow is very high and/or at tube branch points
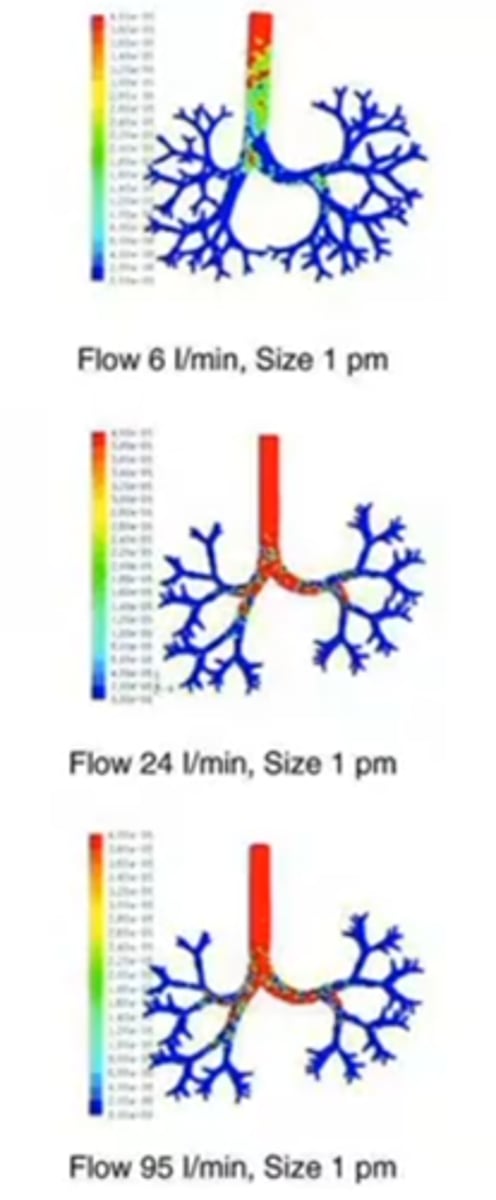
the respiratory particle deposition from aerosols depends on what 4 parameters?
lung anatomy, breathing pattern, gas/vapor properties/ particle properties
--> breathing pattern (holding breath allows more distribution before refreshing of alveolar gas)
--> lung anatomy (branching points)
--> particle size (larger particles in upper airway, smaller particles for lower airway)
--> vapor properties
how does the size of the aerosol particle affect its deposition in the airway?
if the particle is large -> the more likely it will remain with a linear velocity, such that it mainly deposits at impaction points like the back of the pharynx, the trachea bifurcation (i.e. branch points)
if the particle is small -> the more likely it will reach the lower airways
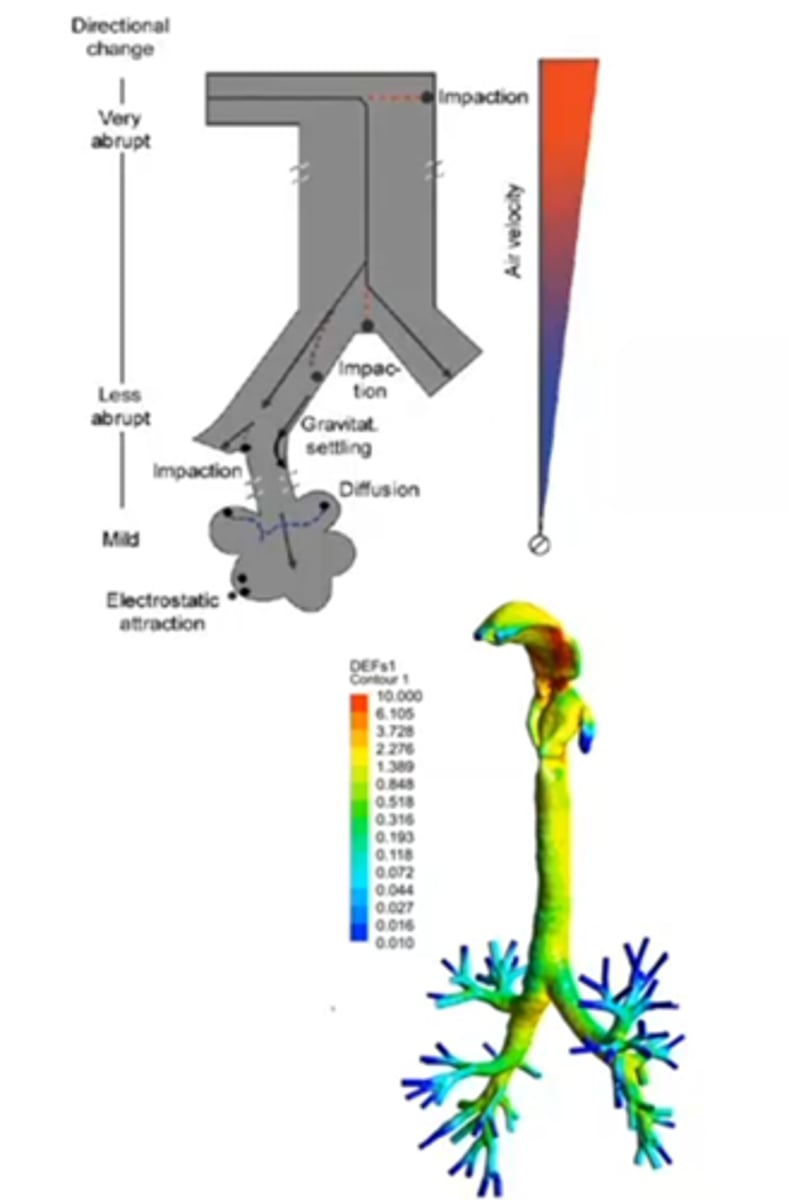
how can we affect the deposition of larger aerosol particles so they reach further down in the airway?
by increasing the speed at which they are introduced (more forceful nebulizations)
--> although still very difficult to bring to lower airways
in order for the force to move air in to the lungs to be strong enough, what must it overcome?
both the compliance of the lungs and the airway resistance
--> pressure to overcome compliance (i.e. is there fibrosis?/emphysema?)
--> pressure to overcome resistance of tube (i.e is there bronchoconstriction? asthma?)
what can cause laryngeal paralysis?
-congenital (huskies, bouvier des flandres, english bulldogs, bull terriers)
-neuromuscular or metabolic diseases (Myasenthia gravis, hypothyroidism)
-trauma (bite wounds or blunt trauma to neck)
-inflammation or neoplasia
what are clinical signs of laryngeal paralysis?
-exercise intolerant
-increased effort/noise assoc. w/ inspiration
-voice change
-gagging or coughing assoc. w/ swallowing food/water
how can a dog w/ a high body temperature be cooled?
by spraying the body w/ cool water, putting cool compresses on pads, and running a fan close to him
--> never cool a patient w/ alcohol it decreases the body temp too quickly and can be dangerous if patient arrests and then needs defibrillating paddles
--> if initial measures unsuccessful, cold water enema can be given
how can you treat laryngeal paralsysis?
emergency treatment -> ensure not choking, provide supplemental oxygen
-later, consider tracheostomy, laryngeal-tie back or unilateral arytenoid lateralization surgeries
^most common complication of theses sx: aspiration pneumonia
what is the resistive pressure?
the difference b/w the elastic recoil pressure and the total pleural pressure, Pₚₗ
how can you calculate the total (airway plus tissue) resistance?
the ratio of pleural pressure (minus it's elastic component) measured during a breath and flow rate
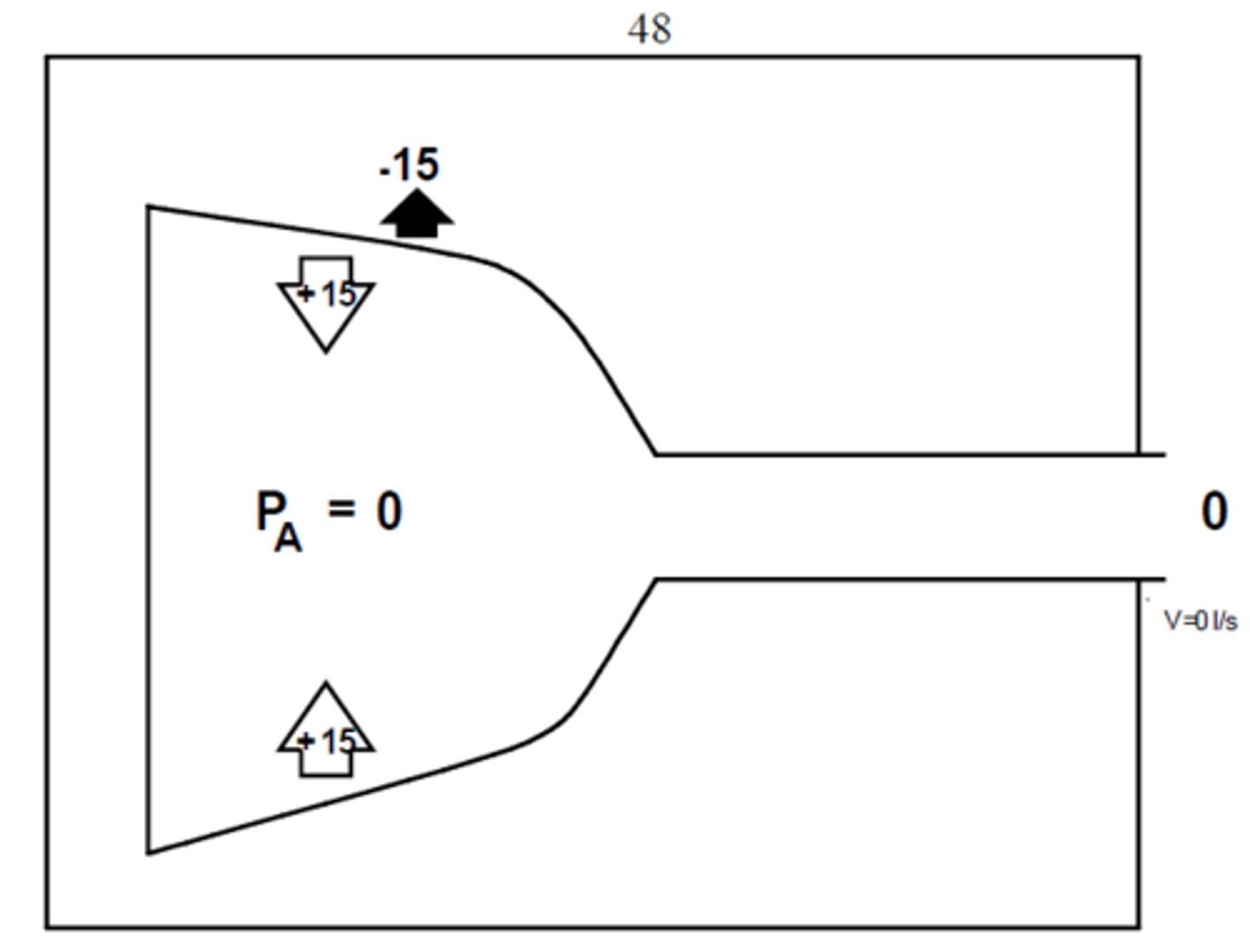
when is alveolar pressure, Pₐ negative?
only for inspiration when there is inspiratory airflow
--> when alveolar Pₐ < atmospheric pressure
when is alveolar pressure, Pₐ zero?
when there is no airflow
--> when alveolar Pₐ = atmospheric pressure
when is alveolar pressure, Pₐ positive?
only for expiration when there is expiratory airflow
--> when alveolar Pₐ > atmospheric pressure
how is airway resistance, Rₐᵥᵥ calculated?
it is the difference between alveolar pressure and atmospheric pressure at a specific flow rate
Rₐᵥᵥ = ΔPₐ/ΔV̇
if the airway resistance, Rₐᵥᵥ is increased, what does this mean with regards to alveolar pressure, Pₐ?
Pₐ will be more negative at the same airflow rate
what diseases can increase the airway resistance, Rₐᵥᵥ?
diseases that cause increased smooth muscle contractions of the distal airways (airway hyper-reactivity)
i.e. asthma
how does bronchial smooth muscle affect airway resistance, Rₐᵥᵥ?
if there is increased smooth muscle contraction, there will be increased airway resistance
this occurs in asthma & allergic type reactions
what is the airflow vs volume relationship?
-the zero is residual volume
-dotted lines are shallower breathing patterns
-solid line is maximal inspiratory/expiratory capacities
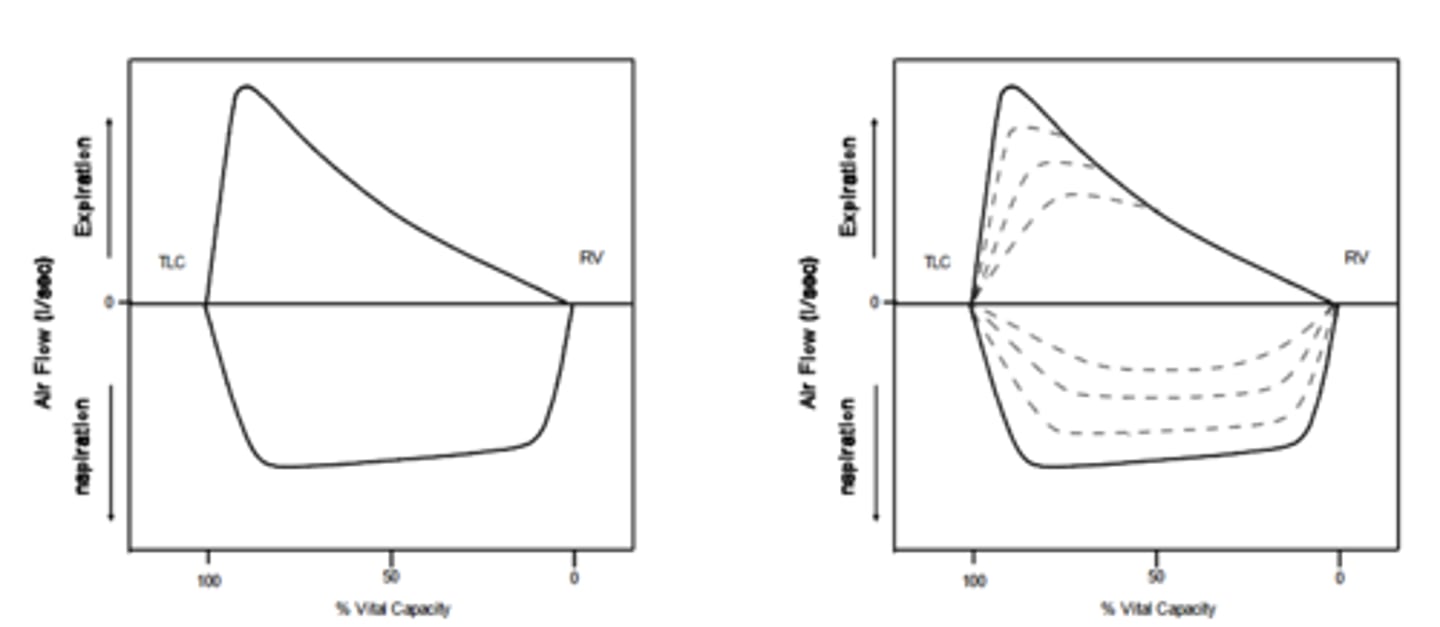
during very hard, forceful expirations what would you expect to see in the expiratory flow rate?
expiratory flow rate has a rapid increase to a peak and then the flow rate decreases almost linearly w/ volume
--> once the peak has been reached, there can not be a greater flow rate beyond it (this is flow limitation)
what is effort independent flow limitation?
no matter how hard you try to expire, you can not increase the flow rate beyond the linear slope (70% TLC)
-it is bc of the relationship b/w resistance, compliance, and expiratory driving pressure
--> increased pressures (pleural and airway) from decreasing/compressing the lung volume (smaller radius, smaller area) results greater resistance and lower airflow
--> there is greater resistance closer to the mouth as well b/c of the smaller diameter airway
--> there is decreased compliance closer to the mouth b/c the tracheal rings are stiffer
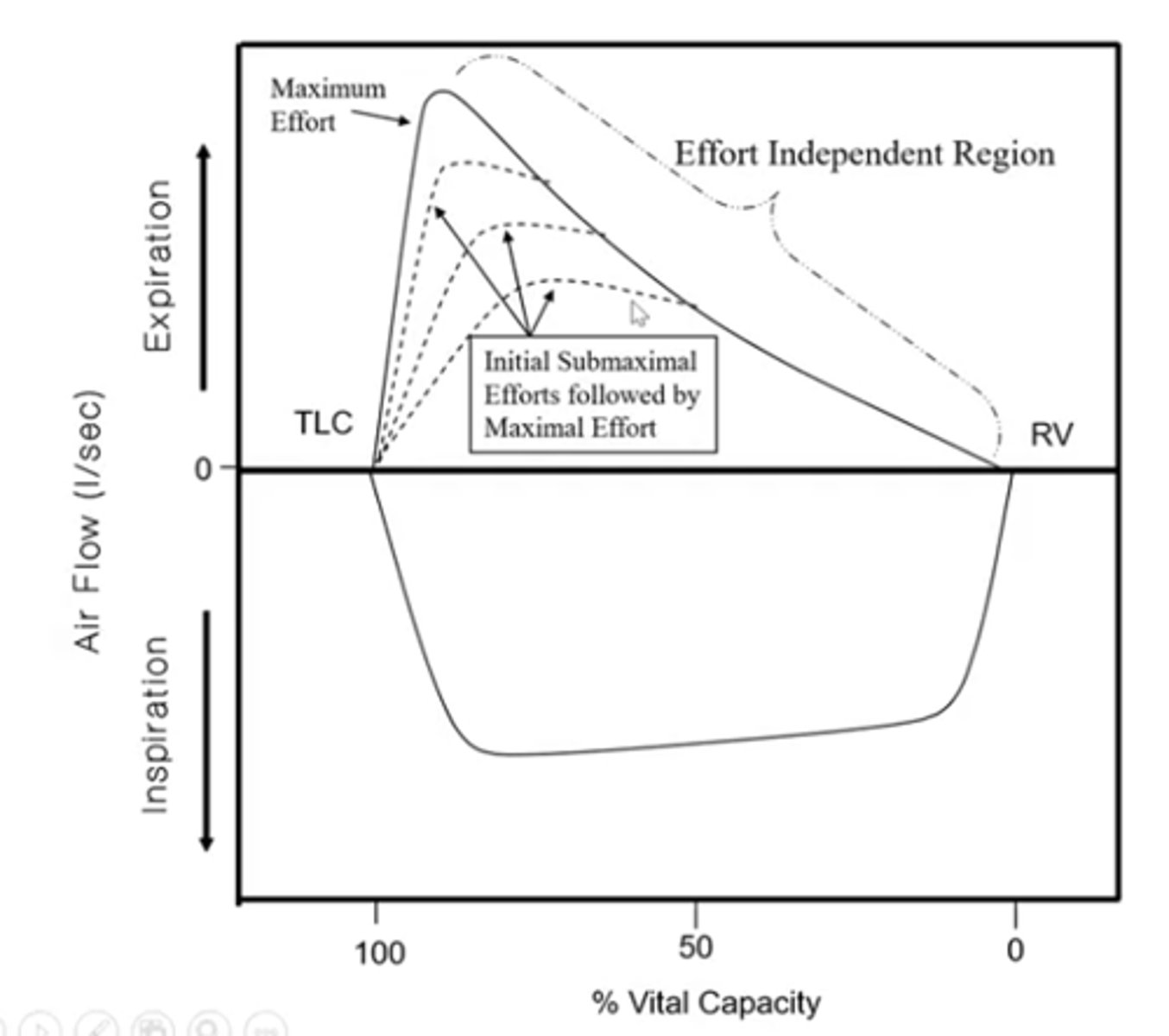
the net expiratory pressure is the _______ plus the _________
recoil pressure plus active pressure
-> recoil pressure from the collapsing force of the lung (surface tension & elasticity)
-> active pressure (from muscle contractions)
how do alveolar pressure Pₐ and pleural pressure Pₚₗ change during inspiration?
Pₚₗ becomes more negative and Pₐ becomes negative equal to the change in Pₚₗ
i.e if Pₚₗ drops from -5 to -8, Pₐ drops from 0 to -3
how do the transpulmonary pressures, Pₜₚ change during inspiration?
Pₜₚ becomes progressively more positive as you get nearer to the mouth
--> results in a greater distending pressure for the airways as you move from alveolus to mouth and helps keep airway open for air to flow
at the end of inspiration, what are alveolar pressure Pₐ and pleural pressure Pₚₗ ?
Pₚₗ is more negative than at FRC
Pₐ is zero
the pressures in the airway are also zero
after inspiration, the relaxation of the expansion forces make the chest and lung want to return to equilibrium position and exhalation occurs. what happens to pleural pressure Pₚₗ , alveolar pressure Pₐ, and transpulmonary pressure Pₜₚ now?
Pₜₚ is less positive as it gets closer to the mouth
Pₐ is positive
Pₚₗ is less negative
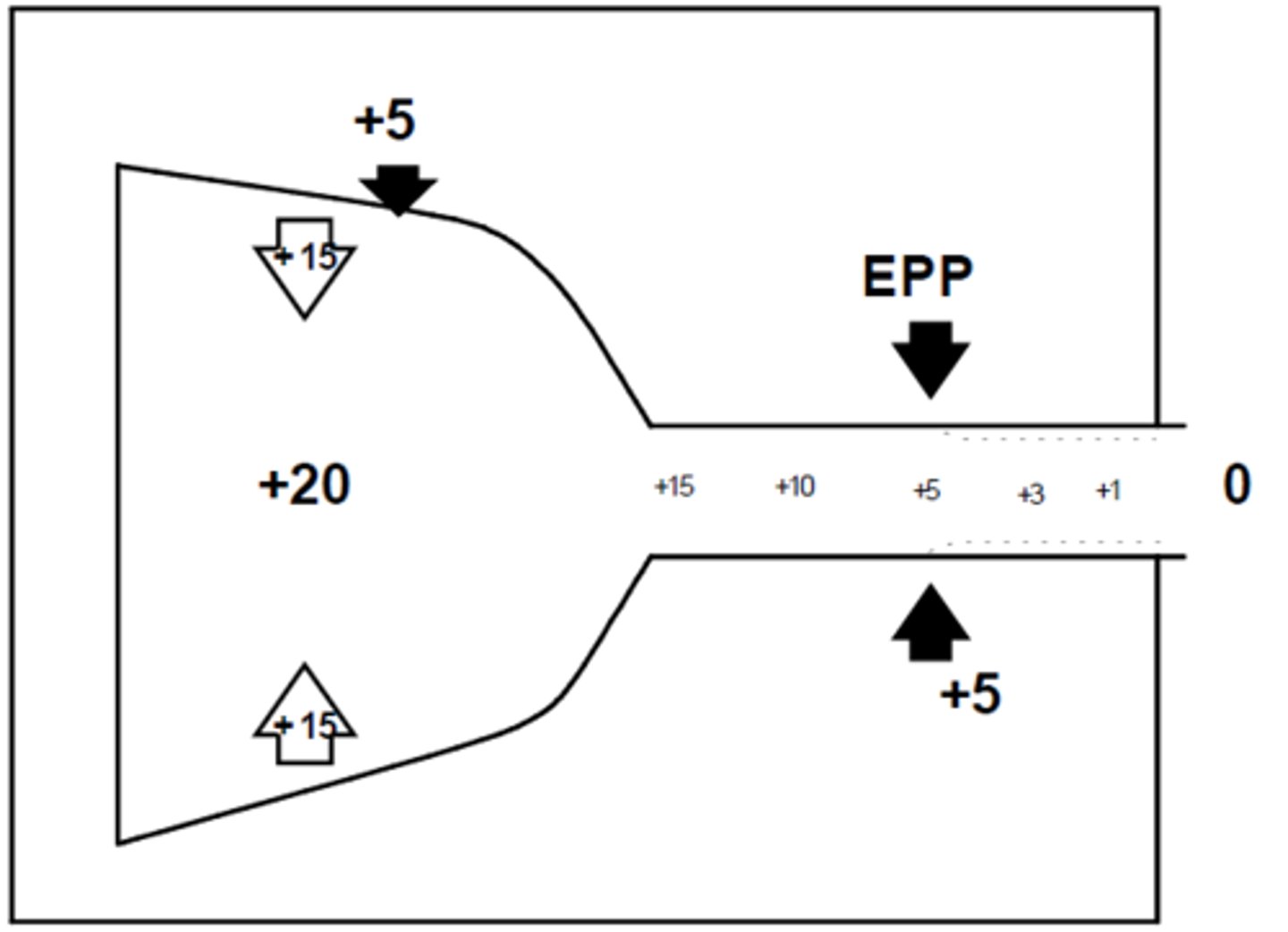
when does transpulmonary pressure Pₜₚ equal zero?
this is the equal pressure point, EEP
--> when the pleural pressure Pₚₗ equals the airway pressure
--> happens during forceful expiration
--> beyond this point (closer to the mouth) the airway will have a collapsing force on it and Pₜₚ negative
in the airway, as long as the intra-airway pressure is greater (more positive) than the Pₚₗ, what happens?
the airway stays open
why does the airway not collapse during an equal pressure point EEP?
because it occurs in the cartilaginous airways (i.e. the trachea) which prevents full collapse