IMED1003 - Glucose Homeostasis (L22)
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
THINGS TO KEEP IN MIND FOR THIS LECTURE
- adrenaline = adrenalin
- up arrow (increase) also means activates
- down addow (decrease) also means inhibits
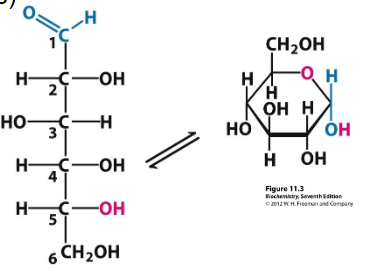
Glucose
- Carbohydrate (monosaccharide)
- energy source (universal fuel)
- Store: glycogen
- 70kg adult < 700g (around 1% wt)
- Liver <120g (around 8% wt)
- Sk muscle <400g (1-2% wt)
.
- Catabolised: aerobically (CO2 and H2O) and anaerobically (lactate) --> ATP
- sourced from diet
- anabolised in liver (and kidney) = gluconeogenesis -> blood -> organs (brain)
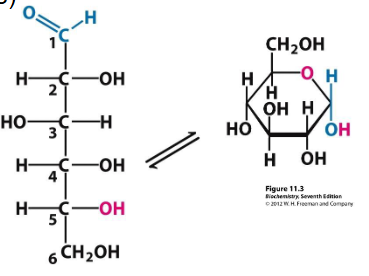
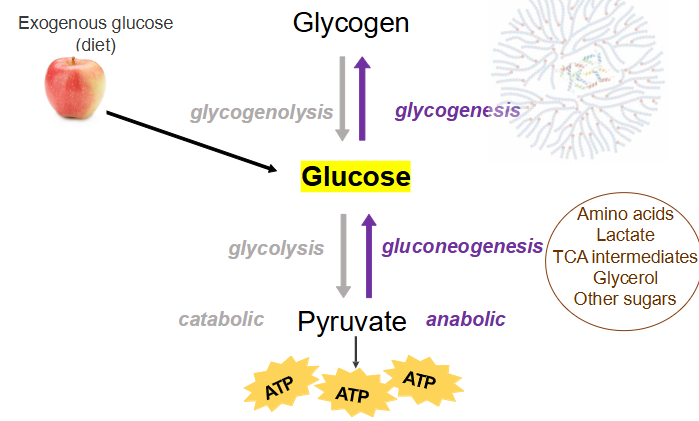
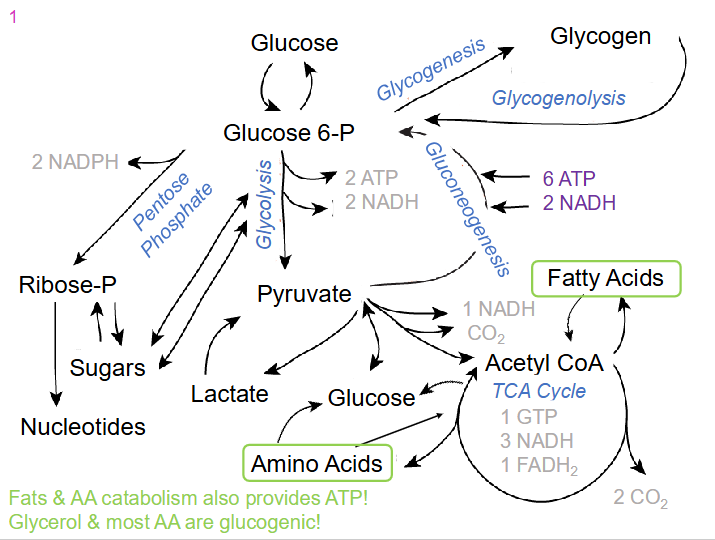
Glucose Metabolism
- glycogenolysis turns glycogen to glucose
- glycolysis turns glucose to pyruvate
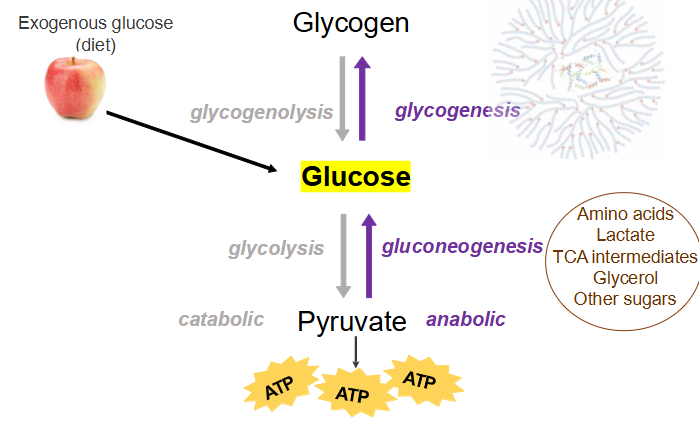
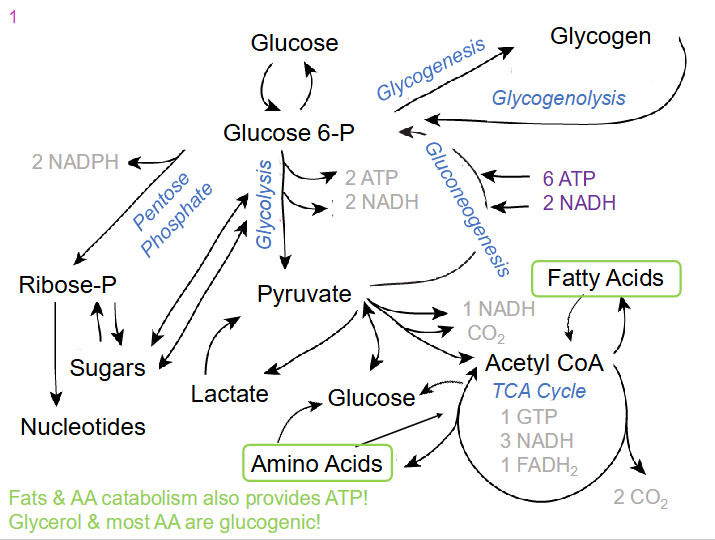
All pathways of Glucose and FA Anabolism and Catabolism
DIAGRAM ON SLIDE 5
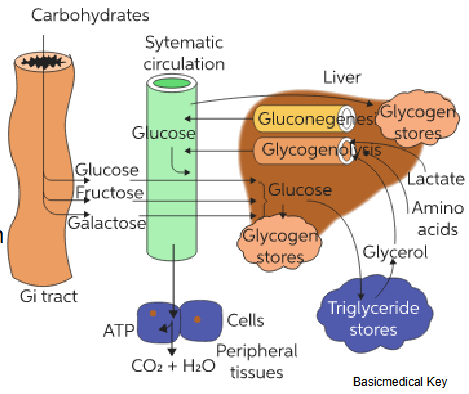
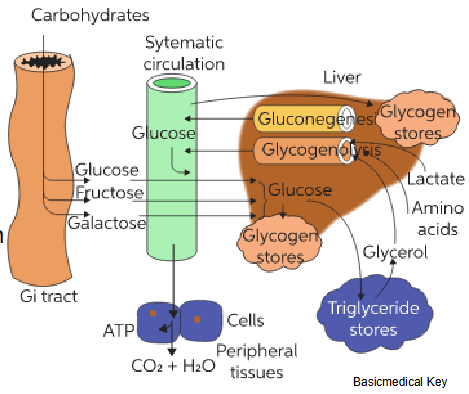
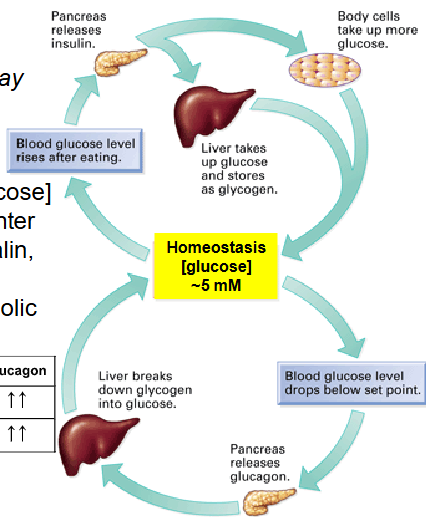
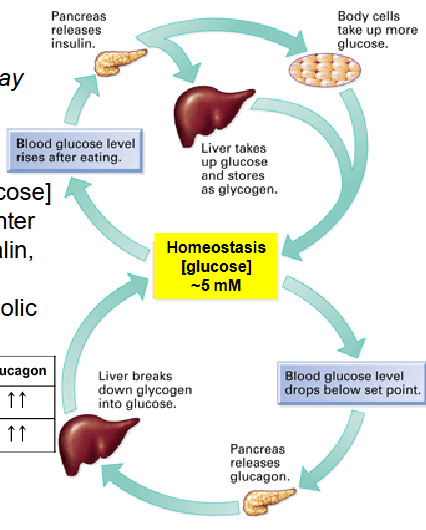
Glucose Homeostasis
- Glucose supply = intermittent and body's metabolic demands vary ... glycogen stores mobilised and utilised when required
- Key organs: liver, brain, skeletal muscle, pancreas, adipose, kidney
- How do we regulate metabolic pathways
- Turn on/off specific enzymes
- Allosteric regulation and hormonal regulation are key to glucose homeostasis: some processes are faster than others
.
- basically diagram shows the path of glucose from GI tract to body
- some glucose goes to peripheral tissues where it is used to make ATP, the rest goes to the liver where it is stored as glycogen
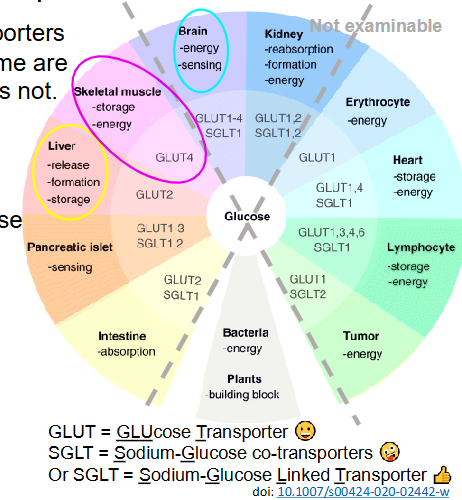
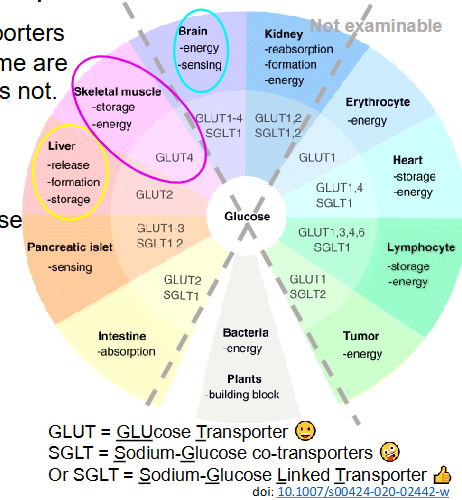
Glucose Transport Across Membrane
- Various glucose transporters in different tissues: some are insulin-sensitive, others not
- Insulin-sensitive: facilitated transport most tissues e.g skeletal muscle, adipose
- insulin-insensitive: facilitated transport liver (bidirectional), brain, RBC, WBC, eye lens, cornea
- active transport intestinal epithelia, renal tubules
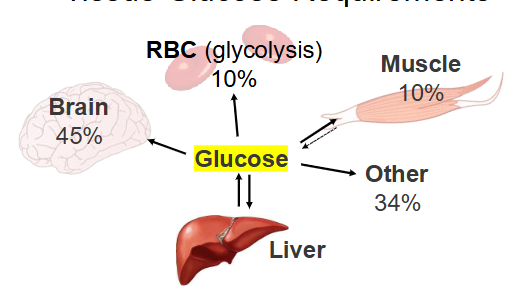
Tissue Glucose Requirements
- Glucose essential fuel for brain (CNS), so blood glucos levels --> tightly controlled around 5mM (mmol/L)
- Can increase glucose use and storage when increaesd blood glucose conc. e.g after eating (postprandial)
- conversely, need to increase glucose conc. when blood glucose conc. is low. e.g after overnight fast
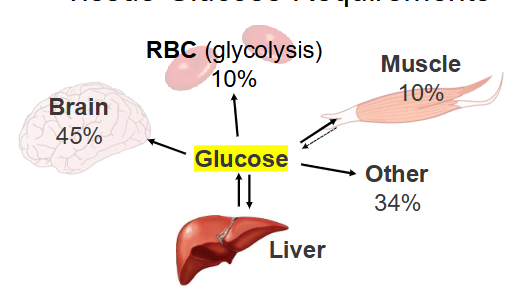
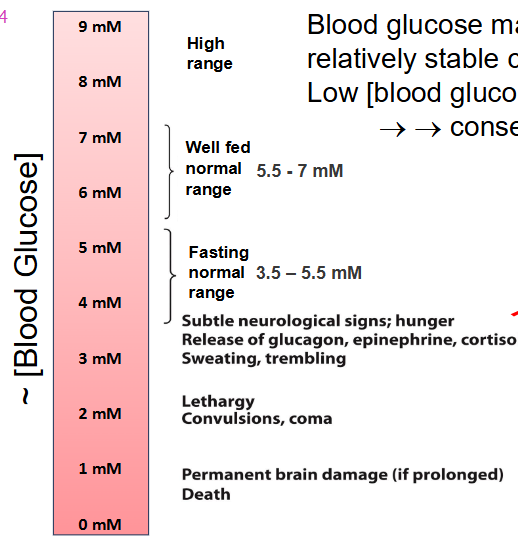
Blood glucose maintained at relatively stable concentration.
Low blood glucose concentration = consequences
- normal range of blood glucose is 3.5-5.5mM if fasting and if well fed normal range is 5.5-7mM
Humans can catabolise triglycerides and proteins (AA) to supply ATP
- The brain consumes around 20% of total body O2 at rest (around 2% body weight)
- metabolism uses around 120g glucose/day
- ATP generated used by Na+/K+ ATPases (ion channels) to maintain membrane potential for nerve impulse conduction
- preferred fuel: glucose
- Can use ketone bodies
- Very low glycogen stores
- Relies on blood glucose
- Extended hypoglycaemia may cause irreversible damage or death
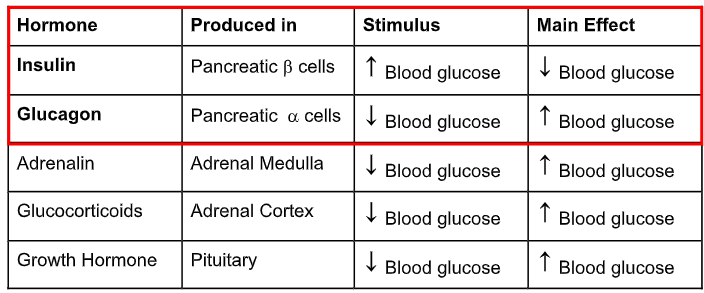
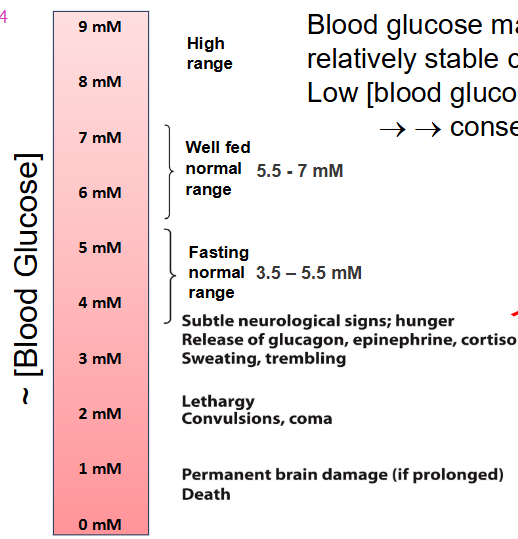
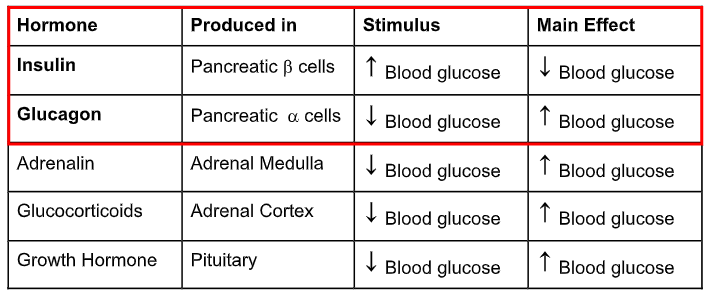
Glucose Regulating Hormones
- Achieved by tissue specific actions of hormones: insulin, glucagon and others and it requires balance
.
- insulin produced by beta cells, they decrease blood glucose
How insulin and glucagon affect blood glucose
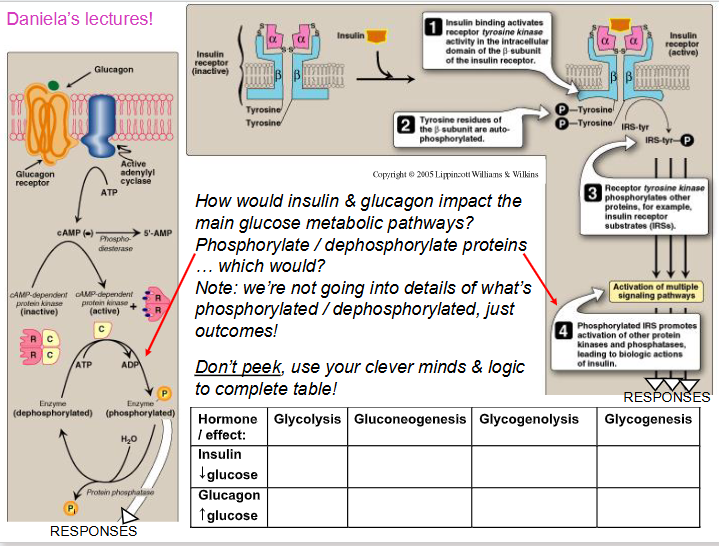
- insulin acts through a receptor tyrosine kinase
NO LEARNING OUTCOME, BUT U DO NEED TO KNOW BASICS ON HOW THEY ACT, NO DETAIL
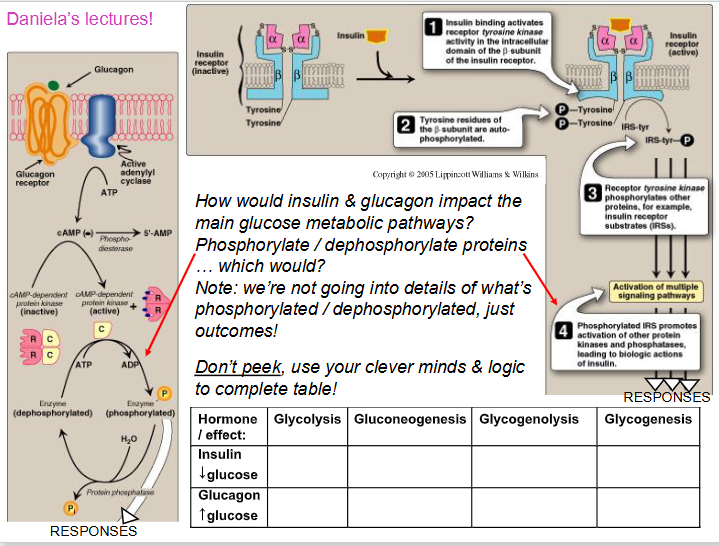
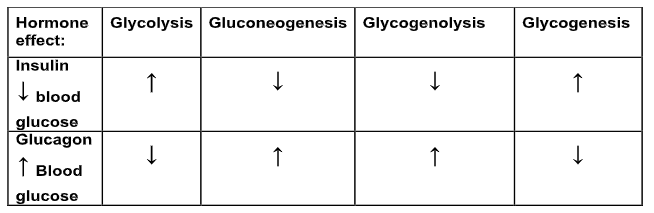
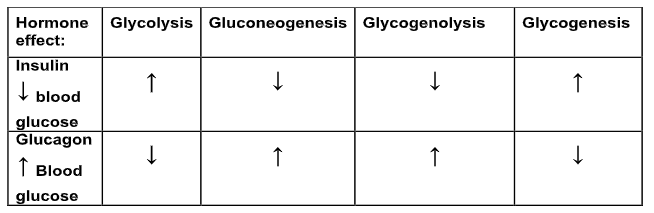
Insulin and Glucagon action
- insulin and glucagon signal via different pathways: overall results in phosphorylating/dephosphorylating target proteins
- Insulin signalling via RTK. commonly dephosphorylates target
- glucagon triggers cAMP-mediated phosphorylation in liver ... commonly phosphorylates target
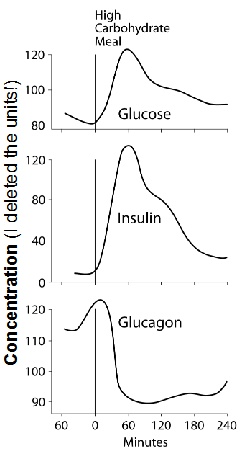
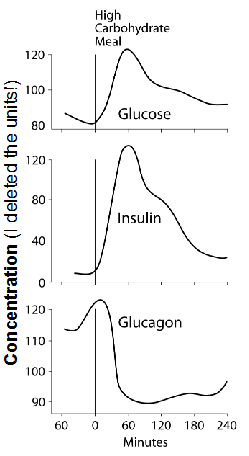
Insulin and Glucagon secretion is responsive to changes in blood glucose concentration
- increased blood glucose after eating
INSULIN: postprandial (after eating) increases, then decreases
- increased blood glucose conc. --> pancreas releases insulin --> signalling
GLUCAGON: postprandial it decreaes, then increaes
- as glucose is taken up and metabolised, blood glucose declines, hence decreased blood glucose conc. --> pancreas releases glucagon -> signalling
Glucose Regulating Hormone Timings of Action
- insulin and glucagon have various timings of actions: fast (<1min), intermediate (10-30min), slower (+1h)
- the "slower" actions can include changes in gene expression
- AND, hormones have varied effects on different tisues... we will concentrate on the liver and a bit on other tissues
- we will look at which enzymes will be impacted for glycogenesis and glycogenolysis
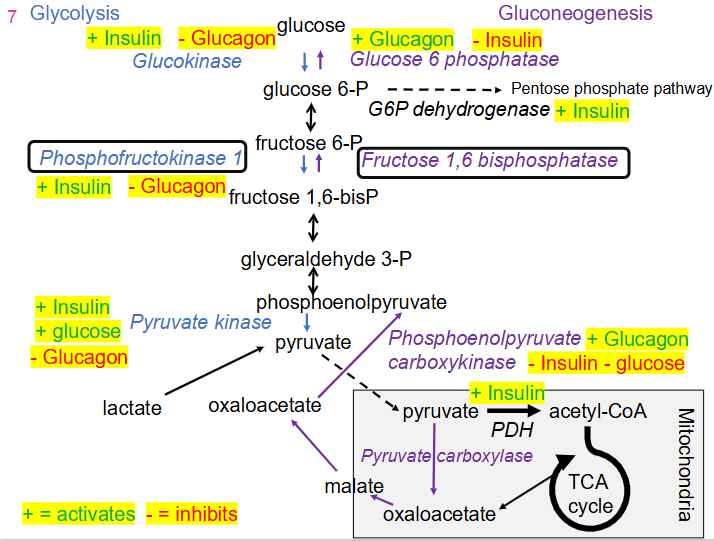
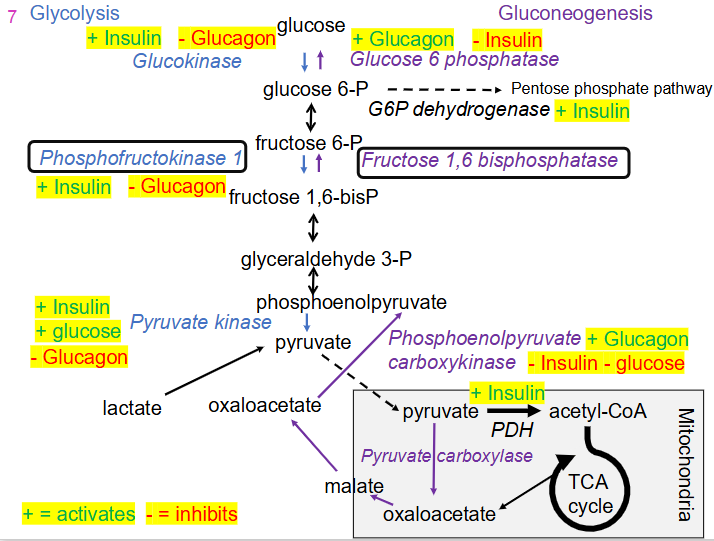
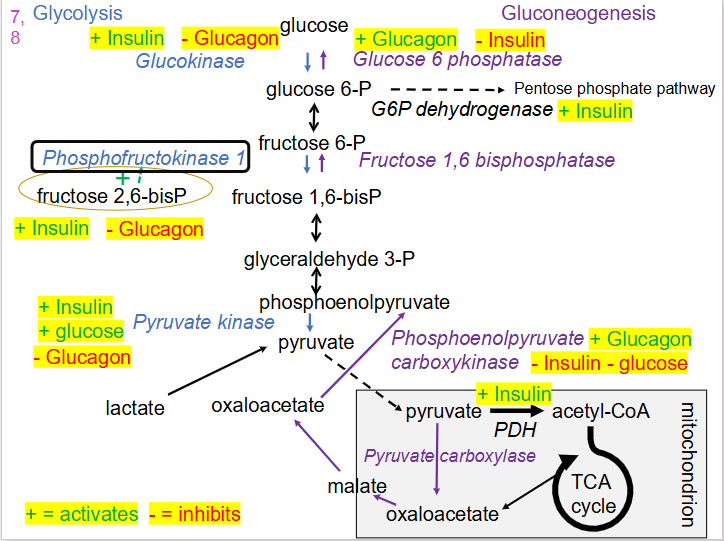
Relationship between Glucose Regulating Hormones and Glycolysis and Gluconeogenesis
- if we want to promote import of glucose into a tissue it makes sense that insulin will promote glucokinase which will phosphorylate it to Glucose-6P, trapping glucose in the cell
- insulin activates phosphofructokinase-1 (key regulatory enzyme) basically it promotes glycolysis, which allows production of pyruvate
.
- glucagon has the opposite effect, it inhibits glycolysis
- glucagon promotes gluconeogenesis
- glucagon promotes activity of phosphoenolpyruvate carboxykinase, which promotes gluconeogenesis, insulin inhibits this pathway
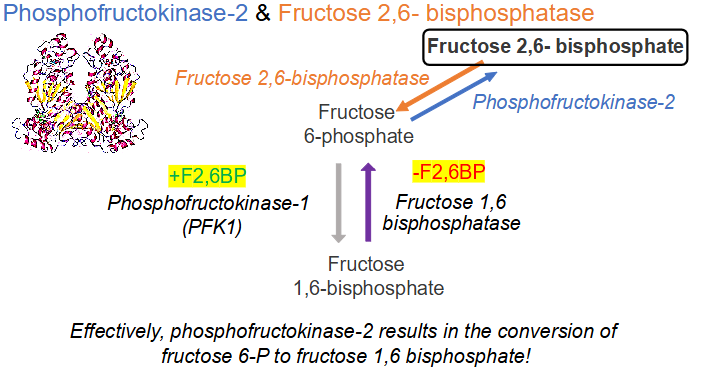
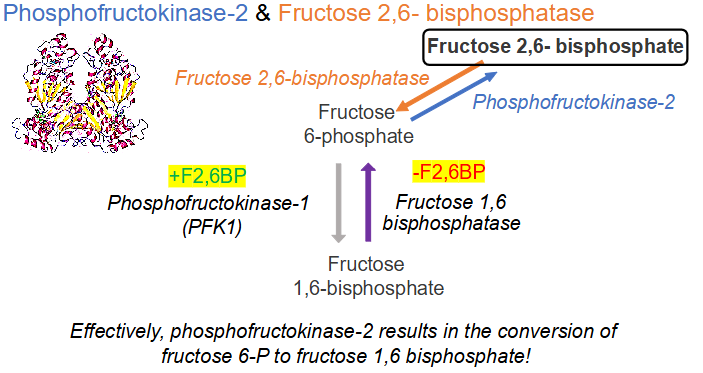
Fructose 2, 6-bisphosphate (F2,6BP) in liver
- F2,6BP = allosteric activator of PFK-1 (promotes glycolysis) and inhibitor of fructose 1,6-bisphosphate (inhibits gluconeogenesis)
- F-2,6BP levels are controlled by a homeodimeric bifunctional enzyme that has 2 domains with different activities = phosphofructokinase-2 and fructose 2, 6-bisphosphotase
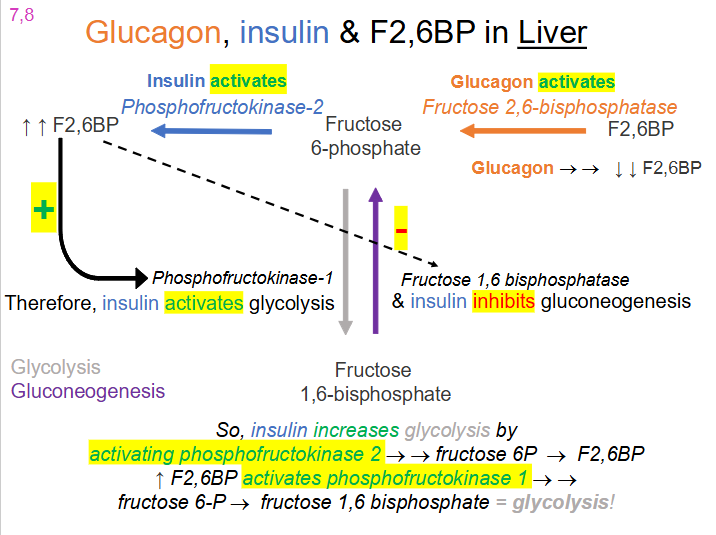
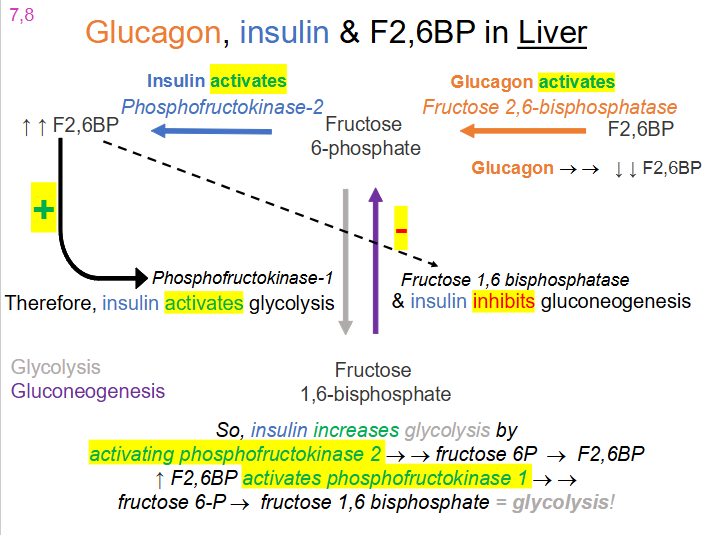
Glucagon, Insulin and F2,6BP in liver
- when insulin is around, it activates the kinase activity of the enzyme which produces a lot of fructose
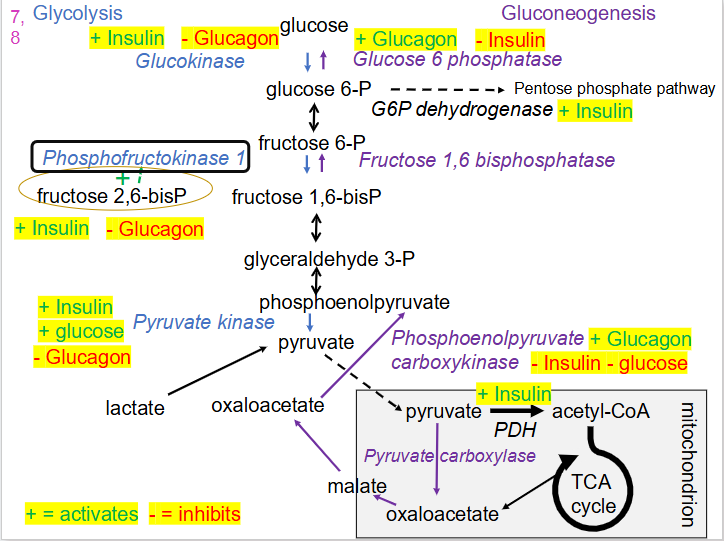
Updated Glycolysis vs Gluconeogenesis
DIAGRAM ON SLIDE 19
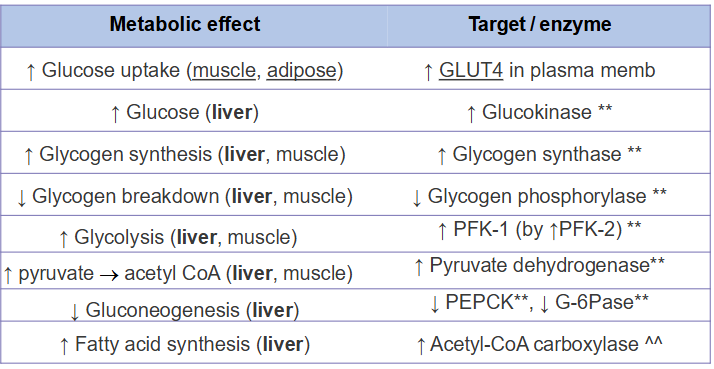
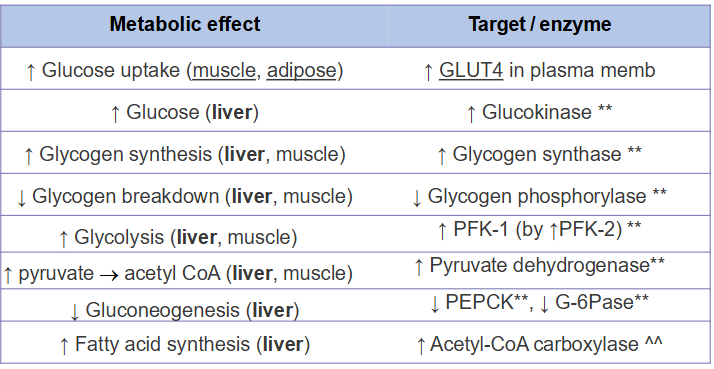
Insulin Secretion
- secreted when blood glucose is high
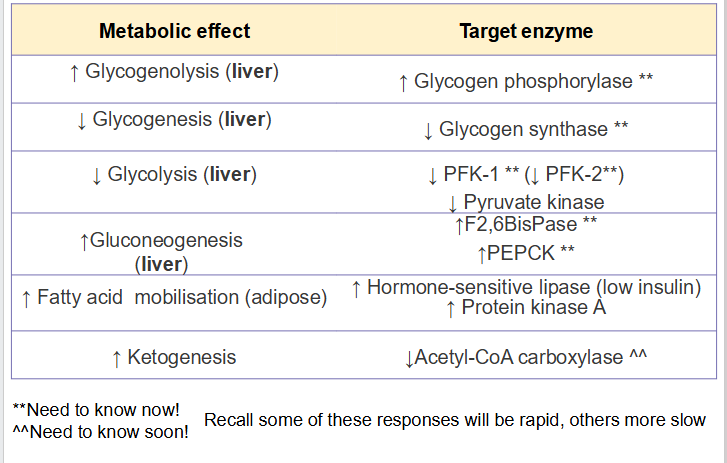
NEED TO KNOW THE ONES WITH ASTERISKS AND ARROWS
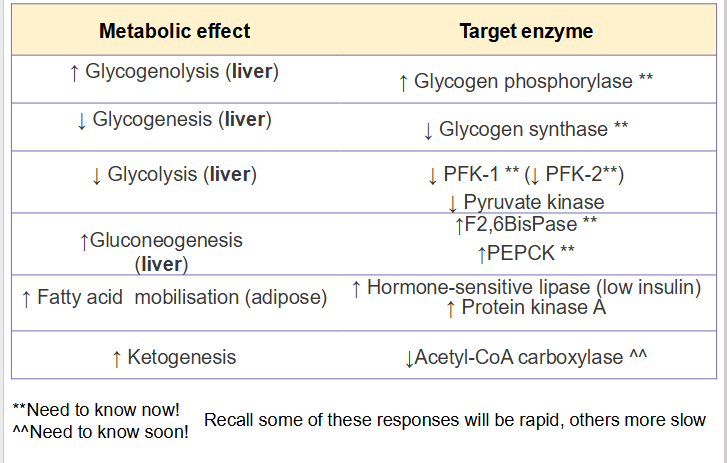
Glucagon Secretion
secreted when blood glucose is low
Simplistic Overview
- Glucose homeostasis is way more complex - multiple organs and hormones
Insulin lowers blood glucose and stimulates:
- conversion of excess glucose to glycogen
- conversion of excess glucose to fat
- Insulin stimulates glucose uptake in muscle and adipose (glucose -> Glucose 6P, hence trapped)
- in liver, insulin stimulates glycogen synthase and inactivates glycogen phosphorylase: glucose 6P -> glycogen
- Liver glucose transport = high capacity and insensitive to insulin (glycogen synthase activated via dephosphorylation, glycogen phosphorylase inactivated via dephosphorylation)
- In liver, insulin stimulates glycolysis and triglyceride synthesis (glucose 6P -> acetyl CoA -> FA/triglycerides)
- in adipose, insulin stimulates triglycerides synthesis (stores)
Glucagon raises blood glucose
- In liver, activates glycogen phosphorylase and inactivates glycogen synthase -> liver can release glucose
- In liver, reduces [F2,6BP] so inhibits glycolysis and stimulates gluconeogenesis -> liver makes glucose and exports it
- inhibits pyruvate kinase: prevents phosphoenolpyruvate from being converted to pyruvate
- Accumulation of phosphoenolpyruvate favours gluconeogenesis, stimulates PEPCK -> liver makes glucose and exports it
Glucagon affects adipose tissue
- recall stores of triglycerides = glycerol + 3FA
- in adipose tissue, glucagon activates triglyercide hydrolysis (through phosphorylation of perillipin) to expose the lipid droplet to lipases and activates hormone-sensitive lipase to release FA
- results in FA transport to other tissues for their energy production needs, so glucose is spared for the brain