Week 1
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
72 Terms
Focus on improving participation & performance of children
By providing direct interventions
Providing indirect interventions (consultation, education, coaching)
Recommend environmental modifications &/or task adaptations
Essentials of Pediatric Intervention:
Focus on improving participation & performance of children
Focus on promoting inclusion
Focus on providing intervention to foster inclusion
Focus on facilitating child engagement
Focus on creating Just-Right challenges
Focus on promoting access & participation
Focus on evidence-based practice (EBP)
Focus on generalization of skills
Focus on using various models of service delivery
Focus on promoting inclusion
Promoting social justice by advocating for inclusion
Children & youth with disabilities have right to participate in all aspects of life, across environments (AOTA, 2015)
Focus on providing intervention to foster inclusion
Educating others (entities, individuals, community)
Recommend modifications to increase physical access
Adaptations to increase social participation
Strategies to improve skills (motor, process, communication/interaction)
Focus on facilitating child engagement
Developing client-centered intervention
Engagement is essential
Child’s brain responds and learns
actively involved vs. receiving passive stimulation
Children are given choices
Selecting interventions that target occupations important to the child (play, taking care of pets, etc.)
Use of specific strategies to promote engaging in & addressing meaningful goals
Focus on creating Just-Right challenges
Create opportunities that match developmental skills & interests
Provide reasonable challenge to their current performance
Activities that keep them engaged & motivated
Foster self-efficacy, self-determination & confidence
Opportunity to develop a sense of mastery
Focus on promoting access & participation
Interventions that modify, change or adapt environments
Increase accessibility (e.g. accessible playground)
Increase safety (e.g. widened doorways in school, home etc.)
Interventions that modify, adapt task
Using technology to assist with participation
Low tech (e.g. switch toys)
High tech (e.g. augmentative communication devices)
Appropriate sensory modifications to accommodate for sensory differences
Focus on evidence-based practice (EBP)
Research shows that EBP not routinely integrated into practice
Hospitals & medical teams, schools & educational systems & stakeholders have called for EBP & policies
Positive correlation between high positive outcomes & EBP
Focus on generalization of skills
Plan interventions that can be generalized across environments
Goal is not just for the child to do well during 1:1 session
Partnering with client & caregiver
Collaborating with other team members (teachers, SLPs, etc.)
Our role in primary care
Using coaching as an interactive style
Supporting parents to implement specific strategies
Focus on using various models of service delivery
Variety of service models in pediatric practice
Direct service- individual &/or group
In-direct services- consultation services with caregivers or other professionals; advocating for clients (universal design)
Push in vs. pull out in school settings
Fluid service delivery model (therapy as needed)
Recent research shows collaborative & inclusive interventions (indirect & push-in models) are the most effective
coaching as an interactive style
•According to Rush & Sheldon (2004) “Coaching is an adult learning strategy in which the learner’s ability to reflect on their actions is promoted in order to determine the effectiveness of an action or practice and develop a plan for refinement & use of the action in immediate & future situations.”
Why coaching as an interactive style?
Facilitates parental self-efficacy
Facilitates teacher self-efficacy
Evidence in improving parental & teacher competence
parental self-efficacy
– refers to how confident a parent feels in their ability to manage their parenting role which ultimately relates to & has an impact on effective care of their child (Benzies et al., 2013; Giallo et al., 2013; Guillamon et al., 2013; Heath et al/. 2015; Weiss et al., 2013)
– is indicative of both how well a child adjusts in their environment (Giallo et al., 2013) & of parental stress (Benzies et al., 2013)
–Parents with high sense of _ tend to use positive strategies & coping mechanisms that allow for resilience when caring for a child with disabilities (Benzies et al., 2013)
▪Parents tend to navigate tasks related to child care with positivity & determination
–Parents with low sense of _ may not be consistent at engaging with their children (Cohen et al., 2015)
teacher self-efficacy
refers to a teacher’s belief in their ability to successfully cope with tasks, obligations & challenges related to their professional role (Caprara et al., 2006)
Strong evidence in the literature that teachers with high levels of_ experience higher levels of job satisfaction, lower levels of job-related stress & more confident in dealing with students’ challenging behaviors (Caprara et al., 2003)
Facilitating teacher _ with the intervention plan
Evidence in improving parental & teacher competence
OT interventions addressing parental & teacher self-efficacy shown to improve occupational performance of children across environments (home, school, community)
Using coaching as an interaction style has shown to improve parental & teacher self-competence (Little et al., 2018; Graham, 2013; Dunn et al., 2012
Coaching
a type of practice within capacity building model to support clients & client constellation in using existing skills & to develop new skills to achieve desired outcomes. (Dunst & Trivette, 1994; Rush et al., 2003)
Family capacity-building
refers to the methods and procedures used by practitioners to create parenting opportunities and experiences to strengthen existing and promote the development of new parenting abilities in a manner that enhances and strengthens parenting self-efficacy beliefs.”
(Division for Early Childhood, 2013)
dependency creating examples
caregivers see tele-intervention as a huge change in service delivery and is fearful of having to be responsible for the intervention
the activity is created, provided, or decided. by the practitioner
practitioner has his/her hands on the child (literally)
practitioner tells the caregiver what to do
learning only happens when practitioner is present
caregiver says “we cant do this without u”
examples of capacity building
caregivers see tele-intervention as merely not sharing the same physical space with the practitioner and continuing to be responsible for helping the child learn
the activity setting for the visit is planned around what the caregiver naturally does with the child. no practitioner toy bag required on a televisit
Practitioner has his/her hands around caregiver (figuratively). tele-intervention builds the capacity of the practitioner to hone his/her coaching skills
practitioner helps the caregiver reflect on what he/she knows and learn new strategies
learning happens as part of everyday activities with the caregiver and other family members based on a jointly developed between visit plan
caregivers say “we got this”
Using Coaching as an interactive style
According to Rush & Sheldon’s model (2011), the purpose of coaching is to acknowledge the existing body of knowledge & practices being used by a coachee as well as potentially enhancing that knowledge, while facilitating them to engage in a continual process of self-reflection & learning
According to their model, coach is not the expert but instead serves to support the coachee in achieving specific goals (Rush & Sheldon, 2011)
Coaching can be used to assess knowledge, facilitate growth & learning of specific content areas, promote EBP during interventions, analyze the effectiveness of interventions & provide support and feedback throughout the process
5 characteristics of coaching
•Joint Planning
•Agreement b/w coach & coachee on strategies
•Observation
•Observing either the coach or the coachee’s actions
•Action/Practice
•Opportunities for the coachee’s to practice, refine, or analyze new &/or existing skills
•Reflection
•Occurs when coachee reflects on existing strategies
•Feedback
•Coach provides info. to the coachee based on direct observations
NOT A LINEAR PROCESS
Coach’s Role- joint planning
Revisit previous plan- what have they been doing/practicing
In between visit plan- determine how and when will they utilize strategies discussed to practice skills
Next visit plan- determine what the OT and caregiver plan to address with the client during the next session
Coachee’s Role- joint planning
Shares what they tried
Identifies what they want to accomplish
Discusses what they would like to work on during next session
coach’s role- observation
Observe the coachee within the context of activities
Look at both what the client & caregiver (coachee) are doing
Activity analysis
Can happen formally or informally
Use modeling & demonstration as needed
coachee’s role-observation
Observe the coach model a behavior
Demo. good understanding of what the coach is modeling
Characteristics of coaching- Observation- Modeling
Definition: observation of the coach by the coachee:
•coach explains what they are going to do and why
•Give the coachee something specific to observe
•Coach models while the coachee observes
•Coach debriefs with coachee what happened during modeling
•Coachee tries what the coach modeled
•Reflection/Discussion
•Develop a plan as to how this strategy or activity will happen when coach is not present
coach’s role- action/practice
Supports the coachee in practicing, refining, and/or analyzing new or existing skills during real life context that occur during sessions
Observation & Action/Practice go hand in hand
coachee’s role- action/practice
Tries new ideas or actions that either were previously discussed & planned with the coach or resulted from a previous coaching conversation
coach’s role- reflection
▪Analysis of existing strategy
–Is it consistent with EBP?
–Is any adaptation or modification required to obtain desired outcome?
▪Use reflective questions to assist coachee in analyzing the current situation, encourage coachee to generate alternatives & actions for improving their knowledge & skills
coachee’s role- reflection
§Determines what worked or did not work?
§Why did it work or not work?
§Analyze and come up with alternatives or ideas for next steps
§Allows them to step back and think about what they know
Characteristics of coaching- Reflection (WILL BE ON EXAM)
awareness questions
analysis questions
alternative questions
action questions

awareness questions
•Promote understanding of what caochee already knows and can do
•E.g.- What have you tried?
awareness question
•Support coachee in comparing their current understanding to their desired goal
•E.g. What do you think will happen if…?
Alternative Questions-
Help coachee consider a variety of options to address desired goal
E.g. What else could you have done?
Action Questions
- Assist coachee in developing a plan for reaching desired goal
E.g. What do you plan to do?
Characteristics of coaching- Feedback
Information provided by the coach that is based on their direct observations of the coachee, or information shared by the coachee or the actions reported by the coachee. This information aims to expand coachee’s current level of understanding about EBP to affirm the coachee’s thoughts/actions
Coach’s Role - feedback
▪Uses knowledge when it is appropriate to affirm what the coachee says or does.
▪Provide positive feedback
▪May share further information to build on coachee’s knowledge & skills
diff types of feedback
affirmative
evaluative
informative
directive
Affirmative Feedback
Non-judgmental acknowledgement
E.g. “I hear what you are saying” or “I understand”
evaluative feedback
Supports strengths & appraises potential growth
E.g. “When you did that, child responded well.”
informative feedback
Shares expertise or knowledge
*ask before you share
directive feedback
Instructs coachee (only used in situations of danger)
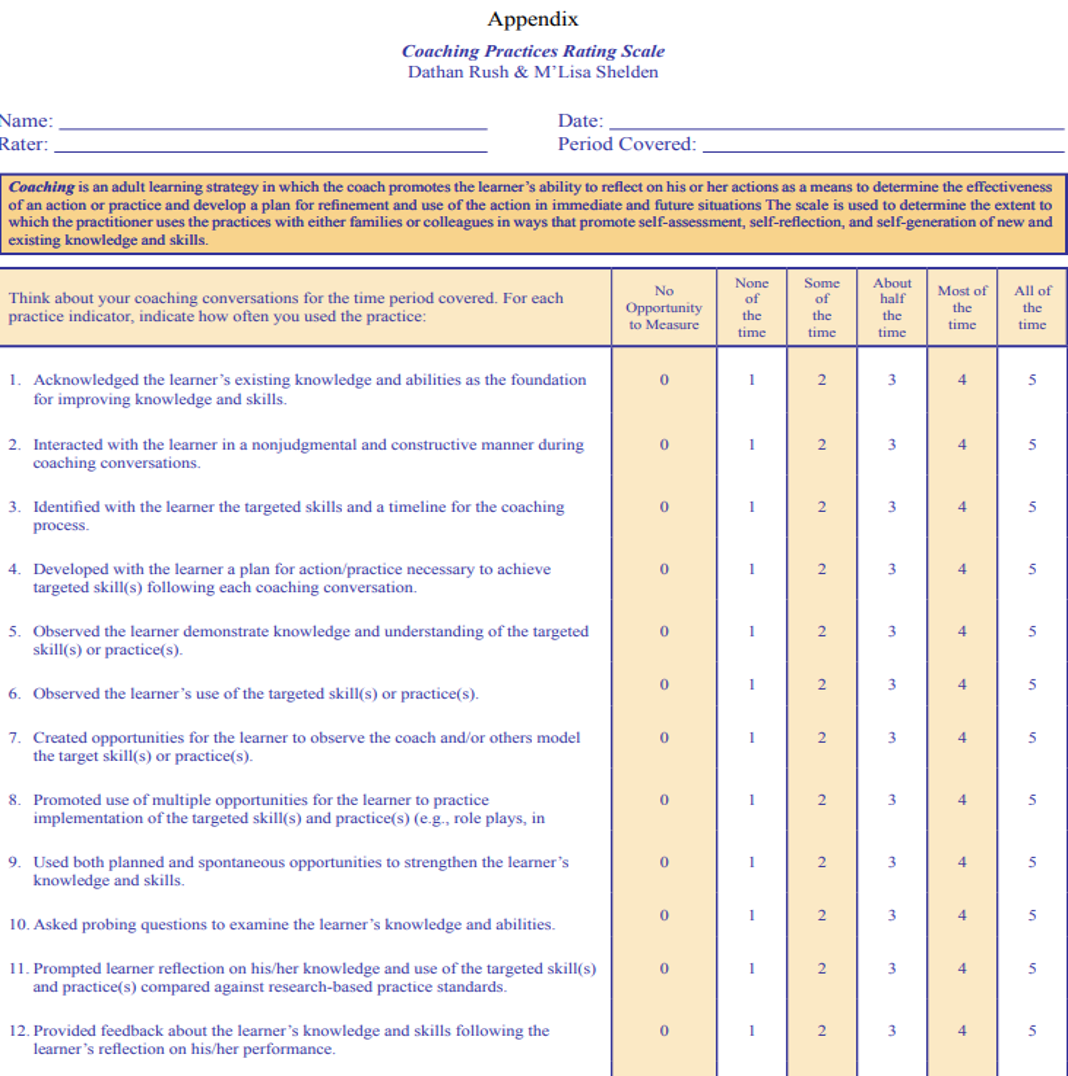
Coaching Practices Rating Scale purpose
The scale is useful for assessing practitioner use of & adherence to evidence-based coaching practices in early childhood intervention
how to use the coaching practices rating scale
The scale is completed based on participation in or observation of:
A single coaching session or a series of coaching interactions
Coaching sessions b/w practitioner & family members or b/w 2 practitioners or b/w a supervisor & practitioner
Used for self-administration
Telehealth- what is it?
Defined as “Application of evaluative, consultative, preventative, & therapeutic services delivered through information & communication technology.” (AOTA Position Paper, 2018, p.1)
Emerging model of service delivery
Minimize difficulties related to regional differences in access to therapists & therapy services
Telehealth- what does research show?
Huge change & shift due to the pandemic in 2020
OTs “forced” to learn tips and tricks to using technology as a mode to provide OT services
General shift in attitudes towards telehealth
Recent research results show-
77% of OTs support telehealth (N = 176/230)
78% support telehealth as a permanent option for OT services (N = 179/230)
Benefits include
Improved parent/caregiver involvement which improved effectiveness of OT service
Effective mode of service delivery for OT services (“see more clients on a given day”)
Increase access to healthcare
Challenges include
Technical issues
Not effective with all populations (e.g. clients with significant cognitive challenges)
Teletherapy other names
tele-intervention, telehealth, tele-practice & virtual home visits
Basic requirements of teletherapy
Check with your state & clinic’s requirements, third party payer’s rules for reimbursement
Both practitioner & client/family receiving services should have access to technology
Device (computer, smart phone)
Internet
Access to web base application (e.g. Zoom, WebEX, GoTo meeting, Teams)
Federal laws governing in-person practice such as HIPPA & FERPA also apply to telehealth practice
Must maintain privacy & security of client’s info. (both electronic & environmental considerations)
Planning the visit - teletherapy
Plan to discuss about your first visit prior to the actual first virtual visit (Planning call)
Discuss use of technology (perhaps parent education on use of technology)
Discuss focus of therapy sessions (in natural activity settings such as mealtime, chores, self-care routine, etc.)
Use coaching as an interactive style to facilitate collaboration
Discuss use of device in facilitating observation of client participation (phone camera providing mobility)
Discuss preferred mode of communication (email, phone, etc.)
List of objects (prior to session)
Agenda for the visit- teletherapy
planning, observation, facilitate reflection
Planning (3-part planning)- teletherapy agenda
Revisit previous plan- what have they been doing/practicing (quick check)
In between visit plan- determine how and when will they utilize strategies discussed to practice skills
Next visit plan- determine what the OT and caregiver plan to address with the client during the next session
Planning (3-part planning)- observation agenda
Essential step
Observe using your OT lens (both what the client & caregiver (coachee) are doing)
Have them practice
Use of modeling & demonstration may have to be modified (e.g. talk through, demo. using a doll)
Facilitate Reflection - teletherapy agenda
Open-ended questions to facilitate caregiver reflection
What worked, what didn’t work
Prompt to reflect on different ways to improve child participation
Provide feedback as appropriate
Be specific with feedback
Primary Care
SYSTEM OF PROVIDING PREVENTATIVE & CURATIVE SERVICES
GEARED TO IMPROVE HEALTH & PROMOTE CHRONIC DISEASE MANAGEMENT
EXPANSIVE DUE TO HEALTHCARE REFORM
FOCUSED ON POPULATION HEALTH
EMPHASIZES COORDINATION OF CARE
ADDRESSES SOCIAL DETERMINANTS OF HEALTH
ALIGNS WITH THE QUINTUPLE AIM
OTs in Primary Care Work
ACROSS THE LIFESPAN WITH WIDE RANGE OF CONDITIONS
AS GENERALISTS
AS INTERPROFESSIONAL TEAM MEMBERS
PROVIDING LONGITUDINAL CARE
CONSULTANT
Provides consultation during clinic
hours, also consistent with "intrusive” model of service delivery
CASE MANAGER/CARE COORDINATOR
Provide in-person and/or telephonic coordination of services based on health risk assessment
INDIVIDUAL PROVIDER
Conducts traditional service delivery, separate encounter in clinic or in client's home
GROUP FACILITATOR/ADVOCATE
Peer mentor group co-leader or collaborator
Where is primary care practiced?
Type of setting determined by organization, reimbursement method, availability of other professionals, and population needs
ACCOUNTABLE CARE ORGANIZATIONS (ACOS)
PATIENT CENTERED MEDICAL HOMES (PCMH)
PRIVATE/FREE-STANDING CLINICS
CLIENT'S HOMES
How is primary care reimbursed?
VALUE-BASED CARE
Reimbursement is based on outcomes or performance, not volume (such as fee for service)
→
POPULATION MANAGEMENT
ACOs and PCMH focus on managing populations with cost-containment methods such as care coordination and risk mgmt.
→
INNOVATIVE MODELS OF CARE
Primary Care Models, e.g., Comprehensive Primary Care Plus (CPC+)focus on access, engagement, planned care, and comprehensiveness
Evidence-Based Primary Care OT Practice
COST EFFECTIVENESS AND EFFICACY FOR INTERVENTIONS ACROSS LIFESPAN
INTERVENTIONS IDENTIFIED ARE:
HEALTH PROMOTION AND LIFESTYLE MODIFICATION
MGMT. OF MUSCULOSKELETAL CONDITIONS
SAFETY AND FALLS PREVENTION
PROMOTING ACCESS TO COMMUNITY RESOURCES
DRIVING AND COMMUNITY MOBILITY RESOURCES
FAMILY AND CAREGIVER ASSISTANCE & SUPPORT
HOME MODIFICATIONS
TOP FIVE INTERVENTIONS for OT in primary care according to scoping review
ADVOCATING AND CONNECTING TO COMMUNITY SERVICES
CHRONIC DISEASE MANAGEMENT
SELF-MANAGEMENT EDUCATION
EHALTH PROMOTION
FALLS PREVENTION
*PREDOMINANT AMOUNT OF LITERATURE IS ON ADULT TO OLDER ADULT POPULATIONS
Primary Prevention
Roles for OT: Individual Provider Consultant
considerations
Determine roles, routines, habits that impact adherence to healthy habits, nutrition and physical activity
Identify barriers & supports to occupations that promote health
Review client's primary care health risk screening site's items that address prevention
Primary Prevention
Roles for OT: Individual Provider Consultant
ot processes: Evaluation options:
Assess self-efficacy for balance and fear of falling using Falls Efficacy Scale
Assess functional mobility for reaching items using Functional Reach Test
Assess client's occupational adaptation and readiness for change to support recommended health behaviors using Occupational Circumstances Assessment Interview and Rating Scale (OCAIRS)
Primary Prevention
Roles for OT: Individual Provider Consultant
ot processes: intervention options:
Educate in techniques to utilize preferred occupations that promote healthy food choices and increase activity level
Provide motivational interviewing techniques to influence health behavior changes using meaningful occupations and engage the client in specific action plans by asking permission, eliciting change, exploring importance with open-ended questions, and emotion seeking skills
Address lifestyle modifications taking into consideration access to exercise facilities, transportation, cognitive abilities to use exercise equipment , meal preparation skills, and access to social/in-person supports
secondary Prevention
Roles for OT: Consultant
considerations
Determine other services child is currently and previously received
Collaborate with nurse practitioner to develop plan of
care and identify next steps with child's therapy team
secondary Prevention
Roles for OT: Consultant
ot processes: evaluation options
Complete occupational profile to understand performance patterns, family and environment
Consult with current practitioners providing service to child
Assess sensory processing using parent-completed inventory and self-regulation questionnaire
secondary Prevention
Roles for OT: Consultant
ot processes: intervention options
Provide parent education on self-regulation techniques, including emotional regulation and sensory processing
Provide an OT developed sensory diet and mindfulness activities
Consult with nurse practitioner about finger skin integrity
tertiary Prevention
Roles for OT: Individual Provider, Group Facilitator, Care Coordinator
considerations
Determine current adaptive equipment resources an environmental supports
Collaborate with interprofessional team members on on-going needs of client
Understand end of life care planning and implications on interventions
Consider progression stage of condition and necessary community resources and support groups
tertiary Prevention
Roles for OT: Individual Provider, Group Facilitator, Care Coordinator
ot processes: evaluation options
Complete occupational profile to understand performance patterns, family and environment
Consult with current practitioners providing service to client
Assess person-environment fit within the home using I-HOPE and/or I-HOPE Assist
tertiary Prevention
Roles for OT: Individual Provider
ot processes: intervention options
Provide client and caregiver education on adaptive technique and equipment focusing on compensatory strategies
Provide supportive and educational services to formal and informal caregivers
Consult with interprofessional team on current status and impact on engagement in occupation and care planning
Discuss with client and family appropriate social and physical environmental supports
Connect client and family with services and resources (e.g., AAT, DME, local chapter support groups)