lumbar spine - radiographic technique
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
what are the clinical indications for lumbar spine x-ray
Wedge fracture
Burst fracture
Chance fracture
Scoliosis/kyphosis
Spondylosis
Ankylosing spondylitis
Spondylolisis
Spondylolisthesis
Spondyloptosis
Spina bifida Occulta
Loss of curvature
# sacrum
Dislocation of Sacro-iliac joints
what should not be an indication for lumbar spine
Prolapsed intervertebral disc (PID) should not be an indication for lumbar spine – it should be MRI
what are the radiation protection measures for lumbar spine examinations
Identification check
Careful technique to avoid repeat examination
Gonad protection applied wherever practicable
Efficient collimation
Application of the 28 day rule where appropriate
Consider an alternative imaging modality eg. Ultrasound
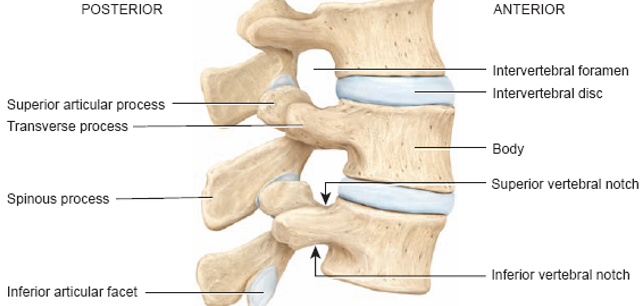
Radiographic anatomy of lumbar vertebrae - lateral
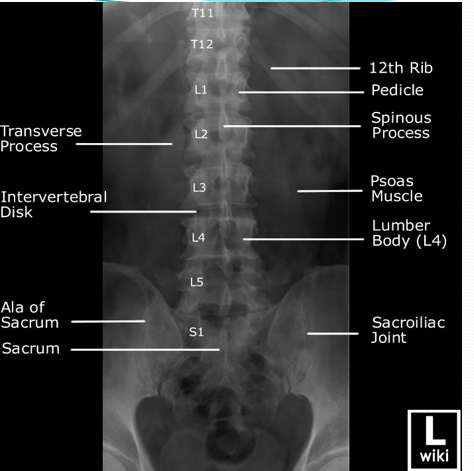
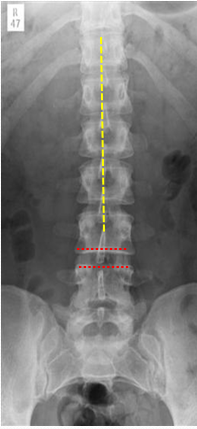
lumbar AP xray labelled
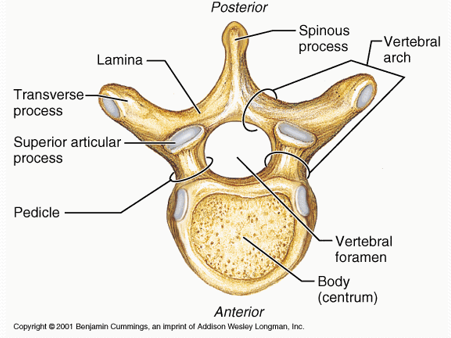
radiographic anatomy of lumbar vertebra
what’s the radiographic technique for lumbar AP
Patient supine with head resting on pillow and arms relaxed to the patient’s side
Long axis of patient co-incident with midline of the table
Anterior superior iliac spines (ASIS) equidistant to table top ensuring no rotation.
MSP of patient 90 degrees to table top.
Direct vertical central ray 90 degrees to level of lower costal margin in the midline
•Ensure alignment of patient to image receptor
•Expose on arrested respiration using 100cm SID
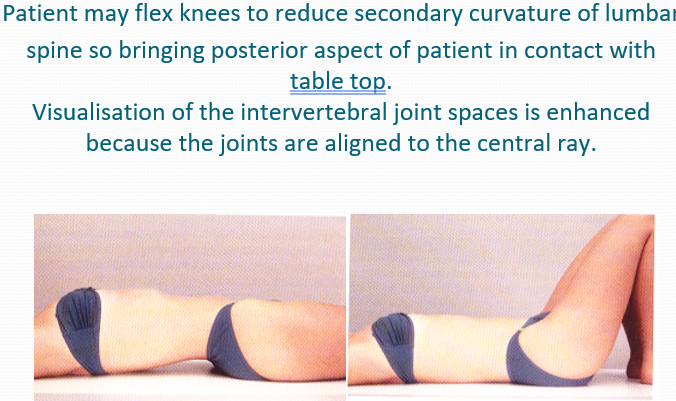
how do you reduce lumbar curvature
whats the image criteria for AP lumbar
Correct name and aspect marker
Correct area of interest to include T12 superiorly. Proximal 2/3 of sacrum and entirety of sacro-iliac joints inferiorly. Soft tissues lateral to lumbar spine (to exclude renal pathology)
Correct positioning to include
Vertebral bodies to co-incident with midline of image receptor.
Spinous processes central to vertebral bodies
Evidence of intervertebral joint space
Equal proportion of transverse process projected laterally from either side of vertebral bodies
No artefacts
Evidence of collimation
Need for repeats or further views
Correct exposure factors
Evidence of pathology
what would you consider when assessing the AP lumbar spine for pathology
Cortical outlines of the vertebrae should be intact and trabecular pattern comparable between each of the vertebrae
Size of vertebral bodies increases progressively from L1-L5
Interspinous distance should be approximately equal throughout the lumbar spine indicating no widening or loss of joint space
Spinous processes should be centralised throughout the lumbar spine indicating no disruption of the vertebral alignment.
Inter- pedicular distance should be virtually equal throughout the lumbar spine indicating no disruption of the vertebral bodies.
Pedicles and transverse processes should be symmetrical throughout lumbar spine indicating no disruption of the vertebral alignment.
No evidence of abnormal soft tissue outlines, which would indicate para-vertebral swelling.
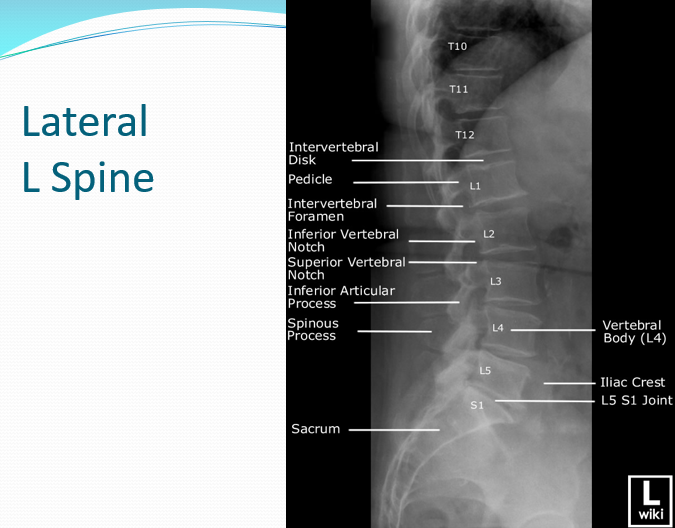
lateral L spine labelled xray
what’s the radiographic technique for lateral L spine
From supine position patient rolls onto affected side(posterior aspect of the patient facing radiographer)
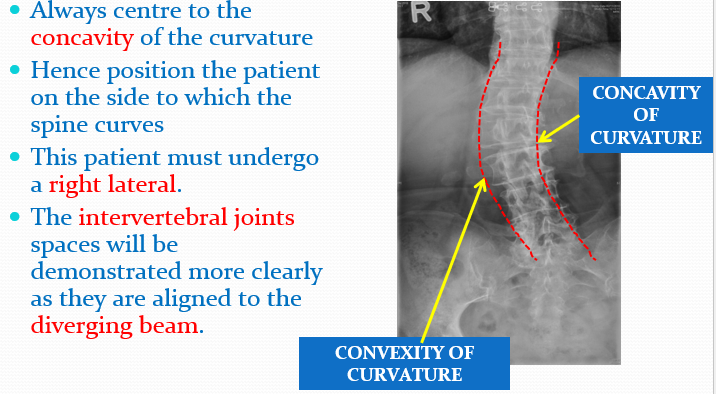
Unless the patient has scoliosis
Elbows flexed and patients arms resting anteriorly.
Patients shoulders and hips adjusted so they are in the same plane allowing the MSP is to be parallel to the table top
The long axis of the spine co-incident with midline of the image receptor.
Knees and ankles flexed to aid stability
Direct vertical central ray at 90 degrees to a point 7.5cm anterior to spinous process at level of lower costal margin using 100cm SID.
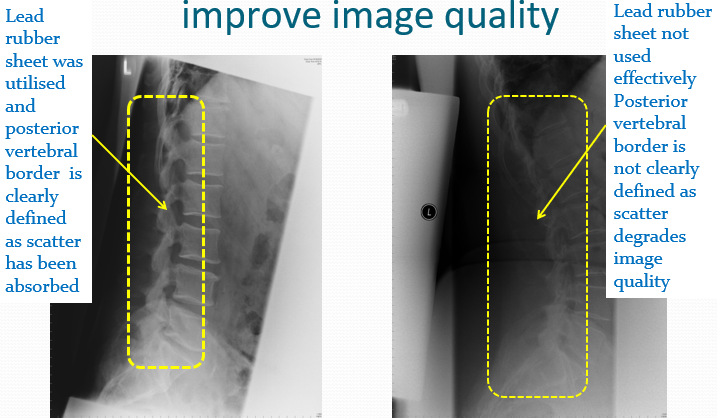
Lead-rubber sheet may be placed posterior to the lumbar region to improve the improve the image quality by absorbing scattered radiation.
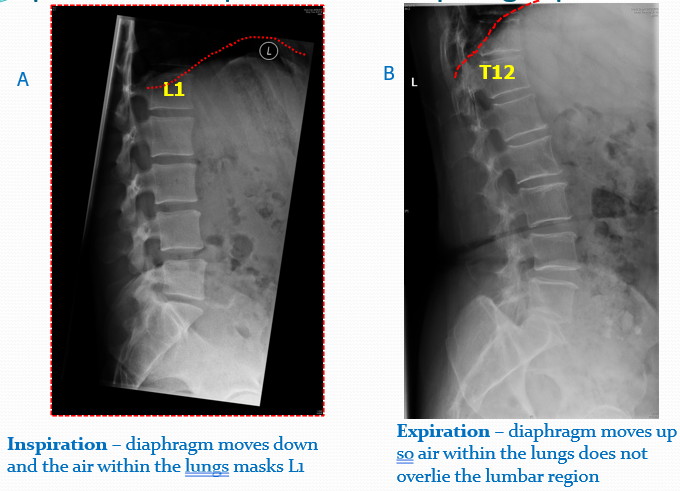
•The image should be taken on arrested expiration.
how does lead rubber improve image quality
how does inspiration and expiration affecr diaphragm positioning
decision on which lateral depending on curvature in scoliosis patients
lateral l spine image criteria
Correct name and aspect marker
Correct area of interest to include
T12 superiorly.
Proximal 2/3 of sacrum inferiorly.
Soft tissues anteriorly and posteriorly
following the curvature of the spine.
Correct positioning to include
Vertebral bodies to co-incident with midline of image receptor.
Superimposition of anterior posterior superior and inferior borders of vertebral bodies
Evidence of intervertebral joint space
Intervertebral foramina superimposed
No artefacts
Evidence of collimation
Need for repeats or further views
Correct exposure factors
Evidence of pathology
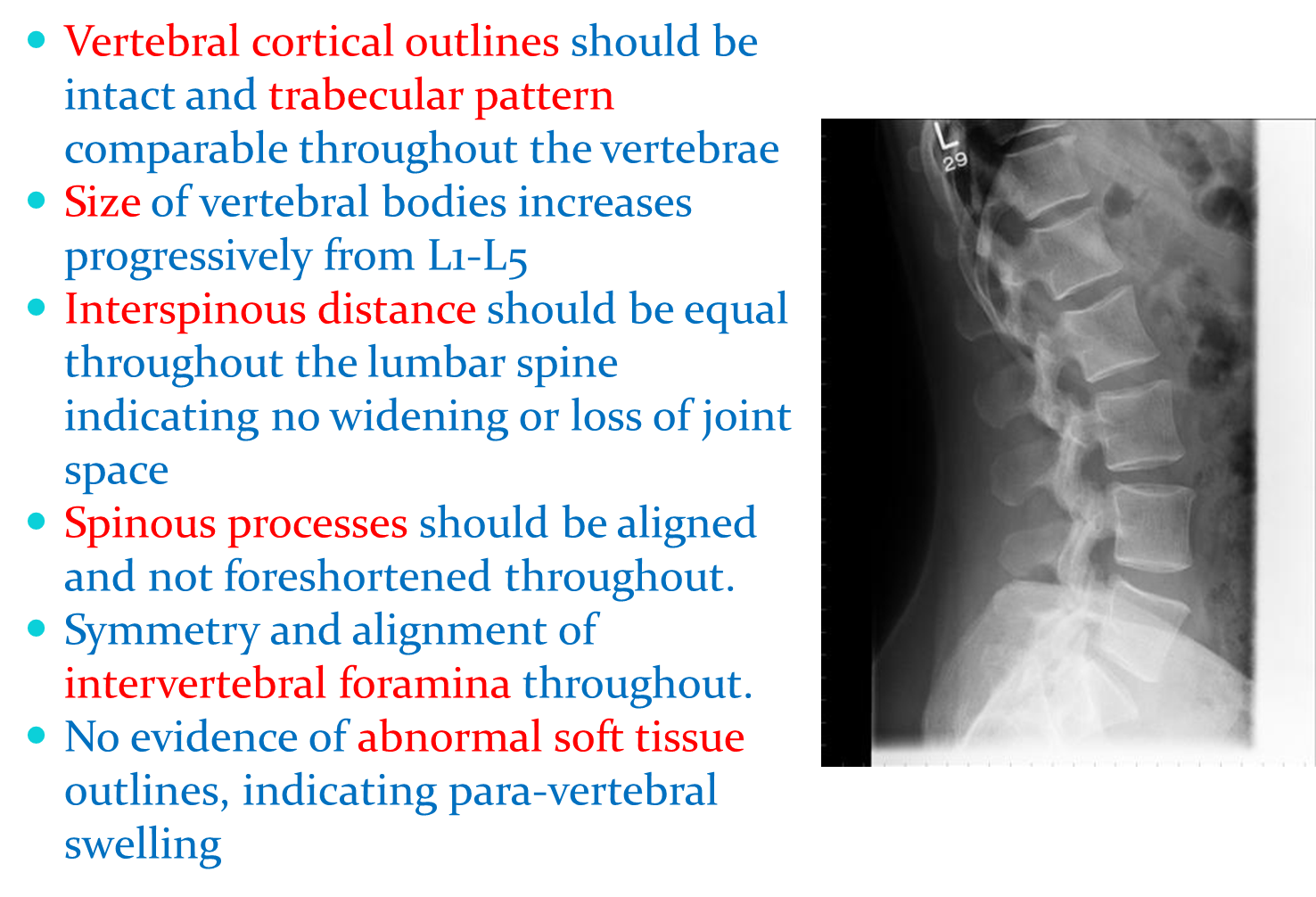
lateral l spine image assessment
Vertebral cortical outlines should be intact and trabecular pattern comparable throughout the vertebrae
Size of vertebral bodies increases progressively from L1-L5
Interspinous distance should be equal throughout the lumbar spine indicating no widening or loss of joint space
Spinous processes should be aligned and not foreshortened throughout.
Symmetry and alignment of intervertebral foramina throughout.
No evidence of abnormal soft tissue outlines, indicating para-vertebral swelling
L5-S1 Junction radiographic technique
From supine position patient rolls on to affected side
(posterior aspect of the patient facing radiographer)
Elbows flexed and patients arms resting anteriorly.
Patients shoulders and hips adjusted so they are in the same plane
allowing the MSP is to be parallel to the tabletop
The long axis of the spine co-incident with midline of the image receptor.
Knees and ankles flexed to aid stability.
Direct vertical central ray at 90 degrees to a point 5cm anterior to spinous process of L5 using 100cm SID.
Lead-rubber sheet may be placed posterior to the patient to improve the improve the image quality by absorbing scattered radiation.
The image should be taken on arrested expiration.
Image criteria for L5-S1 Junction
Correct area of interest to include
L4 superiorly.
Proximal 2/3 of sacrum inferiorly.
Soft tissues anteriorly and posteriorly
following the curvature of the sacrum
Correct positioning to include
Vertebral bodies and sacrum to co-incident with midline of image receptor.
Superimposition of anterior posterior superior and inferior borders of vertebral bodies and sacrum
Evidence of intervertebral joint space L4/L5 and L5/S1
Intervertebral foramina superimposed L4/L5 and L5/S1

image assessment for L5-S1 junction
Vertebral cortical outlines should be intact and trabecular pattern comparable throughout the L4/5 and sacrum
Size of sacrum decreases progressively from S1-S5
No widening or loss of joint space L4/5 and L5S1
Spinous processes of L4 and L5 should be aligned and not foreshortened.
Symmetry and alignment of intervertebral foramina L4/5 and L5S1 .
No evidence of abnormal soft tissue outlines, indicating par-vertebral swelling
what is the radiographic technique for lateral sacrum
From supine position patient rolls on to affected side (posterior aspect of the patient facing radiographer)
Elbows flexed and patients arms resting anteriorly.
Patients shoulders and hips adjusted
so they are in the same plane allowing the MSP is to be parallel to the tabletop
The long axis of the spine co-incident with midline of the image receptor.
Knees and ankles flexed to aid stability.
Direct vertical central ray at 90 degrees to a point midway between the PSIS and the sacro-coccygeal junction using 100cm SID.
Lead-rubber sheet may be placed posterior to the patient to
improve the improve the image quality by absorbing scattered radiation.
The image should be taken on arrested expiration.
whats the image criteria for lateral sacrum
Correct area of interest to include
L5 superiorly.
Coccyx inferiorly.
Soft tissues anteriorly and posteriorly
following the curvature of the sacrum
Correct positioning to include
Sacrum co-incident with midline of image receptor.
Superimposition of anterior posterior superior and inferior borders of sacrum
Evidence of intervertebral joint space L5/S1
Intervertebral foramina superimposed L5/S1
what is the radiographic technique for PA sacro-iliac joints
Patient prone with head resting on pillow and arms placed to either side of head or relaxed to the patient’s side
Long axis of patient co-incident with midline of the table top.
Posterior superior iliac spines (PSIS) equidistant to table top ensuring no rotation.
MSP of patient 90 degrees to table top.
Direct central ray 10 - 15 ̊caudally to the level of the PSIS in the midline
•Ensure alignment of patient to image receptor
•Expose on arrested respiration using 100cm SID
PA sacro-iliac joints image criteria
Correct area of interest L5 superiorly. proximal 2/3 of sacrum inferiorly.
Medial 1/3 of iliac bones laterally
Correct positioning to include
Sacrum co-incident with midline of image receptor.
Superimposition of anterior posterior superior and inferior borders of sacrum.
Sacral foramina equal in size and shape
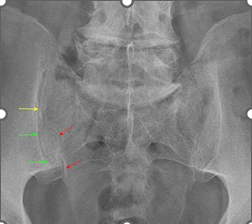
what’s the image assessment for sacrum and SI Joints
Remember ABCD
Vertebral cortical outlines should be intact and trabecular pattern comparable throughout sacrum
Size of sacrum decreases progressively from S1-S5
No widening or loss of joint space throughout sacrum or SI joint
Symmetry and alignment of sacral foramina
No evidence of abnormal soft tissue outlines, indicating para-vertebral swelling