311- Exam 4 (Sensory Perception/Alterations in Sensory Perception, Metabolic Syndrome)
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
143 Terms
Sensory Function
12 cranial nerves receive and transmit sensory data.
These nerves control both sensory and motor function for the head and neck.
Humans have 5 basic senses; sight, smell, hearing, taste, and touch.
Sensory perception= use of 5 senses, helps us interpret the environment.
Sensory Alterations
is the inability to see, smell, hear, taste, or feel are referred to sensory alterations.
These alterations can be caused by age, medications, injuries, neurocognitive disorders or disease.
Types of alterations include- Sensory deficit, Sensory deprivation, sensory overload, sensory processing disorder.
Sensory Deficit
A deficit in expected function of one or more of five sense.
Reduced function of senses. Inability to perceive stimuli, brain still receiving stimuli. But for some reason damage to sensory organ itself or other is blocking the brain from interpreting stimuli.
Sensory Deprivation
A reduction in or absence of stimuli to one or more of the five senses.
No stimuli or absence, injury to brain, stimuli present but not able to perceive it. Absence of stimuli due to reduced function of sensory organ.
-Stimuli is still present but absence of stimuli due to decreased function of organ.
Sensory Overload
Receiving stimuli at rate and intensity beyond the brain’s ability to process the stimuli in meaningful way.
Too much stimuli, patient can become anxious and depressed. Too much stimuli coming into brain constantly ongoing stimuli, suffering from or condition can lead to _.
Sensory Processing Disorder
When client appropriately detects sensory stimuli but their brain has difficulty interpreting and responding appropriately to stimuli.
Mostly identified in childhood, still some in adulthood. Presents in many different ways.
-Seen in children with attention deficit disorder and have trouble organizing/processing various stimuli in the brain. Can lead to difficulty interpreting stimuli around them. EX: ADHD, OCD, Autism.
Factors that Affect Sensory Perception Processes
Age Considerations= senses become dulled, increased risk of injury or infection and increased risk to fall.
-Hearing and vision are the senses most affected.
-Increased risk of eye infection and scarring, vision and hearing are fist to go.
Medication effects= Over 600 medications that can cause Ototoxicity(negative effect on our hearing and causes damage, can be permanent).
-Some medications cause alterations in taste. Bitter or metallic taste, alter overall ability to taste. Dry mouth overtime affect mucous membranes.
Cognitive Disorientation= Dementia and Delerium
Dementia vs Delerium
Dementia= progressive disease that effects neurons and sensory. No cure, Disease process that leads to damage of neurons of brain cells, can lead to brain cell death. Senses can be affected, changes in-hearing, vision, important be aware that senses can decline as well.
Delerium= more temporary, unaware of time and day. Reversible or temporary, disturbance in mental ability, for various reasons. Often due to major stress or trauma or condition they’re suffering from. Oftentimes reversible and lasts for hours or days, decrease in senses, perception of stimuli around them.
Structure of eye
External= eye muscles, upper and lower eyelids, sclera, conjunctive, lacrimal gland.
Internal=
-Iris= colored part of the eye, controlling the amount of light that enters through the pupil.
-Choroid= provides essential nutrients and oxygen to the outer retina.
-Ciliary body= produces the aqueous humor that fills the front of the eye and supplies nutrients
-Retina= capture light and translate it into electrical and chemical signals that the brain can interpret as images.
-Rods= used for low light, assist in detection of images in peripheral vision.
-Cones= allows for light to differentiate changes in color.
-Aqueous humor= clear, watery fluid in the front of the eye, provides= Nourishment, Waste Removal, Pressure Maintenance and Shape.
-Optic nerve= transmits visual information from the retina to the brain, enabling us to see.
Process of sight
Process of sight is for light to enter eye through cornea.
Light passes through pupil to lens and posterior to iris then onto Retina.
Rods (photoreceptors) and Cones located within Retina are responsible for receiving signals and processing them.
Then transmitting them to the brain through the optic nerve.
Refractive Error
Common eye conditions cause by change in the eye’s shape that prevents light from being focused properly to the retina, leading to blurred images or other abnormalities.
Types- Myopia, Hyperopia, Astigmatism, Presbyopia.
Myopia
Inability to see faraway objects clearly, also called Nearsightedness
Nearsightedness, difficult or unable to see far away. Can also suffer from Hyperopia.
Hyperopia
Inability to see nearby objects clearly, also referred to as Farsightedness.
Farsightedness, inability to see objects that are nearby.
-Myopia may also be present at same time.
Astigmatism
A defect in the eye making objects nearby and faraway look blurry or distorted.
a refractive error whereby the eye cannot focus light evenly on the retina, causing blurred vision or distortion.
Defect than makes objects that are nearby and far away look blurry or distorted.
Presbyopia
age related far-sightedness, or a gradual decrease in ability to focus up close or with small print. Usually middle age.
-Gradual decrease in ability for the eye to see nearby objects clearly and commonly begins during middle age or adulthood.
-Caused by loss of flexibility to the lens, and happens over time and due to aging.
Cataracts
A clouding of the lens of the eye that causes vision to be blurry, hazy, or less colorful. Cataracts are cloudy or opaque areas found on the eye lens. These areas alter the passage of light through the eye lens, which may cause painless blurred vision or glare. Cataracts develop as the lens becomes denser and less transparent due to proteins and fibers in the lens breaking down.
A clouding of the eye lens caused by proteins in eye breaking down and clumping together. Develops slowly in one or both eyes. Causes cloudy and blurry vision of eye.
-Difficult to see well at night and causes a glare, difficult to do ADL’s. Double vision is possible.
-Colors appear faded and yellowing. Aging other surgeries, patient with diabetes. Some causes are= previous eye surgeries, chronic disease (diabetes), most common in Aging.
Cataracts pathophysiology and risk factors
Alterations in vision due to lens becoming more dense and less transparent. Alters light passage to lens. Blurred or unclear vision, usually painless.
-Drying out or water loss in lens.
Etiology and Risk Factors= commonly related to aging. Injury, eye trauma, health conditions (diabetes), chronic hypertension, UV light, environmental toxins, family history.
Comorbidities= Anything that causes chronic inflammation. Chronic high blood pressure, Poorly managed diabetes. Psycosocial aspects of life. Like chronic infections, chronic hypertension, certain meds, post eye surgery, genetics, smoking, alcohol use, lifestyle.
Cataracts testing and treatments
Testing= No one test, should be examined by Ophthalmologist.
-Snellen eye chart typically assess first
-Ophthalmological examination= Affected lens is analyzed and risk factors, fundoscopy may also be performed, Slit-lamp biomicroscope.
Treatment- Surgical
-Extraction or removal of cloudy lens and replaced with implanted interocular lens (IOL).
Lab work that can be ordered= blood glucose, kidney function, CBC, BMP, and clotting time. Do they have any other comorbidities going on that lead to this.
Cataracts; Role of Nurse
Preoperative- consider medication that need to be held. Anti-inflammatory meds, health history, start/stop meds, make sure consent form signed.
Operative- eye drops to dilate pupils, consider anti-anxiety meds when appropriate. Patient usually awake, and assess vital signs.
Postoperative- when to contact provider, post-op medications, protective eye wear. Educate client on how to safe, meds needed (anti-inflammatory, antibiotics, and avoid certain things).
Determine environmental factors- history of altered visual perception, current visual accuity. Use Snellen eye chart to assess for changes in a client’s vision.
Client educations= safety, preventative care, lifestyle modifications. lifestyle modifications that should be implemented, including smoking cessation, alcohol reduction, and dietary changes that include an increase in leafy green vegetables. importance of medication compliance and its impact on the recovery process.
Safety considerations
Cataracts; Clinical Judgement
-Recognizing cues (Assessment)= signs that patient could be experincing- clinical manifestations like; blurred vision, double vision, cloudiness to eye. Using a Snellen eye chart, recognize that blurred vision, double vision, difficulty seeing at night, or difficulty reading prescription bottles or food labels are indicators of cataract development.
-Analyze cues (Analysis)= indication of cataracts and risk of injury. Painless hazy vision is indicative of cataracts.
-Prioritize Hypothesis (Analysis)= safety and daily living, high risk for falls or mobility.
-Generate solutions (Planning)= address safety; create safety plan.
-Take Action (Implementation)= consider post-op needs such as medications or UV light protection.
-Evaluate Outcomes (Evaluation)= progressive improvement of vision (8 weeks post-op). Safety and improve ADL’s. Clients should experience progressive visual improvements approximately 8 weeks following cataract removal surgery.
A nurse is providing postoperative medication teaching to a client who had bilateral eye cataract extraction surgery. Which medications should the nurse include in the teaching?
Select all that apply.
a. Antibiotic eye drops
b. Steroid eye drops
c. Anti-inflammatory eye drops
d. Beta blockers
e. Alpha agonist eye drops
a. Antibiotic eye drops
b. Steroid eye drops
c. Anti-inflammatory eye drops
A nurse is providing preoperative teaching to a client who is scheduled for bilateral eye cataract extraction surgery. Which of the following instructions should the nurse include in the teaching?
a. “You will need to remain in bed for one week following the surgery.”
b. “You will need to stop taking aspirin one week before the surgery.”
c. “You may begin your normal exercise routine after the surgery.”
d. “You may continue to wear your prescribed contact lenses that were worn prior to the surgery.”
b. “You will need to stop taking aspirin one week before the surgery.”
A nurse is teaching a client who is an older adult about eye health. Which of the following instructions should the nurse include?
a. Increase the amount of fruits and green leafy vegetables in their diet.
b. Get an eye exam every 3 years.
c. Monitor their cholesterol levels every year.
d. Wear scratch-resistant sunglasses and baseball hats.
a. Increase the amount of fruits and green leafy vegetables in their diet.
Glaucoma
Increased in intraocular pressure on optic nerve due to buildup of fluid, or aqueous humor, that causes compression of optic nerve, progressive disease, condition that can alter vision.
Types include= Open-angle or wide-angle (gradual development) and Angle-closure or narrow-angle(sudden onset, emergent treatment required).
Manifestations=
-Early- blurry vision or halos around lights
-Later progression- worsening peripheral vision.
Risk factors= age (common cause), family history, and trauma or injury. Black and Hispanic clients are at increased risk.
Comorbidities= chronic disease that causes inflammation and lead to increase in optic nerve. Hypertension, diabetes and hyperlipidemia. Elevated arterial pressures and hardening or blockages of blood vessels caused by these medical conditions may be related to the development
Impact on overall health= decreased quality of life, vision loss, health promotion and disease prevention, reducing independence, annual eye exam can help prevent these.
Open-angle or wide-angle
most common, gradual development, most common type and develops slowly and painlessly.
-the drainage angle formed by the cornea and iris remains open; however, the trabecular meshwork responsible for draining aqueous humor becomes inefficient, leading to a gradual increase in IOP. This form of glaucoma is often asymptomatic until significant vision loss has occurred.
Angle-closed or narrow-angle
sudden onset, emergent treatment required.
-Involves a sudden blockage of the drainage angle, which causes a rapid rise in intraocular pressure. This is considered a medical emergency. Clients may experience acute symptoms such as eye pain, headache, nausea, sudden vision loss, and visual disturbances like halos around lights.
Glaucoma; Testing and Treatment
Testing=
-Tonometry= frequent monitoring interocular pressure. Screening as part of regular eye exam, When eye pressure is high or if optic nerve looks abnormal. Provider measures the cornea thickness.
-Visual field testing (perimetry)= assessing central field and peripheral to see if their is any vision loss.
Treatment=
Non-surgical= medications are usually 1st treatment option. does not prevent but reduces progression. Aim to lower intraocular pressure.
-Meds= Alpha antagonists, beta-blockers, carbonic anhydrase inhibitors, prostaglandin analogs.
Surgical= more last resort or emergency.
-Laser trabeculoplasty- uses target lasers to drain angle tissue, helps with fluid flow of aqueous humor fluid and decrease pressure. Least invasive, lower intraocular pressure.
-Trabeculectomy- last resort. Creation of drainage flap, fluid flows into vascular system, used of laser trabeculoplasty does not work. More involved and more invasive.
Glaucoma Medications
Alpha antagonists- reduce aqueous humor production and increase the amount of fluid drained from the eye.
Beta-blockers- inhibitors decrease the volume of aqueous humor created by the eye.
Carbonic anhydrase inhibitors- inhibitors decrease the volume of aqueous humor created by the eye.
Prostaglandin analogs- improve the amount of fluid drainage from the eye.
Glaucoma: Role of the Nurse
Determine environmental and Individual factors, asses client. Lifestyle behaviors, including adherence to prescribed medications, smoking, and general health practices, can affect disease progression and response to treatment.
-History of altered visual perception. Visual accuity= assess for any signs that the patient might have glaucoma.
Client Education- Progression of Glaucoma (provide education), Safety consideration (set up at home and reduce risk of falling), Lifestyle modifications (protective eyewear). Surgical and postoperative client education (what they need to prepare). Medication (side effects, use of meds, adminsitration, prevent infection.
Glaucoma; Clinical judgment
Recognize cues (assessment)- is very important to determine treatment, assess visual acuity.
Identify subtle early symptoms. Clients may report mild eye discomfort, such as slight redness or itchiness, occasional puffiness of the eyelids, or intermittent excessive tearing. Intermittent blurred vision or noticing halos around bright lights
Analyze cues= increased interocular pressure and difficulty reading, what has decreased quality of life.
Manifestations of blurred vision, seeing halos around lights, and decreased peripheral vision in conjunction with elevated intraocular pressure above 21 mm Hg are indicative of glaucoma.
Prioritize Hypothesis (analysis)= prevent progression, ensure safety, at risk for falls.
Treatment will be lifelong and will require frequent monitoring of intraocular pressures. Treatment options will not reverse lost vision but are aimed at preserving the remaining vision and preventing further damage
Generate solutions (planning)= address safety and treatment needs.Treatment and nursing intervention planning will focus on decreasing intraocular pressure to prevent further injury to the optic nerve.
Take action (implementation)= ensure safety- pre and post-op. Providing information on appropriate medication administration is a priority nursing intervention for clients who have glaucoma.
Evaluate outcomes (evaluation)= progressive improvement of vision, frequent monitoring of intraocular pressure and assessments of the effects of prescribed medications.
Sort the following items into risk factors for cataracts, glaucoma, or both.
Drag the options on the left to their match on the right (or match pairs by first selecting the option on the left and then selecting its match on the right).
-Cataracts
-Glaucome
-Both
Cataracts- Overexposure to sun or UV rays, Excessive alcohol use, Smoker, Steroid use.
Glaucoma- Black or Hispanic client, Severe nearsightedness
Both- History of diabetes mellitus, Family history, Previous eye surgery, History of cardiac disease
A nurse is caring for a client who has glaucoma. Which of the following manifestations should the nurse expect?
a. Client reports having blinds spots in the center of their visual field.
b. Client reports seeing halos around lights.
c. Client reports vision appears hazy.
d. Client reports sudden onset of flashes of light.
b. Client reports seeing halos around lights.
A nurse is providing postoperative discharge teaching to a client who had laser trabeculoplasty surgery. Which of the following instructions should the nurse include in the teaching?
Select all that apply.
a. Resume normal physical activities.
b. Notify provider if they have manifestations of infection.
c. Take showers instead of baths.
d. Do not drive until they have a follow up appointment with provider.
e. Wear dark UV sunglasses when outdoors.
b. Notify provider if they have manifestations of infection.
d. Do not drive until they have a follow up appointment with provider.
e. Wear dark UV sunglasses when outdoors.
Macular degeneration
Also called age-related macular degeneration(AMD). An irreversible degeneration of the macula that leads to loss of central vision as clients age.
Match the following vision alterations with their correct definitions.
-Diabetic retinopathy
-Myopia
-Gluacome
-Atigmatism
-Hyperopia
-Presbyopia
-Cataract
-Diabetic retinopathy= Damage to blood vessels of retina due to diabetes.
-Myopia= Inability to see faraway objects clearly, also known as nearsightedness.
-Gluacoma= Increase in intraocular pressure compresses the optic nerve causing loss of peripheral vision.
-Atigmatism= A defect that causes both nearby and faraway objects to appear blurry.
-Hyperopia= Inability to see nearby objects clearly, also known as farsightedness.
-Presbyopia= Inability to see nearby objects clearly, often age-related.
-Cataract= Condition where lens of eye becomes cloudy, causing blurry vision.
Diabetic Retinopathy
Affects blood vessels in the retina causing blindness.
Caused by poorly managed Diabetes mellitus. Ensure and educate importance of managing diabetes. Providing with proper materials and stress importance of annule eye exams.
Affects blood vessels in retina and can lead to vision loss and complete blindness. Manifestations= general decline in vision spots or floaters, blurred vison.
-Can lead to glaucoma, high glucose, smoking, unhealthy diet. Leading cause of blindness in adults.
Risk factors= poorly managed diabetes mellitus, smoking, 2 to 5 times more at risk for cataracts, twice the risk of having open-angle glaucoms. Anything that can increase inflammation in body.
Diabetic Retinopathy diagnostic testing
Ophthalmologic. exam= visualization with slit lamp.
-Assess for swelling for bleeding vessels in retina.
-Scar tissue or other abnormalities of optic nerve. Assess overall health history
Diabetic Retinopathy: Clinical Judgement
Recognize cues (Assessment)= assess visual acuity and management of diabetes mellitus.
Analyze cues= based on cues and clinical manifestations, risk factors.
Prioritize Hypothesis= client safety and preserving remaining vision/preventing further damage
Generate solutions (planning)= plan interventions that support proper blood glucose management and appropriate lifestyle changes.
Take action (implementation)= create safety plan
Evaluate outcomes (Evaluation)= frequent monitoring of progression of eye conditions and diabetes mellitus.
Age-Related Macular Degeneration (AMD)
Involves buildup of photoreceptors waste products called Drusen. Drusen accumulates under the Retina. 2 Types= dry and wet
Retina is unable to function properly= blurred vision, distorted in center if eye field, and irreversible blindness and vision loss.
Risk factors= age(over 65), smoking, hypertension, obesity, family history (twice likely if parent was diagnosed). Elevated cholesterol levels, lighter skin or eye color at higher risk.
Comorbidities= Involve cardiovascular conditions, renal conditions, clients at higher risk for stroke or Myocardial infaction, hypertension, hyperlipidemia.
Impact on overall health- effects vision changes can have effects on ADL’s, lead to significant level of depression and anxiety. lead to higher risk of falls, impaired mobility.
Dry type AMD
Most commonly diagnosed and causes outer portion of retina to break down and develop areas with increased accumulation of drusen
most common, more graduale, blurring of vision, and altered night vision.
-Involves breakdown of under retina.
Wet type AMD
Triggered by abnormal growth of blood vessels underneath the retina, the vessels leak blood and fluid under the center portion of retina(macula) causing distorted vision.
Rapid and abrupt onset, sudden blurred vision and blind spots.
Leakage of waste products under retina, more rapid, and severe.
Involves leakage of blood underneath macula and potential vision loss.
Age-Related Macular Degeneration (AMD); Testing
Usually done during Opthamology exam, due to vision changes, Goal is to identify changes in the Macula. Opthamologist are usually looking for deposits of Drusen or bleeding.
Assessment with opthalmoscope or ondoscope.Involves dilating the pupils and looking at back of eye.
Also Fluorescein Angiography may be used.
-Fundoscopy(dilate pupils with medicated drops to see rear of eye) or opthalmoscopic examination= with dilation, fundus is visualized.
-Fluorescein Angiography= measures adequacy of blood flow to eye, changes with retina sometimes impact blood flow to retina.
Age-Related Macular Degeneration (AMD); Diagnostic studies and Treatment
-Fundoscopy(dilate pupils with medicated drops to see rear of eye) or opthalmoscopic examination= with dilation, fundus is visualized.
-Fluorescein Angiography= measures adequacy of blood flow to eye, changes with retina sometimes impact blood flow to retina.
No cure but intake of carotenoids Lutein and Zeaxanthin can slow progression. Goal is to slow progression. Explain differenced in wet and dry type, and slowing progression
Treatment for visual changes to wet AMD.
-Anti-vascular endothelial growth factor= slow progression of abnormal vessels.
-Photodynamic therapy= laser therapy that aims to eliminate abnormal blood vessels, improves blood flow.
provide clear guidance on lifestyle modifications, including smoking cessation, heart-healthy dietary changes, management of chronic conditions like hypertension,
AMD: CNS and Impaired mobility
Clients with AMD are at higher risk for: Narrowing and thickening of carotid arteries (risk for stroke), Hypercholesterolemia, Hyperlipidemia, Increased bulidup of blood vessel plaque.
Higher risk for developing central nervous system health conditions, such as stroke. Higher risk for falling and potential for hip fractures.
AMD increases the probability of impaired mobility secondary to poor vision and fear of injury or falls.
Which of the following home environment changes would the nurse suggest to improve safety for this client?
Select all that apply.
a. Place area rugs over hardwood floors.
b. Remove floor lamps.
c. Apply floor tape to extension cord plugged into television.
d. Place the dog’s bed next to client’s recliner chair.
e. Move magazine collection in a tote next to the kitchen table.
b. Remove floor lamps.
c. Apply floor tape to extension cord plugged into television.
AMD: Role of the Nurse
Determine environmental factors= history of altered vision perception, and vision accuity- encourage use and at home setting. Assess using Snellen eye chart.
Client education- safety and lifestyle modifications. Provide specialized acuity tools
Safety considerations- educate client, remove tripping or falling hazards.
Treatment- Lifestyle modifications (stop smoking, reduce cholesterol, manage other chronic health conditions to reduce progression). Photodynamic therapy (PDT) to slow progression, and Pharmacology( everything should be labeled).
AMD: Clinical Judgement
Recognizing cues (assessment)= diminished central vision, report any changes like blurriness, dark spots, or difficulty recognizing faces. identification of risk factors such as increasing age, smoking history, family history of AMD, poor diet, and cardiovascular comorbidities.
Analyze cues= indicators for AMD and risk of injury or falls, if dry or wet type. Gradual blurring of vision with decreased night vision and diminished central vision can be indicative of dry AMD. In contrast, a sudden blurring of vision or blind spots that have appeared in the center of the visual field can indicate wet AMD.
Prioritize hypothesis= safety in home enviroment and independence
Generate solutions (planning)= delvelop home safety plan- reduce risk for injury. Collaborate with multidiscplinary plan of care.
Take action (implementation)= education, For both dry and wet AMD, the goal of treatment is to slow the progression of vision loss and to quickly identify when further changes to visual perception have begun to occur. Amsler grids are used in the home setting to monitor a client’s progression of central visual field loss.
Evaluate outcomes= safe home environment
A nurse is teaching a client who has macular degeneration about ADLs that may become more difficult to perform as the condition progresses. Which of the following will the nurse include in the teaching?
Select all that apply.
a. Showering
b. Driving
c. Reading a book
d. Listening to music
e. Typing on the computer
b. Driving
c. Reading a book
e. Typing on the computer
Retinal Detachment
A visual disorder that occurs when the retinal tissue detached from blood vessels that provide oxygen and nourishment to the retina in posterior eye.
Retina separates from blood vessels. Multiple causes= age, eye injury/trauma, previous eye surgery, eye infections, and fluid build-up. -Vitreous humor collapse, dark floaters or a sensation of a curtain being placed in the field of vision. This condition requires emergent treatment to improve visual sensory perception.
Clinical presentations= blurred or distorted vision, and photopsia or floaters.
Risk factors= age-related changes and family history, chronic conditions, diabetic retinopathy, Macular degeneration and cataract removal. Usually can be spontanous and predisposed.
Comorbidities= hypertension, diabetes, and conditions that can lead to chronic inflammation or build-up of pressure.
Impact on overall health= quality of life, increased stress, difficulty with ADL, and extensive recovery with surgical interventions.
Retinal Detachment: Testing and Treatment
Assess for detachment or leak of vitreous fluid, No specific blood tests that aid in the identification of retinal detachment. Blood work may be collected if surgical treatment is scheduled, especially for clients who have diabetes or are on anticoagulant medications.
-Opththalmoscope, slit-lamp, biomicroscope, fundoscopy. To visualize retina and severity of dettachment
Treatment= Prescibed anti-inflammatories, antibiotics, and pain meds.
-Retinal Reattachment- Scleral Buckle (band around eye)
Pars Plana Vitrectomy and Pneumatic Retinopexy= involve the insertion of an absorbable gas bubble into the vitreous chamber. The bubble applies gentle pressure to help promote reattachment of the torn retina, is very important. Promotes spontanous reattachment.
-Postoperative= eye shield, medication, lie facing down unless eating/bathing/bathroom up to 3 months. Avoid vigorous excercise/lifting more than 15 pounds, sunglasses when outdoors.
Recovery is very important.
Retinal Detachment: Role of the Nurse
Look at whole picture.
Environment and Individual Factors= medical history and vision changes or loss. Visual acuity assessment. Might need anxiety meds or assess holistically.
Safety considerations= home and daily living, rooms should be well-lit, floor free of clutter.
Client education= Ensure client has proper education on all care.
-Priority= pre and postoperative. Medications (pain or antibiotics) and ADLs
Match the vision change assessment with the correct eye condition.
Drag the options on the left to their match on the right (or match pairs by first selecting the option on the left and then selecting its match on the right).
-Glaucoma
-Macular degeneration
-Cataract
-Retinal detachment
1.Seeing floating dark spots moving through all vison fields
2.Diminished peripheral vision
3.Blurry or hazy vision
4.Blind spots in the center of the field of vision
Glaucoma-Diminished peripheral vision
Macular degeneration- Blind spots in the center of the field of vision
Cataract- Blurry or hazy vision
Retinal detachment - Seeing floating dark spots moving through all vison fields
A nurse is caring for a client who reports a loss of peripheral vision. Which of the following assessments will the nurse perform to assess peripheral vision?
a. Confrontational visual field test
b. Snellen’s visual acuity test
c. Tonographic examination
d. Dilated fundoscopic examination
a. Confrontational visual field test
Clinical Judgment: Retinal Detachment
Recognize cues (Assessment)= assess visual acuity, reaction to light, floaters. Pressure readings with retinal detachment are typically below 10 mm Hg due to the increase in fluid drainage.
Analyze cues= share findings of assessment with provider of possible retinal detachment. rapid onset of manifestations of blurry or distorted vision in combination with the presence of floaters or blind visual spots with the health care provider,
Prioritize Hypothesis (Analysis)= anticipate emergent situation, perform immediate visual assessments and to identify manifestations
Generate solutions (planning)= preparation of client for surgery
Take action (Implementation)= ensure safety- post-op and pre-op
Evaluate outcomes (evaluation)= improvement of vision may take several months until adequate healing of the retinal detachment has occurred.
A nurse is caring a client who reports a sudden onset of blurry vision with blind visual spots. Which of the following medications should the nurse anticipate the provider prescribing?
a. Anti-vascular endothelial growth factor medication
b. Dilating eye drops
c. Steroid eye drops
d. IV sedation
b. Dilating eye drops
How is sound produced?
Begins with noise or sound waves enter ear through auditory canal and hit eardrum, causing it to vibrate.
Vibration passess through ossical and amplify sound.
Then sound is transmitted to inner ear into cochlea, then converted to electrical impulses.
-Auditory nerves send them to the brain, where sound is then interpreted to brain.
Conditions that affect the ear
Hearing loss
-Trauma, inflammation, Cerumen occlusion/impaction, foreign body, otitis media, otosclerosis, and Ototoxicity(med can lead to this)
Tinnitus
Meniere’s Disease
Types of Hearing loss
-Sensorineural Hearing loss (SNHL)
-Conductive
-Mixed
Sensorineural Hearing Loss (SNHL)
Hearing loss that occurs from problems of either the inner ear or the vestibulocochlear (auditory) nerve (cranial nerve VIII)
Often permanent the result of damage, anything putting permarent pressure (trauma, constant loud noises, meds).Result of damage to cochlear hair follicle or auditor nerve(auditory nerve pathways are what transmit sound waves to brain)
Causes= Aging (presbycusis), Auditory tumor, Explosion/blast. Other trauma from conditions like; hear disease, diabetes mellitus, measles, meningitis.
-Noise-induced= more prevalent among adolescents and young adults from prolonged exposure to loud music/sound.
-Age-related or Presbycusis= usually bilateral and in adults 75 years or older.
-Ototoxicity= medications have adverse effects that cause damage to dysfunction of cochlea or vestibule. Tinnitus, dizziness, impaired balance.
Conductive Hearing Loss
Inability of sound to travel from the outer ear to the eardrum and middle ear.
Blocking soundwaves, from outer ear to middle ear. Usually treatable if treated, can lead to permanent damage if not fixed or chronic. Treated with antibiotics, anti-inflammatories, or surgery. Causes=
Result of external ear condition- fluid accumulation, object, allergies or ruptured eardrum, inflammation, trauma, and impacted earwax
Otitis media is inflammation in or accumulation of fluid in middle ear.
Otosclerosis is abnormal growth of bone in one or both ears. usually mid-adulthood.
Mixed Hearing loss
Involves both SNHL and Conductive hearing loss at the same time.
Causes= head trauma, infection, and genetic predisposition.
Hearing loss
Difficulty or loss of hearing- classic sign, might have problems localizing sound.
Etiology and Risk factors- age-related changes and genetics, prolonged exposure to noise and ototoxic meds
Comorbidities= anything with chronic inflammation or decrease blood supply to organs of ear.
-Decreased blood supply (diabetes) and inflammatory process (arthritis)
Impact on overall health- psychosocial and considerations of aging, health promotion, educate client, ensure client get hearing screening if any indications of hearing loss.
Hearing loss Testing
Screening- Whisper voice and Finger rub test= client closes/covers one ear and test other ear by whispering or rubbing finger next to ear.
-Audiologic testing= client identifies sound heard at different frequencies.
-Rinne Test= hearing test using tuning fork placed against mastoid bone (determine bone vs air conduction issue)
-Bone Oscillator Test= bone oscillator against mastoid bone while monitoring the response of auditory nerve to vibrations.
For newborn screening and patients who are unable to respond.
-Auditory brainstem response (ABR) test= The brain electrical activity in response to sound of clicking noises is measured via electrodes on scalp.
-Otoacoustic emissions (OAE) test= probe placed in ear canal emits sound, echo is recorded to assess response in inner ear.
Hearing loss Treatment
Depends on hearing loss and severity. Starts with least invasive.
1st- Occlusion of External Auditory Canal, removal of earwax.
- Hearing Aids- to amplify sound, less invasive.
-Medications(if needed) for infection or inflammation. Antibiotics, antifungals, and anti-inflammation.
- Surgical Intervention- eardrum repair.
Last resort= Cochlear Implants- surgical implant
Cochlear Implants for hearing loss
For severe hearing loss, damage to auditory nerve. Device that is implanted. By-passes inner ear to stimulate auditory nerve. Implanted behind ear and will directly stimulate auditory nerve. Help promote sound.
-Severe sensorineural hearing loss- direct stimulate auditory nerve.
-Preoperative care- medical history and baseline vital sign and premedicate antibiotics or anti-antiety.
-Operative care- preparation of surgical site.
-Postoperative care= monitoring, pain management. Patient education and signs of infection and treatment surgical site.
Role of Nurse= Hearing loss
Patient has access and support needed.
Environmental factors- interprofessional collaboration, determine factors that led to hearing loss.
Individual factors- communication alteration, assistive listening equipment/devices needed.
Safety considerations- increased risk for injury due to not hearing, ask home environment, prevent injury.
Client Education- meds, how to care, understand their role and responsibilities.
Hearing loss; Clinical Judgment
Recognize cues (assessment)- assess inner and outer ear
Analyze cues- impact on clients ability to effectively communicate.
Prioritize Hypothesis- Improve impaired communication.
Generate solutions (planning)- determine assistive hearing devices.
Take action (Implementation)- educate client on use of communication board.
Evaluate Outcomes (evaluation)- client demonstrates effective use of communication board.
Tinnitus
Hearing sound when no external sound is present, like ringing, buzzing, roaring, clicking, hissing, or humming noises.
Perception of sound when Not present- usually from underlying cause. Can be constant or intermittent. Can be mild to severe. -Disruption of auditory conduction, sounds, humming, or ringing noise. Look for underlying cause.
Risk factors= prolonged exposure to loud noise, age related hearing loss, chronic underlying health issues.
Comorbidities= Meniere’s disease or thyroid disorder.
Impact on Overall health= ADL’s and psycosocial, health promotion. Important to think about ways this can impact quality of life= decrease sleep, dizziness, imbalance, cause frustration and anxiety.
Auditory noises associated with reports of Tinnitus
Common noises that patients may hear;
-Constant ringing
-Loud buzzing
-Pulsating hum
-Low pitched roaring
-Clicking
-Hissing
-High pitched squealing
Tinnitus; Lab testing and Diagnostic
Has many causes, Goal is to treat Tinnitus is finding underlying cause.
Laboratory testing= anemia, thyroid, or heart disease, referred to audio test/exam.
Audiologic Examination- otoscopic exam, hearing testing.
Additional testing- Cranial nerve testing, CT scan or MRI= injury, trauma or tumor.
Tinnitus treatment
Patient is experiencing hearing loss along with_ , then managing might help get rid of _.
Treat Underlying cause;
-Hearing aids, dental treatment, medication changes.
Therapeutic management; therapies that can help client learn to cope/manage _.
-Cognitive behavioral therapy(client works to alter through pattern and emotional reactions), Tinnitus retraining therapy(education counseling specific to cause and cope mechanisms), acoustic therapy. TMJ- effect jaw and head.
Tinnitus role of the Nurse
Role of nurse is to be supportive
Obtain medical history- assess for environmental factors (gather info on clients health), signs of tinnitus
Individual factors- consider mental health concerns related to overexposure to loud noise, withdrawing from social situations.
Safety considerations- impaired sleep related to tinnitus.
Client education- lifestyle modifications like wearing ear protection when exposed to loud noises. How to reduce risk factors. Improve quality of life, educate on treatment that perscribed.
Tinnitus clinical judgement
Recognizing Cues (assessment)= determine onset of constant humming sound.
Analyze cues (analysis)= identify how change in sound perception relates to clinical presentation.
Prioritize Hypothesis= Safety, mental health
Generate Solutions (planning)= address contributing factors such as hypertension
Take Action (implementation)= control hypertension
Evaluate Outcomes (evaluation)= effectiveness of treatment in reducing episodes of tinnitus.
A nurse is preparing a client for diagnostic testing to evaluate for potential glaucoma. Which of the following tests should the nurse anticipate will be performed?
Select all that apply.
a. Fluorescein angiography
b. Measurement of intraocular pressure
c. Visual field test
d. Examination of the optic nerve with a slit lamp
e. Amsler grid test
b. Measurement of intraocular pressure
c. Visual field test
d. Examination of the optic nerve with a slit lamp
Fluorescein angiography is used to assess for diabetic retinopathy
Amsler grid test is used for age-related macular degeneration.
A client is discussing an audiometer test with a client. Which of the following statements should the nurse make?
a. “This test measures the brain’s electrical response to sounds.”
b. “You will wear headphones during the test.”
c. “You will be asleep during the test.”
d. “A small probe in your ear will measure the echoed response from your inner ear.”
b. “You will wear headphones during the test.”
Ototoxicity
Causing damage to or dysfunction of the cochlea or vestibule. Can get if increased when client takes more than one type of medications concurrently; NSAID’s, Antibiotics, Loop diuretics, Antihypertensives, Psychotropics, Antihistamines, Aspirin.
-Can cause SNHL, Tinnitus, dizziness or impaired balance
Meniere’s Disease
A hearing disorder caused from excressive bulidup of fluid in ear that leads to vertigo, tinnitus, and hearing loss.
Progressive disorder; at least 2 individual episoides of sudden onset of vertigo, hearing deficit verified by audiometry and tinnitus. -Vertigo so debilitating that effects ADL’s. Onset around 40 years old.
Excressive endolymphatic fluid, drainage in ear is not draining adequately. With these 3 aspects going on= Vertigo, tinnitus, Hearing loss.
Risk factors= Autoimmune disorder, recent viral infections, genetic predisposition
Comorbidities= migraine headaches, autoimmune disorders (rheumatoid arthritis, lupus, and ankylosing spondylitis)
Impact on overal health= ADL’s, can cause safety risk, increased anxiety, depression, cannot drive or work can significant impact patients life.
Meniere’s Disease common manifestations
-Vomiting
-Nausea
-Blurry vision
-Cold sweats
-Trembling
-Hearing loss
-Headache
-Imbalance
-Congestion in ear=fluid build-up
-Ear fullness
Meniere’s Disease; Diagnosis and Treatments
-Audiometric Assessment= to conform, typically unable to hear low tone. Assessing various tones that client can hear.
-Electronystagmography (ENG)= look at movement of eye, or uncontrolled movement of eye. Help determine if inbalance are related to brain or structure in ear.
-Electrocochleograpy (ECOG)= evaluate pressure in ears. helps determine endolymphatic fluid imbalance in ear.
Pharmacological= Diuretics(reduce fluid), Corticosteroids(reduce inflammation), Motion sickness and anti-nausea.
-Hearing aids, life-style modifications and stress reduction, vestibular rehabilitation and positive pressure therapy.
Meniere’s Disease role of the Nurse
Collect as much as possible to determine what clients unique needs are.
Environment factors- identify needs for client, and assess support system.
Individual factors= medical history to determine severity, meds patient is taking.
Safety considerations= risk for falls
Client education= dietary modifications (reduce sodium), stress reduction, side effects to look for, lifestyle changes- stop smoking.
Meniere’s Disease clinical judgement
Recognizing cues (assessment)= vertigo, hearing loss, tinnitus, pressure in ears.
Analyze cues= determine effects of clinical manifestations
Prioritize Hypothesis= risk of injury or falls.
Generate solutions (planning)= reduce episodes of vertigo and improve quality of life.
Take Action= monitor dietary salt intake and fluid balance.
Evaluate outcomes= severity and frequency of episodes of vertigo and tinnitus.
Speech Alterations
Have direct impact on clients ability to communicate. Communication is process that involves cerebration (thinking), cognition, hearing, speech production and motor coordination.
Disorders of speech= Aphasia, expressive, comprehensive, global.
Causes= brain injury, degenerative neurological disorder, dementia, or cerebrovascular accident (CVA) and stroke. Death of neurons.
Impact on health- can cause depression.
Testing= neurological testing, MRI of brain, Lab testing. Evaluation by speech pathologist.
Aphasia
A disorder that affects clients ability to articulate and understand speech and written language due to damage in brain.
Disorder that effect clients ability to articulate or understand speech due to damage on various parts of brain.
Expressive Aphasia
Broca’s or nonfluent aphasia and is due to damage to the frontal lobe of brain. A client who has Broca’s aphasia may understand speech but unable to speak the words they want to say.
Client not able to form words, nonfluent, damage to broncha/front part of brain. Patient understands speech but unable to communicate what they want to say.
Comprehensive Aphasia
Wernicke’s or fluent aphasia, caused by damage to temporal lobe of brain, A client who has Wernicke’s aphasia speaks in long sentences that have no meaning and often include unnecessary and made-up words.
Long sentances but don’t make sense or no meaning. Damage to temporal lobe of brain.
Global Aphasia
Severe impairments in communication caused by significant damage to various language areas of the brain. Clients who have this type of aphasia have poor comprehension of language and may be unable to form words or sentences.
Combination of types of Aphasia. severe impairment, damage to various parts of brain. Involves damage to comprhensive, and not able to communicate.
Speech Alterations; Role of the Nurse
Is to be supportive and encourage independence. Allow extra time to communicate with client. Exhibit patients
Encourage client to take their time when speaking, avoid interrupting client or finishing their sentences.
Assist client to communicate by using picture boards, and computer or tablet, paper/pen.
Encourage client to actively participate in speech therapy if prescribed. Follow laryngectomy, client might lose ability to speak. Artificial larynx or electrolarynx
Alterations in Touch- Tactile’s
Is the sensation on the skin that results from contact between skin and object. Types;
-Tactile Hypersensitivity= being over sensitive to stimulation or touch.
-Tactile Defensiveness= severe sensitivity to touch, patient can percive touch as severe physical pain.
-Tactile Hyposensitivity= lack of response to tactile stimulation. Under-responsiveness to tactile stimulation.
-Spinal cord injury= can be partial or complete loss of sensation of touch, from trauma or injury to spinal cord.
Diagnostic testing= Neurological and physical assessment, imaging, Nerve conduction velocity testing (EMG)- determine nerve conduction.
Impact on health= impact on social situations and interpersonal relationships.
Alterations in Touch- Neuropathy
-Peripheral Neuropathy= Conditions that occur when nerves in central nervous system become damaged resulting in numbness, pain, and weakness to extremities.
-Diabetic Neuropathy= Nerve damage that occurs in clients who have diabetes mellitus due to high blood glucose levels and high triglycerides, cause damage to nerves and small blood vessels supplying blood to nerves.
-Idiopathic Neuropathy= Neuropathy due to nerve damage of unknown cause.
-Spinal cord injury= can be partial or complete loss of sensation of touch, from trauma or injury to spinal cord.
Diagnostic testing= Neurological and physical assessment, imaging, Nerve conduction velocity testing (EMG)- determine nerve conduction.
Impact on health= impact on social situations and interpersonal relationships.
Alterations in Touch: Role of Nurse
Educate client to avoid activities that increase risk of spinal cord injury. Other safety education to minimize fall risk.
Educate clients who have decrease in absence of sensation in their lower extremities about foot care and inspecting feet daily.
How to avoid injury to feet or toes and wear closed-toe shoes and avoid walking barefoot, Provide education about water temp safety to avoid extreme hot or extreme cold.
Clients who have diabetic neuropathy and should follow dietary instructions and take all meds.
Alterations in Taste
Olfactory and Taste are related.
Protective sense= taste cells are known as Gustatory cells, olfactory sensory neurons.
-Phantom taste perception(persistent, foul taste when mouth is empty)
-Hypogeusia( decrease ability to taste)
-Ageusia( inability to taste anything)
-Dysgeusia(persistent salty, rancid, or metallic taste is said to have it).
Gustatory cells
Taste cells that contain specific receptors that allow for differentiation between sweet, sour, bitter, salty, or savory flavors.
Alterations in Olfactory
Olfactory and Taste are related.
Protective sense= taste cells are known as Gustatory cells, olfactory sensory neurons.
-Anosmia= inability to smell anything
-Hyposmia= reduction in ability to perceive odors
-Parosmia= Alteration in odor perception or a distortion in smells such as when past pleasant smells become unpleasent.
-Phantosmia= Sensation of odor that isn’t there
For each of the following types of medications, select the senses that can be impacted when taking that medication.
-NSAID’s
-Antibiotics
-Loop Diuretics
-Antihypertensives
-Psychotropics
-Antihistamines
-Aspirin
-NSAID’s= hearing and taste
-Antibiotics= hearing, smell, and taste
-Loop Diuretics= hearing
-Antihypertensives= taste
-Psychotropics= taste
-Antihistamines= hearing, sight, smell, and taste
-Aspirin= hearing
A nurse is caring for a client who reports a recent change in smell and taste. Which of the following actions should the nurse take?
a. Instruct the client to keep a food diary for one week.
b. Encourage the client to add more seasonings to their food.
c. Recommend the client to stop all medications for one week.
d. Ask the client about any recent illnesses or injuries.
d. Ask the client about any recent illnesses or injuries.
Alterations in Olfactory and Taste; Role of the Nurse
Educate to maintain smell/taste.
Actions that can decrease risk of smell and taste disorders;
-Maintain proper dental hygiene since dental caries can cause alterations in taste, Avoid activities that increase risk for head injury or use safety measures, smoking cessation.
Instruct client to chew slowly and season foods with spices to enhance flavor. Ensure client has smoke detectors in their home. Reduce number pollutants in their home and ensure there is adequate ventilation.
Alterations in Olfactory and Taste; Testing and Treatment
Testing= physical assessment including review of medical history, Referral to ENT, Imaging, and taste or Smell Tests.
Treatment= protective senses, Taste cells are known as Gustatory Cells.
-Send signals to brain once stimulated, Receptors differentiate between sweet, sour, bitter, salty.
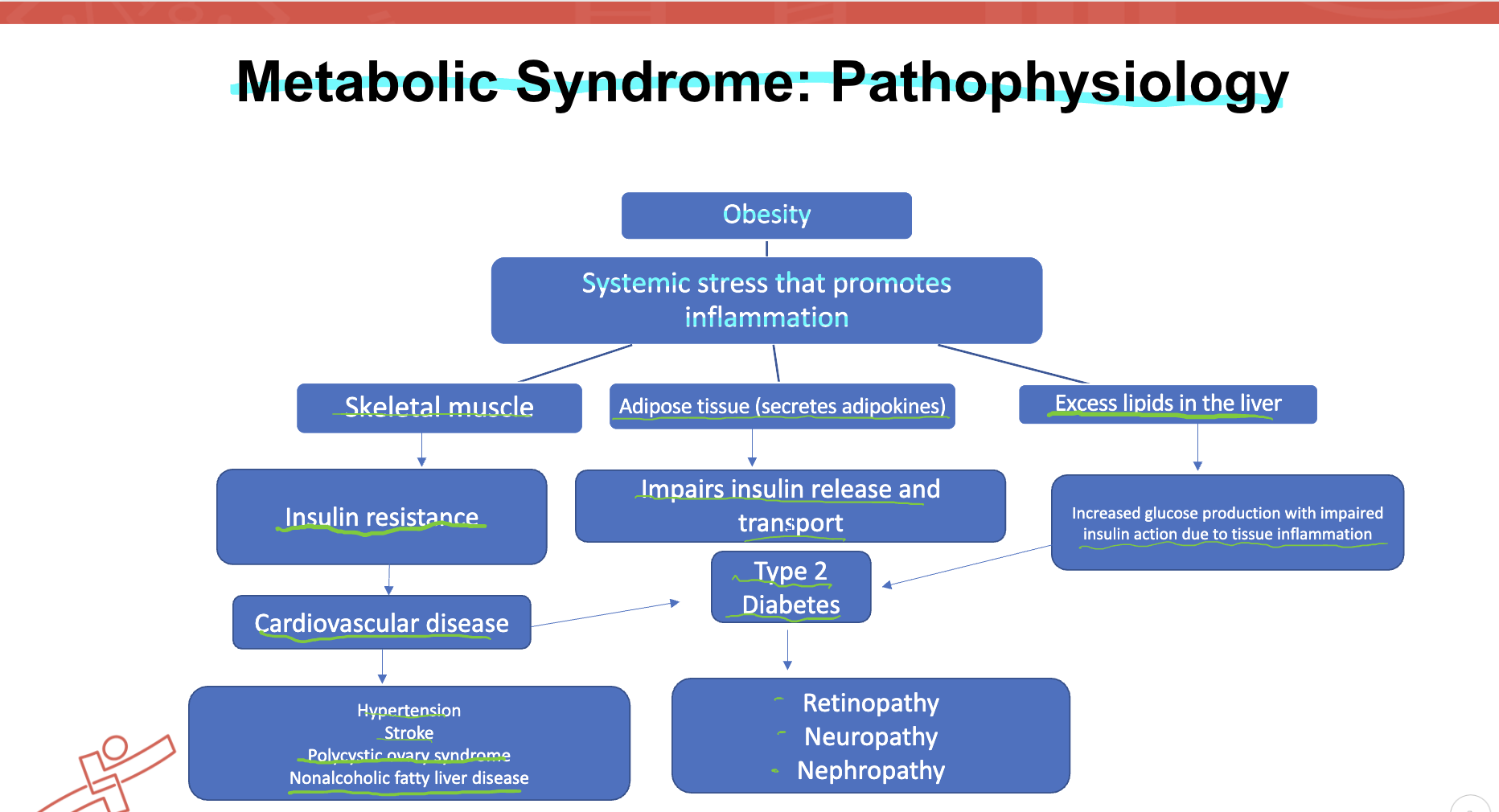
Pathophysiology of Metabolic syndrome
Criteria for _ syndrome= Elevated; blood pressure, glucose, and cholesterol.
Disorders that result= hyperglycemia, hypertension, hyperlipidemia, elevated plasma triglycerides, low HDL-cholesterol, and central obesity.
If untreated this group of disorders or cardio-metabolic risk factors, lead to DMT2 or cardiovascular disease, stroke.
The main feature of _ syndrome is insulin resistance(resistance to hormone insulin, results in increase in blood glucose levels) which can also be seen in DMT2.
Metabolic System; Risk factors
3 criteria- high glucose levels, hypertension, and high cholesterol
-Central obesity, family history, increased age, sedentary lifestyle, unbalanced diet, sleep apnea, stress, low HDL levels, Hypertension, and Inflammation.
Metabolic Syndrome: Complications and Comorbidities
Insulin resistance
Hyperglycemia
Neuropathy
Blindness
Cardiac arrhythmia
Neurological disorder
Polycystic ovary syndrome
Cancer
Cardiovascular disease
Stroke
Problems with dental and eyes can occur.