Adults II exam 2 review
1/116
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
117 Terms
What’s the difference between the right and left lung?
The right lung has 3 lobes while the left has 2
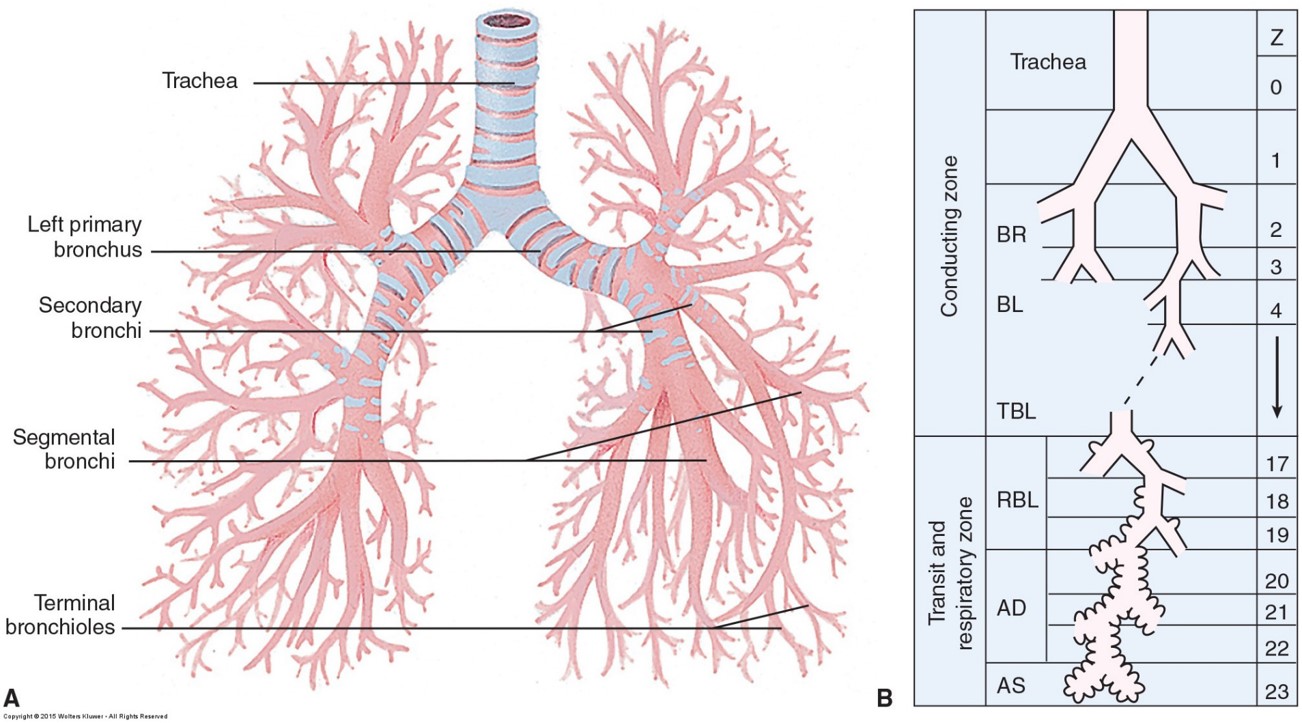
What are the primary structures of the lung?
Primary bronchi, secondary bronchi, segmental bronchi, terminal bronchioles, alveoli, pleurae
Why would disruptions to the pleural lining of the lung be an issue?
The lungs are free-floating (visceral and parietal pleura) and it’s the surfactant that maintains the surface tension that keeps the lungs expanded. So if there’s something that disrupts the lining, the lungs can collapse
What are the two types of circulations in the lungs?
Pulmonary:
It’s when deoxygenated blood flows through the pulmonary artery into the lungs and oxygenated blood comes from the lungs out the pulmonary vein
It’s main purpose is cardiovascular circulation
Bronchial
It’s how the lungs perfuse themselves through the bronchial arteriole from the aortic branch
Bronchiole veins also empty some deoxygenated blood with oxygenated blood
It’s main purpose is to support to the airways and to warm and humidify air
Define the breathing process
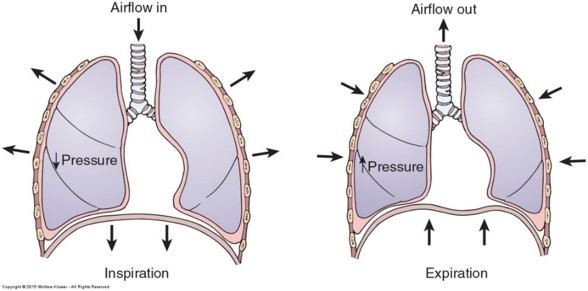
When a person inhales, the diaphragm contracts and moves downward. The intercostal muscles also contract which increases the volume in the lungs. This decreases pressure (negative pressure) and allows air to come in passively. During relaxation, the muscles all relax which forces air out of the lungs (positive pressure)
How is respiration controlled?
The pons and medulla in the brainstem regulate breathing
Breathing can also be autonomic and voluntary depending on the situation
The depth and rate of ones breathing can be affected by stretch receptors
What’s the difference between ventilation, perfusion, and diffusion?
Ventilation: movement of gas/air into and out of the lungs (physically breathing in and out)
Normal minute volume is 5-8 L per min
Perfusion: getting blood through the pulmonary circuit and into the alveoli so gas exchange can occur
Diffusion: movement of gas into tissues
Dependant on ventilation and perfusion
What occurs with restrictive lung diseases?
Inhalation is restricted d/t a physical restriction. As a result, there’s improper INFLATION/EXPANSION of the lungs since the alveoli can’t properly inflate, so the lungs are stiff and non-compliant
Ex. neuromuscular disease, trauma, obesity, deformity (scoliosis), fibrosis (scarring of lung)
What occurs with obstructive lung diseases?
The ventilation is good, but there’s a problem with expelling air (air trapping). Air can come in, but it can’t leave, so a person begins to get hypercapnic and hypoxic
Ex. asthma, COPD
What occurs with a compromise of diffusion?
Obstruction in the alveoli usually d/t fluid inhibits gas exchange
Ex. infections, drowning, edema, ARDS
What are common manifestations of respiratory issues?
•Neuro: confusion, lethargy, dizziness, loss of consciousness
•CV: tachycardia which can transition to bradycardia (indicates a person is at a crisis point)
•Resp: tachypnea, dyspnea, wheezes, crackles, diminished breath sounds
•GI: possible n/v
•GU: possible oliguria
•Integ/Musc: weakness, paresthesia, possible cyanosis and delayed capillary refill
Why is a person tachycardic at first then bradycardic?
Where’s there’s less O2, the body is going to try and pump what O2 is left to compensate, so it becomes tachycardic. But, as the compensation starts to wear out, the person becomes bradycardic
What’s the purpose of labs taken for respiratory issues?
Chem panel: look at K and Na
CBC: look at WBC for possible infection and Hgb/Hct for anemia
ABGs: determine pH and CO2 levels
Sputum examination: inspect for possible infection
What’s the purpose of a bronchoscopy and pulmonary function test (PFT)?
Bronchoscopy is a diagnostic test that involves a camera going down the trachea to visualize what’s happening in the lungs
PFT: it’s another diagnostic test that helps determine inspiratory and expiratory effort
What is the main treatment given for respiratory issues?
O2 supplementation
How does mechanical ventilation work?
The ventilator takes over a person’s breathing by using positive pressure to force air into the person’s lungs.
To use it, an artificial airway (ETT or trach) must be placed
What are indications for a mechanical vent?
●Respiratory failure
●Damaged airway: may see a tracheostomy
●Hypoxemia despite non-invasive methods
●Apnea
●Reduced oxygen consumption
●Allow sedation: withdrawal patients
What’s the order when intubating a person?
•Gather supplies
•Hyper-oxygenate patient: create an oxygen reserve to give yourself time to insert the tube
•Sedation/paralytics: benzo/propofol and paralytic
•Insert blade
•Insert ETT
•Inflate ETT balloon
•Verify placement
•Connect to ventilator
•Stabilize ETT
How do you verify correct placement of an breathing tube?
CHEST X-RAY (main way)
Other
end-tide CO2 levels
Assess breathing sound, chest movement, and air emerging from ET tube
What does nursing care of an ET tube look like?
Assess tube placement, leaking of cuff, breath sounds, and chest wall movement
Give soft wrist restraints
Chart
depth of ETT, pilot balloon status, restraints, vent settings, stability status
What are possible complications of ET tubes?
The tube is in too far or is in the stomach
There’s difficulty to intubate
Dentures
Damage to teeth or airway
Unanticipated extubation
What are common vent settings for nurses to monitor?
Tidal volume (Vt)
volume the vent gives to the pt. Normally 500 mL
Rate (f)
how many breaths per min
Fraction of inspired oxygen (FiO2)
% of how much O2 they’re on
Positive End Expiratory Pressure (PEEP)
extra boost given at the expiratory cycle by the vent to keep the alveoli from collapsing/closing (atelectasis)
What’s the difference between Bi PAP and CPAP?
Bi PAP: It’s the same or different pressure delivered during inspiration (positive pressure) and expiration (negative pressure)
Mostly for COPD pts.
CPAP: One constant pressure that stays being delivered
Mostly for sleep apnea
What’s the difference between Assist Control and Synchronized Intermittent Mandatory Ventilation (SIMV)?
Assist control: A preset rate and preset tidal volume. So a patient can initiate breathing over the set rate, but it always delivers the preset volume. For example, if you have a preset rate of 10 and a Vt of 500 mL, if a person chooses to breathe and they’re breathing 15 bpm, that’s fine, but each breath will always be at 500 mL
SIMV: There’s a preset rate and Vt, so all breaths will go at the rate set and be accompanied by the preset volume. But, the breaths a person chooses to breathe determine the volume. For example, if you have a preset rate of 10 and a Vt of 500 mL, if you’re breathing at 15 bpm, the 5 extra breaths are gonna be at whatever volume your lungs are able to pull
What are common causes for high pressure and low pressure vent alarms?
High pressure
Coughing
Biting of ET tube
Decreased lung compliance (ARDS)
Increased secretions
Low pressure
Leak in the cuff or circuit
Disconnection of tube from patient
Apnea
Commonly seen in those who don’t have a preset rate or are trying to get weaned off the vent
Why is it important for your vent circuit to stay intact?
It decreases infection risk and keeps pressures constant
What does the weaning process from a mechanical vent look like?
Determine that the pt. is ready
Turn off sedation
Change mode to bi-pap or cpap
Monitor (1hr) and draw ABGs
Extubate is no issues arise
What does the extubation process from a mechanical vent look like?
Hyperoxygenate pt.
Suction ETT and oral cavity
Quickly deflate ETT cuff
Remove tube at peak inspiration
Instruct pt. to cough
Monitor pt. q5min and assess
What are common complications from a mechanical vent?
Infection: ventilator-associated pneumonia (VAP)
increased susceptibly d/t easy access for bacteria
STRESS ORAL CARE
Muscle deconditioning
Esp resp muscles since breathing was taken up for them
Ventilator dependance
Seen a lot of COPD pts.
Barotrauma (damage d/t pressure) and Volutrauma (damage d/t overstretching from high volume)
Cardiac (hypotension, fluid retention, and PSNS stimulation)
How is the cardiac system involved in mechanical ventilation?
There is increased intrathoracic pressure d/t the positive pressure being forced in. The pressure compresses the aorta affecting its function. This leads to hypotension but also leads to fluid retention since the body thinks that it’s hypovolemic d/t the hypotension
How does a chest tube work?
A catheter is inserted through the rib space of thorax into the pleural space to remove air and/or fluid
A common chest tube used is the Pleur-Evac System
What are the indications of a chest tube?
●Restores negative pressure in pleural space
●Re-expands lung
●Attached to water-seal chest drainage device
●Common after chest surgery and lung collapse
What are the 3 chambers of a chest tube?
Chamber 1 (D): it’s the drainage collection chamber. It has the number figures and can collect fluid AND air. Measure fluid hourly for the first 24 hrs
Chamber 2 (C): it’s the water seal chamber. The water acts as a seal to prevent air from going back into the pleural space. You should NOT SEE continuous bubbling here. One bubble is fine as air passes through and it should always have 2 cm of sterile water
Chamber 3 (E): it’s the suction regulator and can be wet or dry. Continuous bubbling is normal if you have a wet suction chamber (normal suction Is -20cm)

How does chest tube placement differ when it’s air or fluid?
Air
Tube is placed near the front lung apex (up)
Fluid/blood
Tube is placed near the base of the lung (down)
What does continuous bubbling in the water seal chamber indicate?
Air leak in the system
What’s expected of the water seal chamber?
Rise and fall of 2-4 cm with inhalation and exhalation (tidaling)
When should the provider be notified (chest tube)?
> 70ml/hr of drainage
What are common nursing interventions for chest tubes?
●Encourage patient to cough, deep breathe, use incentive spirometer (splinting)
●Position patient in semi-to high-Fowler’s to promote lung expansion/drainage
●Pain management
●Keep hemostats, sterile water, occlusive dressing at bedside
●Do not strip or milk tubing unless ordered (creates high negative pressure and can damage lung tissue)
●Do not clamp chest tube unless you are only briefly clamping to check for air leak, to quickly change drainage devices, and to assess readiness for CT removal (what is risk?)
●Keep chest tube drainage system lower than the level of the patient’s chest
What are common complications of chest tubes?
Air leak
Suspected if there’s continuous bubbling from water seal chamber
Use padded clamp to fix leak
Disconnection, system breakage, chest tube removal
Tube separation from device: exhale and cough, place tube into sterile water
Tube out of patient: dress insertion site with dry sterile gauze
What’s the process of removing a chest tube?
●premedicate as needed
●Instruct patient to exhale and bear down with removal
●apply airtight sterile petrolatum gauze dressing after removal
●Chest x-ray to verify resolution of presenting problem
●monitor for recurrent pneumothorax
What diagnostics would be preferred if a patient is unstable d/t a pulmonary embolism?
Spiral CT
Echo or Compression ultrasound (hemodynamically unstable)
What diagnostics would be preferred if a patient is stable d/t a pulmonary embolism?
V/Q scan
When would an embolectomy be done for a person with a pulmonary embolism?
If the person can’t receive thrombolytics or if the thrombolytics are ineffective
When would a vena cava filter be used for a person with a pulmonary embolism?
If the person can’t be anticoagulated
Why should PEEP be tapered off when being given to someone on a mechanical ventilator?
There’s the risk of dependence and respiratory collapse if the patient is suddenly taken off it
What are key functions of the kidney?
Fluid and electrolyte balance
Waste removal
BP regulation
Erythropoietin production
Insulin degradation
Prostaglandin synthesis
Ca and Phosphorus regulation (hyperphosphatemia and hypocalcemia)
Vit D metabolism (decreased levels affect Ca)
What are causes of PRERENAL issues?
Lack of blood flow to the kidneys
Hypovolemia/severe hypotension
Shock states/sepsis
Hypertension meds (if taken in excess can cause decreased BP)
HF (lack of pressure from hear to perfuse)
Burns (fluid shifts)
Renal artery stenosis
What are causes of INTRARENAL issues?
damage to the kidneys
Glomerulonephritis
Renal laceration
Hypercalcemia
Thrombi
Pyelonephritis
Nephrotoxic drugs
HTN (high pressure damages small vessels in the kidneys)
What are causes of POSTRENAL issues?
something block flow out of the kidneys or bladder
Cancer of bladder, prostate, cervix
Prostate hypertrophy
Kidney stones
Clots in the urinary tract
What are common renal issue manifestations?
◼Neuro: Lethargy (electrolyte imbalance), dizziness (fluid imbalance), seizures (sodium imbalance)
◼CV: edema, dysrhythmias (potassium imbalance), tachycardia (hypo/hypervolemic)
◼Resp: dyspnea, crackles, tachypnea
◼GI: oliguria, anuria
◼GU: nausea, vomiting
◼Integ/Musc: dry mouth, stomatitis, pruritic (escape mechanisms of toxins that couldn’t be secreted from the kidneys), fever, dry skin
What are common renal labs?
BUN (blood urea nitrogen)
Waste product of protein and increases w/ kidney dysfunction
Creatinine
End-product of muscle metabolism and increases with renal dysfunction
GFR
Based on creatinine results and low numbers indicate decreased filtration and kidney function
What are common renal diagnostics?
Renal ultrasound
CT without contrast
Renal biopsy
Why are CTs done without contrast when dealing with patients with renal issues?
The contrast is nephrotoxic
What are common methods to treat renal issues ?
Pharm
Diuretics or fluids, phosphorus binders, vitamin and mineral replacement
Care
Strict Is & Os, monitor everything
Dialysis
Renal transplant
What does nutrition looks like for people with renal issues?
Possible fluid, sodium, potassium, or phosphorus restrictions
Low protein diet
How does renal replacement therapy work?
Fluid is moved across a semipermeable membrane to do the job of the kidneys and filter out toxins helping the body normalize its concentrations
Usually given to those with AKI, CKD, or ERSD
What are common access points for those receiving RRT?
Venous
Quinton cath (through internal jugular or subclavian)
AV fistula
What is peritoneal dialysis?
It’s when the peritoneum is used as a filter to remove waste products
Good for those who can’t have anticoagulation, vascular access, or are unstable
Used for CKD or ESRD patients
Output should be greater than or equal to input and the outflow should be placed lower than the abdomen
Be sure to monitor for clots, INFECTION, weight, and labs
What are the indications of infection (peritonitis) during peritoneal dialysis?
rigid painful abdomen
What is hemodialysis?
It’s when blood is removed, passed to the filter, warmed, then returned
You don’t want to give someone unstable undergo this since it causes large fluid shifts and requires vascular access
Can be used for CKD, ESRD, or an AKI
You also want to withhold medication until after dialysis
Monitor
dialysate temp
for hypotension and bleeding
nausea and headache
What can a headache indicate during hemodialysis?
disequilibrium
What is CRRT (continuous renal replacement therapy)?
Short-term therapy is given to those for an AKI
Also requires vascular access, but it’s much gentler compared to other RRT therapies, so it doesn’t cause hemodynamic changes
it can also be given with meds
When is a kidney transplant usually considered?
ESRD
What does post-op care for a kidney transplant look like?
Hourly output monitoring
Daily weights
Frequent labs
Administer immunosuppressants
What are some kidney transplant complications?
Rejection
fever, pain at site, oliguria, hypertension
Renal artery stenosis
d/t scarring from surgery and often presents as hypertension and decreased renal function
treated with angioplasty
Infection
Risk b/c of immunosuppression
What is normal fluid output?
30 mL/hr
What are the phases of an AKI?
Oliguric phase
Occurs quickly since the body senses its’ in a hypovolemic state so it starts to retain fluid
Renal labs start to become anormal (BUN, creatinine, GFR)
Diuretic phase
Caused by osmotic diuresis from urea buildup as well as tubule dysfunction
Recovery phase
GFR increases, BUN and creatinine decrease
Why does the oliguric phase occur quicker with volume depletion than nephrotoxic drugs?
When the body senses itself in a hypovolemic state, it activates RAAS and causes fluid retention. This is why their compensatory mechanism is quicker than nephrotoxic drugs.
What is the RIFLE criteria system
A system to determine how severe the renal damage is. It’s based on objective GFR and UO data
▪Risk
▪Injury
▪Failure
▪Loss of function
▪ESRD
Why would someone with an AKI display neuro issues if they aren’t hypovolemic?
Abnormal labs like sodium that result from fluid retention (hyponatremia)
Why do stomatitis and pruritis occur in AKI patients?
the body is trying to get rid of waste through different routes other than the kidneys
What do chem panels usually show in a person with an AKI?
Hyponatremia d/t hemodilution
Hyperkalemia d/t kidneys retaining potassium if they aren’t functioning
Hyperphosphatemia since kidneys normally secrete phosphorus, but if they’re not working, they retain it
Hypocalcemia since Ca and phosphorus have an inverse relationship
How does hyperkalemia present in AKI patients?
Sinus tach with multifocal PVCs and tented, tall t-waves
What’s a substitute to contrast?
Carbon dioxide
Why would phosphate binders be given to treat an AKI?
Phosphate is usually secreted by the kidneys, but when there’s an renal injury, the kidneys retain phosphorus. The phosphate binders help decrease the high phosphate levels in the body
How is hyperklemia treated in AKI patients if it’s present?hyperkalemia
Similar to phosphate, the kidneys retain K if they’re not functioning well
So, you’d want to first push insulin to cause K to move into the cells
To prevent hypoglycemia, you’d want to also push D50 to keep glucose up
Then to fully secrete K from the cells, you’d give kayexalate (sodium polystyrene sulfonate) to allow for K to be passed during a BM
How is acidosis treated in AKI patients if it’s present?
Give sodium bicarb, but be mindful of fluid overload since it’s usually administered in fluid form
What do you want to teach an patient with an AKI about fever?
Fever may not be present with infection bc of blunted febrile response
Why are HTN and DM2 the main causes of CKD?
They are slow and insidious allowing the body to compensate until the compensation wears out
What are the stages of CKD?
1-5 with 5 being the worst and 1 being normal kidney function
1: normal
2: mild damage
3: moderate damage
4: severe damage
5: ESRD
RRT is usually started at stage 4
Why does someone with a CKD have abnormal bleeding/bruising?
the blood is thinner since clotting cascade gets affected by kidney damage
What is CKD mineral and bone disorder (CKD-MBD)?
With kidney disorders, there’s an increase in phosphorus since the body retains it. As a result, the phosphate binds to Ca which decreases free Ca in the blood
Ca is further reduced bc the kidneys are also responsible for activating Vit D which helps with Ca absorption
When the kidneys are damaged, Vit D is not activated, reducing Ca levels
To compensate, the parathyroid glands release parathyroid hormone to pull calcium from the bones into the blood. This weakens the bones over time.
Where is ADH (vasopressin) produced and released?
It’s produced in the hypothalamus and released by the posterior pituitary gland into the blood stream
What are the 3 categories of hormone characteristics?
Endocrine: travel through the blood and act at distant receptor sites
Paracrine: act locally at cells close to area of release
Autocrine: act on cells that release the hormone
What kind of hormones have a longer hald-life?
Protein bound hormones
What two diseases affect the hypothalamus posterior pituitary axis?
Diabetes Insipidus (DI) and Syndrome of Inappropriate Anti-diuretic hormone excretion (SIADH)
What is the primary issue in Diabetes Insipidus?
Deficiency in anti-diuretic hormone (ADH)/vasopressin
What occurs to serum electrolytes and urine electrolytes in DI?
Seum electrolytes are concentrated
Urine electrolytes are diluted
What complication from surgery can cause Central DI?
Post-op inflammation
What’s the root link to DI manifestations?
Hypovolemia
Tachy, hypotension
fatigue, lethargy, HA
Polyuria, polydipsia, ice water craving
How would ADH levels vary depending on the type of DI?
Central DI: low ADH
Nephrogenic DI: high ADH
How can a water deprivation test help differentiate between DI and primary polydipsia?
It would be DI if the body continues to excessively urinate even with water being withheld. If it’s primary polydipsia, urine should be more concentrated and there should be no change
How can a vasopressin test determine DI?
Synthetic ADH is given. If the urine gets more concentrated, then it shows that the root issue was a deficiency in AHD (Central DI)
But, if there is no change in the patient’s condition, it shows that there’s a problem with the kidneys (Nephrogenic DI)
What are the MOAs of some meds used to treat DI?
Carbamazepine: anticonvulsant that helps the pituitary release ADH for nephrogenic DI
NSAIDs: reduce UOP for nephrogenic DI
Indomethacin: increases renal sensitivity to ADH
Thiazide diuretics: reduce OUP for nephrogenic DI
What is the primary issue in SIADH?
Excessive release/amounts of ADH/vasopressin causing fluid retention
What’s the big worry when dealing with SIADH?
Electrolyte imbalance, especially in sodium (hyponatremia) since brain cells start to swell which increases intracranial pressure (RISK FOR HERNIATION)
What meds can cause increases secretion of ADH leading to SIADH?
Carbamazepine
Cyclophosphamide
SSRIs
Why would you want to fix severe hyponatremia in SIADH slowly?
Central pontine myelinolysis
You don’t want to fix Na quickly since it can demyelinate the neurons in the brainstem and affect their function (HR, respiratory rate, etc.) The slow change stops this complication from happening
What are the adrenal cortical disorders?
Cushing’s Syndrome
Addison’s disease
What’s the difference between Cushing’s Syndrome and Cushing’s Disease?
Cushing’s Syndrome: symptoms related to the pituitary gland releasing too much ACTH
Cushing’s disease: presence of a pituitary tumor that secretes excess ACTH (adrenocorticotropic hormone)