Corneal Trauma, Non-infectious Keratopathy, Immunologic Disorders
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
52 Terms
Closed injury
injury where the corneoscleral wall of the globe is still intact
Contusion
a closed injury caused by blunt trauma. Damage may occur distant to the impact site.
Open injury
injury where there is a full thickness wound of the corneoscleral wall
Rupture
a full thickness wound caused by blunt trauma. The globe gives way at its weakest point, which may be distant from the injury site.
Laceration
a full thickness wound caused by a direct impact tearing injury. Not very common.
Lamellar laceration
a partial thickness laceration
Penetrating injury
a full thickness injury without an exit wound which is often caused by a sharp object
Perforation
two full thickness wounds, one entry and one exit, which are often caused by a projectile object.
Incised injury
injury caused by a sharp object such as glass or a knife
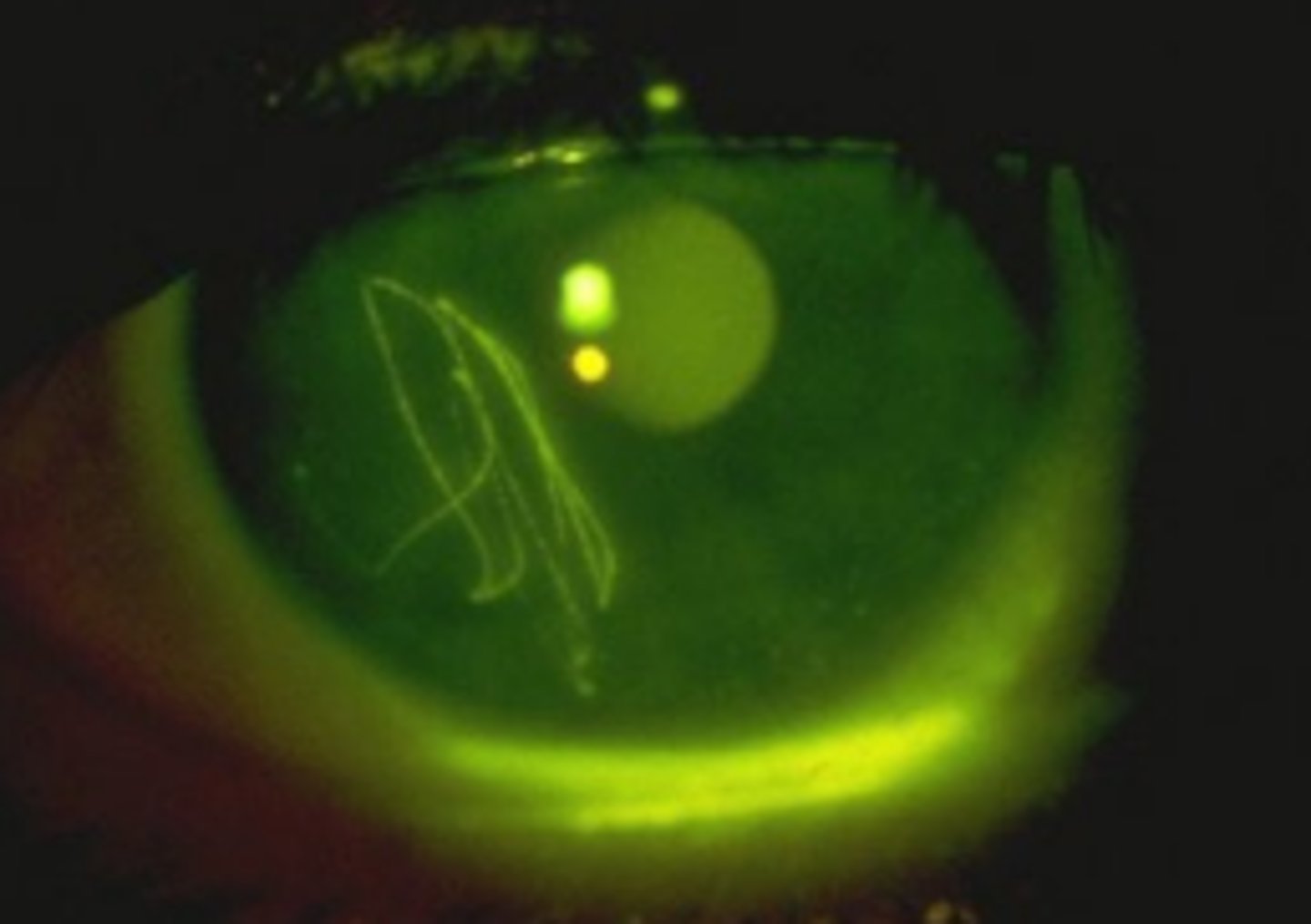
Corneal epithelial abrasion
one of the most common ophthalmic injuries involving partial or complete removal of the corneal epithelium. If Bowman's layer is intact, no scarring will occur. Pain occurs that is typically out of proportion to the injury size. Variable VA depending on the location of the defect and the presence of edema. Do not use bandage CL in contact lens wearers
Stromal corneal abrasion
corneal injury that is uncommon, but will form a scar due to penetration into Bowman's. If it occurs without a flap, it can be treated as a cornea abrasion. If it has a smooth flap, a bandage CL will suffice. If it has a rough flap, it will require sutures.
Blunt force trauma
injury occurring from impact of a noncutting instrument which may lead to an abrasion or deeper corneal injury. Can be contusive (caused by direct impact), or concussive (caused by rapid movement and energy transfer to surrounding tissues). Damage is usually not localized to the cornea. Decrease on vision is usually significant due to corneal edema or damage to other underlying ocular tissues.
Foreign body
one of the most common ocular traumas occurring at work due to lack of safety eye protection. Symptoms include pain, photophobia, tearing, inability to open the eye, and redness. Vision will varying depending on location. If it is superficial, remove and treat as an abrasion. If it is penetrating, refer for surgery and protect with a fox shield in the meantime.
Penetrating/perforating injury
ocular trauma involving a foreign body that completely enters the eye. Is more common in younger males. Some signs of an open globe are a Seidel sign, prolapse uveal tissue, low IOP, flat anterior chamber, iris deformities, dislocated lens, and retinal detachment.

Infection, hypotony, secondary glaucoma, corneal scarring, and retinal complications
five complication of perforating corneal injury
Acid injury
injury to the cornea which causes coagulation of protein that results in coagulative necrosis and clouding of ocular tissues which prevents further penetration into other structures. Increased concentration or exposure time leads to greater damage.
Alkali injury
injury to the cornea which caused saponification of fatty acids that results in liquefactive necrosis and fogging of the stroma allowing for deeper penetration into the anterior segment. This can result in increased IOP caused by secondary glaucoma, iritis, and decreased VA.
I
grade of chemical burn with no corneal opacity and no limbal ischemia. Excellent prognosis
II
grade of chemical burn with corneal haziness, but still visible iris details. Ischemia is less than 1/3 of the limbus. Good prognosis
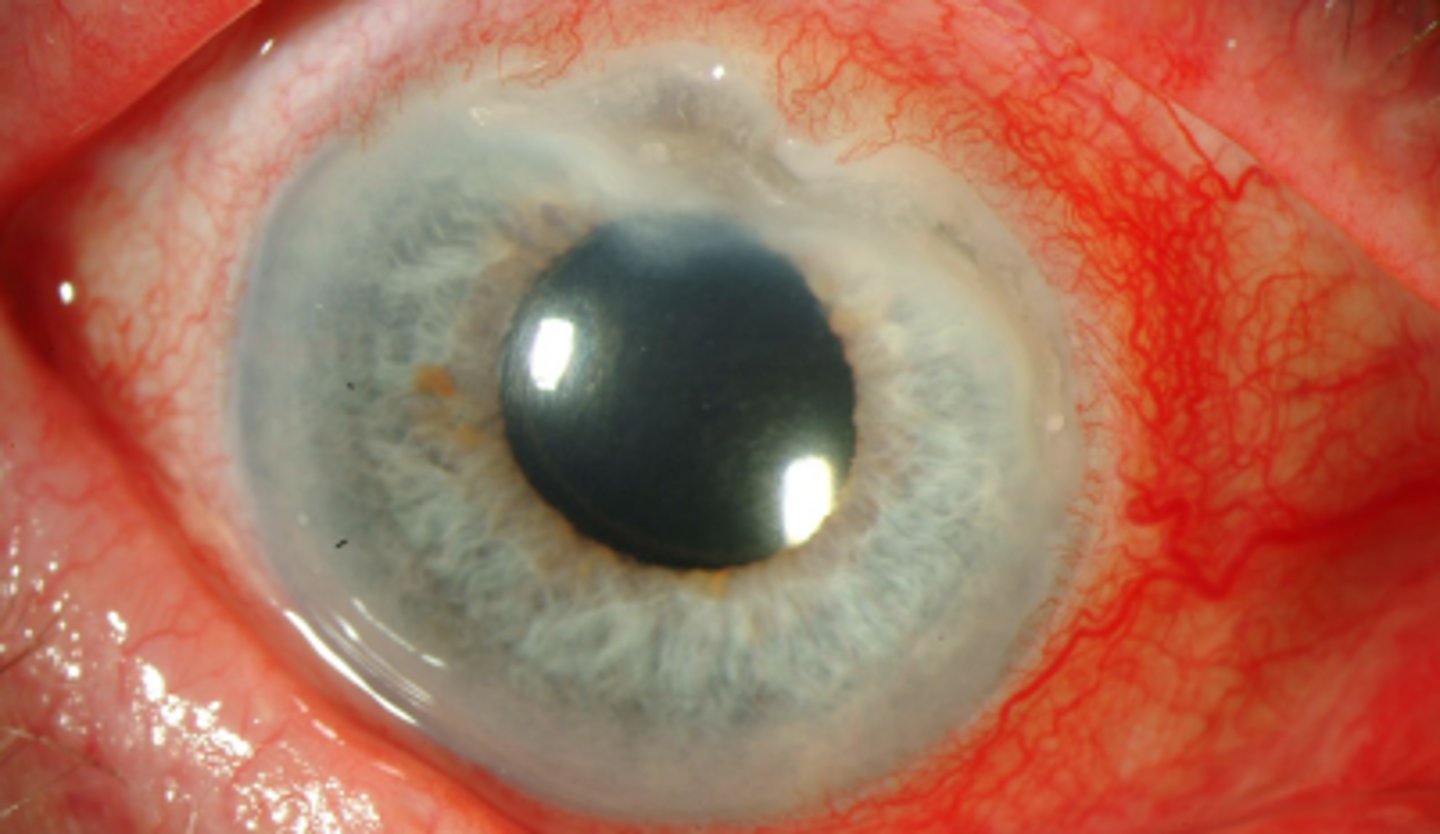
III
grade of chemical burn with significant corneal haziness that obscures the iris details. Ischemia is 1/3 to ½ of the limbus. Guarded prognosis
IV
grade of chemical burn with a complete opaque cornea blocking both the iris and pupil. Ischemia is greater than half the limbus and ischemic necrosis is present. Prognosis is poor
15-55
Secondary glaucoma occurs in _____% of patients having severe chemical burns. Is more likely in alkali burns than acid.
stabilizing the blood aqueous barrier
Cycloplegics are useful in minimizing anterior chamber reaction in chemical injuries by _____ which prevents further infiltration by inflammatory cells
minimize scarring
Steroids are useful in the treatment of chemical injuries of the cornea in order to...
Recurrent corneal erosion
episodic erosion of the corneal epithelium with complete resolution between attacks. Is unpredictable and variable in presentation, but occurs due to an abnormally weak attachment between basal cells and the basement membrane. Risk factors include prior corneal trauma, EBMD, DES, bullous keratopathy, and diabetes. Acute management is the same as for than of an abrasion, prevention involves lubrication prior to sleep, hypertonic saline (DO NOT USE IN ACUTE, BURNS), and surgery.

prior corneal trauma, EBMD
the two main risk factors for recurrent corneal erosion
Filamentary keratopathy
condition where an area of loose epithelium acts as a focus for deposition of mucus and cellular debris filaments involving aqueous deficiency and increased mucin production. Is more common in women and incidence increases with age. Is caused by aqueous deficient DES, excessive CL wear, etc. Symptoms include discomfort, photophobia, etc. Will stain well with Rose Bengal. Treatment involves addressing the underlying condition, manually removing filaments, mucolytic agents, topical NSAIDs
Thygeson's superficial punctate keratitis
an uncommon, usually bilateral asymmetric idiopathic keratopathy (possibly viral or inflammatory). Most commonly effects females and young adults. Has episodes of exacerbations (1-2 months) and remissions (6 weeks). Appears as coarse punctate epithelial keratitis with little or no hyperemia. Don’t usually present with symptoms, maybe mild discomfort. Treatment includes lubrication and steroids.
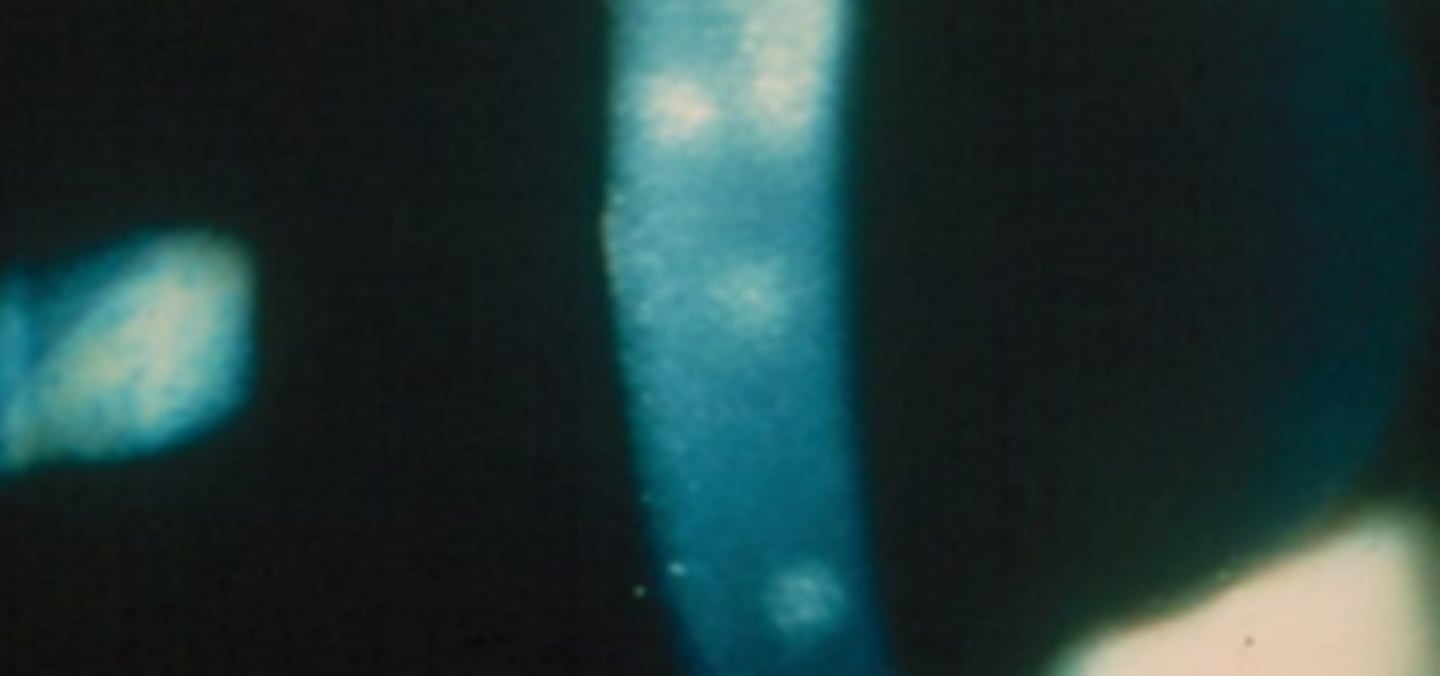
bilateral, asymmetric
describe the laterality and symmetry of Thygesons
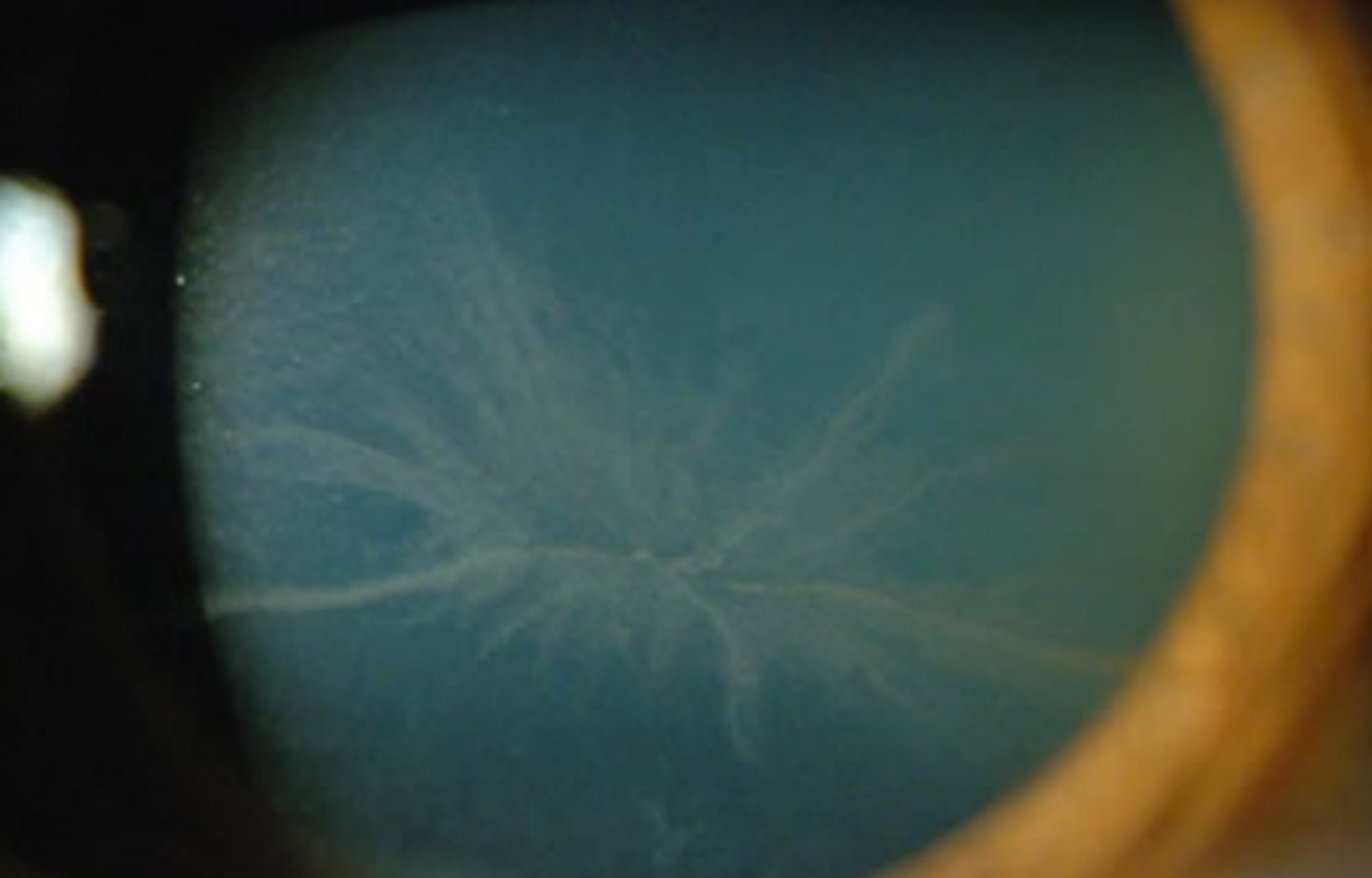
Corneal verticillata (vortex keratopathy, corneal whorls, whorl keratopathy)
condition involving a whirl like pattern of powdery white epithelial deposits that form a vortex pattern in the inferocentral cornea that spares the limbus.
Amiodarone
an antiarrhythmic drug that can cause vortex keratopathy in 69-100% of patients using the drugs. Also causes lenticular changes, madarosis, and retinal or ON complications Haloing is the most common vision change
Chloroquine/hydroxychloroquine (Plaquenil)
an antimalarial drug used in the treatment of autoimmune diseases such as RA and SLE that can cause vortex keratopathy, although its retinal complications are much more concerning and are usually the culprit for visual changes. Corneal edema and decreased corneal sensitivity may also occur.
Tamoxifen
drug that is used in the treatment of breast cancer by blocking the actions of estrogen and can cause vortex keratopathy, although its retinal complications are more concerning and are usually the culprit for visual changes..
Rho-kinase inhibitors (Rhopressa, Rocklatan)
IOP lowering drugs that work by increasing trabecular outflow and decreasing episcleral venous pressure. 8-25% of these patients using these drugs develop vortex keratopathy. Minor visual changes may occur.
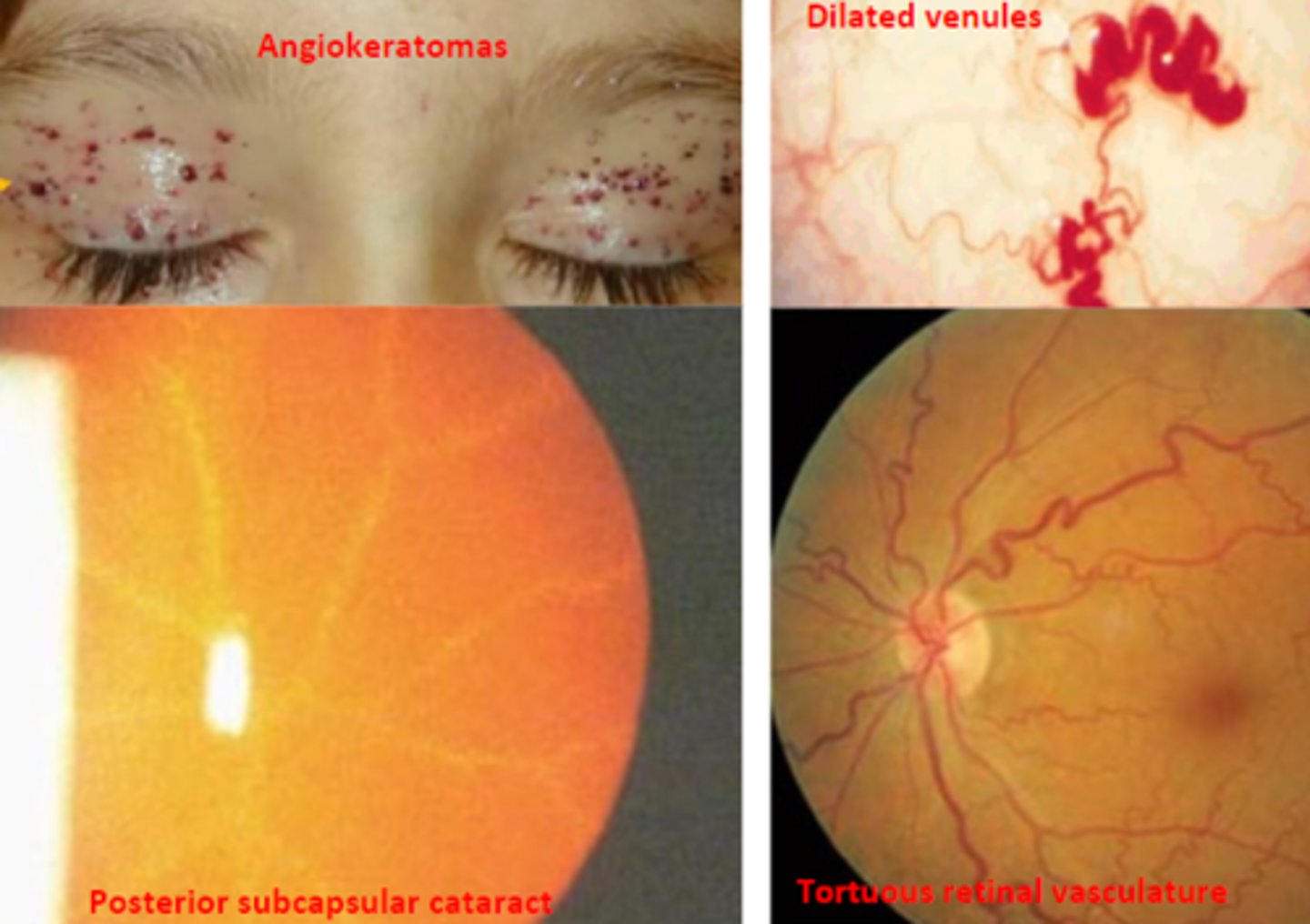
Fabry's disease
an X linked recessive disorder that results in irreversible, potentially life threatening diseases of the kidney, heart, and brain. Is caused by a deficiency of alpha galactosidase A that results in dysfunction of lysosomal storage. Corneal changes, including vortex keratopathy, are the earliest and most consistent ocular abnormality. Symptoms generally appear in childhood, but go undiagnosed until adulthood.
alpha galactose A
enzyme that is deficient causing Fabry's disease
Angiokeratomas
benign lesions of blood vessels appearing as dark spots on the skin, as seen in Fabry's disease.

Posterior subcapsular cataracts
cataract type seen in Fabry's disease
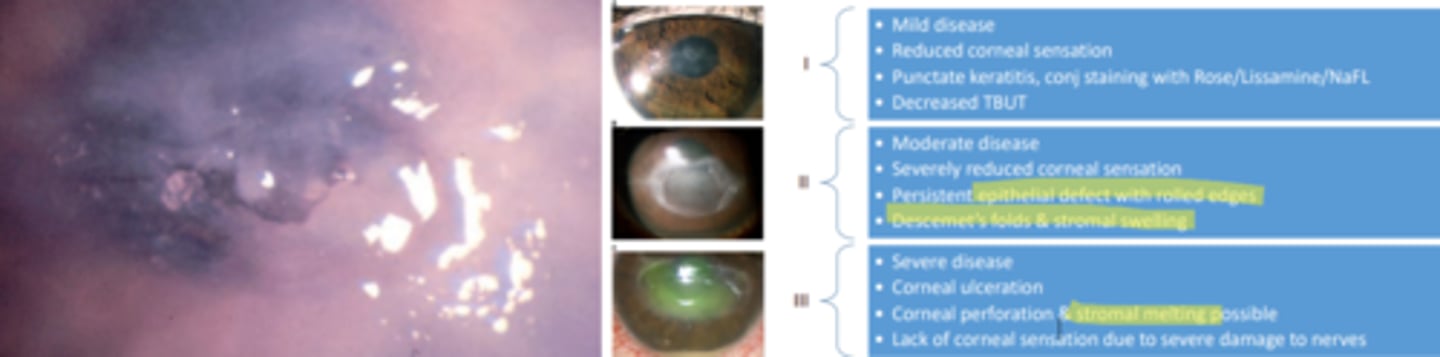
Neurotrophic keratitis
condition caused by partial or complete loss of trigeminal innervation to the cornea that leads to decreased corneal sensation and subsequent breakdown of corneal epithelium and loss of vision. Is very rare, but prevalence depends on the underlying cause. Treatment is dependent on the stage of disease, but all topical drops that contain preservatives should be discontinued. A prophylactic antibiotic should be employed.
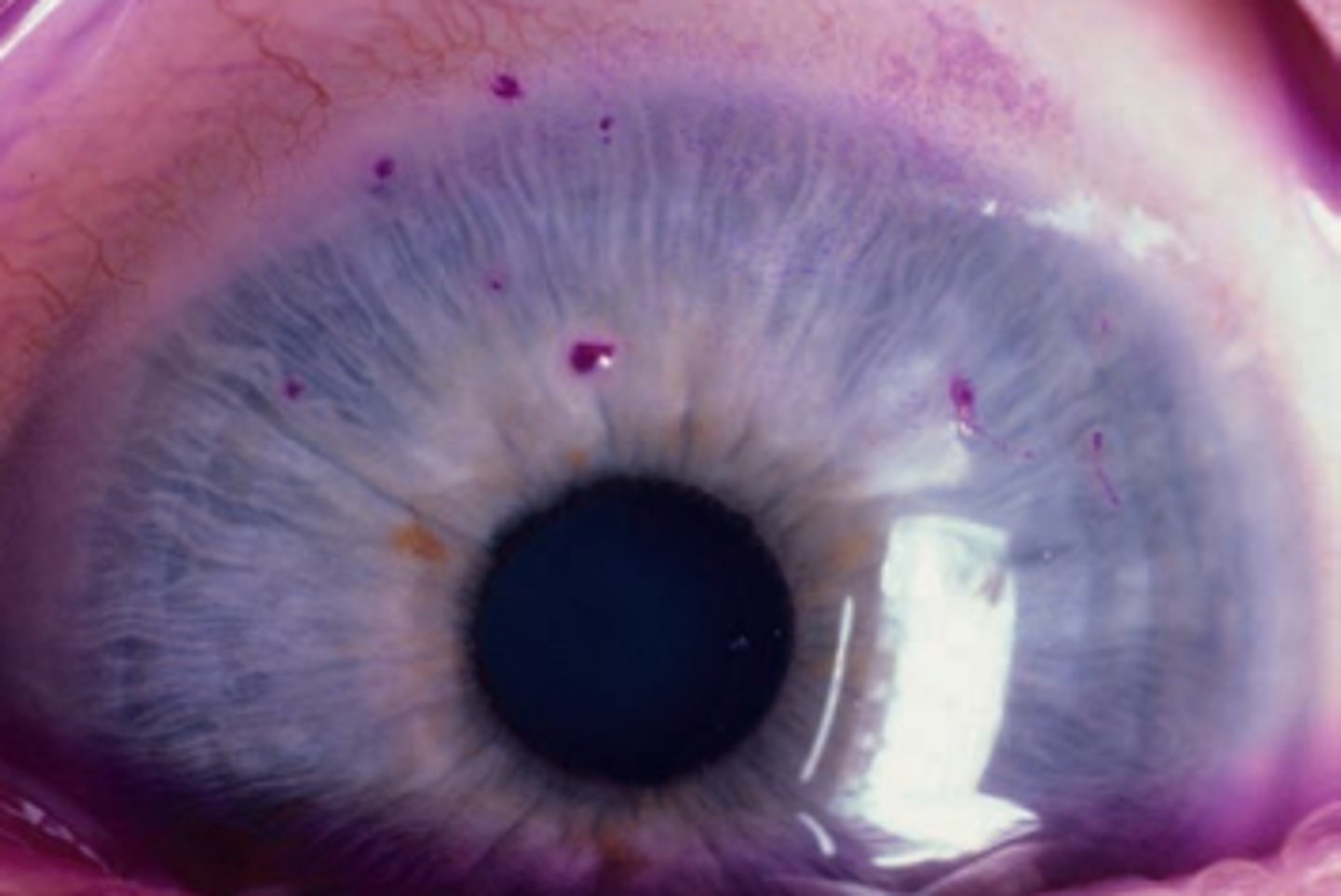
Phylctenular keratoconjunctivitis (phlyctenulosis)
a local conjunctival/corneal type IV hypersensitivity reaction to a bacterial antigen requiring repeat exposure to that specific antigen. Was previously associated with TB (more symptomatic), but is now more common with staph. Is more common in children. Involves that formation of subepithelial nodules of inflammatory cells. Initial encounter will affect the limbus and subsequent encounter migrate to the cornea and conjunctiva. If the cornea is affected, the reaction tends to be more severe – pain, photophobia, blepharospasm. Culturing of the organism is important. Management includes steroids AND antibiotics.
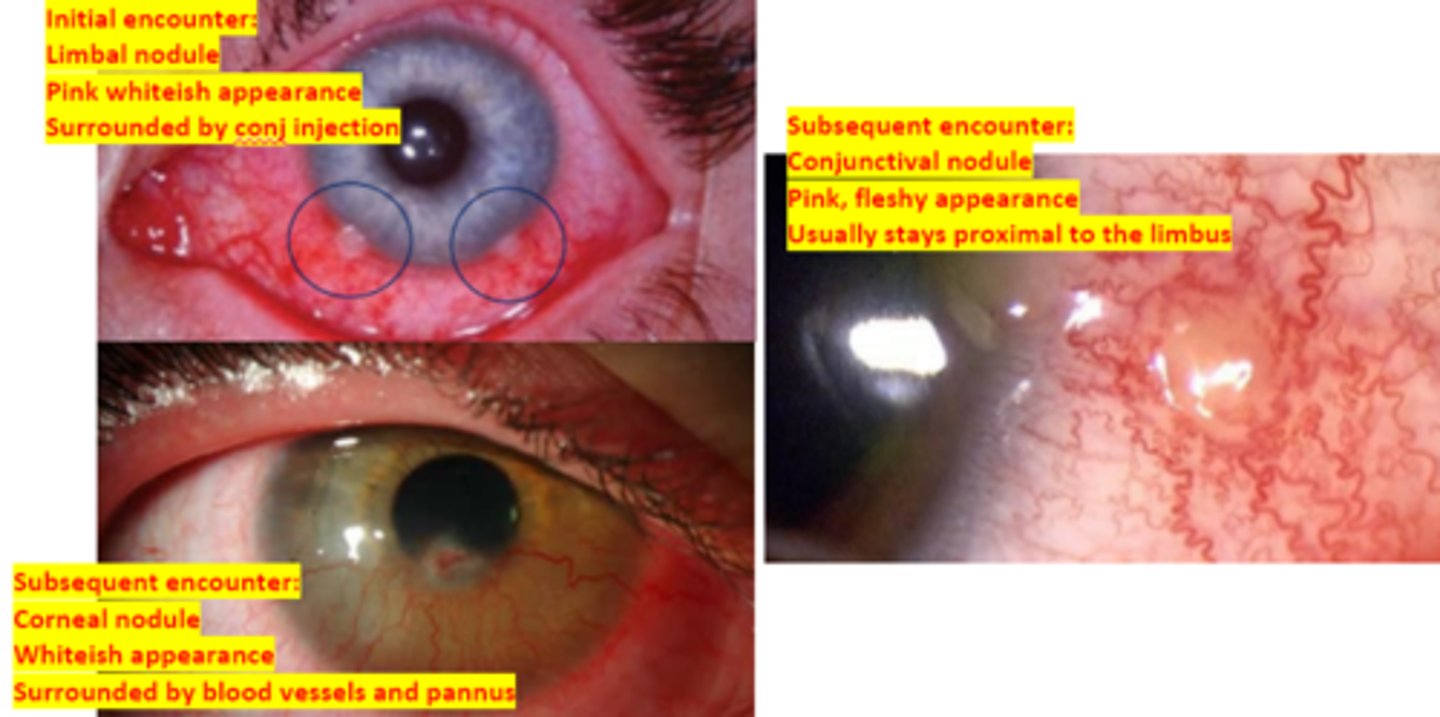
tb, staph
phylctenular keratoconjunctivitis use to be more commonly associated with _____ infection, but is currently more commonly associated with ______ infection
type IV
what type of hypersensitivity reaction is phlyctenular keratoconjunctivitis?
Marginal staphylococcal keratitis
an inflammatory infiltration of the cornea that may lead to ulceration. Is a type III hypersensitivity reaction associated with staphylococcal blepharoconjunctivitis. Is the most common disorder of the peripheral cornea. Presents as peripheral stromal infiltrates where the lid crosses the limbus and often chronic blepharitis. Treatment involves addressing the underlying cause. Ie) lid hygiene, steroid, antibiotic, oral doxy
Marginal staphylococcal keratitis
what is the most common disorder of the peripheral cornea?
type III
What type of hypersensitivity reaction is marginal staphylococcal keratitis?
Graft versus host disease
condition where donor cells from a graft mount an immune response against the recipient. Has an array of symptoms presenting throughout the body. 60-90% of cases present with ocular findings similar to that of severe dry eye (FBS, burning, redness, decreased VA due to SPK, photophobia). Complications include corneal scarring, neovascularization, and cicatricial changes of the conj. Goals of treatment involve lubrication, control of evaporation, and decreasing ocular surface inflammation.
Peripheral ulcerative keratitis
a rare inflammatory disorder of the peripheral cornea occurring due to underlying disease (RA, infection, post-surgery, dermatological disease, etc.). Exact mechanism is unknown. Is unilateral almost always. Appears as a crescent shaped peripheral corneal ulceration with overlying stromal infiltration. Presents as redness, pain (+++), tearing, and photophobia. VA may be degraded due to induced astigmatism. Treatment involves addressing the underlying cause.
unilateral (almost always)
describe the laterality of peripheral ulcerative keratitis
Mooren's ulcer
a painful, progressive, idiopathic chronic ulcerative keratitis that begins peripherally and move circumferentially and centrally. Appears as a grey white crescent shape with vascularization leading to the edge of the ulcer. Is more common in men and 40-70 yo. Is usually unilateral. Has no associated systemic disease or scleritis. Management begins with steroids, prophylactic antibiotics, and supportive therapy.
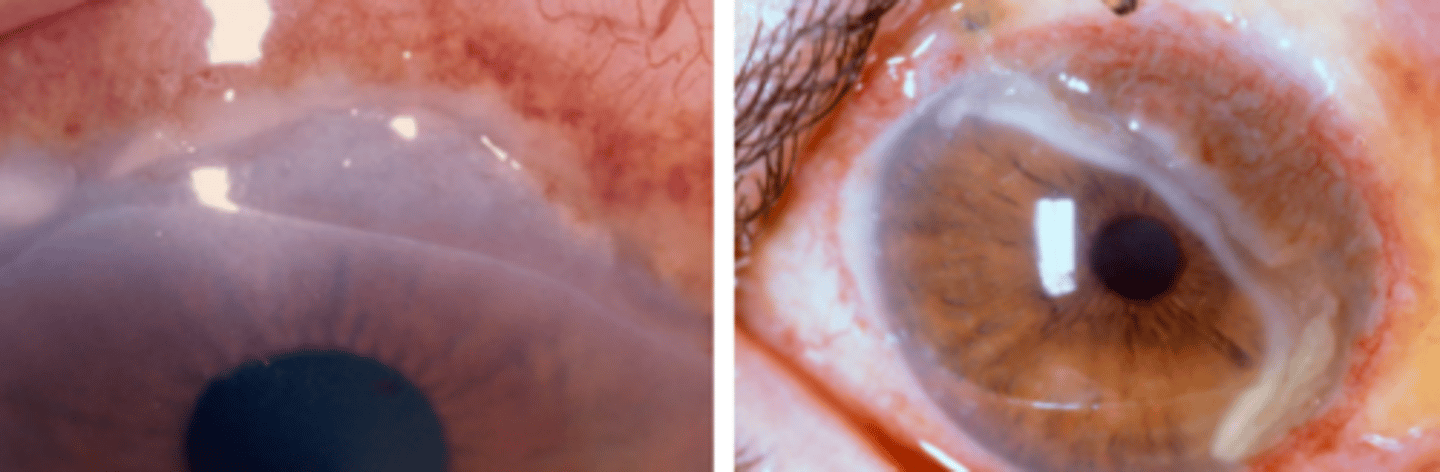
Unilateral (type I)
Mooren's ulcer more commonly seen in elderly patients. Is associated with non-perfusion of the superficial plexus of the anterior segment. severe pain and rapid progression
Bilateral, aggressive (type II)
Mooren's ulcer more commonly seen in young patients. Ulcerations begins circumferentially then migrates centrally with vascular leakage and neovascularization extending to the base of the ulcer. Most common.
Bilateral, indolent (type III)
Mooren's ulcer more commonly seen in middle aged patients. Is bilateral, progressive with peripheral guttering and little inflammatory response. Has no vascular changes or neovascularization.