Chapter 7.3 Study Materials - Cerebrospinal, Serous, and Synovial Fluids in Medicine
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
Cerebrospinal fluid (CSF) is formed by ultrafiltration of plasma through the:
A. Choroid plexus
B. Sagittal sinus
C. Anterior cerebral lymphatics
D. Arachnoid membrane
A. Choroid plexus
Which statement regarding CSF is true?
A. Normal values for mononuclear cells are higher for infants than adults
B. Absolute neutrophilia is not significant if the total WBC count is less than 25/uL
C. The first aliquot of CSF should be sent to the microbiology laboratory
D. Neutrophils compose the majority of WBCs in normal CSF
A. Normal values for mononuclear cells are higher for infants than adults
When collecting CSF, a difference between opening and closing fluid pressure greater than 100 mm H2O indicates:
A. Low CSF volume
B. Subarachnoid hemorrhage
C. Meningitis
D. Hydrocephalus
A. Low CSF volume
The difference between opening and closing pressure reflects how much CSF was removed and how well the intracranial pressure equilibrates.
A large drop (>100 mm H₂O) usually means that the CSF volume or pressure reserve is already low, so even removing a small amount causes a big pressure decline — typical of low CSF volume or intracranial hypotension, not hydrocephalus.
In hydrocephalus, both opening and closing pressures are elevated, but the difference between them is usually small because CSF pressure equilibrates slowly but remains high.
Which of the following findings is consistent with a subarachnoid hemorrhage rather than a traumatic tap?
A. Clearing of the fluid as it is aspirated
B. A clear supernatant after centrifugation
C. Xanthochromia
D. Presence of a protein in the sample
C. Xanthochromia
Xanthochromia, a yellow or pink discoloration of the CSF supernatant after centrifugation, indicates the presence of hemoglobin breakdown products (bilirubin, oxyhemoglobin) from an older hemorrhage, distinguishing a subarachnoid hemorrhage (SAH) from a traumatic tap, where fresh blood clears in successive tubes and the supernatant remains clear.
The term used to denote a high WBC count in the CSF is:
A. Empyema
B. Neutrophilia
C. Pleocytosis
D. Hyperglycorrhachia
C. Pleocytosis
Pleocytosis refers to an increased white blood cell count in the cerebrospinal fluid (CSF), indicating inflammation or infection of the central nervous system, such as meningitis or encephalitis.
Which of the adult CSF values in the table below are consistent with bacterial meningitis?
Pattern: WBCs, Lymphs, Monos, Eos, PMNs, Neuroectodermal Cells
A. 50/uL, 44%, 55%, 0%, 0%, 1%
B. 300/uL, 75%, 21%, 3%, 0%, 1%
C. 2,000/uL, 5%, 15%, 0%, 80%, 0%
D. 2,500/uL, 40%, 50%, 0%, 10%, 0%
C.
WBCs: 2,000/uL
Lymphs: 5%
Monocytes: 15%
Eos: 0%
PMNs: 80%
Neuroectodermal Cells: 0%
Bacterial meningitis typically shows marked pleocytosis with neutrophil predominance (often >1,000/µL PMN-heavy). The other options are lymph/mono-predominant or low count, more consistent with viral or nonbacterial etiologies.
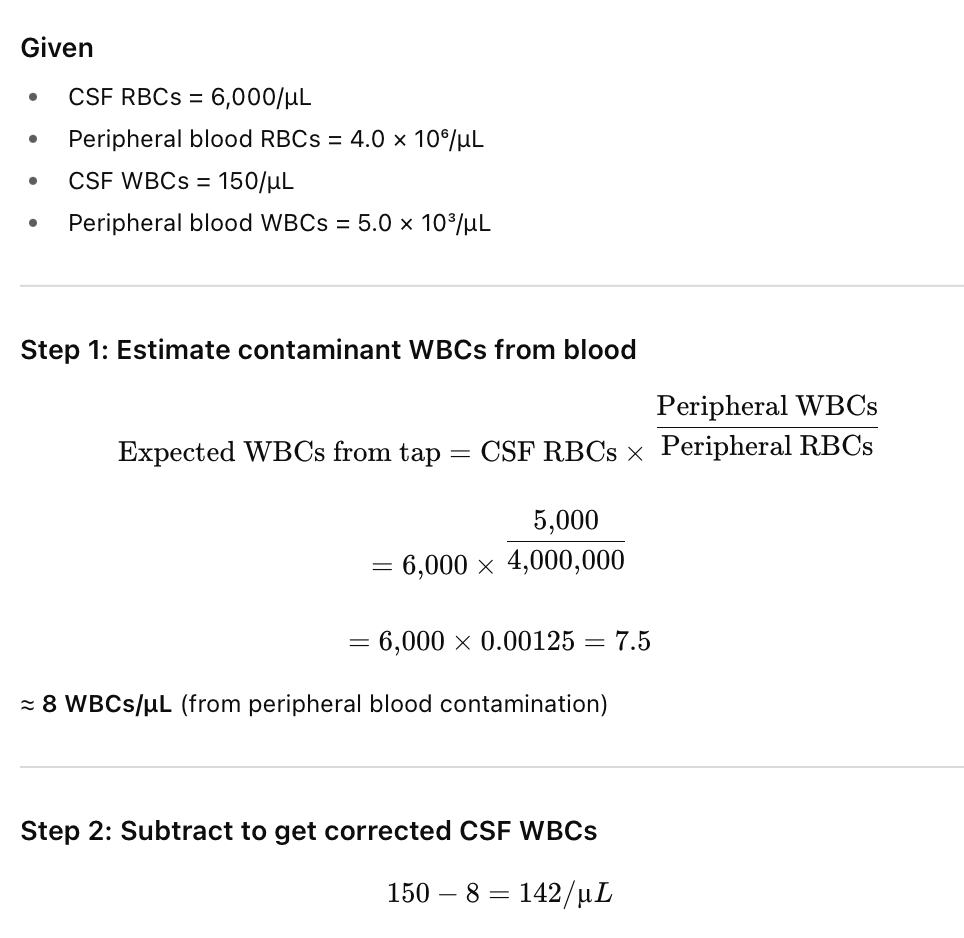
Given the following data, determine the corrected CSF WBC count.
CSF RBCs: 6,000/uL Peripheral Blood RBCs: 4.0 x 10^6/uL
CSF WBCs: 150 /uL Peripheral Blood WBCs: 5.0 x 10^3/uL
A. 8/uL
B. 142/uL
C. 120/uL
D. 145/uL
B. 142/uL
Corrected WBC count = WBCs in CSF - [(Blood WBCs x CSF RBCs) / Blood RBCs]
![<p>B. 142/uL</p><p>Corrected WBC count = WBCs in CSF - [(Blood WBCs x CSF RBCs) / Blood RBCs]</p><img src="https://knowt-user-attachments.s3.amazonaws.com/76c41ec5-8047-4bac-9a1a-56b77b97c245.png" data-width="100%" data-align="center"><p></p><p></p>](https://knowt-user-attachments.s3.amazonaws.com/349a1cfc-f867-47c6-81fc-b4c4277a5d8f.png)
What is the most likely cause of the following CSF results:
CSF glucose: 20 mg/dL
CSF protein: 200 mg/dL
CSF lactate: 50 mg/dL (reference range 5 - 25 mg/dL)
A. Viral meningitis
B. Viral encephalitis
C. Cryptococcal meningitis
D. Acute bacterial meningitis
D. Acute bacterial meningitis
Bacterial meningitis is characterized by low CSF glucose (organisms and WBCs consume glucose), high protein(increased permeability of the blood-brain barrier), and elevated lactate (>35 mg/dL), reflecting anaerobic metabolism and tissue hypoxia.
In contrast, viral meningitis/encephalitis typically shows normal glucose and only mildly elevated protein and lactate.
Which of the following conditions is most often associated with normal CSF glucose and protein?
A. Multiple sclerosis
B. Malignancy
C. Subarachnoid hemorrhage
D. Viral meningitis
D. Viral meningitis
In viral meningitis, CSF glucose remains normal because viruses do not consume glucose, and protein is only mildly elevated due to limited inflammation.
In contrast, bacterial, fungal, or malignant processes typically cause marked protein elevation and low glucose.
The diagnosis of MS is suggested by which finding?
A. The presence of elevated protein and low glucose
B. A decreased IgG index
C. The presence of oligoclonal bands by electrophoresis
D. An increased level of CSF beta-macroglobulin
C. The presence of oligoclonal bands by electrophoresis
Which of the following results is consistent with fungal meningitis?
A. Normal CSF glucose
B. Pleocytosis of mixed cellularity
C. Normal CSF protein
D. High CSF lactate
B. Pleocytosis of mixed cellularity
Fungal meningitis (e.g., Cryptococcus neoformans) typically shows a moderate pleocytosis with a mixture of lymphocytes, monocytes, and sometimes neutrophils — hence mixed cellularity.
Glucose is often decreased, protein increased, and lactate may be elevated, but the cell type pattern (mixed pleocytosis) is considered the classic diagnostic clue.
In what suspected condition should a wet prep using a warm slide be examined?
A. Cryptococcal meningitis
B. Amoebic meningitis
C. Mycobacterium tuberculosis infection
D. Neurosyphilis
B. Amoebic meningitis
In amoebic meningitis (most often due to Naegleria fowleri), a fresh wet prep of CSF must be examined immediately on a warm slide to observe motile trophozoites, which lose mobility quickly as the sample cools.
Rapid examination is essential because delayed or cooled samples can lead to false negatives.
Which of the following CSF test results is most commonly increased in patients with MS?
A. Glutamine
B. Lactate
C. IgG index
D. Ammonia
C. IgG index
In multiple sclerosis (MS), the CSF IgG index is often elevated, reflecting intrathecal (within the CNS) IgG synthesisindependent of blood—this helps distinguish MS from systemic IgG changes.
Which of the following is an inappropriate procedure for performing routine CSF analysis?
A. A differential is done only if the total WBC count is greater than 10/uL
B. A differential should be done on a stained CSF concentrate
C. A minimum of 30 WBCs should be differentiated
D. A Wright-stained slide should be examined rather than a chamber differential
A. A differential is done only if the total WBC count is greater than 10/uL
A CSF differential should always be performed, regardless of WBC count, because even a few abnormal cells (e.g., blasts, malignant cells, plasma cells) can have significant diagnostic value.
The other options describe appropriate procedures for routine CSF cytologic evaluation.
Which cell is present in CSF in greater number in newborns than in older children or adults?
A. Eosinophils
B. Lymphocytes
C. Monocytes
D. Neutrophils
C. Monocytes
Newborn CSF normally contains a higher proportion of monocytes (up to 70%) compared with older children and adults, whose CSF is typically lymphocyte predominant.
This reflects developmental differences in immune cell distribution within the central nervous system during infancy.
Neutrophilia pleocytosis is usually associated with all of the following except?
A. Cerebral infarction
B. Malignancy
C. Myelography
D. Neurosyphilis
D. Neurosyphilis
Neutrophilic pleocytosis occurs in acute or inflammatory conditions such as bacterial meningitis, cerebral infarction, CNS malignancy, or following myelography.
In contrast, neurosyphilis typically produces a lymphocytic pleocytosis, not neutrophilic.
Which statement about CSF protein is true?
A. An abnormal serum protein electrophoretic pattern does not affect the CSF pattern
B. The upper reference limit (URL) for CSF total protein in newborns is one half the adult level
C. CSF IgG is increased in panencephalitis
D. Antibodies to Treponema pallidum disappear after successful antibiotic therapy
C. CSF IgG is increased in panencephalitis
Panencephalitis and other chronic inflammatory CNS disorders (like MS) cause increased intrathecal IgG synthesis, leading to elevated CSF IgG levels.
The other statements are incorrect: serum protein patterns do influence CSF electrophoresis, newborns have higher (not lower) CSF protein levels, and antibodies to T. pallidum may persist even after successful therapy.
Which of the following statements regarding routine microbiological examination of CSF is true?
A. A gram stain is performed on the CSF prior to concentration
B. The gram stain is positive in fewer than 40% of cases of acute bacterial meningitis
C. India ink and acid fast stains are indicated if neutrophilia pleocytosis is present
D. All CSF specimens should be cultured using sheep blood agar, chocolate agar, and supplemented broths
D. All CSF specimens should be cultured using sheep blood agar, chocolate agar, and supplemented broths
For routine microbiologic CSF evaluation, sheep blood agar and chocolate agar support growth of most bacterial pathogens, while enriched (supplemented) broths enhance detection of fastidious or low–colony-count organisms.
The Gram stain is performed after concentration, and it is positive in about 60–90% of untreated bacterial meningitis cases, not fewer than 40%.
Which organism is the most frequent cause of bacterial meningitis in neonates?
A. Neisseria meningitidis
B. Group B Streptococcus
C. Haemophilus influenzae
D. Klebsiella pneumoniae
B. Group B Streptococcus
Group B Streptococcus (Streptococcus agalactiae) is the most common cause of bacterial meningitis in neonates, often acquired during birth from maternal colonization of the genital tract.
Other important neonatal pathogens include E. coli (K1 antigen) and Listeria monocytogenes, but Group B Strepremains the leading cause.
Following a head injury, which protein will identify the presence of CSF leakage through the nose?
A. Transthyretin
B. Myelin basic protein
C. Tau protein
D. C-reactive protein
C. Tau protein
Tau is a microtubule-associated neuronal protein found in high concentration in cerebrospinal fluid (CSF) but absent in serum or nasal secretions.
Its presence in nasal or ear fluid after a head injury confirms CSF leakage, since Tau originates from neuronal tissueand indicates breach of the blood–brain barrier or direct CSF escape.
Which of the following statements regarding serous fluids is true?
A. The normal volume of pleural fluid is 30 to 50 mL
B. Mesothelial cells, PMNs, lymphocytes, and macrophages may be present in normal fluids
C. Radiography can detect a 10% increase in the volume of a serous fluid
D. Normal serous fluids are colorless
B. Mesothelial cells, PMNs, lymphocytes, and macrophages may be present in normal fluids
The term effusion refers to:
A. A chest fluid that is purulent
B. A serous fluid that is chylous
C. An increased volume of serous fluid
D. An inflammatory process affecting the appearance of a serous fluid
C. An increased volume of serous fluid
The term effusion refers to an abnormal accumulation of serous fluid within a body cavity (pleural, pericardial, or peritoneal) resulting from disruption of fluid formation and absorption balance, often due to inflammation, infection, or hydrostatic/oncotic pressure changes.
Which of the following laboratory results is characteristic of a transudative fluid?
A. SG = 1.018
B. Total protein = 3.2 g/dL
C. LD fluid/serum ratio = 0.25
D. Total protein fluid:serum ratio = 0.65
C. LD fluid/serum ratio = 0.25
Here’s how to interpret each index in the context of transudates vs. exudates (based on Light’s criteria):
Specific Gravity (SG = 1.018):
Exudates usually have SG > 1.016, reflecting high protein and cellular content.
A value of 1.018 is borderline but leans toward exudate.
Total Protein (3.2 g/dL):
Transudates typically have <3.0 g/dL, while exudates have >3.0 g/dL.
At 3.2 g/dL, this is slightly above the transudate cutoff — borderline.
LD Fluid/Serum Ratio (0.25):
A ratio <0.6 indicates transudate; ≥0.6 indicates exudate.
0.25 clearly fits transudative fluid.
Total Protein Fluid/Serum Ratio (0.65):
>0.5 indicates exudate.
0.65 therefore points to exudate, not transudate.
Summary:
Only the LD fluid/serum ratio of 0.25 fits the transudate profile, which reflects low protein, low LD, and low cellularity—typically seen in systemic conditions like CHF, cirrhosis, or nephrotic syndrome rather than local inflammation.
Which observation is least useful in distinguishing a hemorrhagic serous fluid from a traumatic tap?
A. Clearing of fluid as it is aspirated
B. Presence of xanthochromia
C. The formation of a clot
D. Diminished RBC count in successive aliquots
C. The formation of a clot
Clot formation may occur in either hemorrhagic effusions or traumatic taps if the sample contains fibrinogen, making it unreliable for differentiation.
In contrast, clearing of fluid, decreasing RBCs in successive tubes, and xanthochromia (indicating older blood) are useful indicators for distinguishing between the two.
Which of the following laboratory results on a serous fluid is most likely to be caused by a traumatic tap?
A. An RBC count of 8,000/uL
B. A WBC count of 6,000/uL
C. A hematocrit of 35%
D. A neutrophil count of 55%
A. An RBC count of 8,000/uL
Which of the following conditions is commonly associated with an exudative effusion?
A. Congestive heart failure
B. Malignancy
C. Nephrotic syndrome
D. Cirrhosis
B. Malignancy
Exudative effusions result from increased capillary permeability or lymphatic obstruction, allowing protein-rich fluid and cells to enter the cavity—common in malignancy, infection, and inflammatory disorders.
Transudative effusions, by contrast, occur with systemic pressure or oncotic imbalances such as congestive heart failure, cirrhosis, or nephrotic syndrome.
Which of the following conditions is associated with a chylous effusion?
A. Necrosis
B. Pulmonary infarction or infection
C. Systemic lupus erythematosus or rheumatoid arthritis (RA)
D. Lymphatic obstruction
D. Lymphatic obstruction
Which of the following conditions is most often associated with a pleural fluid glucose below 30 mg/dL?
A. Diabetes mellitus
B. Pancreatitis
C. Rheumatoid arthritis
D. Bacterial pneumonia
C. Rheumatoid arthritis
Pleural fluid glucose <30 mg/dL is most often seen in rheumatoid pleuritis, where high metabolic activity of inflammatory cells and glucose transport inhibition across the pleura cause profound glucose depletion.
Bacterial pneumonia can also lower glucose, but typically not to such extreme levels—values this low are most characteristic of rheumatoid effusions.
In which condition is the pleural fluid pH likely to be above 7.3?
A. Bacterial pneumonia with parapneumonic exudate
B. Rheumatoid pleuritis
C. Esophageal rupture
D. Pneumothorax
D. Pneumothorax
n a pneumothorax, pleural fluid (if present) is typically alkaline (pH >7.3) because there is minimal inflammation or metabolic activity to produce acid.
In contrast, bacterial pneumonia, rheumatoid pleuritis, and esophageal rupture all produce acidic pleural fluids (pH <7.3) due to infection, inflammation, or leakage of gastric contents.
Which of the following hematology values best frames the URLs for peritoneal fluid?
Pattern: WBC Count, Percentage of PMNs, RBC Count
A. 300/uL, 25%, 100,000/uL
B. 10,000/uL, 50%, 500,000/uL
C. 50,000/uL, 50%, 500,000/uL
D. 100,000/uL, 75%, 1,000,000/uL
A.
WBC Count: 300/uL
Percentage of PMNs: 25%
RBC Count: 1,000,000/uL
Normal peritoneal (ascitic) fluid contains <300 WBCs/µL, with <25% PMNs and <100,000 RBCs/µL.
Higher counts or neutrophil predominance suggest peritonitis or intra-abdominal inflammation, while very high RBC counts indicate traumatic tap or hemorrhagic effusion.
Which of the following characteristics is higher for synovial fluid than for the serous fluids?
A. Specific gravity
B. Glucose
C. Total protein
D. Viscosity
D. Viscosity
Synovial fluid is normally highly viscous due to the presence of hyaluronic acid, which lubricates joints.
In contrast, serous fluids (pleural, peritoneal, pericardial) are watery and low in viscosity.
The viscosity of synovial fluid decreases in inflammatory joint diseases (e.g., rheumatoid arthritis) due to hyaluronidase activity.
In which type of arthritis is the synovial WBC count likely to be greater than 50,000/uL?
A. Septic arthritis
B. Osteoarthritis
C. Rheumatoid arthritis
D. Hemorrhagic arthritis
A. Septic arthritis
Septic arthritis produces a markedly elevated synovial WBC count (>50,000/µL), with >90% neutrophils, reflecting intense inflammation due to bacterial infection within the joint.
Other types—like rheumatoid arthritis or hemorrhagic arthritis—may increase WBCs moderately, while osteoarthritis typically shows <3,000/µL.
What type of cells is a "ragocyte"?
A. Cartilage cell seen in inflammatory arthritis
B. A PMN with inclusions formed by immune complexes
C. A plasma cell seen in RA
D. A macrophage containing large inclusions
B. A PMN with inclusions formed by immune complexes
A ragocyte (also called a rheumatoid cell) is a neutrophil containing cytoplasmic inclusions made up of immune complexes (IgG and complement) that have been phagocytosed.
They are characteristic of rheumatoid arthritis and other immune complex–mediated inflammatory joint diseases.
Which of the following crystals is the cause of gout?
A. Uric acid or monosodium urate
B. Calcium pyrophosphate or apatite
C. Calcium oxalate
D. Cholesterol
A. Uric acid or monosodium urate
Which crystal causes "pseudogout"?
A. Oxalic acid
B. Calcium pyrophosphate
C. Calcium oxalate
D. Cholesterol
B. Calcium pyrophosphate
Pseudogout is caused by the deposition of calcium pyrophosphate dihydrate (CPPD) crystals in the joint space, leading to acute inflammation and pain similar to gout but not due to uric acid.
These rhomboid-shaped crystals exhibit weak positive birefringence under polarized light, distinguishing them from needle-shaped, negatively birefringent uric acid crystals seen in true gout.
A synovial fluid sample is examined by using a polarizing microscope with a red compensating filter. Crystals are seen that are yellow when the long axis of the crystal is parallel to the slow vibrating light. When the long axis of the crystal is perpendicular to the slow vibrating light, the crystals appear blue. What type of crystal is present?
A. Calcium oxalate
B. Calcium pyrophosphate
C. Uric acid
D. Cholesterol
C. Uric acid
Interpretation of birefringence (under compensated polarized light):
When viewed with a red compensator, monosodium urate (MSU) crystals — the cause of gout — show negative birefringence:
Yellow when the crystal’s long axis is parallel to the slow (compensator) vibration direction.
Blue when perpendicular to the slow vibration direction.
In contrast, calcium pyrophosphate (CPPD) crystals (pseudogout) show positive birefringence — blue when parallel and yellow when perpendicular.
In which condition is the synovial fluid glucose most likely to be within normal limits?
A. Septic arthritis
B. Inflammatory arthritis
C. Hemorrhagic arthritis
D. Gout
C. Hemorrhagic arthritis
In hemorrhagic arthritis, the synovial fluid composition reflects blood contamination rather than metabolic or infectious inflammation, so glucose levels remain normal.
In contrast, septic, inflammatory, and gouty arthritis typically show decreased synovial glucose due to increased cellular metabolism and consumption by leukocytes and organisms.
Which statement about synovial fluid in RA is true?
A. Synovial:serum IgG is usually 1:2 or higher
B. Total hemolytic complement is elevated
C. Ninety percent of RA cases test positive for rheumatoid factor in synovial fluid
D. Demonstration of rheumatoid factor in joint fluid is diagnostic for RA
A. Synovial:serum IgG is usually 1:2 or higher
In rheumatoid arthritis, there is local (intra-articular) synthesis of immunoglobulins, especially IgG, within the inflamed synovium.
As a result, the synovial:serum IgG ratio is elevated (≥1:2), reflecting enhanced antibody production within the joint—a key immunologic feature of RA.
While rheumatoid factor is common (80–90%), its presence alone is not diagnostic, since it can occur in other chronic infections or autoimmune conditions.
Which of the following organisms accounts for the majority of septic arthritis cases in young and middle-age adults?
A. H influenzae
B. Neisseria gonorrhoeae
C. Staphylococcus aureus
D. Borrelia burgdorgeri
B. Neisseria gonorrhoeae
In young and middle-aged adults, especially those who are sexually active, Neisseria gonorrhoeae is indeed the most common cause of septic arthritis.
Staphylococcus aureus dominates in older adults, immunocompromised patients, or post-surgical/joint replacement cases.
Gonococcal arthritis typically presents as migratory polyarthritis or tenosynovitis with pustular skin lesions, reflecting disseminated gonococcal infection.
Summary:
<40 years / sexually active → N. gonorrhoeae
>40 years / general adult population → S. aureus
Which of the following hematology values best frames the URLs for synovial fluid?
Pattern: WBC Count, Percentage of PMNs, RBC Count
A. 200/uL, 25%, 2,000/uL
B. 5,000/uL, 50%, 10,000/uL
C. 10,000/uL, 50%, 50,000/uL
D. 20,000/uL, 5%, 500,000/uL
A.
WBC Count: 200/uL
Percentage of PMNs: 25%
RBC Count: 2,000/uL
Normal synovial fluid is clear, viscous, and acellular, with:
WBC count: <200/µL
PMNs: <25%
RBCs: <2,000/µL
Higher counts indicate inflammatory, septic, or hemorrhagic joint disease, depending on the pattern and cell predominance.