MODULE 1 - Pathogens and the Body's Defense System
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
pathogens
bacteria, fungi, viruses
bacteria, fungi and viruses can target specific organs or multiple body systems. This is known as being ________
pansystemic
bacteria is defined as
single celled organisms within the power to divide and multiple
each ____ of bacteria has different shapes and characteristics
strain
many forms of bacteria are _______ and even helpful to an animal’s body
harmless
there are bad strains of bacteria that cause _____ in both humans and companion animals
disease
Key facts about bacteria
single celled, capable of dividing and multiplying
spread through direct contact
have a simple structure without a true nucleus or membrane bound organelles
many bacteria are harmless or beneficial, but some strains cause disease in humans and companion animals
found in various environments — animals, humans, air, water, soil, plants
each strain has a different shape and characteristic
Basic components of bacteria
cell wall
plasma membrane
capsule (in some bacteria)
cell wall
provides structural support and protection
plasma membrane
surrounds the cytoplasm and distinguishes it from the external environment
capsule
aids in evading the host’s immune system
How bacteria can cause disease:
entry to host
adherence to cells
colonization and multiplication
evasion of immune system
production of toxins
inducing inflammation
disruption of normal functions
entry to host
ingestion: consuming contaminated food or water
inhalation: breathing in airborne bacteria
skin contact: entering through cuts, wounds, or mucous membranes
vectors: being transmitted by insects or other animalsa
adherence to host cells
once in body, bacteria must adhere to host cells to establish an infection
they use structures like pili or fimbriae to attach to surfaces of the cells in resp tract, GI tract, or other tissues
colonization and multiplication
after adhering to cells, bacteria colonize and multiply
form colonies on the surface of tissues or invade deeper into body
evasion of the immune system
capsules: some bacteria produce a protective capsule that prevents them from being engulfed by white blood cells
antigenic variation — changing their surface proteins to avoid detection by the immune system
inhibiting phagocytosis — producing substances that inhibit the ability of white blood cells to engulf and destroy them
production of toxins
can damage host tissues and disrupt normal cellular functions
exotoxins — secreted by bacteria that can cause damage to specific tissues or organs
—- example: clostridium botulinum, produces botulinum toxin which affects the nervous system
endotoxins: components of the bacterial cell wall that are released when the bacteria die and break apart. endotoxins can cause inflammation, fever, and septic shock
inducing inflammation
presence of bacteria and their toxins can trigger an inflammatory response in the host
inflammation is the body’s way of trying to contain and eliminate infection, but can also cause tissue damage and contribute to the symptoms of disease
disruption of normal functions
resp infections — bordetella and other bacteria can cause, leads to diffculty breathing, nasal discharge
GI infections: bacteria such as salmonella can cause. V/D, abdominal pain
systemic infections: staphylococcus aureus — spread through bloodstream, and affecting multiple organs
structure of fungi
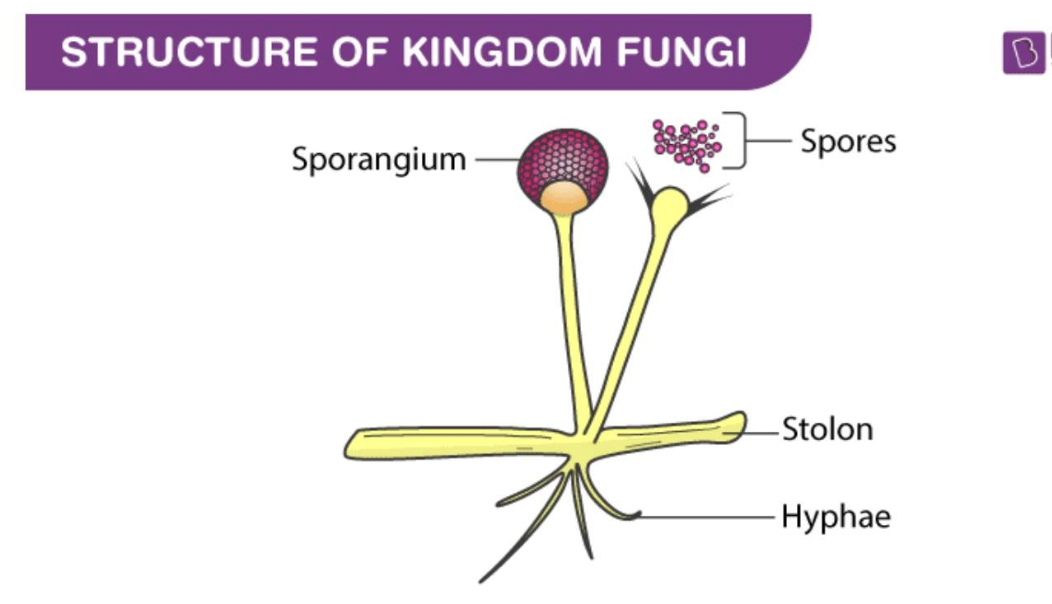
fungi or fungus
any member of the eukaryotic organisms (any cell or organism that possesses a clearly defined nucleus)
yeasts
molds
mushroomlike microorganisms
Key Points about Fungi
pathogenic fungi are parasitic, spore-producing organisms
obtain nourishment by absorbing food from their hosts
many species exist in the environment, but only a few cause infections
can be acquired by:
inhalation
ingestion
skin contact
some fungal infections can affect healthy animals; other require immunosuppressive agents or host that is immunocompromised
prolonged use of antimicrobial drugs or immunosuppressive agents increases the likelihood of fungal infections
Fungal diseases
localized or systemic
may be confined to surface (ringworm) or become systemic (systemic mycosis)
affect various parts of the body; each species having preferred locations (lungs, eyes, lymph nodes
types of fungi that commonly affect pets are abundant in ____ and tend to adhere to specific geographic locations
soil
Histoplasmosis location
midwest/south (texas, OK, colorado)
blastomycosis location
north and south (michigan and wisconsin, NC, SC, GA)
C gatti cryptococcosis location
california, washington, oregon
systemic fungal diseases tend to affect three types of pets most commonly:
young, large breed dogs
pets that have a weakened immune system
pets that are taking cyclosporine
how fungi cause disease
entry to host — inhalation, skin contact, ingestion
adherence and colonization — once inside body, adhere to tissues and begin to colonize. can grown on surface of tissues or invade deeper into body
evasion of immune system — thick cell walls: providing protection against immune responses, changing forms: switching between yeast and mold forms to avoid detection
tissue damage — direct evasion: evading and destroying host cells, enzyme production: break down host tissues, facilitate further evasion
inducing inflammation — inflammatory response leads to redness, swelling, painVir
Virus characteristics
obligate intracellular pathogens
small microbes that cannot replicate or live outside cell
debate whether viruses are living organisms
no cell wall, able to reproduce independently
composed of nucleic acid core (DNA/RNA) surrounded by protein capside
can be enveloped (lipoprotein coating) or non-enveloped
promote replication, not necessarily to kill host
virus structure
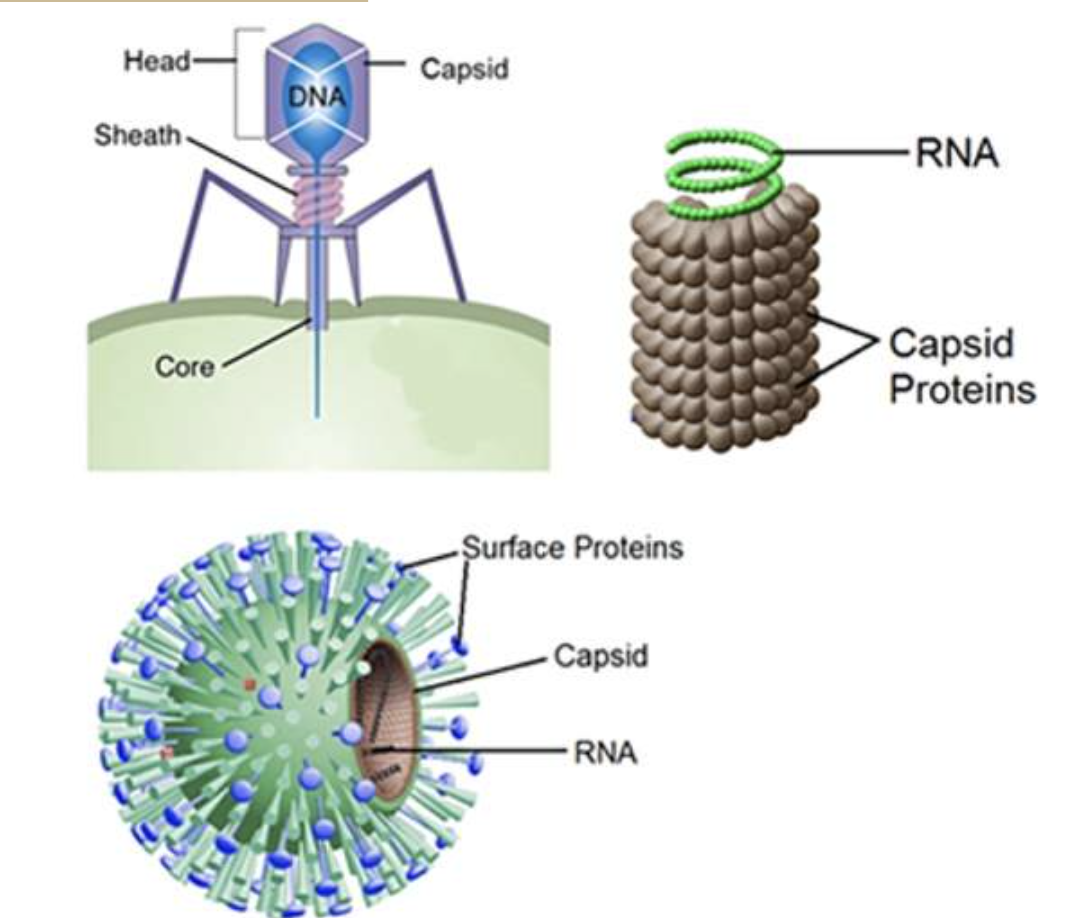
steps of viral infection
Attachment - binds to specific receptors on host surface
absorption/penetration - invades host cell, breaks down capsid, injects genetic material into cytoplasm
Biosynthesis - inhibits host cells DNA, RNA, or protein synthesis. Uses host cell’s resources to reproduce viral genome and proteins
Assembly - new virions are formed inside host cell
Release - leave host cell via exocytosis (enveloped viruses) or lysis (non-enveloped viruses)
possible outcomes include minimal host cell damage, host cell destruction, or malignant transformation
Bacterial diseases
Leptospirosis
bordetella
brucellosis
salmonellosis
tetanus
hemorrhagic septicemia
anthrax
fungal diseases
cryptococcus
blastomyces
histoplasma
aspergillus
coccidiodes
candidiasis
viral diseases
panleukopenia
rhinotracheitis/calcivirus
FIV
FeLV
FIP/Feline Coronavirus
Rabies
Distemper
Parvovirus
Canine Influenza
Lyme
Toxoplasmosis
Canine Monocytic Ehrlichiosis
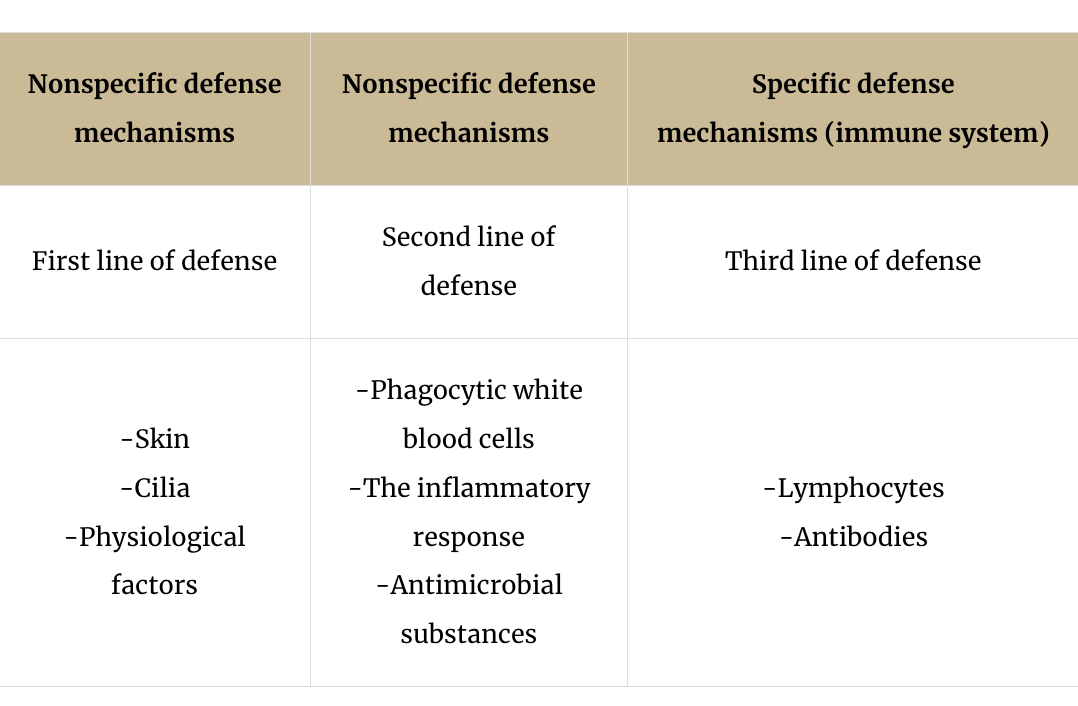
Nonspecific immunity
composed of many elements, responds to any pathogen in the same way every time
species resistance: genetic ability of a species to defend against certain pathogens
mechanical/physical and chemical barriers: skin and mm = mechanical, chemical = sebum, mucus, enzymes
healthy skin = first line of defense
inflammatory response
Activated when tissues are invaded or injured.
Mediators attract white blood cells, dilate blood vessels, and increase permeability.
Signs: Heat, redness, swelling, pain.
Neutrophils perform phagocytosis to eliminate invaders.
interferon and complement
interferon = prevents viral replication within host cells
complement = enzymes that create holes in invading cell walls, causing lysis
Specific immunity
third line of defense/final defense
cell mediated immunity
T cell lymphocytes
T cells recognize and destroy pathogens directly
origin: bone marrow, mature in thymus
rapid and targeted response
Humoral immunity
conducted by B-cell lymphocytes
B cells produce antibodies in response to specific antigens
origin: bone marrow or bursa of Fabricus
slower respone, involves memory cells for quicker future responses
differential immunity chart
other immunity types
species resistance
mechanical barriers
chemical barriers
species resistance
Definition: The genetic ability of a particular species to provide defense against certain pathogens.
Example: Canines do not acquire feline leukemia virus, and felines do not contract canine distemper virus.
mechanical barriers
Definition: Physical structures that prevent the entry of microorganisms into the body.
Example: The skin and mucous membranes act as a barrier to protect underlying tissues from injury and infection.
chemical barriers
Definition: Substances produced by the body that inhibit or destroy pathogens.
Example: Sebum, mucus, and enzymes produced by the skin and mucous membranes that act to inhibit or destroy pathogens
inherited immunity
Genetic factors influencing immunity before birth/ is the immune system that is inherited
acquired immunity
Develops after birth.
Natural: Result of exposure to pathogens.
Artificial: Result of vaccinations.
Acquired Immunity:
Learns from previous encounters, responds more effectively upon re-exposure.
passive immunity
Transfer of antibodies from one animal to another (through placenta, blood products, injections)
Provides immediate but temporary protection.
active immunity
Animal's own immune system produces a response to a pathogen.
Provides long-lasting protection.
Virus-Host Interaction:
Inherited /Innate Immunity: Destroys many viruses before they infect cells.
Acquired immunity: Antibodies recognize viral proteins, prevent cell entry, and target the virus for destruction.
Vaccination
utilizes humoral response by introducing antigens to stimulate antibody production
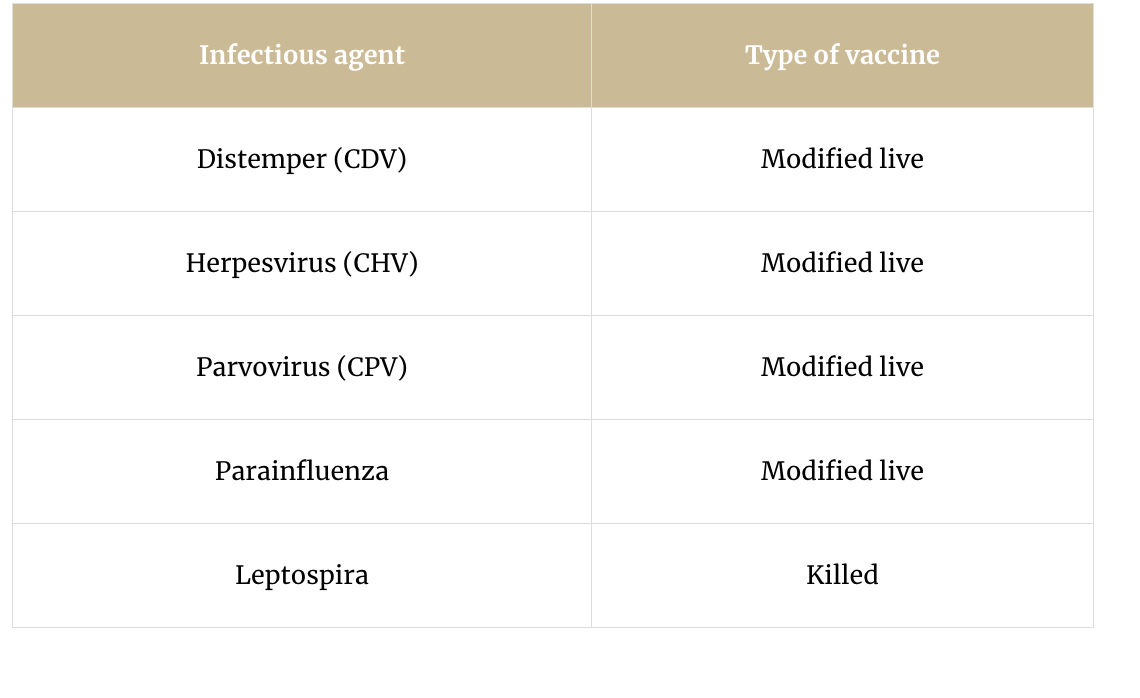
type of vaccines
killed virus — inactive, incapable of causing disease
modified live virus — genetic material altered to reduce virulence
vaccination mechanism
process — initial antigen exposure triggers antibody production
booster shots — enhance and prolong antibody response
anamestic response — memory response from immune system leading to faster and stronger reaction upon re-exposure
importance of multiple injections
Maternal Antibodies: Received at birth, protect initially but can interfere with vaccine efficacy.
Vaccination Schedule:
Start at 8 weeks, boosters every 3-4 weeks until 12-16 weeks. (Depends on age starting if older than this).
Certain breeds (e.g., Rottweilers, Dobermans) may require longer schedules.
Risk of Infection:
Window where maternal antibodies block vaccines but don’t protect against infection, leading to potential vulnerability.
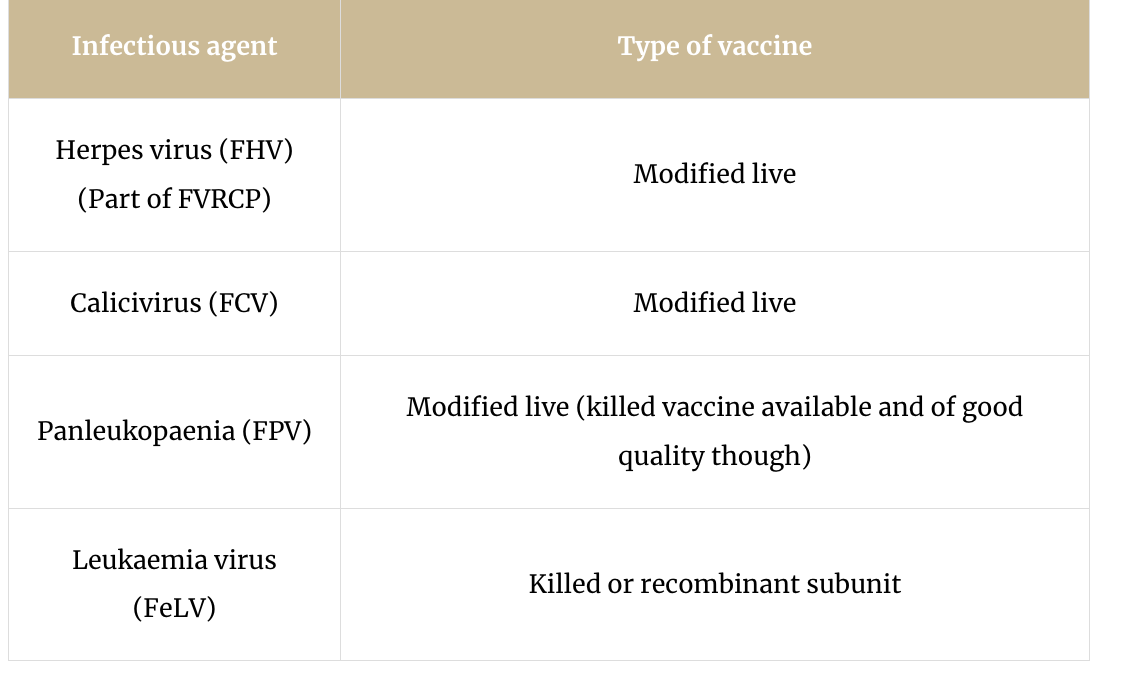
cat vaccines
dog vaccines