Lecture 3 Psychosis and Schizophrenia
1/34
Earn XP
Description and Tags
MBB2
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
The Psychoses - Definition
The term ‘psychosis’ is an umbrella term meaning ‘out of touch with reality’.
Can refer to a variety of clusters of symptoms. These symptoms can occur not only in schizophrenia spectrum disorders, but also in a range of disorders including:
organic presentations like dementia.
Substance use: amphetamine psychosis, and so on
At the disorder level, psychosis refers to a group of disorders distinguished from one another in terms of:
symptom configuration (e.g., delusional disorder versus schizophrenia).
Delusional beliefs that are either Non-bizarre (plausible, e.g., “I am being poisoned,” “My partner is unfaithful”) or bizarre delusion (implausible and not derived from ordinary experiences; e.g., “aliens replaced my organs with plastic”).
duration (e.g., schizophrenia versus schizophreniform disorder)
< or > than 6 months
relative pervasiveness - in terms of both duration and the clinical picture - of psychotic symptoms versus affective symptoms (e.g., bipolar disorder and schizoaffective disorder). Which is the core?
Psychoses (schizophrenia)
Focus here is on schizophrenia but I will point out differences between it and other psychotic disorders as we proceed.
The term ‘schizophrenia’ refers to “split mindedness” or “a mind torn asunder” (Bleuler).
Schizophrenia it is not multiple personalities (i.e. not Dissociative Identity Disorder).
Schizophrenia involves disruption in various aspects of perceiving, thinking, feeling and behaviour. Phenomena associated with schizophrenia can be classified into two major groups of symptoms – positive symptoms and negative symptoms
Positive symptoms – additive to normal experience.
Negative symptoms – deficit in normal function
Psychosis: Positive symptoms
Hallucinations
Delusions
Hallucinations
A perception in the absence of environmental stimuli.
Hallucinations occur in any sensory modality, of which auditory is the most common then visual.
For example, “I can hear a voice that is providing a running commentary of what I am doing in the third person. It just said, ‘he is watching the lecture’.”
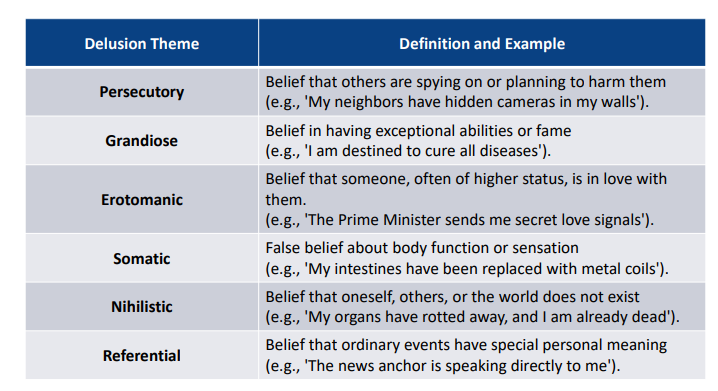
Delusions
A fixed and false belief that is not amenable to change in light of conflicting evidence.
Can be “bizarre” or “non-bizarre”.
For example, “I believe that an interdimensional being is making me feel sad today”.
Delusions theme
-
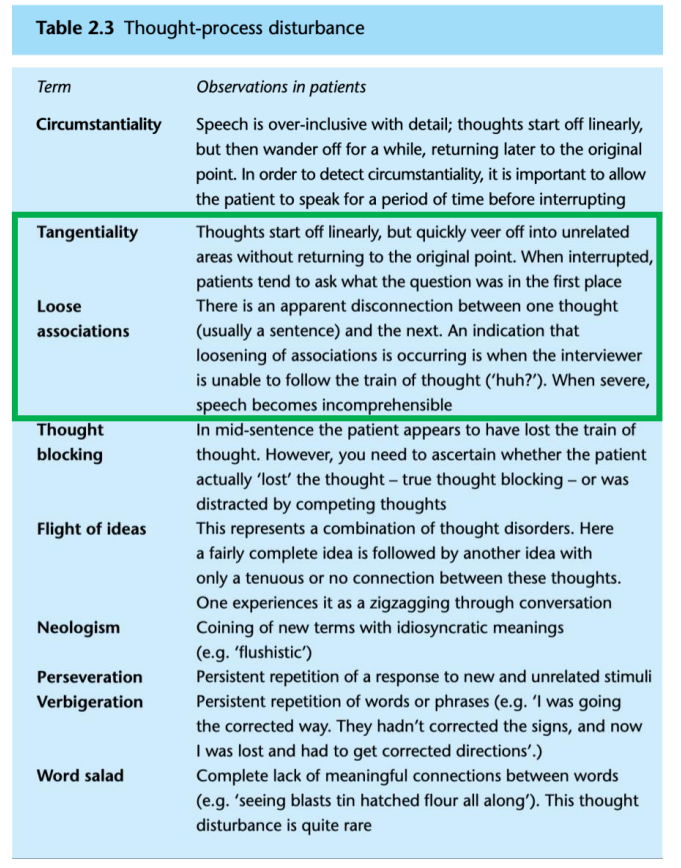
Thought Disorder
-
Psychosis: Negative symptoms and others.
Negative symptoms
Avolition
Alogia
Anhedonia
Affective flattening
Inattention
Other symptoms
Catatonia
Incongruent or in appropriate affect
Bizarre behaviour
Avolition
lack of motivation to achieve goals
Alogia
includes poverty of speech (less speech than normal), poverty of content of speech (less content than normal - vague), latency of speech and thought blocking
Anhedonia
inability to experience pleasure
Affective flattening
dulled emotional expression
Inattention
disturbance in selective attention
Catatonia
immobility, rigidity, and unusual posturing, as well as abnormal speech (e.g., mutism, echolalia) and movement patterns
Incongruent or inappropriate affect
Display incongruent with person’s emotion or inappropriate to context
Bizarre behaviour
No rational basis.
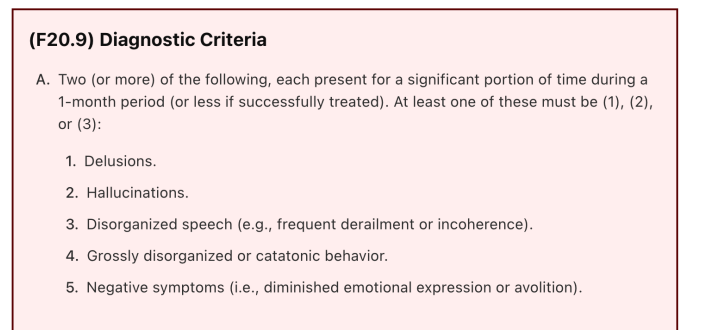
Schizophrenia diagnostic criteria - symptoms
-
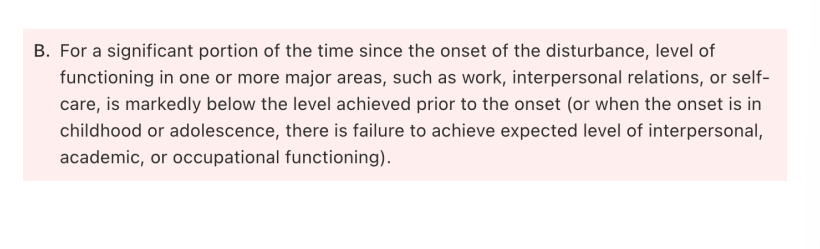
Schizophrenia Diagonostic criteria - relations
-
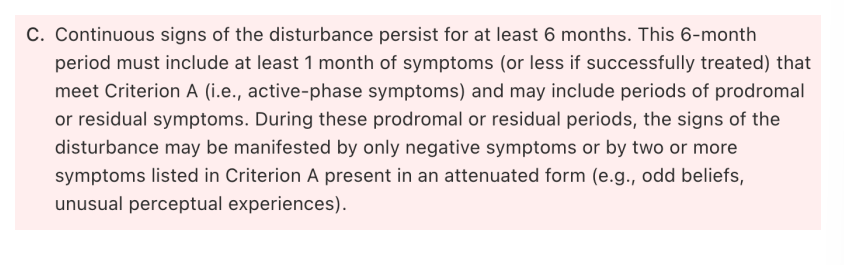
Schizophrenia diagnostic criteria - signs of disturbance
-
Schizophrenia diagnostic criteria - differentiate from other diagnostics
-
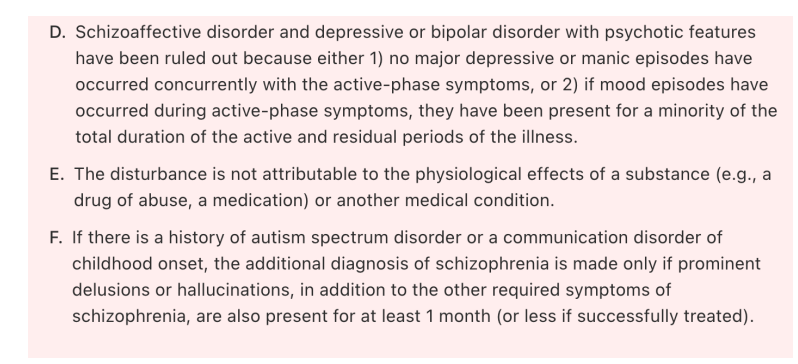
Schizophrenia diagnostic criteria - specifics
-
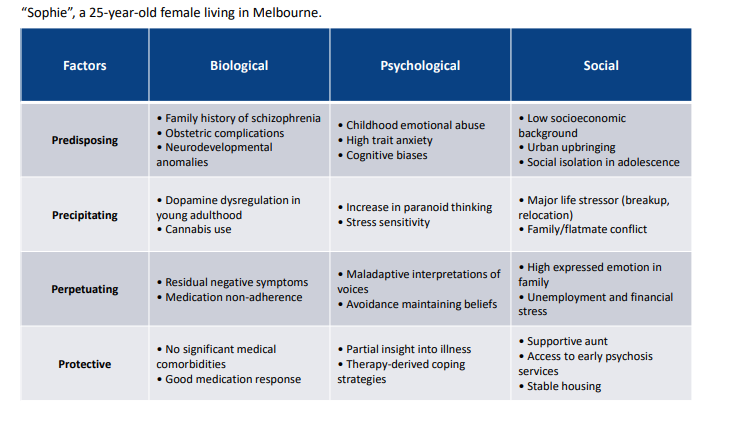
Biopsychosocial Case Formulation
-
History of psychosis and schizophrenia
Descriptions of psychotic experiences occur throughout historical and religious texts. Explanations of psychosis in these sources are often supernatural.
But when was the first purposeful and scientific description of what we now call schizophrenia?
Benedict Augustine Morel (1860) – “Démence précoce”
Morel was the first to rigorously describe what we now understand as schizophrenia.
His observations focused on individuals exhibiting a specific set of symptoms, marked by early onset and a deteriorating course of illness.
He recognized the progressive nature of the disorder, which led to the term “démence précoce” (early dementia), referring to the early onset of cognitive decline
Emil Kraepelin (1898) refined Morel’s concept and introduced the term “dementia praeco”
The key features of dementia praecox for Kraepelin were:
Early onset: Symptoms typically appear in late adolescence or early adulthood.
Progressive deterioration: The illness often leads to cognitive decline over time.
Symptom clusters: Focused on hallucinations, delusions, emotional dysfunction, and cognitive impairments.
Distinction from other disorders: Kraepelin differentiated schizophrenia from manic-depressive psychosis (bipolar disorder) and others based on the course and long-term outcome.
His work in “Compendium der Psychiatrie” (Compendium of Psychiatry; 1883), helped shape the classification of mental disorders and laid the groundwork for modern psychiatric diagnosis.
Paul Eugen Bleuler (30 April 1857 – 15 July 1939) - ‘Schizophrenia’
Dementia Praecox or the Group of Schizophrenias” (1908 - paper/1911 - book) presented a broader definition than Krapelin’s.
Disagreed with Kraepelin – based on his observation that schizophrenia does not necessarily display early onset, deteriorating course and therefore not characteristic of a dementia.
Emphasised splitting of associative processes in thought, affect and action – this seen as the core of the disorder. Four “A”s were Bleuler’s primary symptoms.
1. Association (disorganised thinking) – Impaired logical connections in thought, leading to disorganized speech and thought disorder.
2. Affect (emotional disturbance) – Inappropriate or blunted emotional responses, often mismatched with the situation.
3. Ambivalence (conflicting thoughts & feelings) – Holding contradictory beliefs, emotions, or desires at the same time, leading to indecision.
4. Autism (social withdrawal & inner world preoccupation) – Detachment from reality, with focus on internal thoughts rather than external reality
Kurt Schneider (7 January 1887 – 27 October 1967)
In 1959,proposed ‘first rank symptoms’ and made the diagnosis on cross section (deemed duration criteria not necessary) .
11 first rank symptoms: Hearing one’s voice out loud; hallucinatory voices talking about him or her; hallucinations in the form of a running commentary; somatic hallucinations produced by external agencies; thought withdrawal; thought insertion; thought broadcasting; delusional perception (ideas of reference); made feelings, made actions; made impulses.
Problems with Schneider’s approach:
These symptoms are not specific to schizophrenia (not ‘pathognomonic’)
Cross-sectional diagnosis a problem too. Consider DSM-5-TR diagnosis “brief psychotic disorder”, for example
Modern diagnostic tools
like the DSM-III (1980) and its successor, including DSM-5-TR, emphasize narrow (Neo-Kraepelinian) view of schizophrenia.
Diagnosis is based on criteria that:
Outline signs and symptoms, duration of disturbance, and impact of functioning that is characteristic of schizophrenia.
Highlight exclusion factors.
Psychological, social and environmental, and behavioural risk factors for psychosis
Migration and discrimination: First-generation migrants have increased risk, while second-generation migrants face an even higher risk of developing psychosis. Migrants from developing countries or who live in areas where they experience prejudice and discrimination exhibit high risk. Social adversity is high, support can be lower.
Urbanicity: Living in urban environments during childhood or adolescence increases schizophrenia risk by approximately 2-fold, likely due to chronic social stress and reduced social cohesion.
Expressed emotion (EE): High levels of EE (hostility, criticism, over-involvement) in families are associated with increased relapse rates and symptom severity in schizophrenia.
Cannabis use: Cannabis use during adolescence is consistently linked to a higher risk of psychosis, particularly in genetically predisposed individuals.
Schizotypal personality traits: Schizotypal personality traits are significant predictors of psychosis risk, especially when combined with cognitive deficits and other vulnerabilities including exposure to stress and developmental trauma. Related to genetic vulnerability.
Genetic contributions to schizophrenia and psychosis
Genetics play an important and complex role in determining who might be at risk for schizophrenia and other psychotic disorders. Schizophrenia is highly polygenic
This means that many different genes—hundreds or even thousands— each play a small role in increasing the risk of schizophrenia. No single gene causes schizophrenia. Instead, it’s the combined effect of many genes working together.
Both common and rare genetic variations contribute to risk for schizophrenia.
Common variations (in the general population) contribute just a little.
Rare variations (e.g. ‘copy number variants’ – DNA section deletion or duplication) tend to have greater impact.
Genetic risk is increased if family history is present.
Gene-environment interactions: Stressors usually required to activate genetic vulnerability. Risk increases with age as stressors accumulate
How do genes work to create risk for psychosis?
Many of the genes linked to schizophrenia are involved in how brain cells communicate with each other at the synapse (the connection between two neurons).
These genes affect brain development and how neurons are organised.
Schizophrenia shares some genetic risk factors with other conditions, like bipolar disorder or autism.
This means that mental health conditions sometimes (often) have overlapping biogenetic roots.
It is not surprising that psychotic symptoms occur transdiagnostically (across disorders)
Understanding the biogenetic contributions to schizophrenia can help us
Identify people who might be at higher risk.
Develop better treatments by targeting specific biological pathways.
Reduce stigma by showing that schizophrenia is influenced by biology, not just personal choices or behavior. Although, the opposite can also be true – focusing on biogenetic explanations can increase perceptions of uncontrollability.
Structural brain abnormalities in schizophrenia
Reduced grey matter volume in schizophrenia
Prefrontal Cortex (PFC) – Impaired decision-making, planning, and cognitive control; contributes to disorganized thinking and executive dysfunction.
Temporal Lobes – Involved in auditory processing and memory; reductions here are linked to hallucinations (especially auditory) and memory deficits.
Hippocampus – Critical for memory formation and reality monitoring; reduced volume is associated with disrupted memory and difficulties distinguishing reality from delusions.
Amygdala – Regulates emotion and threat perception; volume reductions may contribute to blunted emotional responses or heightened paranoia.
Thalamus – A key sensory relay station; reductions may lead to abnormal sensory processing and cognitive disturbances, possibly contributing to hallucinations and thought disorders.
White matter abnormalities in schizophrenia
Disrupted connectivity between brain regions (especially between the PFC, thalamus, and hippocampus) leads to impaired communication and disorganized thinking.
Enlarged Ventricles – Larger fluid-filled spaces suggest loss of surrounding brain tissue, a common finding in schizophrenia, often linked to cognitive deficits and more severe symptoms
What treatments work for schizophrenia?
Antipsychotic medications – cornerstone of treatment, effective for positive symptoms, less so for negative/cognitive symptoms.
Psychosocial interventions – including CBT for psychosis, social skills training, supported employment; improve functioning and reduce relapse.
Family interventions – psychoeducation and support reduce expressed emotion and lower relapse risk.
Early intervention services – coordinated care for first-episode psychosis improves long-term outcomes.
Lifestyle and physical health care – addressing cardiovascular risk, smoking, and physical activity supports overall recover