lec 17. Benign tumors
1/64
Earn XP
Description and Tags
KNOW THE LANGUAGE - dr. Lipka
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
benign vs. Malignant tumors
also what is lytic lesions and in which type of tumor do we find these?
benign | malignant | |
well-define | lytic lesion | |
smooth/oval shape | irregular shape | |
no skin dimpling | skin dimpling | |
note: ***lytic lesions are spots of bone damage that result from cancerous plasma cells building up in your bone marrow.***
the “needs to know” from the patient to predict a tumor is present (history)
age
habits
duration of c/o
rate of growth
any pain
trauma hx
pfmx of cancer
systemic signs
The most common benign bone tumor
osteochondromas
what type of tumor is this?
outgrowths of normal bone and cartilage in abnormal locations.
most often in people aged 10 to 20
may be single or multiple.
Multiple tend to run in families.
The Plain film will cause an initial “scare”
Osteochondromas
secondary malignant chondrosarcoma develops in about
___% of patients with multiple osteochondromas
and
in ___ %of those with single lesions.
10% in mulitple
less than 1% in single

X-rays demonstrate a bony outgrowth from the cortex.
what type of tumor is this?
—> osteochondroma
The trabecular pattern and density of the outgrowth are the same as in the normal bone.
no reactive bone at the base.
The lesion may be stalked (pedunculated) or flat (sessile).
Pedunculated lesions usually point away from the adjacent joints.
!! Because most of the tumor is the cartilage cap, the x-ray opacity is smaller than the mass feels clinically. !!
Hereditary multiple osteochondromatosis
follows what type of heredity?
Autosomal dominant condition
that can lead to both sessile (flat) and pedunculated (stalked) lesions
note: The lesions may occur on different bones or on the same bone, and symptoms present in the first decade of life.
what is the risk of osteochondromas to become malignant (chondrosarcoma)?
is sessile or pedunculated (stalked) lesions more likely to become a sacrome?
hereditary multiple osteochondromatosis is unknown
but may be 25-30% compared to approximately 1% for a solitary osteochondromas.
a sessile lesion is more likely to degenerate into sarcoma than an exostosis.
what two things increases the chances of osteochondromas to become malignant —> chondrosarcoma?
number (mutli vs single tumor(s))
&
size
what are the 4 reasons we tx osteochondromas?
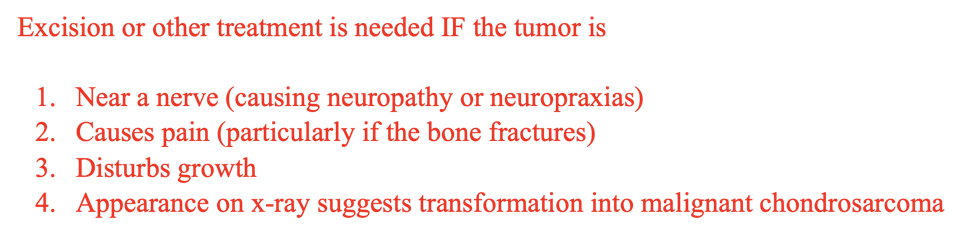
… basically if it causes a problem lol
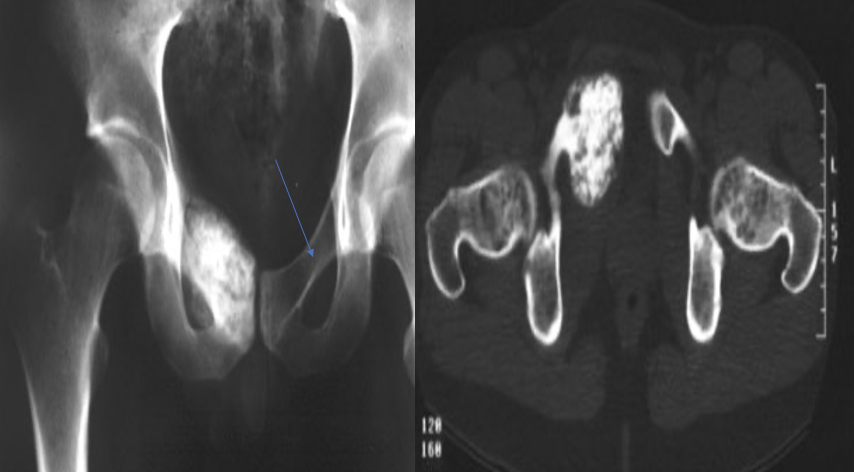
what is this disorder?
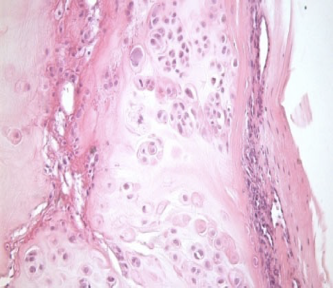
the medullary bone is replaced by fibrous tissue,
which appears radiolucent on radiographs,
w/ GROUND GLASS appearance.
Trabeculae of woven bone contain fluid-filled cysts that are embedded largely in collagenous fibrous matrix, which contributes to the generalized hazy appearance of the bone
Fibrous dysplasia
a skeletal developmental problem
what occurs to the medullary bone in fibrous dysplasia?
replaced by fibrous tissue,
what does the Trabeculae bone look like in fibrous dysplasia?
Trabeculae of woven bone
contain fluid-filled cysts
embedded largely in collagenous fibrous matrix,
—> causes HAZY appearance on x-rays
whats the apperance of fibrous dysplasia on a plain radiograph?
—> ground glass , radiolucent - medullary bone
—> hazy due to fluid cysts in trabulae bone
what are the 4 disease patterns of Fibrous Dysplasia??
Monostotic form
Polyostotic form (up to 75% of skeleton)
Craniofacial form
Cherubism
Monostotic fibrous dysplasia affects only ____ bone,
most commonly: ???
one bone
Ribs , proximal femur ,craniofacial bones.
which is more common: monostotic or polystotic fibrous dysplasia?
Monostotic fibrous dysplasia is:
7-10 times more common than polyostotic fibrous dysplasia.
note:
It also can be associated with systemic conditions,
precocious puberty and skin pigmentation (as in McCune-Albright syndrome)
soft-tissue myxomas (as in Mazabraud syndrome)
what systemic cond’s can monostotic fibrous be associated with?
precocious puberty and skin pigmentation (as in McCune-Albright syndrome)
soft-tissue myxomas (as in Mazabraud syndrome)

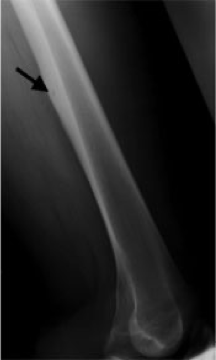
Plain radiograph of a tibia in a patient who is skeletally mature, demonstrating expansion of the metaphysis and diaphysis, endosteal scalloping, and a ground glass appearance of the matrix.
what disorder is this?
Fibrous dysplasia
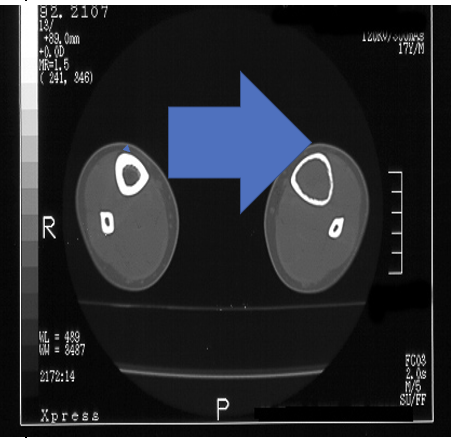
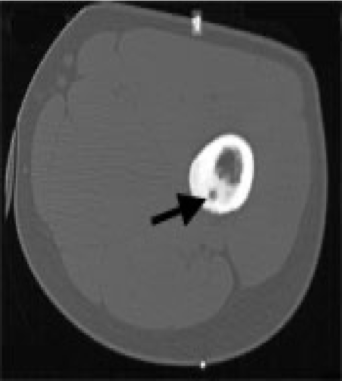
CT scan of the tibia
what is the arrow showing?
what disorder is this most likely?
fibrous dysplasia
CT scan of the tibia —> Expanding intramedullary lesion
Fibrous dysplasia —> Medical therapy??
conservative and primarily to prevent deformity.
Treat any underlying endocrine disturbance.
In upper extremity lesions —> most respond to nonsurgical management.
No specific medical treatment exists for the bone disease
although early evidence suggests that vitamin D and bisphosphonates after physeal closure (growth plate fusion) may be helpful in ameliorating pain and possibly in reconstituting lesions with normal bone.
Bisphosphonates used have included
alendronate, pamidronate, etidronate, risedronate, tiludronate and zoledronate.
Pamidronate has been used the most and is usually given intravenously as an infusion of 180 mg over 3 days every 6 months.
Concomitant calcium (500-1500 mg/day) and vitamin D2 (800-1200 IU/day) must be given to avoid secondary hyperparathyroidism.
These agents are used Intravenously to treat the hypercalcemia of malignancy
Ca, vit D, biphosphates
what drugs are given to prevent secondary hyperparathyoidism in someone with fibrous dysplasia ?
calcium and vit D
what are the 3 medications that you can give to someone with fibrous dysplasia?
Ca
vit D
biphosphates (after growth plate closes)
when do we take a pt to surgery with fibrous dysplasia
Severe or progressive disease
Nonunion
Persistent pain
Fracture of a weight bearing bone
Curettage is affective but may not be permanent
Long bones require stabilization only, and this is best achieved by intramedullary nail fixation.
Expendable bones can be treated by excision.
Deformity may require corrective osteotomy and internal fixation. A vascularized fibular graft has been used for some lesions with success
20’s- 40’s year olds
They are usually located within the bone marrow cavity.
forms mature cartilage
These tumors are usually asymptomatic but may enlarge and become painful.
located in the small bones of the hand and/or feet
can be found elsewhere
often found when x-rays are taken for another reason.
On x-ray, the tumors may appear lytic, with areas of stippled calcification.
usually visible on a bone scan and thus may raise concern of a malignancy.
Chondroma
Chondroma types?
classified according to their location:
enchondroma: within the bone (within the medullary cavity),
periosteal chondroma: on the surface of the bone,
soft tissue chondroma: in the soft tissue.
chondroma: X-ray findings may be diagnostic; if they are not, or if the tumor is painful, the diagnosis should be confirmed by??
biopsy.
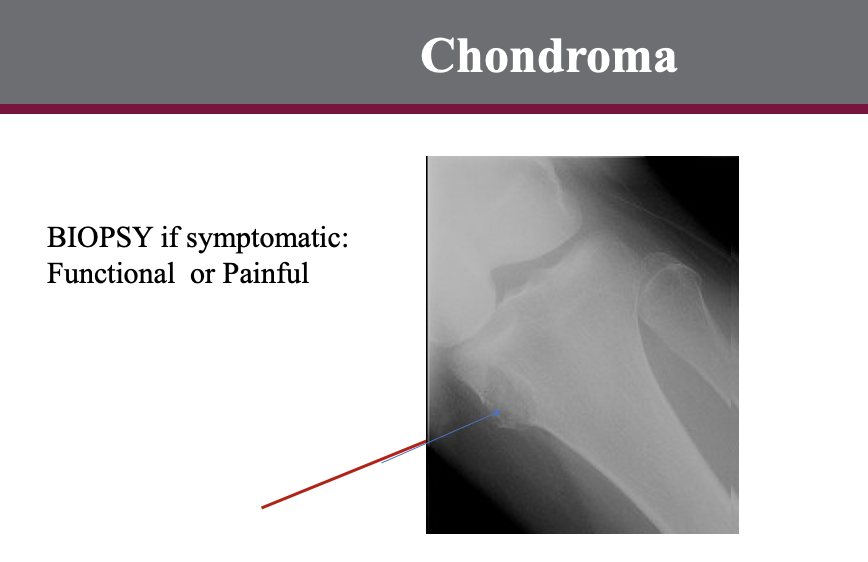
An asymptomatic chondroma does not need excision or other treatment;
follow-up x-rays are indicated to rule out disease progression.
These are performed 6 months and 1 year later or whenever symptoms develop
a well circumscribed, solitary fibrous proliferation.
This lesion is found mostly in children with 75% occurring in the second decade.
The lesion is found in males more commonly than in females and may occur in as many as 35% of all children.
It is a non-neoplastic process that occurs in the juxtaepiphyseal region of the long bones.
The most common site is the femur followed by the tibia.
Asymptomatic and are usually discovered as an incidental finding on x-ray.
Occasionally, a larger lesion presents as a pathologic fracture.
Very typical appearance on x-ray.
They are eccentric, multi-loculated sub-cortical lesions with a central lucency and a scalloped sclerotic margin.
There is sometimes cortical thinning but NO periosteal reaction.
Serial x-rays will show the lesion migrating away from the epiphyseal plate with time.
These lesions normally regress spontaneously.
The only definite indication to treat pathologic fracture.
The natural history of these lesions is that they either spontaneously resolve or move to the diaphysis of the bone.
Non-ossifying fibroma (NOF)
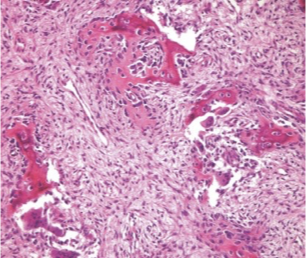
Non-ossifying fibroma (NOF)
Asymptomatic
usually discovered as an incidental finding on x-ray.
Occasionally, a larger lesion presents as a pathologic fracture.
Very typical appearance on x-ray.
They are eccentric, multi-loculated sub-cortical lesions with a central lucency and a scalloped sclerotic margin.
There is sometimes cortical thinning but NO periosteal reaction.
Serial x-rays will show the lesion migrating away from the epiphyseal plate with time.
whats the only definite indication to tx non-ossifying fibromas?
a pathologic fracture.
(T/F) Non-ossifying fibroma (NOF) regress spontaneously?
mostly true
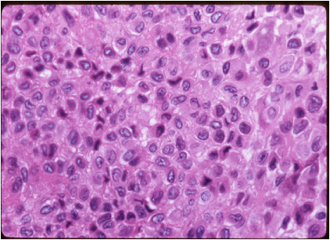
Sometimes called “Codman's tumor”,
is a rare type of benign bone tumor that originates from cartilage.
Chondroblastoma
most often affects the ends of the long bones
in the arms and legs at the hip, shoulder, and knee.
is rare, occurring most commonly in people aged 10 to 20.
Arising in the epiphysis, this tumor may continue to grow and destroy bone.
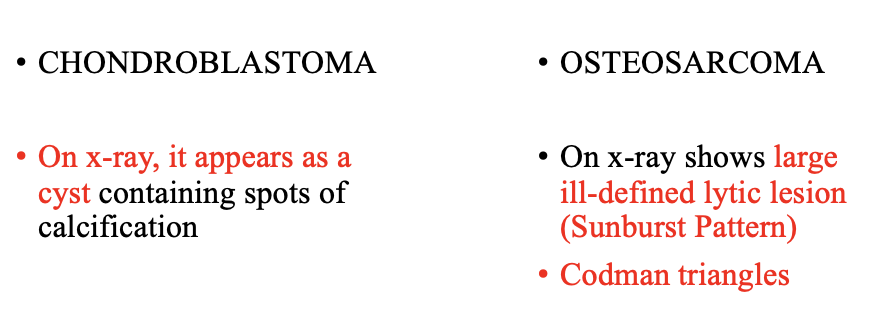
On x-ray, it appears as a cyst containing spots of calcification.
The lesion is lytic with well defined margins
Scalloping or expansion of cortical bone may be present.
Fine calcifications, either punctate or in rings, may be visible.
Cysts are present about 20% of the time and both MRI and CT can define the fluid levels.
Chondroblastoma
tx for chondroblastoma?
It MUST BE surgically excised/removed
bone grafting
physical therapy (to restore strength and function after surgery)
The tumor may recur.
For this reason, follow-up with your physician is essential!!!!
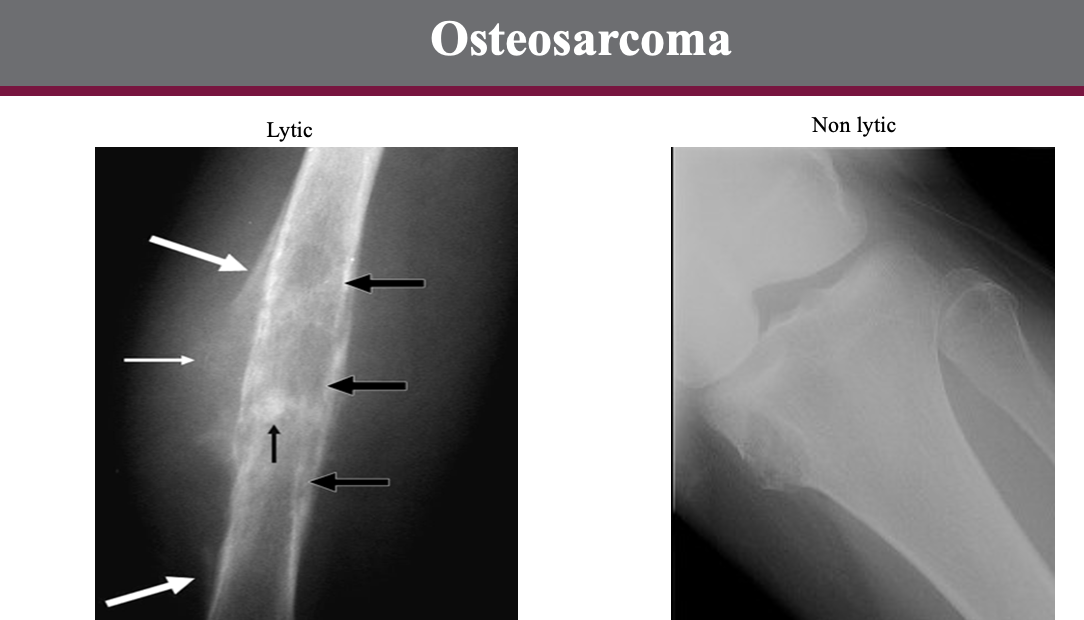
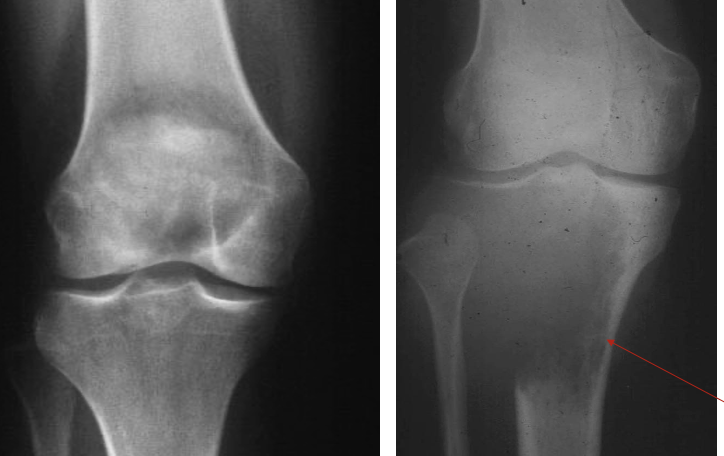
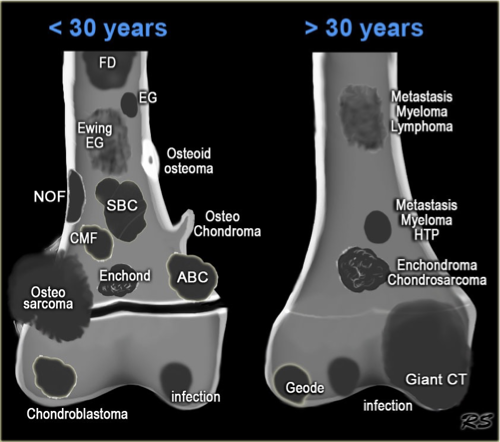
RADIOGRAPHIC Comparison of lesions
Chondroblastoma vs. osteosarcoma
why is CT used for chondroblastoma’s?
defining the relationship of the tumor to the joint,
integrity of the cortex,
intralesional calcifications.
this is symptoms of….?
may vary depending on the location of the tumor.
pain in the knee, hip, and shoulder joint (pain may be slight or moderate and may be present for months or years)
withered or shrunken appearance of the muscle near the affected bone
impaired mobility of the adjacent joint
fluid accumulation in the joint adjacent to the affected bone
Chondroblastoma
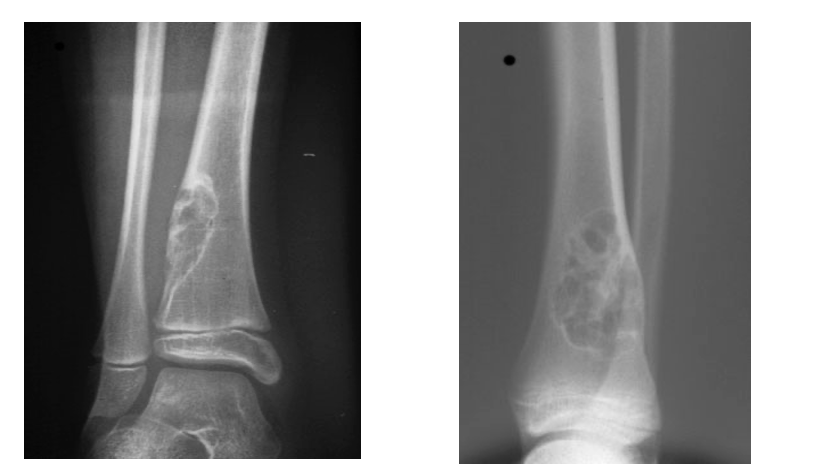
rare and occurs before age 30.
Its x-ray appearance (usually eccentric, sharply circumscribed, lytic, and located near the end of long bones)
Treatment is surgical excision or curettage.
Chondromyxofibroma

Radiological findings demonstrate an eccentrically placed Lytic lesion with well defined margins in the metaphysis of the lower extremity.
The lesion usually has a sclerotic margin of bone and a lobulated contour.
Ridges and grooves that appear in the margins
secondary to scalloping falsely appear to be trabeculae.
If not sure —> BIOPSY
Chondromyxofibroma
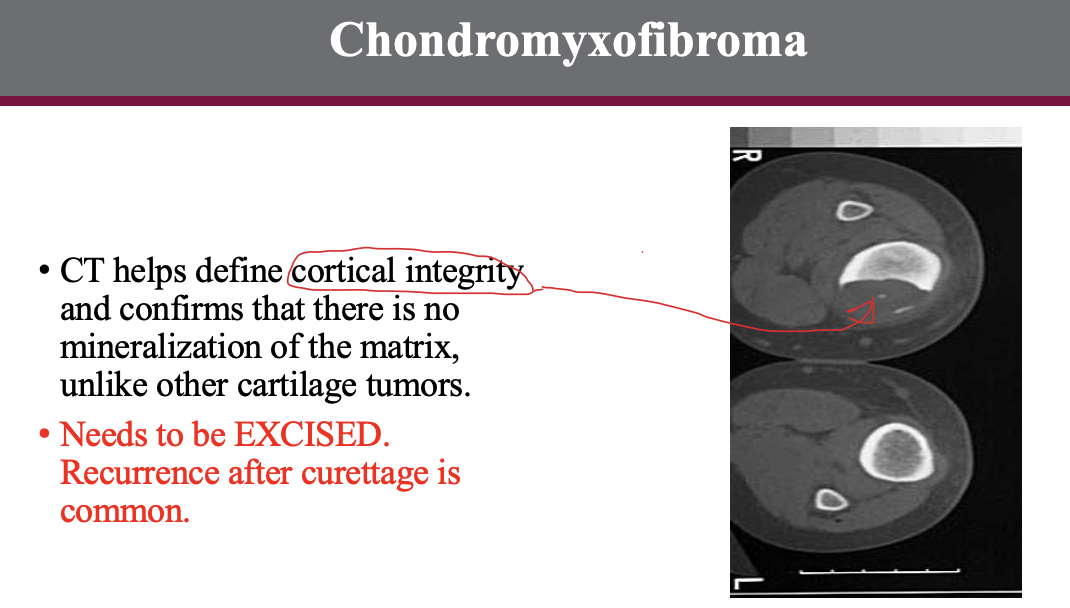
in CT for Chondromyxofibroma,
helps define what???
define cortical integrity
and confirms that there is no mineralization of the matrix, unlike other cartilage tumors
(MALES » females)
tends to affect young adults, can occur in any bone but is most common in long bones.
The proximal femur is the most common site.
Dull aching pain is the most frequent symptom.
can cause pain (usually worse at night)
typically relieved by mild analgesics, particularly aspirin.
Physical examination may reveal atrophy of regional muscles.
Characteristic appearance on x-ray:
is a small radiolucent zone surrounded by a larger sclerotic zone.
If a tumor is suspected, a technetium-99m bone scan should be performed;
—> appears as an area of increased uptake.
MAY have a unique pathogenic nerve supply as well, a unique finding among bone tumors
Permanent relief is obtained if the small radiolucent zone is removed surgically or with percutaneous radiofrequency ablation.
Osteoid osteoma - The most common benign osteoid-forming tumor
in osteoid ostemoa — Permanent relief is obtained if …?
small radiolucent zone is removed surgically
or
with percutaneous radiofrequency ablation.
(most significant symptom of osteoid osteoma is pain)
how are symptoms relived for someone with osteoid osteoma w/o surgery or ablation?
(NSAIDs)
secondary to a high concentration of prostaglandins in the nidus.
Pain can be treated with aspirin, ibuprofen or other over-the-counter anti-inflammatory drugs.
Some patients have relief with a given medication for a while, but then it stops working.
A change to another anti-inflammatory medication may then be required.
Osteoid Osteoma
Imaging usually is very typical:
X-rays show new bone formation and sometimes a small lucent spot (smaller than 1.5 cm), which is defined as the nidus.
recall: pain tx —> high concentration of prostaglandins in the nidus.(w/ NSAIDS)
nidus in osteoid osteoma
Osteoid osteoma — treat with surgery
why is this no longer the standard of tx?
long recovery time // VERY evasive
&
for successful surgery the tumor must be completely removed.
surgeries are quite extensive, require resection of large areas of bone and implantation of bone grafts.
higher risk of complications and a longer recovery period.
entails a longer hospital stay of at least several days.
Osteoid osteomas are frequently located in weight-bearing bones
—> crutches for several weeks.
what is now the standard tx for osteoid osteoma?
radio frequency ablation.(RFA)
tumor is heated up for a period of approximately 6 minutes and thus ablated.
(a minimally invasive approach) is done on an outpatient basis and has a short recovery time.
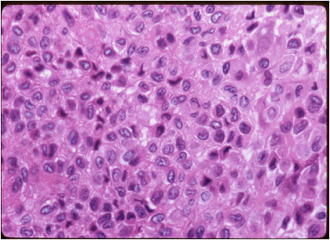
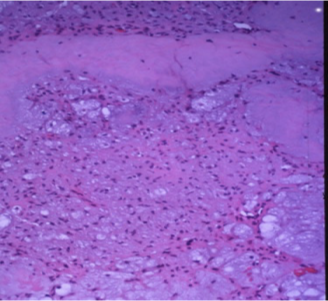
h most commonly affect people in their 20s and 30s
occur in the epiphyses and may erode the rest of the bone and extend into the soft tissues.
notorious for their tendency to recur.
Rarely,]may metastasize, even though it remains histologically benign.
appears lytic on x-ray.
symptoms: visible mass, swelling, bone fx
Radiologic findings demonstrate the lesion is most often eccentrically placed to the long axis of the bone.
The center is most radiolucent with increasing density towards the periphery.
There is a well-defined defect in the metaphysis and epiphysis, with destruction of the medullary cavity and adjacent cortex.
The destruction may stop just short of the joint.
Intact borders and a sharp inner margin may be associated with a better prognosis.
These tumors often thin the cortex and may expand into the soft tissues surrounding the bone, or they may expand the bone extensively, remaining within an eggshell-thin rim of periosteal new bone.
Treatment is curettage and packing. Excision rarely needed
Benign giant cell tumor

what are some symptoms of Benign giant cell tumors?
pain at the adjacent joint
a visible mass
swelling
bone fracture
limited movement in the adjacent joint
fluid accumulation in the joint adjacent to the affected bone
Example of being functionally malignant but histologically benign
Benign giant cell tumor
a solitary, benign and self-limited tumor that produces osteoid and bone.
The tumor occurs in the dorsal aspect of vertebrae, the metaphysis or diaphysis of long bones, and rarely in the pelvis.
In the spine, the tumor is usually located in the posterior processes while the vertebral bodies are spared.
On x-ray, appear as a radio-lucent defect with a central density due to ossification.
The lesion is well circumscribed and may have a surrounding sclerosis.
The tumor demonstrates increased isotope uptake on bone scan.
A biopsy is usually performed to confirm the diagnosis
Osteoblastoma
Osteoblastoma Treatment??
Surgical resection by curettage,
intralesional excision or en-bloc excision are all treatment options depending on the site.
Cryosurgery, radiation and chemotherapy may have a role in aggressive and surgically unresectable lesions of the spine.
********AGAIN, Histologically Benign But Functionally Malignant
benign cartilage tumors that are commonly found in the tubular bones of the hand and the foot.
They tend to be diaphyseal or metaphyseal lesions and probably arise from residual nests of cartilage cells left behind by the growing physis
Chondrocytes of enchondromas grow slowly, expanding the cortical bone and thinning the cortex.
They may cause an unsightly swelling or pathologic fracture of the bone.
symptoms: hand pain IF tumor is large or enlargment of finger — however, usually asymptophatic
tx: surgery or bone graft
Enchondroma
often have no symptoms at all.
hand pain that may occur if the tumor is very large
if the affected bone has weakened causing a hand fracture
enlargement of the affected finger
slow bone growth in the affected area
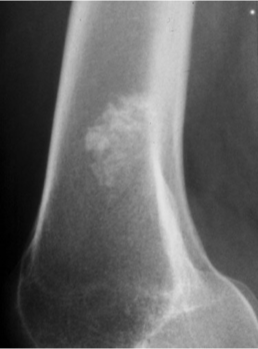
enchondroma

The lesion demonstrates the calcification typical of enchondromas that occur outside of the hand.
Radiopaque!!!
—> Enchondroma
Enchondroma Treatment??
surgery (in some cases, when bone weakening is present, or fractures occur
bone grafting - a surgical procedure in which healthy bone is transplanted from another part of the patient's body into the affected area.
bone pathology
list Benign Imitators
Bone cysts
Gout
Brown Tumors of hyperparathyroidism
Primary — parathyroid adenoma
Secondary — chronic renal disease
Osteomyelitis —> Brodie’s Abscess – hematogenous spread
list Benign Imitators of Malignant Disease
Enchondromas
Osteoid Osteoma: Proximal femur, Relieved with NSAIDs
Myositis Ossificans: Post traumatic
Enchondroma

Osteoid Osteoma
Treat with NSAIDS

Osteomyelitis (Brodie’s Abscess)

Brown Tumors of hyperparathyroidism
Primary — parathyroid adenoma
Secondary — chronic renal disease
