8. TRANSPORT IN MAMMALS
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
129 Terms
What is the mammalian circulatory system, and how does it function?
Type: Closed Double Circulatory System.
Components: Heart, blood, and blood vessels (arteries, arterioles, capillaries, venules, and veins).
Unique Feature: Blood passes through the heart twice in one complete circuit of the body.
Pulmonary Circulation:
Right side of the heart pumps deoxygenated blood to the lungs for gas exchange.
Systemic Circulation:
Oxygenated blood returns to the left side of the heart and is pumped at high pressure around the body.
The Need for a Circulatory System
All cells require oxygen and glucose for metabolism.
Single-Celled Organisms:
Obtain oxygen and glucose directly from surroundings via diffusion.
Short diffusion distances make this efficient.
Multicellular Organisms:
Have many layers of cells, making diffusion inefficient due to greater distances.
Solution: Exchange surfaces connected to a mass transport system (e.g., digestive and respiratory systems connected to the circulatory system).
Mass Transport:
Bulk movement of gases or liquids in one direction via vessels and tubes.
Example: Mammalian circulatory system ensures one-way blood flow for efficient nutrient and gas transport.
Open vs. Closed Circulatory Systems
Closed Circulatory System:
Blood is always contained within blood vessels.
Found in vertebrates and many invertebrates.
Open Circulatory System:
Blood is pumped directly into body cavities.
Common in arthropods and molluscs.
Humans have a closed circulatory system, enabling efficient transport of nutrients and gases.
Structures and Their Functions
HEART
ARTERIES
ARTERIOLES
CAPILLARIES
VENULES
VEINS
Heart:
Muscular organ in the chest cavity specialized for involuntary contractions without rest.
Pumps blood throughout the body.
Arteries:
Carry blood away from the heart.
Thick walls with muscle and elastic tissue maintain high pressure.
Diameter: 0.4 - 2.5 cm.
Arterioles:
Smaller arteries connecting larger arteries to capillaries.
Diameter: 30μm.
Capillaries:
Tiny blood vessels (diameter: 5-10μm) for gas and nutrient exchange.
Proximity to cells and tissues enables efficient exchange.
Venules:
Small veins linking capillaries to larger veins.
Diameter: 7μm - 1mm.
Veins:
Carry blood back to the heart.
Thin walls, wide lumen, valves to prevent backflow.
EXAM TIP
Aerobic respiration requires oxygen to release energy from glucose, but other substances also need transportation (e.g., nutrients).
Study circulatory diagrams carefully:
Understand single vs. double circulatory systems.
Distinguish pulmonary and systemic circulation.
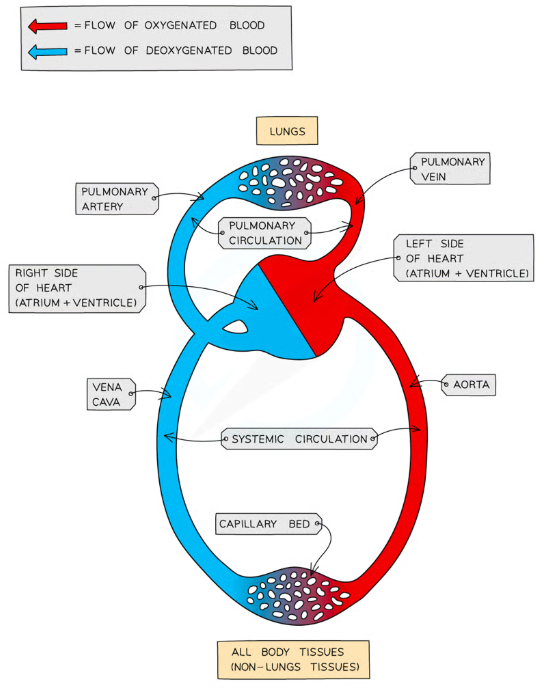
What is the function of the pulmonary artery?
The pulmonary artery carries deoxygenated blood from the right ventricle of the heart to the lungs for gas exchange. It is the only artery in the body that carries deoxygenated blood.
What does the pulmonary vein do?
The pulmonary vein carries oxygenated blood from the lungs to the left atrium of the heart, enabling the heart to pump oxygen-rich blood to the systemic circulation. It is the only vein in the body that carries oxygenated blood.
What is the role of the aorta in the circulatory system?
The aorta is the largest artery in the body. It carries oxygenated blood from the left ventricle of the heart to the rest of the body, supplying oxygen and nutrients to all organs and tissues.
What is the function of the vena cava?
The vena cava carries deoxygenated blood from the body to the right atrium of the heart. The superior vena cava drains blood from the upper body, and the inferior vena cava drains blood from the lower body.
What is the difference between pulmonary and systemic circulation?
Pulmonary Circulation: Transports deoxygenated blood from the heart to the lungs for oxygenation.
Systemic Circulation: Transports oxygenated blood from the heart to the rest of the body, delivering oxygen to tissues and collecting carbon dioxide.
How is oxygen transported and diffused in the circulatory system?
Oxygen transport relies on concentration gradients:
Oxygen diffuses from the alveoli in the lungs to the blood.
Oxygen diffuses from the blood into cells and mitochondria for respiration, while carbon dioxide diffuses in the opposite direction.
Why are capillaries important in the circulatory system?
Capillaries are small blood vessels that connect arterioles and venules. Their thin walls and proximity to cells allow for efficient exchange of gases, nutrients, and waste products.
What key difference exists between arteries and veins?
Arteries: Carry blood away from the heart, have thick walls, and transport blood at high pressure.
Veins: Carry blood towards the heart, have thinner walls, a wider lumen, and valves to prevent backflow.
Why is the circulatory system considered a mass transport system?
It involves the bulk movement of blood carrying essential substances (e.g., oxygen, glucose) in one direction, ensuring all cells receive the nutrients they need for metabolism.
What is an important observation about the surface area of large blood vessels compared to capillaries?
Large blood vessels transport blood quickly but have a smaller overall surface area compared to capillaries. Capillaries have a much larger surface area, enabling efficient exchange of substances.
Why are capillaries essential in the circulatory system?
Capillaries provide a large surface area, which is crucial for the efficient exchange of gases, nutrients, and waste products between blood and tissues.
What should you use during exams to differentiate between pulmonary and systemic circulation?
Use diagrams to distinguish between pulmonary and systemic circulation, as they clearly show the movement of deoxygenated and oxygenated blood.
What are the key differences between arteries and veins?
Arteries carry blood away from the heart.
Veins carry blood towards the heart.
How do arteries, veins, and capillaries differ in their structure and function?
Arteries: Thick walls with elastic and muscular tissue to withstand high pressure and maintain blood flow away from the heart.
Veins: Thin walls with a large lumen to accommodate low-pressure blood flow towards the heart; valves prevent backflow.
Capillaries: One-cell thick endothelial walls for efficient exchange of materials between blood and tissues.
What is the role of elastic and muscular tissue in arteries?
Elastic tissue allows arteries closer to the heart to stretch and recoil, accommodating blood surges during ventricular contractions.
Muscular tissue in arteries further from the heart adjusts their diameter, regulating blood flow to different tissues.
What are capillary beds, and why are they important?
Capillary beds are networks of capillaries throughout tissues.
They bring blood close to cells for efficient exchange of oxygen, nutrients, and waste products.
How does the structure of capillary walls enable efficient material exchange?
Capillary walls are one-cell thick, reducing diffusion distance.
They have leaky walls with small gaps between squamous epithelial cells, allowing small substances to move into surrounding tissue fluid.
What structural adaptations do veins have for their function?
Outer layer: Tough collagen fibers provide structural support.
Middle layer: Thin, with small amounts of smooth muscle and elastic fibers, due to low blood pressure.
Valves: One-way valves prevent backflow.
Lumen: Large lumen reduces resistance and aids low-pressure blood flow.
What examiner tips should you remember when observing blood vessels under a microscope?
Recognize arteries, veins, and capillaries based on their distinct structural features.
Use magnification and resolution effectively to analyze micrographs.
Draw accurate plan diagrams, noting wall thickness and lumen size.
Identify arteries by their thick walls and small lumen, veins by their thin walls and large lumen, and capillaries by their one-cell-thick walls.
What is the structure of muscular arteries, and how does it relate to their function?
Structure:
Thicker tunica media composed mainly of smooth muscle.
Narrow lumen.
Contains less elastin compared to elastic arteries.
Function:
Smooth muscle allows vasoconstriction and vasodilation to regulate blood flow to tissues.
Narrow lumen maintains high pressure for efficient blood delivery.
Limited elasticity prevents stretching and recoil, ensuring consistent pressure.
How does the structure of elastic arteries support their function?
Structure:
Tunica media thinner than muscular arteries but composed of elastin and collagen.
Relatively few smooth muscle fibers.
Narrow lumen.
Function:
Elastin provides stretch and recoil in response to pulses from the heart, preventing bursting and maintaining blood pressure.
Limited smooth muscle means elastic arteries cannot perform vasoconstriction or vasodilation.
What structural features of veins are adapted to their function?
Structure:
One-way valves prevent backflow.
Wide lumen accommodates low-pressure blood flow.
Less smooth muscle and elastin than arteries.
Outer layer rich in collagen for strength and structure.
Function:
Valves ensure blood flows consistently towards the heart despite low pressure.
Collagen provides durability, while the large lumen reduces resistance to blood flow.
How does the structure of capillaries enable their function?
Structure:
Very small diameter (5–10 μm).
Thin walls composed of a single layer of squamous epithelial cells.
No elastic, smooth muscle, or collagen.
Branch extensively between cells.
Function:
Thin walls reduce diffusion distance, enabling efficient exchange of oxygen, nutrients, and waste.
Small gaps between epithelial cells allow substances to leak into surrounding tissue fluid.
Slow blood flow enhances diffusion opportunities.
How do magnification and resolution influence the observation of blood vessels?
Magnification increases the size of the image relative to the actual object (e.g., X10, X100).
Resolution determines how close two objects can be before they appear as one.
Light microscope resolution: ~0.2 μm.
Electron microscope resolution: ~0.1–1 nm.
These features allow detailed study of blood vessel structures.
What is the key difference between elastic arteries and muscular arteries regarding vasoconstriction and vasodilation?
Elastic arteries cannot perform vasoconstriction or vasodilation due to a low proportion of smooth muscle.
Muscular arteries, with their thicker tunica media of smooth muscle, can perform vasoconstriction and vasodilation to regulate blood flow.
What examiner tip should you remember for “Explain” questions in this topic?
Pair a description of a structural feature with an explanation of how it supports the blood vessel's function. For example:
Capillaries: “Capillaries are one-cell thick, which enables quick and efficient diffusion of substances.”
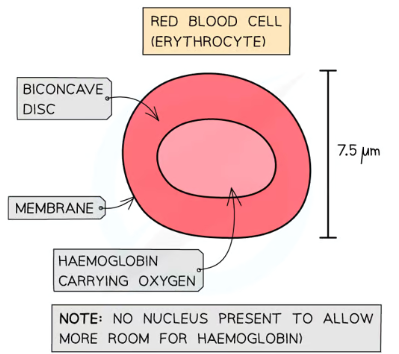
What are red blood cells (erythrocytes), and how can they be identified?
Structure:
Distinctive biconcave disc shape caused by the absence of a nucleus.
Contains haemoglobin, a protein with haem iron groups that bind reversibly to oxygen.
Function:
Transports oxygen to tissues and removes carbon dioxide.
Quantity:
Approximately 5 million per mm³ of blood.
Microscope Identification:
Easily recognizable due to their biconcave shape under light microscopes and photomicrographs.
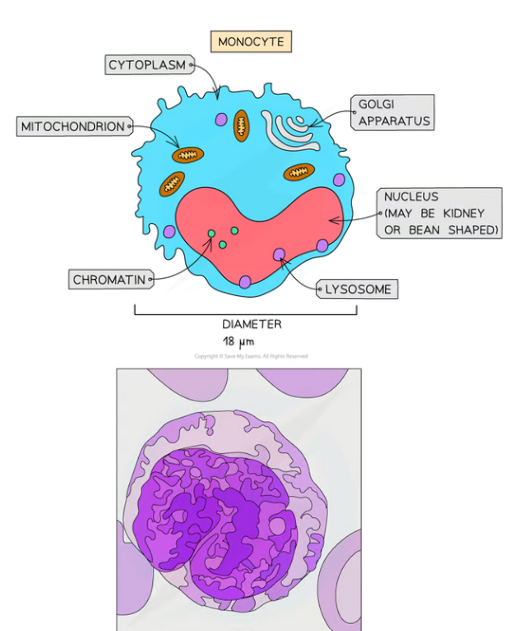
How can monocytes be identified under the microscope?
Structure:
Monocytes are the largest leukocytes (white blood cells).
Kidney-shaped or bean-shaped nucleus, which appears lighter after staining.
Function:
Engages in phagocytosis, engulfing pathogens and debris.
Microscope Identification:
Stained nucleus appears light blue, with distinct chromatin.
Easy to identify due to size and shape.
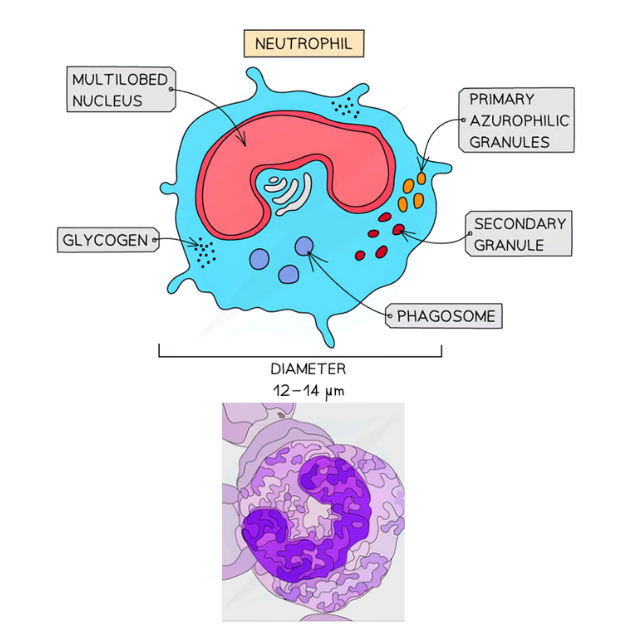
What are the distinguishing features of neutrophils?
Structure:
Neutrophils have a multi-lobed nucleus.
Cytoplasmic granules stain pink or purple-blue.
Function:
First responders to bacterial infection through phagocytosis.
Microscope Identification:
Up to 70% of all leukocytes are neutrophils, making them easy to spot.
Recognizable due to granules and nucleus shape.
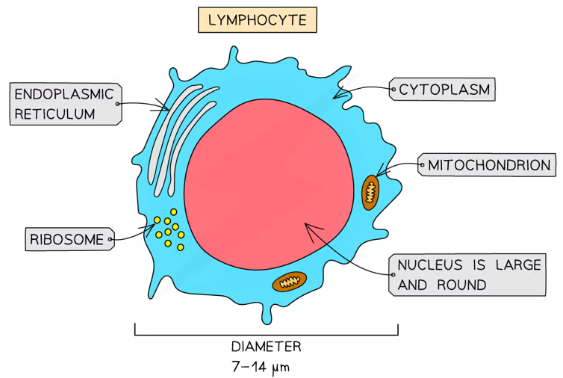
How can lymphocytes be recognised in microscope slides and micrographs?
Structure:
Small leukocytes with a very large, dark-staining nucleus.
Similar in size to red blood cells.
Function:
Involved in immune response by producing antibodies and destroying infected cells.
Microscope Identification:
Constitute 20–25% of all leukocytes, identified by their dark-staining nucleus.
What is the key tip for distinguishing monocytes from neutrophils under a microscope?
Monocytes: Kidney-shaped nucleus, lighter in appearance after staining.
Neutrophils: Multi-lobed nucleus and granules that stain pink or purple-blue.
Practice identifying these features in micrographs to avoid confusion.
What is the main component of blood and tissue fluid?
Water is the main component of blood and tissue fluid. It constitutes 95% of plasma, the straw-colored liquid in blood, and forms most of tissue fluid, which leaks from capillaries into spaces between cells.
Why is water’s solvent action ideal for transport in mammals?
Water acts as an excellent solvent, dissolving substances for transport.
Examples:
Glucose is transported in solution from the small intestine to body cells for respiration.
Urea is transported in solution from the liver to the kidneys for excretion.
What is specific heat capacity, and what is the specific heat capacity of water?
Specific heat capacity is the amount of energy required to raise the temperature of 1 kg of a substance by 1°C.
Water has a high specific heat capacity of 4200 J/kg°C, meaning it requires a large amount of energy to change its temperature.
How does water’s high specific heat capacity benefit mammals?
Water can absorb heat without causing significant temperature changes.
This helps in maintaining optimal temperatures for enzyme activity.
Water in blood plasma and tissue fluid regulates body temperature by transferring heat efficiently.
How does water in blood plasma help regulate body temperature?
As blood passes through warmer regions of the body, water in plasma absorbs heat energy but maintains a fairly constant temperature.
This allows heat to be distributed throughout the body without large fluctuations.
What is the difference between blood plasma and tissue fluid in composition?
Both are mainly composed of water.
However, blood plasma contains proteins, such as albumin, which are too large to pass through capillary walls, while tissue fluid does not.
Why is water crucial for enzymes in the body?
Water’s ability to maintain stable temperatures ensures optimal conditions for enzyme activity, preventing denaturation or decreased functionality.
How do water’s properties support its role in transport in mammals?
Solvent action: Water dissolves and transports nutrients, waste products, and gases.
High specific heat capacity: Water stabilizes body temperature and helps evenly distribute heat.
What examiner tip is useful for this topic?
In exam answers, always connect water’s properties (e.g., solvent action, high specific heat capacity) to how they support transport or regulate body temperature in mammals.
What is tissue fluid, and how is it formed?
Tissue fluid is a liquid that bathes almost all body cells outside of the circulatory system.
Tissue fluid is formed when plasma passes through capillaries and some plasma leaks out from capillaries through gaps in their walls, surrounding body cells, into the spaces between cells in the capillary walls. Its main component is water.
What is the composition of tissue fluid compared to blood plasma?
Both are mainly composed of water, dissolved ions, and small molecules.
However, tissue fluid does not contain large proteins as they are too large to pass through capillary walls.
What is the primary function of tissue fluid?
Tissue fluid facilitates the exchange of substances between cells and the blood.
For example:
Oxygen and nutrients diffuse from the tissue fluid into cells.
Carbon dioxide and waste products diffuse from cells into the tissue fluid and then into capillaries.
How does hydrostatic pressure contribute to the formation of tissue fluid?
Hydrostatic pressure is the blood pressure exerted on the walls of capillaries.
At the arterial end of the capillary, hydrostatic pressure is high, forcing plasma out through the capillary walls into the surrounding tissue, forming tissue fluid.
What role does the solute concentration gradient play in tissue fluid formation?
Proteins in the blood lower its water potential, creating a gradient between the capillaries and surrounding tissue.
Water moves back into the capillaries by osmosis, especially at the venous end, where hydrostatic pressure is lower.
What happens at the arterial and venous ends of the capillary in terms of tissue fluid dynamics?
Arterial End:
Hydrostatic pressure > Osmotic pull.
Plasma is forced out, forming tissue fluid.
Venous End:
Hydrostatic pressure decreases.
Osmotic pull draws water back into capillaries from tissue fluid.
How can factors like high blood pressure affect tissue fluid formation?
High blood pressure:
Increases hydrostatic pressure, forcing more fluid out of capillaries.
May lead to excess tissue fluid (edema).
Low blood protein content:
Reduces osmotic pull back into capillaries, causing fluid buildup in tissues.
How does tissue fluid facilitate the removal of carbon dioxide?
Carbon dioxide from aerobic respiration diffuses out of cells into the tissue fluid.
It then diffuses into capillaries and is transported away for excretion.
What role does tissue fluid play in the transport of nutrients?
Nutrients like glucose diffuse from capillaries into tissue fluid and then into cells.
This ensures cells have a continuous supply of substances needed for metabolism.
What examiner tips are essential for this topic?
When explaining tissue fluid formation, clearly state the role of hydrostatic pressure and osmotic gradients at the arterial and venous ends.
Compare the composition of tissue fluid and plasma, emphasizing the absence of large proteins in tissue fluid.
What is the primary role of red blood cells (erythrocytes) in the body?
Red blood cells transport oxygen from the lungs to tissues and carbon dioxide from tissues to the lungs.
They contain haemoglobin, a protein essential for oxygen and carbon dioxide transport.
How does haemoglobin transport oxygen?
Each haemoglobin molecule has four haem groups, each capable of binding one oxygen molecule.
When oxygen binds to haemoglobin, oxyhaemoglobin is formed:
Oxygen + Haemoglobin ⇌ Oxyhaemoglobin
4O₂ + Hb ⇌ Hb4O₂
Cooperative binding: The binding of the first oxygen molecule causes a conformational change, making it easier for subsequent oxygen molecules to bind.
What happens to haemoglobin when oxygen is released in tissues?
In tissues, oxygen dissociates from haemoglobin due to lower oxygen concentration, forming deoxygenated haemoglobin.
This process ensures oxygen delivery to cells for respiration.
How is carbon dioxide transported in red blood cells?
Carbon dioxide is transported in three main ways:
Dissolved in plasma (small percentage).
Bound to haemoglobin, forming carbaminohaemoglobin.
As hydrogen carbonate ions (HCO₃⁻), formed through a reaction catalyzed by carbonic anhydrase.
What is the role of carbonic anhydrase in carbon dioxide transport?
Carbonic anhydrase is an enzyme in red blood cells that catalyzes the reaction:
CO₂ + H₂O ⇌ H₂CO₃ (carbonic acid)
Carbonic acid dissociates into H⁺ and HCO₃⁻ (hydrogen carbonate ions), which are transported in plasma.
What is haemoglobinic acid, and how is it formed?
Haemoglobinic acid is formed when H⁺ ions (from carbonic acid dissociation) bind to haemoglobin.
This prevents a drop in pH, as haemoglobin acts as a buffer to maintain blood pH.
What is carbaminohaemoglobin, and how is it formed?
Carbaminohaemoglobin is formed when carbon dioxide binds directly to haemoglobin.
This occurs at tissues where carbon dioxide concentration is high, facilitating its transport to the lungs.
How does haemoglobin act as a buffer in red blood cells?
Haemoglobin binds to H⁺ ions, forming haemoglobinic acid.
This prevents the accumulation of H⁺ ions, which could lower blood pH and disrupt enzyme activity.
What is the significance of cooperative binding in oxygen transport?
Cooperative binding ensures efficient oxygen loading in the lungs and unloading in tissues.
The binding of one oxygen molecule increases haemoglobin’s affinity for more oxygen, while dissociation decreases it.
What examiner tips are useful for this topic?
Clearly explain the roles of haemoglobin, carbonic anhydrase, haemoglobinic acid, and carbaminohaemoglobin in oxygen and carbon dioxide transport.
Use equations to illustrate key processes (e.g., oxygen binding, carbon dioxide conversion).
Remember that haemoglobin acts as a buffer to maintain blood pH.
What is the chloride shift?
The chloride shift is the movement of chloride ions (Cl⁻) into red blood cells (RBCs) to maintain electrical neutrality when hydrogen carbonate ions (HCO₃⁻) are transported out of the RBCs.
How are hydrogen carbonate ions (HCO₃⁻) formed in red blood cells?
Carbon dioxide (CO₂) diffuses into red blood cells from tissues.
The enzyme carbonic anhydrase catalyzes the reaction of CO₂ and water (H₂O) to form carbonic acid (H₂CO₃):
CO₂ + H₂O ⇌ H₂CO₃
Carbonic acid dissociates into H⁺ ions and HCO₃⁻ ions:
H₂CO₃ ⇌ HCO₃⁻ + H⁺
Why do chloride ions (Cl⁻) enter red blood cells?
As negatively charged HCO₃⁻ ions leave the red blood cells via a membrane transport protein, this could result in an electrical imbalance.
To prevent this, Cl⁻ ions move into the RBCs through the same transport protein, maintaining electrical neutrality.
What would happen if chloride ions did not enter red blood cells during the chloride shift?
Without the influx of Cl⁻ ions, the red blood cells would become positively charged due to the buildup of H⁺ ions from carbonic acid dissociation.
This would disrupt normal cellular function.
How does the chloride shift help in carbon dioxide transport?
The chloride shift allows red blood cells to efficiently transport CO₂ as HCO₃⁻ ions in the plasma.
By preventing electrical imbalances, the chloride shift ensures continuous CO₂ uptake and conversion in RBCs.
What is the role of carbonic anhydrase in the chloride shift?
Carbonic anhydrase catalyzes the formation of carbonic acid (H₂CO₃) from CO₂ and H₂O.
This is the key step for generating H⁺ ions and HCO₃⁻ ions, facilitating the chloride shift.
Why is the chloride shift important for maintaining blood pH?
The formation of HCO₃⁻ ions removes CO₂ from the blood, preventing acid buildup.
H⁺ ions bind to haemoglobin (forming haemoglobinic acid), further buffering the blood and maintaining a stable pH.
How does the chloride shift differ from the Bohr shift?
The chloride shift involves the exchange of ions (Cl⁻ and HCO₃⁻) in red blood cells to maintain electrical neutrality during CO₂ transport.
The Bohr shift describes how a high partial pressure of CO₂ lowers haemoglobin's affinity for oxygen, enhancing oxygen release to tissues.
How does the chloride shift support oxygen delivery to tissues?
By facilitating CO₂ transport out of tissues, the chloride shift helps maintain the partial pressure gradient needed for efficient oxygen delivery by haemoglobin.
What examiner tips are useful for understanding the chloride shift?
Clearly differentiate between the chloride shift and Bohr shift in exam answers.
Use equations (e.g., CO₂ + H₂O ⇌ H₂CO₃ ⇌ HCO₃⁻ + H⁺) to support your explanation.
Highlight the importance of ion movement for electrical neutrality and CO₂ transport.
How is waste carbon dioxide produced and where does it go?
Waste carbon dioxide is produced during respiration in body tissues.
It diffuses from the tissues into the blood and is transported around the body in different forms.
In what forms is carbon dioxide transported in the blood, and what are the proportions?
Hydrogen carbonate ions (HCO₃⁻): ~85% of CO₂ is transported in this form.
Dissolved in plasma: ~5% of CO₂ is directly dissolved in blood plasma.
Carbaminohaemoglobin: ~10% of CO₂ binds to haemoglobin.
What process occurs to carbon dioxide in red blood cells?
Carbon dioxide diffuses into the cytoplasm of red blood cells.
It combines with water to form carbonic acid (H₂CO₃) in a reaction catalyzed by the enzyme carbonic anhydrase:
CO₂ + H₂O ⇌ H₂CO₃
Carbonic acid dissociates into H⁺ ions and HCO₃⁻ ions:
H₂CO₃ ⇌ HCO₃⁻ + H⁺
How is the majority of carbon dioxide transported in blood plasma?
Most carbon dioxide is transported as hydrogen carbonate ions (HCO₃⁻).
These ions are formed in red blood cells and then diffuse out into the plasma, where they are carried to the lungs.
Why does the reaction between CO₂ and water occur faster in red blood cells than in plasma?
Red blood cells contain the enzyme carbonic anhydrase, which catalyzes the reaction.
Plasma contains very little carbonic anhydrase, so carbonic acid forms more slowly in plasma than in red blood cells.
What happens to hydrogen ions (H⁺) produced in red blood cells?
H⁺ ions combine with haemoglobin to form haemoglobinic acid, preventing a drop in pH.
Haemoglobin acts as a buffer, maintaining the red blood cell's pH stability.
What is the role of haemoglobin in carbon dioxide transport?
Haemoglobin binds some carbon dioxide, forming carbaminohaemoglobin (~10% of CO₂ transport).
It also binds to H⁺ ions (from carbonic acid dissociation), forming haemoglobinic acid and buffering the blood's pH.
What happens to hydrogen carbonate ions (HCO₃⁻) formed in red blood cells?
HCO₃⁻ ions diffuse out of red blood cells into the plasma, where they are transported in solution.
This accounts for the majority (~85%) of carbon dioxide transport in the blood.
Why is the transport of carbon dioxide in plasma important for gas exchange?
Carbon dioxide in plasma is carried to the lungs, where it diffuses into alveoli and is exhaled.
The efficient removal of CO₂ ensures a concentration gradient for continuous gas exchange.
What examiner tips should you remember for this topic?
Clearly describe the steps of carbon dioxide transport, emphasizing the role of carbonic anhydrase and HCO₃⁻ formation.
Highlight the proportions of CO₂ transport: 85% as HCO₃⁻, 5% dissolved, 10% as carbaminohaemoglobin.
Use equations to explain key processes (e.g., CO₂ + H₂O ⇌ H₂CO₃ ⇌ HCO₃⁻ + H⁺).
What does the oxygen dissociation curve represent?
The curve shows the rate at which oxygen associates and dissociates with haemoglobin at different partial pressures of oxygen (pO₂).
What is partial pressure of oxygen (pO₂)?
It is the pressure exerted by oxygen within a mixture of gases, serving as a measure of oxygen concentration.
When is haemoglobin considered saturated?
Haemoglobin is saturated when all four oxygen-binding sites are occupied by oxygen molecules.
This occurs at high pO₂, typically in the lungs.
What does haemoglobin's affinity for oxygen mean?
Affinity refers to how easily haemoglobin binds to oxygen and how slowly it dissociates.
High affinity: Oxygen binds easily and dissociates slowly (e.g., at high pO₂).
Low affinity: Oxygen binds slowly and dissociates easily (e.g., at low pO₂).
Why does haemoglobin's affinity for oxygen vary?
Haemoglobin's affinity changes with partial pressure of oxygen (pO₂). This ensures oxygen binds efficiently in the lungs (high pO₂) and dissociates efficiently in tissues (low pO₂).
What is the shape of the oxygen dissociation curve for haemoglobin?
The curve is sigmoidal (S-shaped) due to cooperative binding and the varying affinity of haemoglobin for oxygen at different pO₂ levels.
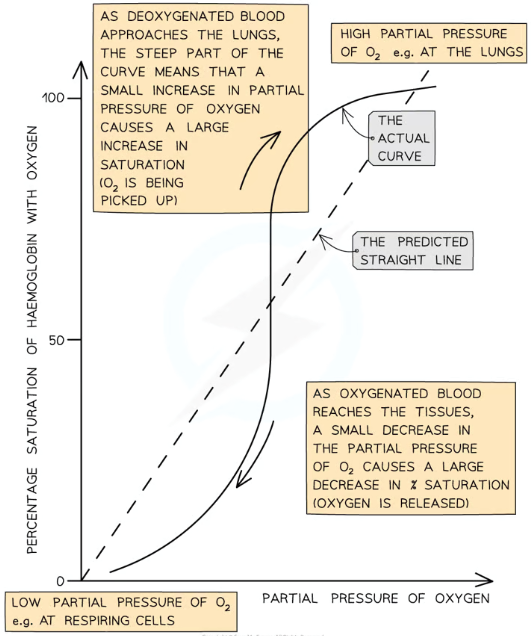
What happens at low pO₂ on the curve?
Haemoglobin binds oxygen slowly.
Saturation percentage is low, as occurs in oxygen-depleted tissues.
What occurs at medium pO₂ on the curve?
Haemoglobin binds oxygen more readily.
Saturation percentage increases rapidly, as shown by the steep region of the curve.
A small increase in pO₂ causes a large rise in haemoglobin saturation.
What happens at high pO₂ on the curve?
Haemoglobin binds oxygen quickly and easily, becoming fully saturated.
Increasing pO₂ further has little effect on saturation, as most binding sites are occupied.
Why does oxygen dissociation occur in tissues?
In tissues (medium pO₂), oxygen dissociates readily from haemoglobin to support cellular respiration.
A small decrease in pO₂ causes a large drop in haemoglobin saturation, releasing oxygen.
What explains the sigmoidal shape of the curve?
Cooperative binding:
The first oxygen binds slowly, explaining the shallow curve at low pO₂.
The binding causes a conformational change, making it easier for the next oxygen molecules to bind, leading to the steep part of the curve.
Saturation levels off at high pO₂ as fewer binding sites remain available.
What examiner tips are helpful for this topic?
Clearly describe haemoglobin's affinity changes at different pO₂ levels.
Use graphs to interpret binding and dissociation rates.
Explain cooperative binding to justify the curve's shape.
What happens at high partial pressures of oxygen (pO₂) in the lungs?
At high pO₂ (e.g., in the lungs), oxygen binds easily to haemoglobin.
Haemoglobin has a high affinity for oxygen, resulting in near 100% saturation.
Most haemoglobin oxygen-binding sites are occupied, so increasing pO₂ further has little additional effect.
Why is the high affinity of haemoglobin for oxygen in the lungs important?
It ensures haemoglobin becomes fully saturated with oxygen while passing through the lungs.
This allows maximum oxygen transport to tissues for cellular respiration.
What happens at low partial pressures of oxygen (pO₂) in respiring tissues?
At low pO₂ (e.g., in oxygen-depleted tissues), haemoglobin has a low affinity for oxygen.
Oxygen readily dissociates from haemoglobin, allowing its release to cells.