Respiratory System Week 5
1/54
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
55 Terms
pNeumonia
Acute inflammation of the lung parenchyma caused by a microbial agent
• Associated with high morbidity and mortality rates (Especially in the young and elderly)
• Can be caused by bacteria, viruses, fungi, parasites, or chemicals
Community acquired pneumonia (CAP)
Onset in the community or during the first two days of hospitalization
Hospital acquired pneumonia (HAP)
Onset 48hours or more after hospitalization
Aspiration pneumonia:
caused by abnormal entry of secretions or substances into the lower airway
Material from mouth or stomach aspirated into lung
*Importance of Oral hygiene
What lobe is affected more with aspiration pneumonia and why?
the right lower lobe is most commonly affected. This is due to anatomical and gravitational factors.
Here's why:
1. Anatomy of the Bronchial Tree
The right main bronchus is:
Shorter
Wider
More vertical than the left
This makes it easier for aspirated material (like food, saliva, or gastric contents) to enter the right lung, particularly the lower lobe.
2. Gravitational Effect
In supine (lying down) patients, aspiration material tends to settle in the posterior segment of the right upper lobe or the superior segment of the right lower lobe.
In upright or semi-upright individuals, the right lower lobe (especially the posterior basal segment) is more commonly involved.
Risk with Aspiration Pneumonia
loss of consciousness, tube feeding, dysphagia
Opportunistic Pneumonia:
patients with altered immune response are highly susceptible to respiratory infections
the infection happens when the body’s normal defenses are weakened—the germs take advantage of the opportunity to infect the lungs.
Risk factors with Opportunistic Pneumonia
malnutrition, immunodeficiencies, transplant patients, patients receiving radiation or chemotherapy
4 Stages of Pneumonia pathophysiology
Congestion, red hepatization, grey hepatization, resolution
Congestion
- Outpouring of fluid to alveoli
- Organisms multiply
- Infection spreads
Red hepatization
- Massive dilation of capillaries
-Alveoli fill with organisms, neutrophils, RBCs, and fibrin.
Grey hepatization
- ↓ Blood flow
- Leukocyte and fibrin consolidate in affected part of lung.
Resolution
- Resolution and healing if no complications
- Exudate lysed and processed by macrophages
- Tissue restored
Clinical Manifestations Community Acquired
Pneumonia
Weakness, Fatigue, Malaise
Sore throat, headache, abdominal pain, muscle aches, nasal congestion
Sudden onset of fever/chills
Pleuritic chest pain
Dyspnea
Cough (productive or nonproductive)
Viral pneumonia manifestation is highly variable – often associated with systemic viral disease (measles, influenza)
Pneumonia Prevention
• Elevate head of bed 30–45 degrees for clients with feeding tube.
• Assist clients at risk for aspiration with eating, drinking, and taking medications.
• Frequent mouth care
• Assist immobile clients with turning and deep breathing.
• Checking gag reflex after local anesthesia to the throat
• Smoking cessation
• Hand hygiene
• Vaccinations
- Influenza, COVID
- Pneumococcal for high-risk patients
Nursing Assessment Findings for pneumonia
•Splinting affected area
•Tachypnea
•Asymmetric chest movements
•Use of accessory muscles
•Crackles, friction rub
•Dullness to percussion
•↑ Fremitus
•Bronchial breath sounds
•Pink, rusty, purulent, green, yellow, or white sputum
•Tachycardia
•Changes in mental status
Pneumonia Nursing Diagnoses
•Impaired gas exchange
•Ineffective breathing pattern
•Acute pain
•Activity intolerance
Patient goals with pneumonia
to have clear breath sounds, a normal breathing pattern, no hypoxemia, and to reduce the risk of complications
Clinical manifestations of Influenza
•Onset abrupt; systemic symptoms of cough, fever, myalgia, headache, sore throat
•In uncomplicated cases, symptoms subside within 7 days; older persons may experience persistent weakness or lassitude that persists for weeks.
•Most common complication: Pneumonia
Nursing and interprofessional management with Influenza
•Hand hygiene
•Vaccination
•Supportive measures
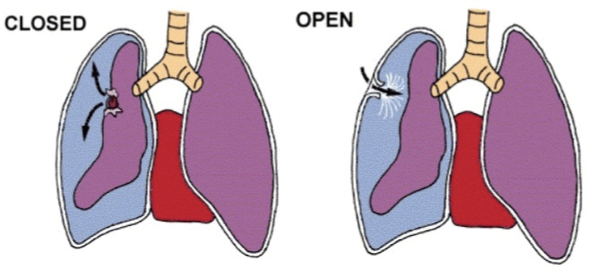
Pneumothorax(long definition )
The presence of air or gas in the cavity between the lungs and the chest wall, causing collapse of the lung.
Open: from trauma/injury
Closed: spontaneous
Note: BIG factor is the Degree of collapse and nature of collapse
Pneumothorax:
air in the pleural space
Hemothorax:
blood in the pleural space
Hemopneumothorax:
air and blood in the pleural space
Chylothorax:
lymphatic fluid in pleural space
a rare condition in which lymphatic fluid leaks into the space between the lung and chest wall. When this fluid builds up in the lungs, it can cause a severe cough, chest pain and difficulty breathing. _________ is a lymphatic flow disorder.
Pneumothorax Clinical Manifestations
Mild tachycardia
Dyspnea
“Air hunger”
Decreased O2 sats
Absent breath sounds over affected area
Hyper-resonance may be present
Pneumothorax Treatment
no treatment if mild.
•Small with little or no drainage à Heimlich valves, Pigtail drains
•Most common à chest tube (with suction)
•Repeated spontaneous à surgical interventions (pleurectomy, pleurodesis)
•In emergencies with open chest wounds à use vented dressing (to eliminate air entering chest yet allowing trapped air to escape)
Tension Pneumothorax
When air accumulates between the chest wall and the pleural space causing increased pressure in the chest - causes tension on the heart and great vessels reducing the amount of blood returned to the heart.
*MEDICAL EMERGENCY*
Risk factors for Tension pneumothorax
trauma, underlying lung disease and procedures such as central line placement or bronchoscopy, *clamped or blocked chest tube
Pressure increases à Lung collapses à Mediastinum shifts towards the unaffected side à Cardiac output altered from decreased venous return and pressure on the aorta
Tension Pneumothorax
Clinical Manifestation
Tachypnea/severe respiratory distress
Hypotension
Pleuritic chest pain
Tracheal deviation*
Jugular vein distention
Unilateral absence of breath sounds
Tension Pneumothorax Treatment
•Emergency decompression of chest cavity (needle insertion 2/3rd intercostal space midclavicular line)
•Insertion of chest tube once stabilized (lateral chest insertion)
Chest Tube Nursing Management
•Monitor Chest tube tubing and drainage system
•Monitor output (color, quantity)
•Monitor dressing (change as ordered)
•Monitor for air leaks and oscillation
•Respiratory assessment (including S/C emphysema)
•DB+ coughing exercises, shoulder ROM
•*Do not clamp (unless quickly changing drainage system or ordered by the provider)
What if there is no oscillation seen in chest tube
1. Lung Re-expanded (Normal Finding)
If the lung has fully re-expanded, there may be no more air or fluid draining, so oscillation stops.
Check with chest X-ray to confirm re-expansion.
⚠ 2. Obstructed or Kinked Chest Tube
Common causes:
Clots or fibrin in the tube
Kinks or loops in the tubing
Tube is pressed against chest wall or lung
➤ Check the tube from patient to drainage system for any visible blockage.
⚠ 3. Tube Dislodged from Pleural Space
If the tube has come out of the pleural cavity, it won’t drain or oscillate.
Look for signs like:
Sudden stop in drainage
Subcutaneous emphysema
Worsening respiratory status
⚠ 4. Suction May Be Too High (If Using Wall Suction)
Excessive suction can eliminate oscillation, especially if it’s not set properly.
Try temporarily disconnecting suction and see if oscillation returns.
⚠ 5. Malfunction of the Drainage System
Rare, but the chest drainage unit itself could be defective.
Try replacing the system if other causes are ruled out.
Oscillation
(or tidaling) is the movement of water in the water-seal chamber with the patient’s respiration:
Moves up with inspiration
Moves down with expiration (in spontaneously breathing patients)
Pulmonary Embolism
Blockage of pulmonary artery by a thrombus, fat, or air embolism
Most PEs arise from DVTs
What patients are at risk for PEs?
Virchow’s Triad: Venous stasis, vascular injury, hypercoagulability
Most Pulmonary Embolisms arise from
DVTs
PE Clinical Manifestation & Diagnostics
Classic triad: dyspnea, chest pain, and hemoptysis
Decreased SpO2
Cough
Pleuritic chest pain
Tachycardia
Anxiety
Diagnostic tests: D-Dimer, CT scan with contrast
PE Management
•Preventative treatment (SCDs, mobility post-op)
• Monitor vitals and assessments
• O2 (as needed)
• Anticoagulant therapy
Fibrinolytic drug (tPA, ateleplase in some cases)
Heparin drip (IV)
Low molecular wight heparin (Enoxaparin/Lovonox)
- Monitor for adverse effects (bleeding, bruising)
- Often on long-term therapy for 3-6months, maybe indefinitely
Pleural Effusion
collection of fluids in the pleural space.
can be transudate or exudate.
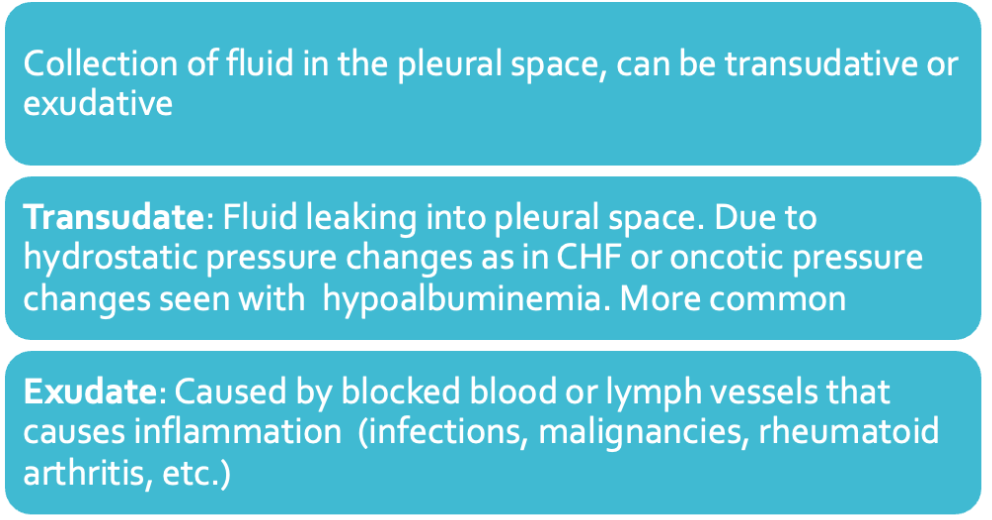
Types of fluid
Type of fluid can be determined with a thoracentesis
Pus: Empyema from infections
Blood: From trauma
Chyle: From rupture of thoracic duct.
Urine: Urinothorax in hydronephrosis.
Pleural Effusion Clinical Manifestation
•Progressive dyspnea
•Pleuritic chest pain
•Decreased breath sounds (or absent)
•Dullness on percussion
•Fever, cough (if empyema)
Pleural Effusion Treatment
•Minor =no treatment
• Thoracentesis
- *only 1- 1.2 L removed at a time to avoid hypotension, hypoxemia, or pulmonary edema
- Monitor for respiratory distress during procedure
- Chest x-ray post procedure
• Chest tube
• Treat underlying cause
Respiratory Syncytial Virus (RSV)
Viral infection of the lungs & respiratory tract
Enters the body through the eyes, nose or mouth
Spreads easily through the air on infected respiratory droplets- Easily spread through coughing/ sneezing
Virus also passes to others through direct contact, such as shaking hands
Virus can live for hours on hard objects such as countertops, crib rails and toys- Touch your mouth, nose or eyes after touching a contaminated object and you're likely infected
An infected person is most contagious during the first week after infection
In infants and those with weakened immunity, the virus may continue to spread even after symptoms go away, for up to four weeks
—— is so common that most children have been infected with the virus by age 2
Usually mimics the common cold and only symptomatic treatment needed
Can cause severe illness in those at risk: Infants 12 months and younger (especially premature)/ Elderly/ Comorbidities/ Immunocompromised
Signs & Symptoms: RSV
Fever
Severe cough
Wheezing
Tachypnea/ Dyspnea
Cyanosis
Patient may prefer to sit up rather than lie down
•Mild Symptoms: Congested/ Runny nose/ Dry cough/ Low-grade fever/ Sore throat/ Sneezing/ Headache/ Wheezing/ Difficulty Feeding
in Infants:
Short/ Shallow/ Rapid Breathing
Nasal Flaring
Grunting
Accessory Muscle Use
Sternal Retractions
Cough
Poor Feeding
Lethargy
Irritability
Circumoral Pallor
Most children and adults recover in one to two weeks, although some might have repeated wheezing
Severe Cases of RSV
infection can spread to the lower respiratory tract, causing bronchiolitis/ pneumonia- Inflammation of the small airway passages entering the lungs
Complications of RSV
Hospitalization: Severe —- may require hospitalization to monitor/ treat breathing problems and give IV fluids- Tx is symptomatic
Pneumonia/ Bronchiolitis: —- is the most common cause of inflammation of the lungs (pneumonia) or the lungs' airways (bronchiolitis) in infants- These complications occur when the virus spreads to the lower respiratory tract- Lung inflammation can be serious in Infants/ Young children/ Elderly / Immunocompromised/ Chronic Heart or Lung Disease
Otitis Media: If spreads to the space behind the eardrum- happens most frequently in babies and young children
Asthma: Suspected link between severe —- in children and the chance of developing asthma later in life
Repeated Infections: Repeated Infection possible- even during the same —- season- Symptoms usually aren't as severe- But can be serious for those at risk
Prevention: Pharmacological (for RSV)
Antibody Product: (Beyfortus): A single-dose injection given the month prior/ during RSV season- For infants < 8 months born during/ entering their first RSV season
Vaccination during Pregnancy: (Abrysvo): To prevent RSV in infants from birth - 6 months of age- Given from 32- 36 weeks of pregnancy during September- January
RSV Vaccination: (Arexvy): For adults aged 60(+)/ Those at risk
Prevention Behavioral, Patient Teaching: (for RSV)
Frequent hand washing
Avoid exposure: Cover mouth/ nose when cough/ sneeze
Limit infant contact with sick individuals
Disinfect surfaces frequently
Don’t share glasses/ utensils
Don't smoke: Infants exposed to tobacco smoke have a higher risk of getting RSV and potentially more-severe symptoms
Wash toys regularly
Bronchiolitis:
A lower respiratory tract infection that primarily affects the small airways (bronchioles)- A common cause of illness and hospitalization in infants/ young children
•Most common cause is RSV (followed by rhinovirus)
Pathophysiology of Bronchitis
Occurs when virus infects the terminal bronchiolar epithelial cells
Causes damage and inflammation in the small bronchi and bronchioles: Edema/ Excessive mucous- Leads to airway obstruction and atelectasis
Symptoms: of Bronchitis
Preceded by 1–3-day history of URTI
Mimic all those of RSV
Respiratory Distress
Clinical Course: of bronchitis
Symptoms peak on days 3-5- then gradually resolve
Can take 28 days for full recovery
Duration of illness depends on child age/ Severity of illness/ Associated symptoms
Risk Factors: of bronchitis
•Prematurity/ Chronic pulmonary/ Cardiac disease
Complications: of Bronchiolitis
In healthy infants, resolution can occur without complication/ intervention
Some children require extensive cardiopulmonary support
Apnea causing respiratory arrest is a common complication in severe cases
Dehydration from fever/ Decreased oral intake
Clinical Management of Bronchiolitis
Symptomatic Management
IV fluids
Antipyretic
+/- Bronchodilators
+/- Systemic Corticosteroids
Respiratory Support
Nasal Suctioning
Supplemental Humidified O2
High-flow O2 and CPAP
Mechanical Ventilation