Carbohydrate Metabolism
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
Classification of Carbohydrates:
Size of base carbon chain: triose (3 carbons), tetrose (4), pentose (5), hexose (6)
Location of CO Function group
Aldose: terminal carbonyl group (aldehyde group)
Ketose: Carbonyl group in the middle, linked to 2 other carbon atoms (ketone group)
Stereochemistry of compound
Different spacial arrangements around each asymmetric
carbon, forming stereoisomerscarbon, forming stereoisomers
Two different series are possible: D and L.
Number of sugar units in chain
Monosaccharides: 1 unit (glucose, fructose, galactose)
Disaccharides: 2 units (maltose, lactose, sucrose)
Polysaccharides: >10 units (starch [glucose], glycogen)
Stereochemistry of compound:
Different spatial arrangements around each asymmetric carbon, forming steroisomers
Two different series are possible: D and L
Number of sugar units in chain:
Monosaccharides: 1 unit (glucose, fructose, galactose)
Disaccharides: 2 units (maltose, lactose, sucrose)
Polysaccharides: >10 units (starch [glucose], glycogen)
Size of base carbon chain:
Triose (3 carbons), Tetrose (4), Pentose (5), hexose (6)
Location of CO function group:
Aldose
Terminal carbonyl group (aldehyde group)
Ketose
Carbonyl group in middle, linked to 2 other carbon atoms (ketone group)
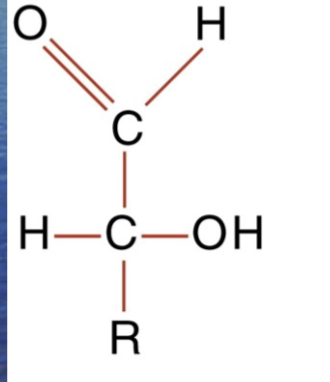
Aldose
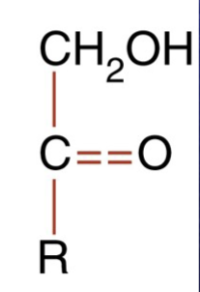
Ketose
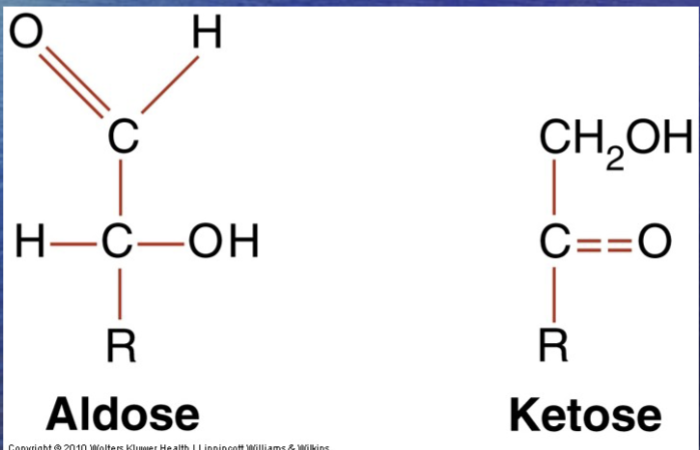
Two forms of carbohydrates
Chemical properties of Carbohydrates: Reducing carbohydrates:
Carbohydrate must have ketone or aldehyde group
All monosaccharide & disaccharides = reducing agents
Examples: glucose, maltose, fructose, lactose, galactose
Chemical properties of Carbohydrates: Nonreducing carbohydrates:
Do not have ketone or aldehyde group & will not reduce
Glucose metabolism:
Primary source of energy for humans; nervous system totally depends on glucose from extracellular fluid
Fate of glucose:
Most ingested carbohydrates are polymers (starch, glycogen)
These are converted to disaccharides, & disaccharides are converted to monosaccharides by enzymes
Monosaccharides are absorbed by the gut & transported to liver
THE ONLY CARBOHYDRATE DIRECTLY USED FOR ENERGY OR STORED AS GLYCOGEN;GALACTOSE & FRUCTOSE MUST BE CONVERTED TO GLUCOSE
Once glucose enters cell, it is shunted into 1 of 3 metabolic pathways
ULTIMATE GOAL OF THE CELL IS TO CONVERT GLUCOSE TO CARBON DIOXIDE AND WATER
Regulation of Carbohydrate Metabolism:
Liver, pancreas & other endocrine glands control blood glucose concentrations within a narrow range
Hormones that control glucose levels (gl):
Insulin: from pancreas; decreases glucose
Glucagon: from pancreas: increases glucose
Epinephrine & glucocorticoids: from adrenal gland: increases glucose
Growth hormone & ACTH: from anterior pituitary: increases glucose
Thyroxine (thyroid gland) & somatostatin (pancreas): increases glucose
Will be question asking which one is NOT one that increases glucose levels
Hyperglycemia:
An increase plasma glucose levels caused by imbalance of hormones
Diabetes Mellitus:
A group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both
Type 1 Diabetes Mellitus:
Results from cellular-mediated autoimmune destruction of beta cells of pancreas, causing absolute deficiency of insulin
Constitutes 10-20% of all diabetes cases; occurs in childhood & adolescence and is genetic/hereditary
Type 2 Diabetes Mellitus:
Characterized by hyperglycemia caused by an individual’s resistance to insulin, resulting in a relative insulin deficiency
Constitutes majority of diabetes cases & is adult onset
Risk factors include age, obesity, lack of exercise, genetic predisposition
Other specific types of diabetes mellitus:
Associated with genetic defects of beta cell function or insulin action, pancreatic/endocrine diseases, etc.
Gestational diabetes mellitus:
Glucose intolerance with onset during pregnancy
Pathophysiology of Diabetes Mellitus:
Hyperglycemia, possibly severe
Glucosuria can occur after renal tubular transporter system for glucose becomes saturated
Pathophysiology of Diabetes Mellitus: Type 1:
Absence of insulin with excess of glucagon
Greater tendency to produce ketones
Pathophysiology of Diabetes Mellitus: Type 2:
Presence of insulin & hyperinsulinemia, attenuated glucagon
Greater tendency to develop hyperosmolar nonketotic states
Criteria for Testing for Pre-Diabetes and Diabetes:
All adults >45 years old should have fasting blood glucose measured every 3 years, unless already diagnosed with diabetes
Testing of glucose should be earlier or more frequent with these risk factors:
Overweight tendencies (BMI greater than or equal to 25 kg/m²)
Habitual physical inactivity
Family history of diabetes in a first-degree relative
High-risk populations
History of gestational diabetes or delivering a baby >9lb
Hypertension (>140/90)
Criteria for testing for pre-diabetes and diabetes: Type 2 diabetes
Testing in children, beginning at age 10 or at onset of puberty & with follow-up testing every 2 years
Family history (first-or second degree) of type 2 diabetes
Race/ethnicity
Signs of insulin resistance
Maternal history of diabetes or gestational diabetes mellitus
Three methods of diagnosis:
Must each be confirmed by one of the others on a subsequent day
HbA1c > or = 6.5% using a method that is NGSP certified
A fasting plasma glucose of > or = 126 mg/dL
An oral glucose tolerance test (OGTT) w/ 2-hour postload (75g- glucose level) > or = 200 mg/dL (mostly to confirm gestational diabetes)
Diabetes symptoms + random glucose level of > or = 200 mg/dL
Diabetes symptoms:
Excessive urination
Rapid weight loss
Drinking a lot of water
Patients with following criteria have “pre-diabetes”:
Fasting glucose of > or = 100 mg/dl but <126 mg/dL
OGTT 2-hour level of > or = mg/dL but <200 mg/dL
Normal glucose level:
~99 mg/dL
When does a glucose level start to be concerning?:
~180 mg/dL
Criteria for Testing & Diagnosis of Gestational Diabetes:
Age >25 years
Overweight
Strong family history of diabetes
History of abnormal glucose metabolism
History of poor obstetric outcome
Presence of glycosuria
Diagnosis of polycystic ovarian syndrome
Hypoglycemia:
Decreased plasma glucose levels
Can be transient & relatively insignificant or life-threatening
Occurs in health-appearing and sick patients, as a result of reaction to medication or of illness
Symptoms appear at glucose level of about 50-55mg/dL
Symptoms of hypoglycemia:
Increased hunger
Sweating
Nausea
Vomiting
Dizziness
Nervousness
Shaking
Blurred speech
Blurred sight
Mental confusion
Methods of Glucose Measurement:
Can be measured from serum, plasma, or whole blood
Serum or plasma must be refrigerated & separated from cells within 1 hour to prevent loss of glucose
Fasting blood glucose should be obtained in morning after 8-10 hour fast
Most common methods of glucose analysis use enzymes glucose oxidase or hexokinase
Nonspecific methods are used in urinalysis section of lab to detect reducing substances other than glucose
Self-Monitoring of Blood Glucose:
Those with type 1 diabetes should check levels 3 or 4 times/day
Glucose Tolerance and 2-Hour Postprandial Tests:
Patient drinks standardized (75g) glucose load
Glucose measurement is taken 2 hours later
What is used as a point of care method:
Statstrip
Results/Flowsheets Glucose Level
Glycosylated Hemoglobin/Hemoglobin A1C:
Long-term blood glucose regulation can be followed by measurement of glycosylated hemoglobin
Provides clinician with time-averaged picture of patient’s blood glucose concentration over past 3 months
Glycosylated hemoglobin: Formation of a hemoglobin compound produced when glucose reacts with amino group of hemoglobin
Hemoglobin A1C (HbA1C) is most commonly detected glycosylated hemoglobin
Affinity chromatography is preferred method of measurement
Ketones:
Produced by liver through metabolism of fatty acids
Provide a ready energy source from stored lipids
Increase with carbohydrate deprivation or decreased carbohydrate use (diabetes, starvation/fasting, high fat-diets)
Specimen requirement is fresh serum or urine
Three ketone bodies:
Acetone (2%)
Acetoacetic acid (20%)
3 beta-hydroxybutyric acid (78%)
Acetone:
2%
Acetoacetic acid:
20%
2-beta-hydroxybutryric acid:
78%
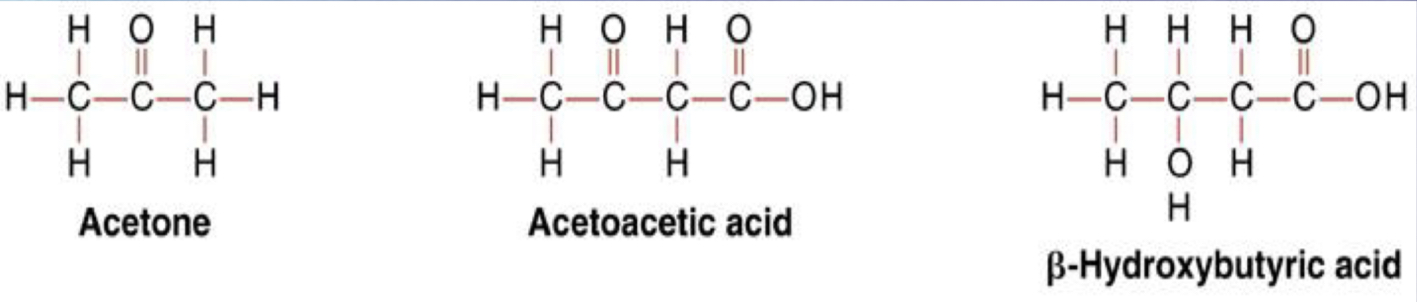
Three ketone bodies
Microalbuminuria:
Increase in urinary albumin is an early sign of renal nephropathy, a complication of diabetes mellitus
Annual assesment of kidney function by determination of urinary albumin excretion is recommended for diabetic patients
Defined as persistent albuminuria in range of 30-299 mg/24 hr or albumin-creatinine ratio of 30-300 ug/mg
Islet Autoantibody and Insulin Testing:
Presence of autoantibodies to beta-islet cells of pancreas is characteristic of type 1 diabetes
Not currently recommended for diabetes diagnosis