KIN 132 - RS exam
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
what is ventilation?
air exchange between atmosphere and alveoli
what is the typical atmospheric pressure?
~760 mmHg
how do people report pressure changes? give an example
they take the relative change from atmospheric (760 mmHg)
a pressure of 758 would have (-2)
ventilation is driven by… ?
driven by an air pressure gradient
from high to low pressure
what does the pressure gradient look like during inspiration?
the atmospheric pressure is high
the alveolar pressure is low
what does the pressure gradient look like for expiration?
the atmospheric is low
the alveolar pressure is high
What do we manipulate to obtain a pressure gradient?
the body can manipulate alveolar pressure, as the atmospheric generally stays the same. and if we travel to higher altitude, the body adjusts alveolar pressure accordingly to get needed pressure gradients for respiration
Boyles Law states that:
in a closed system at constant temperature, pressure and volume are inversely related.
P = 1/V
as one increases, the other decreases, vice versa.
what is compression?
decreasing volume
lower V, higher P
what is decompression
increasing volume
higher V, lower P
Name the three pressures:
what would they look like between inspiration and expiration?
atmospheric pressure (0)
alveolar pressure (0)
intrapleural pressure (-4)
what is atmospheric pressure?
the surrounding environment.
Patm (mmHg)
also knows as air pressure or barometric pressure
what is alveolar pressure?
within alveoli
Palv (mmHg)
what is intrapleural pressure?
the pressure within the thin intrapleural space; between pleura layers
Pip (mmHg)
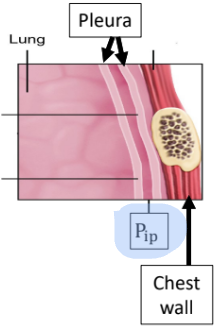
whats particular about intrapleural pressure?
it always has to be less than atm regardless of magnitude.
always subatmospheric (lower than atm)
what does the pressure between alveolar and intraplural create?
creates an outward pressure (0 - -4) that opposes lung elastic recoil
without this outward pressure, the lung would collapse.
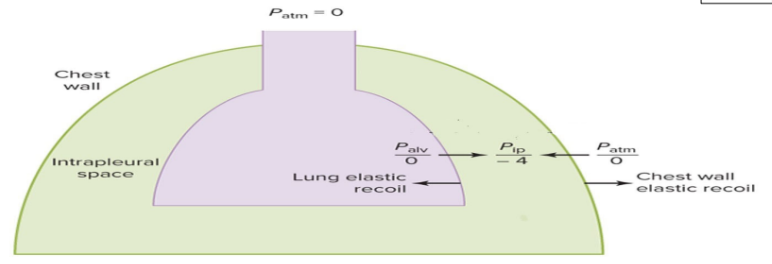
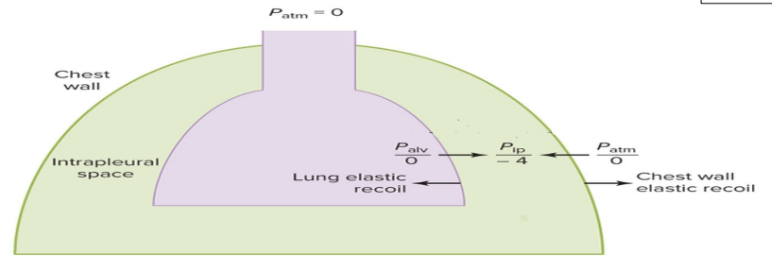
what does the pressure between intraplural and atmospheric create?
creates an inward pressure (-4 - 0) that opposes chest wall elastic recoil
without this pressure, the chest wall would spring out
what happens when you combine the effects of inward and outward pressures?
this links the lung and chest walls together so that they move as a unit.
what is eupnea
quiet, resting, unlaboured breathing
this is like “zone 1”
what muscle movements occur during eupnea inspiration?
the diaphragm contracts downward (flattening) ~2cm
the external intercostals contract out and upward which makes movement of the chest wall
what do the muscle movements in eupnea inspiration cause?
this increases the thoracic cavity volume - leading to a decreased pressure inside the lung (alveolar), making atmospheric pressure higher, allowing air to move along the pressure gradient for inspiration.
diaphragm/external intercostals contract
thoracic cavity volume increases
lung volume increases
Palv becomes subatmospheric
air flows in to lungs
what does a more forceful inspiration look like in terms of muscle movement?
“zone 2”
stronger diaphragm contraction, more downward flattening (up to 10cm)
stronger external intercostal contraction, more outward and upward movement of chest wall
“zone 3”
recruitment of accessory muscles of inpiration such as: scalenes, sternocleidomastoid, pectoralis minor.
contraction allows for more outward and upward movement of chest wall
what are the results of the muscle movement changes that happen during a more forceful inspiration?
greater increase in lung volume
P alv decreases below atmospheric to a greater extent - creating a larger pressure gradient
even more air flows into lungs
what happens is expiration during eupnea and what muscle movements occur?
this is like the recoil to pre-inspiration positions “zone 1”
the diaphragm “turns off” - contraction ends and it recoils back to dome shape
the external intercostals “turn off” - contractions ends and you get the inwards and downward recoil of the chest wall
what do the muscle movements during eupnea expiration cause?
compresses the alveoli + lung volume, raising Palv to be greater than atmospheric pressure, allowing air to flow out
diaphragm/external intercostals stop contracting
recoil - thoracic cavity volume decreases
lung volume decreases; returning to pre-inspiration size which compresses alveoli
Palv becomes greater than Patm
air flows out of lungs
respiratory muscles _______ during inspiration and _______ during expiration
turn on, turn off
what does a more forceful expiration look like in terms of muscle movements?
“zone 2”
stronger contraction of diaphragm and external intercostals ends. as they relax it creates a greater recoil - diaphragm back to dome shape - and inward and downward of chest wall
“zone 2”
recruitment of accessory muscles of expiration (internal intercostals, abdominals) to cause a more inward and downward movement of the chest wall
what are the results the muscle movement changes that happen during a more forceful expiration
greater decrease in lung volume; more compression of alveloi
Palv increases beyond atmospheric to a greater extent causing a greater pressure gradient
even more air flows out of the lungs.
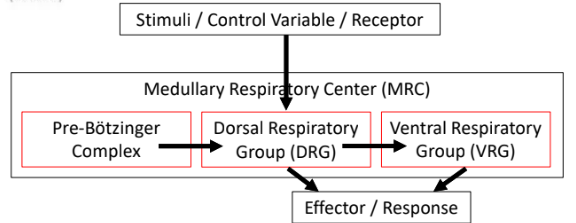
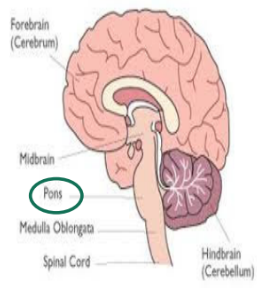
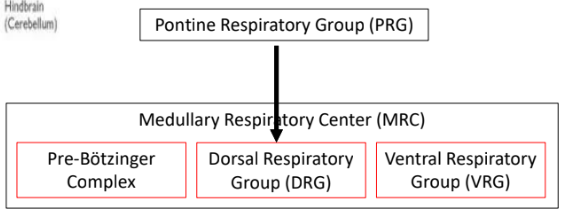
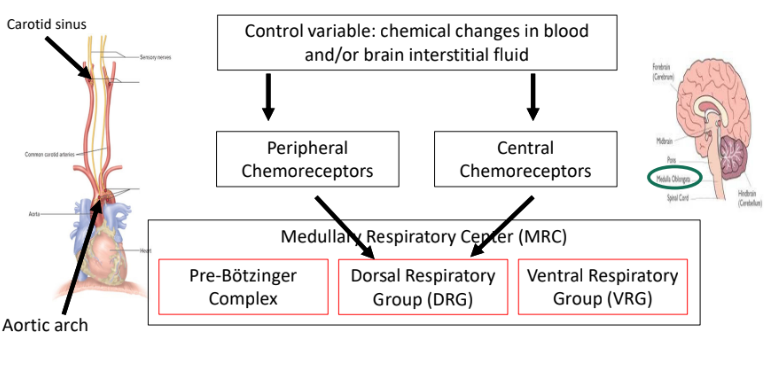
where is the ventilation control center located? what is it called?
in the medulla oblongata; medullary respiratory center (MRC)
*how breathing works is still somewhat disputed*
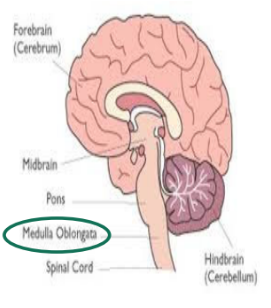
what is in the MRC (medullary respiratory center)
Pre-Botzinger Complex
Dorsal Respiratory Group (DRG)
Ventral Respiratory Group (VRG)
what is the Pre-Botzinger Complex?
this is a possible “pacemaker” ssending signal to DRG to initiate breathing cycle
what is the DRG composed of?
composed of inspiratory neurons
what is the VRG composed of?
composed of inspiratory and expiratory neurons recruited by the DRG
explain a breif stimuli - response involving the MRC
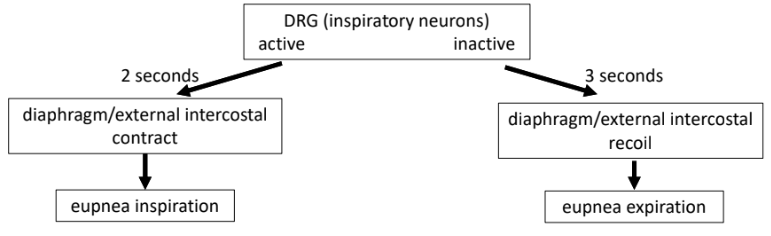
what happens with DRG inspiratory neurons during eupnea
cycle between active and inactive - usually takes about 5 seconds for inspiration and expiration where the breathing frequency = 12 bpm
typical breathing frequeny in eupnea ranges from 6 - 16 bpm
how long are inspiratory neurons active for in a 5 second cycle?
2 seconds - diaphragm/external intercostal contract = eupnea inspiration
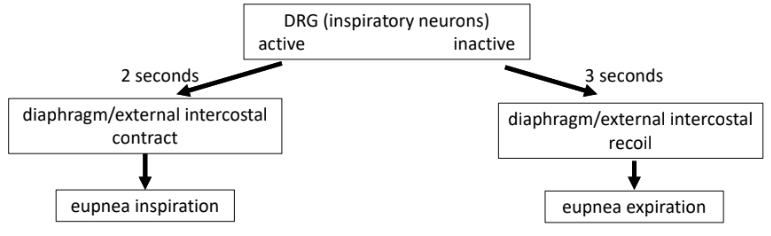
how long are inspiratory neurons inactive for in a 5 second cycle?
3 seconds - diaphragm/external intercostal recoil = eupnea expiration
what can suppress DRG inspiratory neurons and what is the risk of this?
drugs! such as morphine, fentanyl and heroine can suppress DRG inspiratory neurons
overdose deaths with these substances usually involve breathing stopping
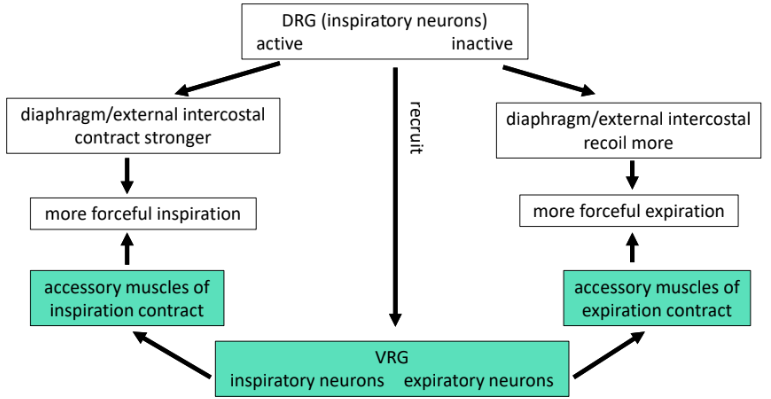
what is different about DRG inspiratory neurons in more forceful breathing?
DRG inspiratory neurons still cycle like at eupnea but a stronger active contractions causes more inactive recoil.
at a certain point…
DRG recruits VRG inspiratory/expiratory neurons to activate accessory muscles of inspiration and expiration
inspiratory VRG neurons activate accessory muscles of inspiration to contract for inspiration
expiratory VRG neurons activate accessory muscles of expiration to contract in expiration
where is pontine respiratory group (PRG) located?
in pons
what influence does the PRG have?
sends a signal to DRG to switch between active and inactive to modify breathing cycle
ex. very strong signal to DRG with speaking and some exercises like swimming.
proprioceptors having an influence on breathing would typically be located where?
proprioceptors in joints and muscles
what influences do proprioceptors have on breathing?
proprioceptors in joints and muscles respond to changes in body movement i.e. rest to exercise
send signal to DRG
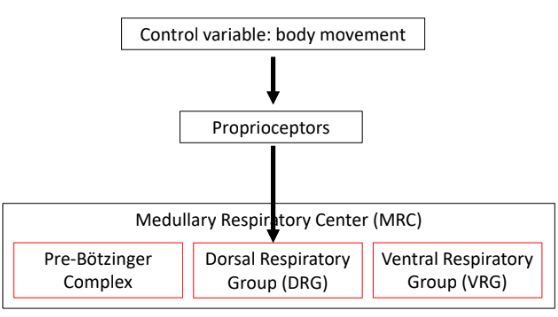
what is the function of proprioceptors having an influence on breathing?
they help match ventilation to movement needs; likely involved when DRG recruits VRG
where are chemoreceptors involved in breathing located?
Peripheral:
carotid sinus
aortic arch
Central:
medulla oblongata
what do peripheral chemoreceptors (in carotid sinus and aortic arch) do?
respond to changes in arterial blood and send signal to control center in DRG
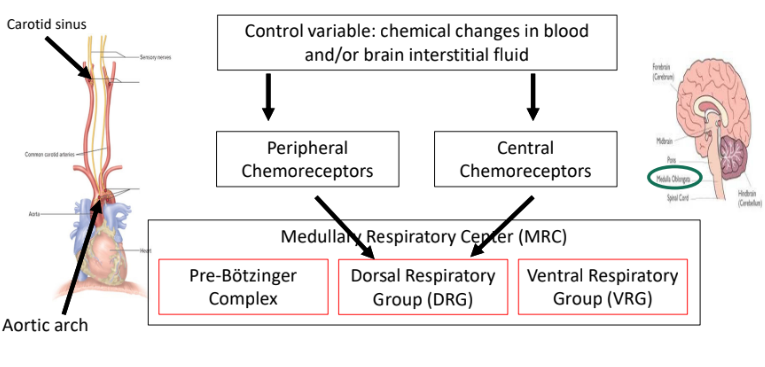
what do central chemoreceptors (in medulla oblongata) do?
respond to changes in interstitial fluid surrounding brain and send signal to control center in DRG
what influence do chemoreceptors have in ventilation when they sense low arterial oxygen?
low arterial oxygen
causes an increased firing in peripheral chemoreceptors
causes increased DRG active/inactive cycling
ventilation
what influence do chemoreceptors have when they sense increased non-CO2 path (like lactate)
higher non-CO2 path (like lactate)
increased arterial H+
increased firing of central chemoreceptors
increased DRG active/inactive cycling
ventilation
what influence do chemoreceptors have when they sense a higher arterial CO2?
higher arterial CO2
increased arterial H+
increased firing peripheral chemoreceptors
increased DRG active/inactive cycling
ventilation
AND
increased brain interstitial fluid CO2
increased brain interstitial fluid H+
increased firing of central chemoreceptors
increased DRG active/inactive cycling
ventilation
what is apnea?
stopped breathing
higher brain center influences (anything above brainstem control system; cerebrum and/or cerebellum)
its a voluntary signal with limited ability to override involuntary breathing
what are the risks of apnea?
if arterial O2 becomes low enough you could pass out - involuntary breathing should resume
if arterial CO2 gets high enough - involuntary breathing starts
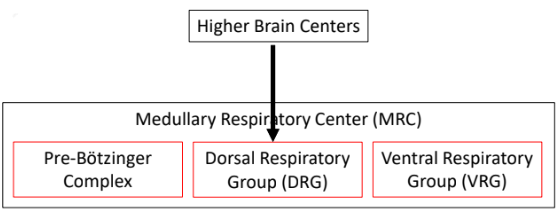
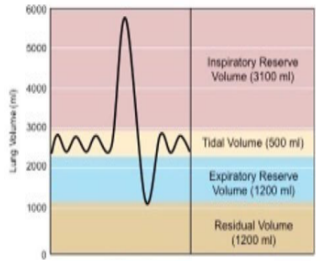
what is tidal volume (TV)?
air volume inspired (tidal inspiration) or expired (tidal expiration) in one breath
inspiratory reserve volume (IRV)?
how much more air volume can be inspired after a tidal inspiration
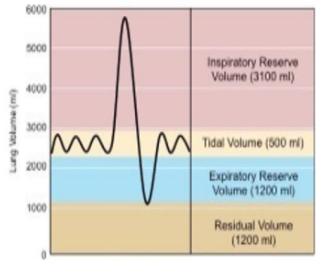
expiratory reserve volume (ERV)?
how much more air volume can be expired after a tidal expiration

residual volume (RV)?
air volume remaining in lungs after maximum expiration
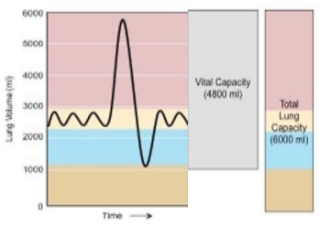
what is vital capacity
VC = combination of IRV + TV + ERV
the air volume expired from maximum inspiration to maximum expiration
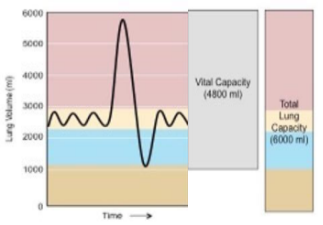
what is total lung capacity?
TLC = combination of IRV + TV + ERV + RV
maximum air volume lungs can contain
what ventilation volumes change from rest to exercise?
increasing TV
decreasing reserve volumes (both IRV and ERV)
what was previously “reserve” is now being used as part of tidal volume
these changes dont really affect much else - no change in RV, TLC, or VC

forced vital capacity
air volume expired from maximum inspiration to maximum expiration as hard and as fast as possible
forced expiratory volume in 1 second (FEV1)
volume of air expired in 1st second of FVC effort
%FEV1 = FEV1/FVC x 100%
changes in forced vital capacity can be caused by?
obstructive lung diseases; difficulty expiring air out of lungs
restrictive lung diseases; difficulty fully inspiring air into lungs
whats the difference in FCV and FEV1 between obstructive and restrictive lung diseases?
obstructive: both FCV and FEV1 decrease, but FEV1 decreases much more so percentage goes down substantially
restrictive: both FCV and FEV1 decrease, but similar amount so percentage stays relatively the same or even can increase.

what is minute ventilation (VE)?
air volume flowing into or out of lungs per unit time (L/min or mL/min)
combines tidal volume and breathing frequency
VE = VT x f
VT - air volume inspired or expired in one breath
f - breathing frequency or respiratory rate (bpm; breaths per minute)
what does eupnea minute ventilation look like?
TV = 500 mL/breath ; f = 12 bpm
VE = 500 × 12 = 6000 mL/min or 6 L/min
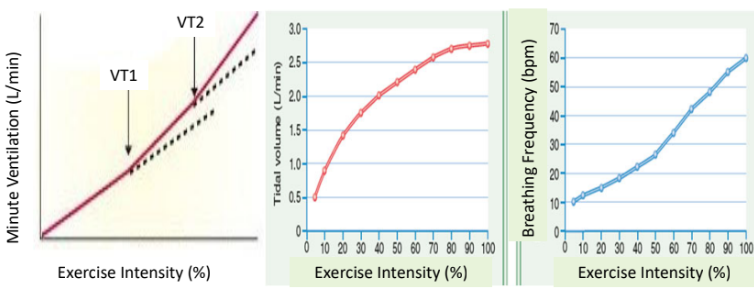
if we look at trends on a graph for either minute ventilation, tidal volume, and breathing frequency, during excercise, what would each graph look like?
minute ventilation: fairly linear from eupnea up until moderate intensity. followed by 2 exponential increases with further increasing intensity (named VT1 and VT2 - ventilatory threshold points)
tidal volume: fairly linear from eupnea to moderate intensity then plateauing from moderate to max
breathing frequency: fairly linear from eupnea to max intensity
what is dead space (VD)?
the portion of minute ventilation that does reach gas exchange areas
types of dead space?
anotomical; conduction zone portion of airways (structures that do not participate in gas exchange
alveolar dead space; damaged or blocked alveoli
physiological dead space = anatomical + alveolar
alveolar ventilation
air volume flowing into or out of alveoli per unit time
= (VT - VD) x f