Lecture 2: Molecules and Cells of The Immune System
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
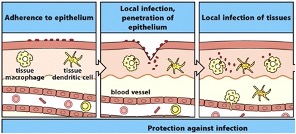
Stages of the Immune Response
1. Prevention – barriers
2. Awareness-recognition – barrier cells are alerted, with mechanisms present to recognise an infection
3. Immediate Response: innate immune cells
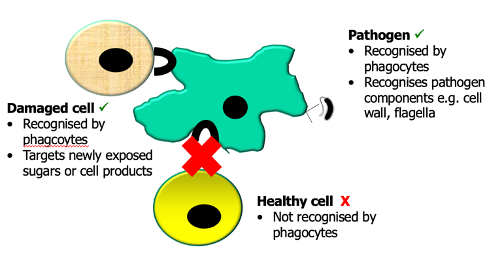
Initiation of Phagocytosis
Phagocytes/ innate cells recognise specific molecules on/in targets:
Pathogens: Recognise conserved features like LPS, cell wall, flagella
Damaged cells: Recognise damage signals like exposed sugars, cell products, and intracellular ATP
Healthy cells: Not recognised by phagocytes (no phagocytosis)
Mannose Receptors
Part of the C-type lectin receptor family
Bind to carbohydrate structures (mannose) found on e.g. yeast, parasites, bacteria
Dectin-1/ B-Glucan Receptors
Part of the C-type Lectin Receptors
Binds b-glucan structures
Involved in anti-fungal responses
Scavenger Receptors
Bind low density lipoproteins, sialic acid
Found on bacteria and yeast
Lipid Receptors
Regulate how cells metabolise fats and sugars
This metabolic control is especially important for macrophages
Metabolism influences which pathogens macrophages respond to
Lipid receptors direct immune function through the metabolic path
CR3 and CR4
Complement receptors
Recognise consevered features e.g. LPS, liphosphoglycan, bcateria and yeast
Nobel Prize in Physiology and Medicine 2011
Awarded to Bruce A. Beutler and Jules A. Hoffmann
“for their discoveries concerning the activation of innate immunity"
Jules Hoffman: Discovered Toll gene in Drosophila – discovered innate receptors that recognised bacteria
Bruce Beutler: Discovered Toll Like Receptors in mammals
Toll Like Receptors
Family of Pattern Recognition Receptors.
Recognise:
highly conserved structures on pathogens called Pathogen Associated Molecular Patterns (PAMPs)
Danger Associated Molecular Patterns (DAMPs) from damaged cells e.g. uric acid, Heat Shock Protein
Located on the cell surface or intracellularly
Form dimers (homo- or heterodimers) that determine pathogen specificity
Once activated, they recruit intracellular molecules, resulting in a signalling cascade with the net result of gene transcription of specific cytokines that are important in infection responses and events e.g. phagocytosis
Examples of TLRs
TLR5 – homodimer that recognises bacteria flagella
TLR9 recognises CPG DNA
TLR3 – located intracellularly and recognises doubles stranded RNA – important in virus recognition
TLR7 and 8 recognise single-stranded RNA
Retinoic Acid Inducible Gene (RIG)-Like Receptor (RLR)
A pattern recognition family
Includes RIG-1 and cytosolic receptors that are involved in viral recognition
C-Type Lectin Receptors (CLRs)
A family of pattern recognition receptors
Major role in the recognition of yeast, some bacteria and parasitic worms
Nucleotide Binding Domain (NOD)-Like Receptors
E.g. NOD2, NLRP3, NLRP11, Cytosolic receptors
Recognise intracellular substances e.g. viruses and bacteria
some are more evolved to recognise damage
Damage Receptors
Detect damage caused by pathogens to initiate phagocytosis
Do not respond to harmless/ beneficial microbes (e.g. microbiome)
Key receptors include:
NLRs (e.g. NLRP1, NLRP3, NLRC4) – sense cellular stress/damage
RAGE – binds to damage markers like calprotectin, a product of neutorphils (inflammation marker in stool/serum)
P2X7R – binds extracellular ATP, a danger signal
Phagocyte Receptors
Cells that act to recognise generic features of pathogens, infections and feature of damaged cells
Phagocytosis
= eating
1. Attachment via PRRs
2. Ingestion – cells change their structure to enfold and engulf the pathogen
3, Killing – pathogen taken in via the phagocytic vacuole where there are enzymes present to degrade and destroy it
4. Degradation
Cytokines
Soluble hormone like molecules of the immune (and other) systems e.g. Epidermal growth factor
any one _________ can act on a cell to make a whole range of _________
Families of Cytokines and Their Main Function
Interleukins (1-41): Diverse functions in immune response
Interferons: Specialised for anti-viral response
Colony Stimulating Factors: Promote differentiation and generation of new immune cells (Haematopoiesis)
Tumor Necrosis Factor (TNF): Involved in inflammation, targeted in autoimmune disease therapy
Chemokines: Small cytokines involved in chemotaxis (cell movement)
Types of Cytokine Action
Will act on other cells that have a receptor for it via:
Endocrine: target is located far away – reached via the circulation (rare)
Paracrine: act on nearby cells
Autocrine: act on the cell that produces it, if it has the receptor present
Inflammasome
Part of the damage-sensing response
Triggered when receptors activate a signaling cascade to form the inflammasome
PRRs-NLRs (e.g., NLRP1, NLRP3, NLRC4) initiate the inflammasome platform, allowing signalling molecules to come together
Functions:
Initiates a specialised type of programmed cell death
Enables secretion of active cytokines (IL-1β, IL-18) by cleaving and releasing them from their pro-forms
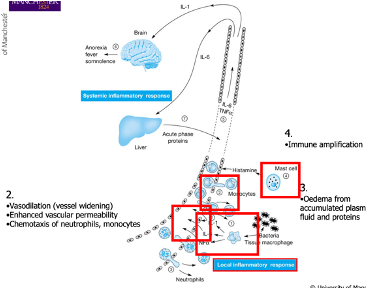
Drivers of Inflammation
Cytokines and the recruitment of immune cells
Local Inflammatory Response to Infection
PRRs on macrophages recognise infection and trigger cytokine production
Cytokines cause:
Changes in vasculature: vessel widening and increased permeability
Recruitment of immune cells to the site of damage through leaky blood vessels
Chemokines mediate recruitment, bringing additional immune cells
Neutrophils: Major first responders to infection, most common innate immune WBC
Monocytes: Recruited and can later differentiate into macrophages or dendritic cells
Results in oedema: Swelling due to plasma fluid and protein accumulation in response to cytokine and inflammatory product generation
Mast cells may also be recruited
Mast Cells
Granulocyte
Innate cells that contain granules that are filled with pre-formed chemical mediators that can be rapidly deployed
Resting vs Activated Granulocyte
Resting: nucleus, cytoplasm containing granules
Activated: contents of granules are released - able to carry out transcription and make a range of new products
Mast Cell Products:
Two types
Pre-formed granules - released immediately
Histamine
Heparin (anticoagulant)
Enzymes e.g. tryptase, chymase – important in effector response
Effector substances - synthesed later - delayed release
Prostaglandins
Leukotrienes
Cytokines
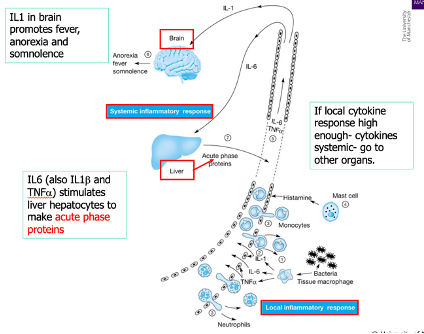
Systemic Inflammatory Response
Mast cells release and synthesise various products upon recruitment
If the local response is high enough, it can trigger a ______ response
Cytokines can act endocrinically, affecting distant tissues (e.g., the brain)
This can give rise to symptoms like loss of appetite and fever due to immune system changes
The liver may be implicated and releases IL-6, contributing to the systemic response
Acute phase proteins (ancient part of the innate immune system) are activated, playing a role in immune defence with various effector functions
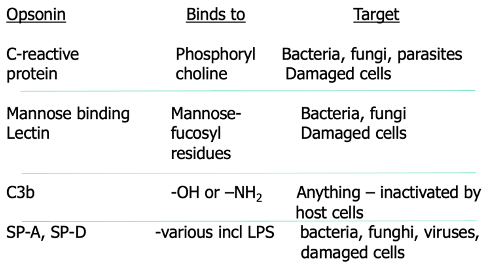
Acute Phase Proteins
Fibrinogen: Involved in clotting
Haptoglobulin: Binds iron
Complement C3: Cleaved to form C3a and C3b, which act as opsonins
Mannose Binding Lectin (MBL): An opsonin that triggers the complement system
Serum Amyloid: Inhibits fever and platelet activation
C-reactive protein (CRP): Binds phosphorylcholine, acts as an opsonin, and can trigger complement
Surfactant proteins SP-A and SP-D: Act as opsonins
All these proteins are synthesised by the liver and play a key role in amplifying the innate immune response
Opsonin
Something that will bind to a molecule on a pathogen and acts as an ‘eat me’ signal for macrophages and other signals
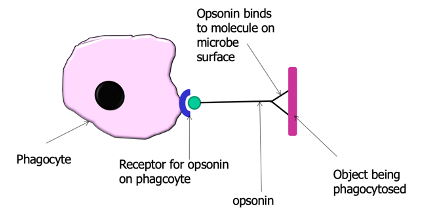
Opsonins of the Innate Immune System
Complement
A collection of soluble proteins important in innate defence
Circulates in inactive form in plasma
Activated by infection or immune cells, initiating a cascade that result in the release and activation of prodcuts that contribute to inflammation or will act as opsinins
Function of Complement
Target lysis (destruction of pathogens)
Chemotaxis (e.g., C3b directs immune cells)
Activation of mast cells (e.g., C3a, C5a)
Clearance of immune complexes (via C3b)
Amplifies the immune response by helping to kill cells, activate mast cells, guide immune cells, and aid in immune resolution and repair
Complement Pathways
Classical Pathway: Triggered by antibody or CRP
Alternative Pathway: Triggered by C3b
Lectin Pathway: Initiated by MBL
Interferons
Big cytokine family
Inflammatory cytokine – involved in the virus responses
Inhibit viral replication within infected cell
Bind to cells expressing interferon receptors – render them resistant to infection
Activate macrophages and natural killer cells
Sources of Interferons
Produced by virus-infected cells
Also made by other immune cells
Actions of Interferons
Can act autocrine (on the same cell) or paracrine (on nearby cells)
Trigger an antiviral state in surrounding cells – a shielding effect - renders cells resistant to infection
Help kill viruses inside infected cells; renders neighbouring cells resistant to infection
Enhance macrophage function
Secreted IFNs bind to IFN receptors and initiate antiviral defence (e.g. blocking infection)
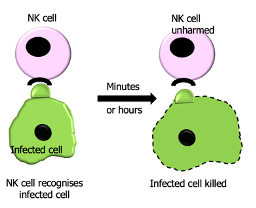
Natural Killer Cells
Innate cells with a simillar progenitor to lymphocytes (simillar apperance)
They can release lytic granules that kill some virus-infected cells
They are an important early source of interferons – crucial in controlling an early viral infection
Function was inhibited by Sars-Cov2
Natural Killer Cells Mechanism of Action
Different mechanisms for recognising infected cells
Detect changes via receptor recognition or detection of missing normal 'self' receptors (e.g. MHC I loss)
Once an infected cell is recognised, NK cells bind rapidly and can kill the cell within
Innate Cells
Granulocytes (Inc. Mast Cells)
Eosinophils (common)
Basophils
Lymphoid Like cells (Inc. NK cells)
Innate lymphoid cells
Phagocytes/ APC (inc. macrophages, monocytes and neutrophils)
Dendritic Cells - direct adaptive immunity
Eosinophils
Common cells
Involved in
anti-pathogen responses
roles in immune cell recruitment – amplification
Obesity
Basophils
Rare in circulation
Involved in
anti-pathogen response
may support the generation of adaptive immunity
Innate Lympoid Cells
Part of the lymphoid lineage
3 subtypes defined by cytokine profile/function ILCs1-3
ILCs1 has a similar function to NK cells
ILCs 2: helminth infections and allergens,
ILC3s: responses against extracellular microbes and tissue homeostasis
Can support gut immune responses
Critical role in barrier function
Innate Immune System (Function)
Provides vital early responses to infection
Innate cells work together to limit the spread of infection
Without an effective innate response, infections are more likely to become uncontrolled
Deals with the threat and communicates with other aspects of the immune system (adaptive immunity and lymphcytes)
Innate Immune System
Immediate
Varied methods of attack
Not very specific; generic
Helps direct adaptive response
“Memory”- imprinting; crude memory where if the same type of flu is encountered after a few years it will result in a more powerful response
neutrophils, macrophages,
natural killer cells
Adapative Immune System
Later in the immune response
via B and T-cells
Targeted and SPECIFIC killing
Has Memory ‘forever’
B lymphocytes,
T lymphocytes
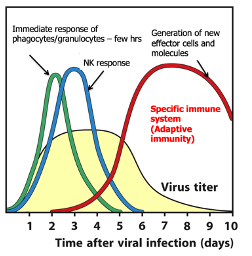
Innate and Adaptive Immmunity
Immediate response of phagocytes/granulocytes – within a few hrs, followed by the NK response
As the innate response beings to peak to control the virus and stop it from getting ‘too high,’ the adaptive response will be activated and will take over
Generation of new effector cells and molecules
Specific immune system (Adaptive immunity)