The Complement System
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
15 Terms
What is the complement system?
An innate immune defence system→ triggered rapidly and by a range of pathogens, no specificity, adaptation and memory.
It consists of multiple proteins that are activated in sequence, main role is to kill pathogens immediately when they enter the body.
It is involved in the clearance of antigen-antibody complexes.
It is either activated by the presence of either PAMPs or by antigen by antibodies.
Where are most complement proteins synthesised?
The liver, however some components are made by mast cells, macrophages and neutrophils.
What are the majority of components used in the complement system?
Most components are inactive enzymes (serine proteases); these require cleavage by the complement protein immediately upstream in the cascade and then, in turn cleave the component downstream of them.
What is the outcome of the complement system?
Direct lysis of microbes; opsonisation (coating or tagging microbes for killing); inflammatory mediator release to help recruit more immune cells.
What are the 3 pathways for complement activation?
There are 3 major pathways to complement activation; each triggered in a different manner by different components
1) Alternative pathway, triggered by microbes, innate
2) Lectin pathway, triggered by microbes, innate
3) Classical pathway, triggered by antibodies (IgM and IgG), bound to antigens, consequence of adaptive immune response.
What characteristics does the three major pathways to complement activation have in common?
They all consist of a proteolytic cascade that allows for signal amplification
2. They all result in the creation of a C3 and C5 convertase
3. They all end in a common terminal pathway also known as a membrane attack complex (known as MAC).
How can the complement system be amplified?
A C3 convertase can cleave hundreds to thousands of C3 molecules into C3a and C3b.
What is the classical complement pathway triggered by?
Triggered by antibody/antigen complexes. Activation of this pathway relies on the production of specific antibodies that may take several days to appear after a new infection.
IgM and IgG are the activators of the classical complement pathway
Describe the complement pathway:
1) The complexes bind to the first complement component C1 complex (C1q,r,s)
2) C1 binding activates the protease activity of C1r and C1s → works on the next component in the cascade
3) C4 and C2 are cleaved by C1 in sequence ➔ form a complex as C4b2a ➔ this is a C3 convertase (cleave C3 to C3a, C3b)
4) C3b is a key component: it attaches to the microbe surface
- Opsonisation: tag it for phagocytes
- Initiates MAC for cell lysis
• C4b2bC3b complex converts C5 to C5a and C5b
• C5b leads downstream to MAC
5) C3a and C5a are proinflammatory mediators
What are lectins?
Lectins are proteins that bind sugar (carbohydrate) residues on the microbe cell surface or cell wall
Best characterised is mannose-binding lectin MBL (PRR) which binds PAMPs in bacterial cell wall.
This triggers enzymatic activity in MBL-Associated Serine Proteases (MASP)
How does the lectin complement pathway work?
MBL-Associated Serine Proteases (MASP) cleave C4 and initiate cascade as seen for classical pathway.
How does the alternative complement pathway work?
Innate pathway, does not require antibody or recognition of PAMPs.
Relies on C3: In normal host C3 spontaneously hydrolyses at a low level to C3a and C3b; C3b can then bind cell surfaces --- MAC.
However, C3b can also bind host cell surface –needs to be controlled.
Factor H and Factor I inactivate and degrade C3b when it’s bound to host cells (linked to the level of sialic acid residues present)
When C3b is bound to microbial cells there is no sialic acid; therefore Factor H and I cannot act.
Instead Factor B and Factor D bind and this initiates MAC assembly.
What is a membrane attack complex?
End product of each of the 3 pathways
Complex of components C5b, C6, C7, C8 and C9
Aim: construct a protein complex (MAC) that essentially punches a hole in the target membrane - microbe is destroyed by osmotic lysis
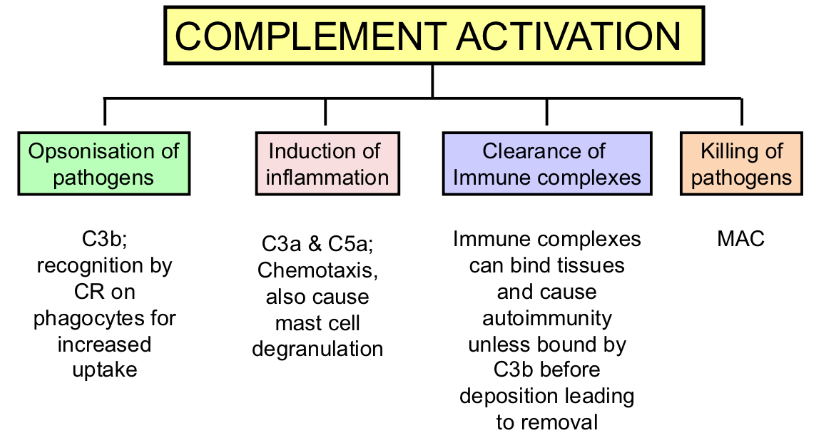
What are the outcomes of complement activation?
How is the complement pathway regulated?
Regulated by a series of proteins that increase selectivity (microbe only) and limit cascades from continuing too long.
Most function by inhibiting the enzymatic activity, or by promoting degradation of the components
Factor H and I bind C3b on host cells
C1 inhibitor: stops unwanted activation of classical pathway