locomotion final mcq
1/264
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
265 Terms
what is movement?
the contraction of a skeletal muscle attached across a moveable joint
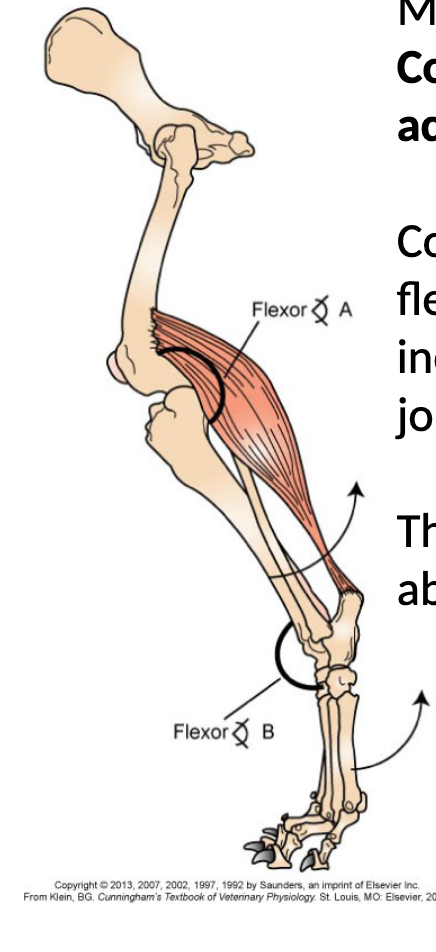
contraction will decrease the flexor angle at joint A and increase the flexor angle at joint B producing the movement indicated by the arrows
what makes up the structure of a striated skeletal muscle fibre?
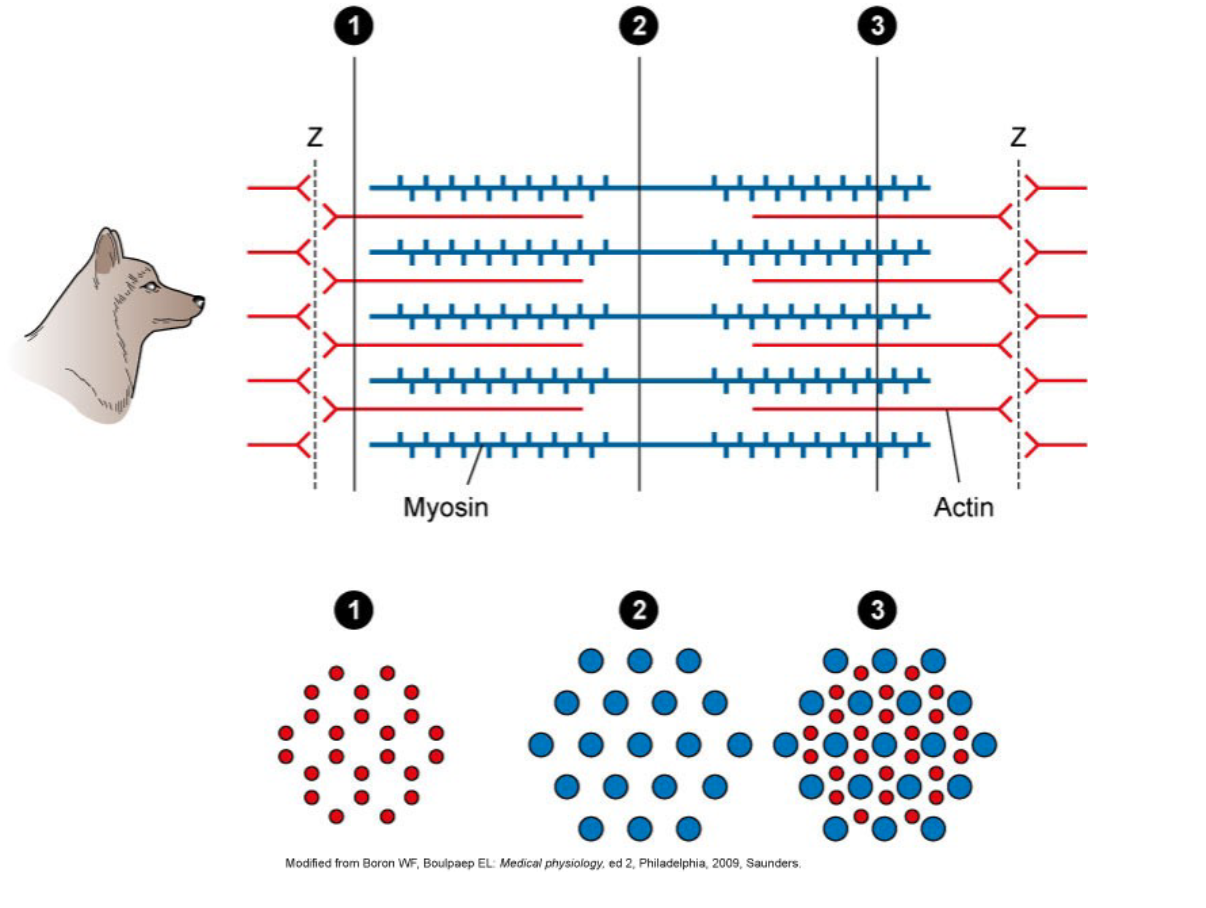
parallel arrangement of actin and myosin filaments in a sarcomere, every 1 myosin has at least 6 actic associated with it
What are thick and thin filaments in a striated muscle?
thin filament = actin
tick filament = myosin
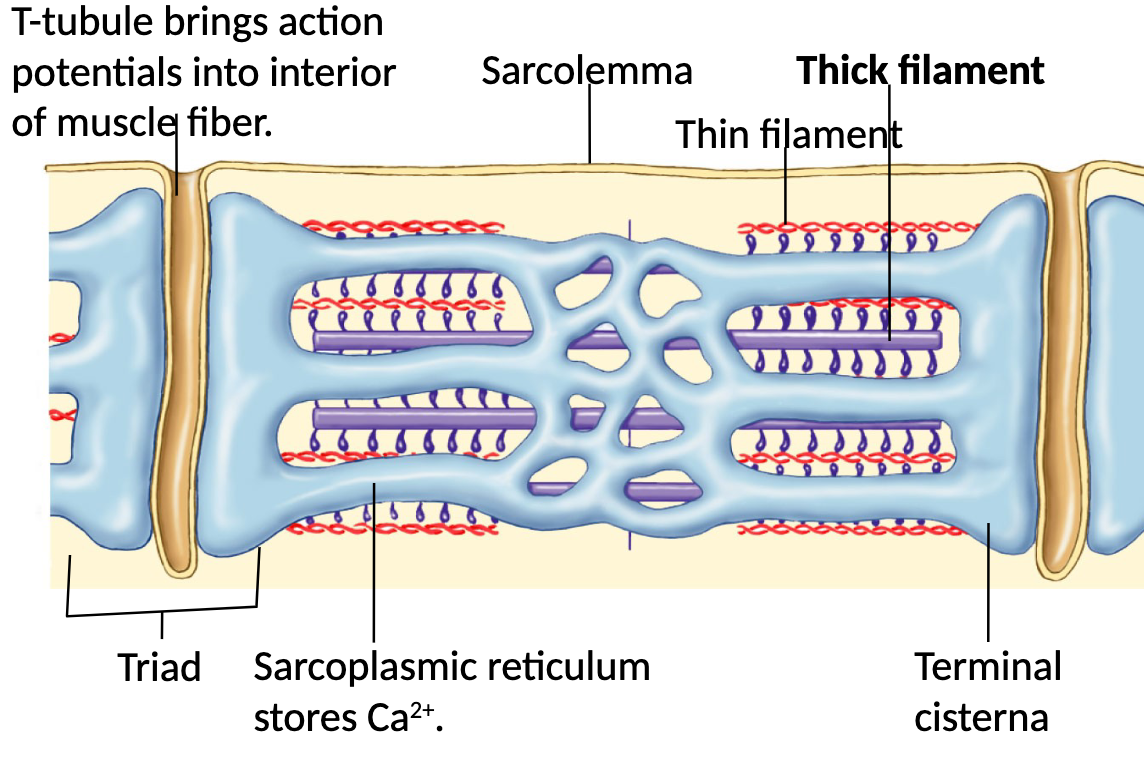
What is the purpose of the T tubles and sarcoplasmic reticulums present in muscles?
T-tubles = bring action potentials into interior of muscle fibre
sarcoplasmic reticulum = stores Ca2+, nerves are brought close during contraction
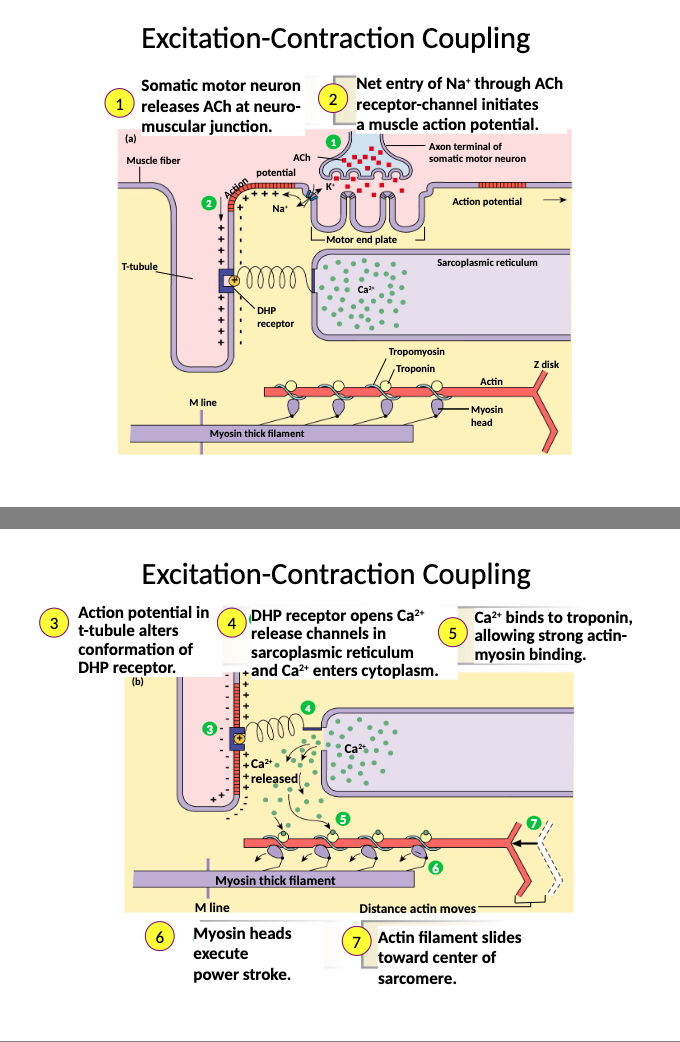
What are the steps to excitation-contraction coupling?
1) somatic motor neuron releases ACh at neuro-muscular junction
2) net entry of Na+ through ACh receptor-channel initiates a muscle action potential
3) action potential in T-tubule alters conformation of DHP receptor
4) DHP receptor opens Ca2+ release channels in the sarcoplasmic reticulum and Ca2+ enters the cytoplasm
5) Ca2+ binds to troponin C allowing strong actin-myosin binding
6) myosin heads execute power stroke
7) actin filament slides toward centre of sarcomere
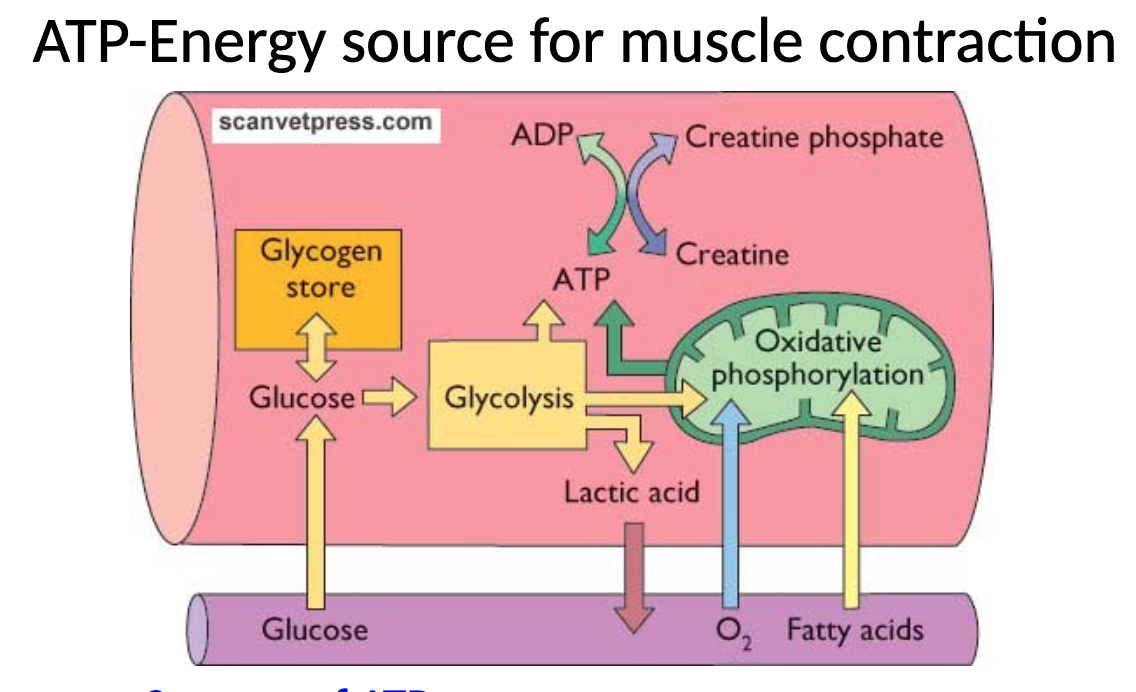
What are the three sources of ATP as an energy source for muscle contraction?
oxidative phosphorylation, glycolysis, and creatine phosphate
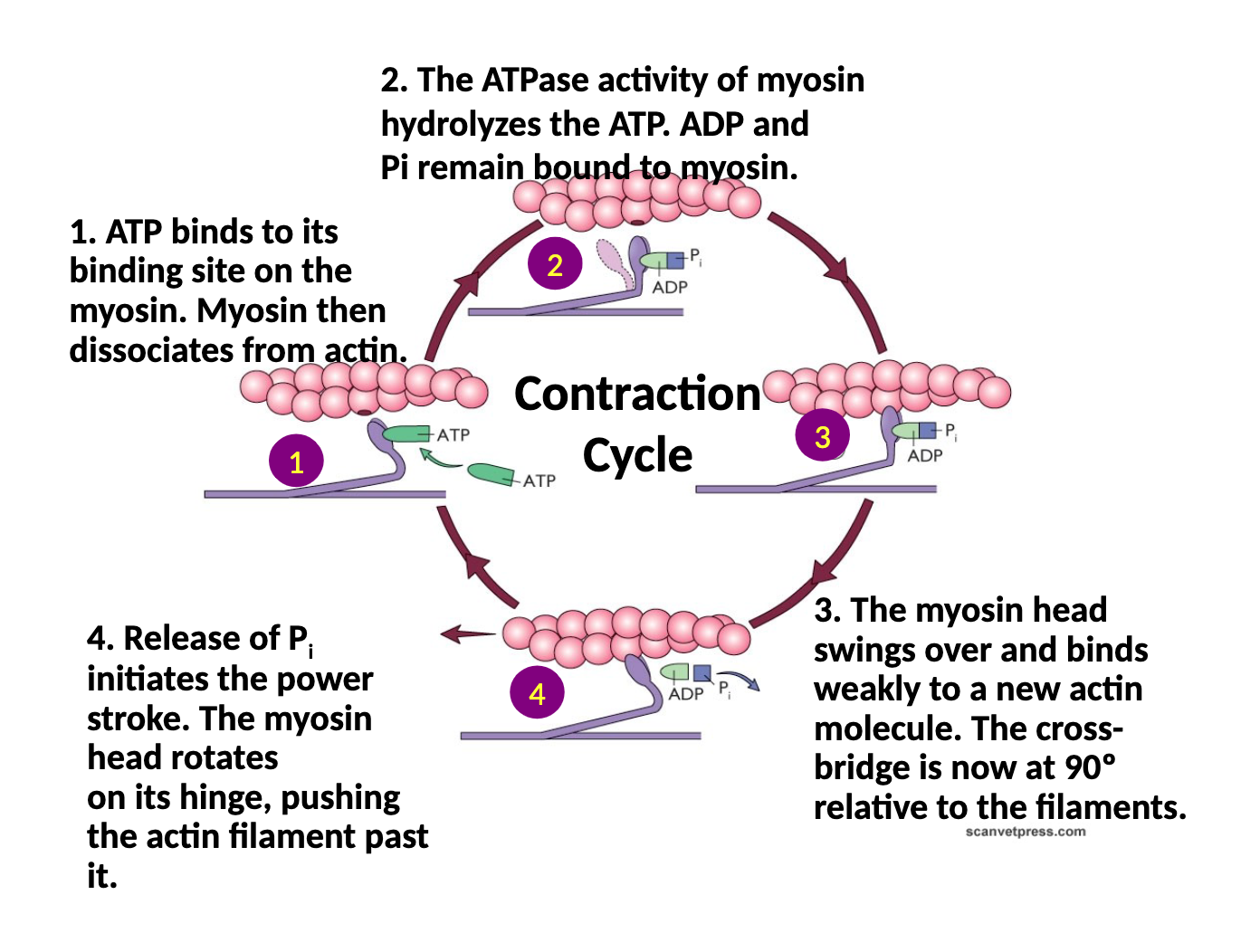
What are the steps in the contraction cycle/power stroke?
1) ATP binds to binding site on myosin, myosin dissociates from actin
2) ATPase activity of myosin hydrolyzes the ATP, ADP and phosphate remain bound to myosin
3) myosin head swings over and binds weakly to a new actin molecule, the crossbridge is now at 90 degrees relative to the filaments
4) the release of the phosphate initiates the power stroke, the myosin head rotates on its hinge pushing the actin filament past it
What are the two different muscle classifications?
1) Fast twitch fibres (white muscle, glycolytic) - larger, extensive SR, less mitochondria, less blood vessels, rapid fatigue, adapted for jumping, sprinting and powerful movement
2) Slow twitch fibres (red muscle, oxidative) - smaller, rich in mitochondria and blood supply, large myoglobin, less prone to fatigue, adapted for continual contraction
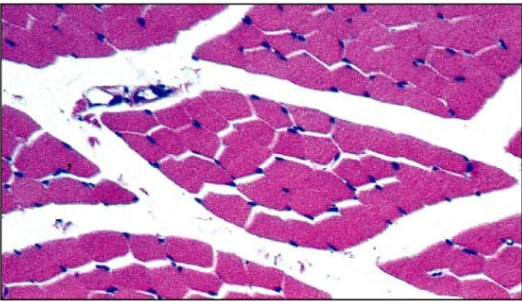
what is this showing?
slow twitch oxidative muscle fibres, note smaller diameter (fatigue resistant)
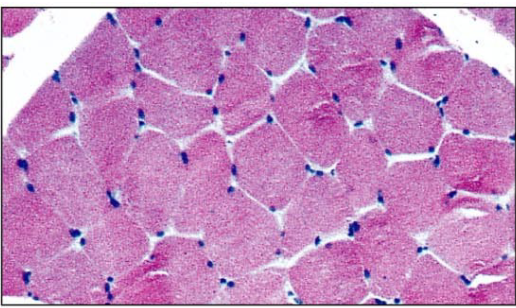
what is this showing?
fast twitch glucolytic muscle fibres, note larger diameter (easily fatigued)
What is the motor unit made of?
motor neuron and all the muscle fibres that it innervates
What is the strength of contraction in muscles based on? What is it recorded on?
1) active motor units - recruitment or spatial summation (number of motor units that contract)
2) rate of motor unit activation - temporal summation (frequency of motor unit activation)
All recorded on an electromyogram
what is a motor unit pool?
basically a ‘ganglion’ but for muscle nerves, a group of motor neurons that all innervate the same muscle
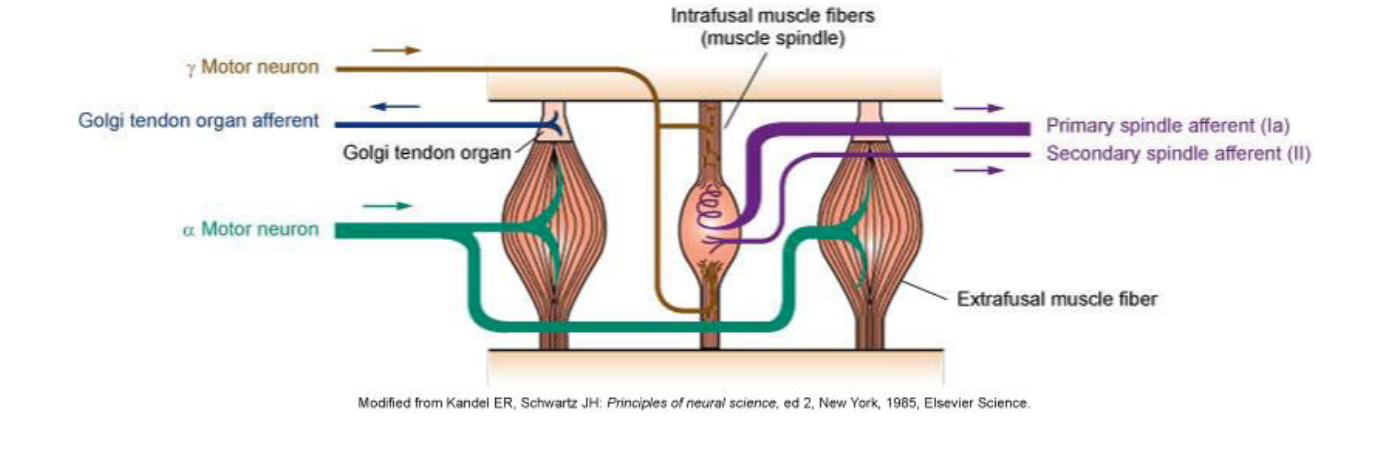
what is a skeletal muscle receptor organ?
muscle spindle = parallel arrangement, detects muscle length so is a stretch receptor, can signal dynamic and steady-state length of muscle
golgi tendon organ = arranged in series, detects muscle tension
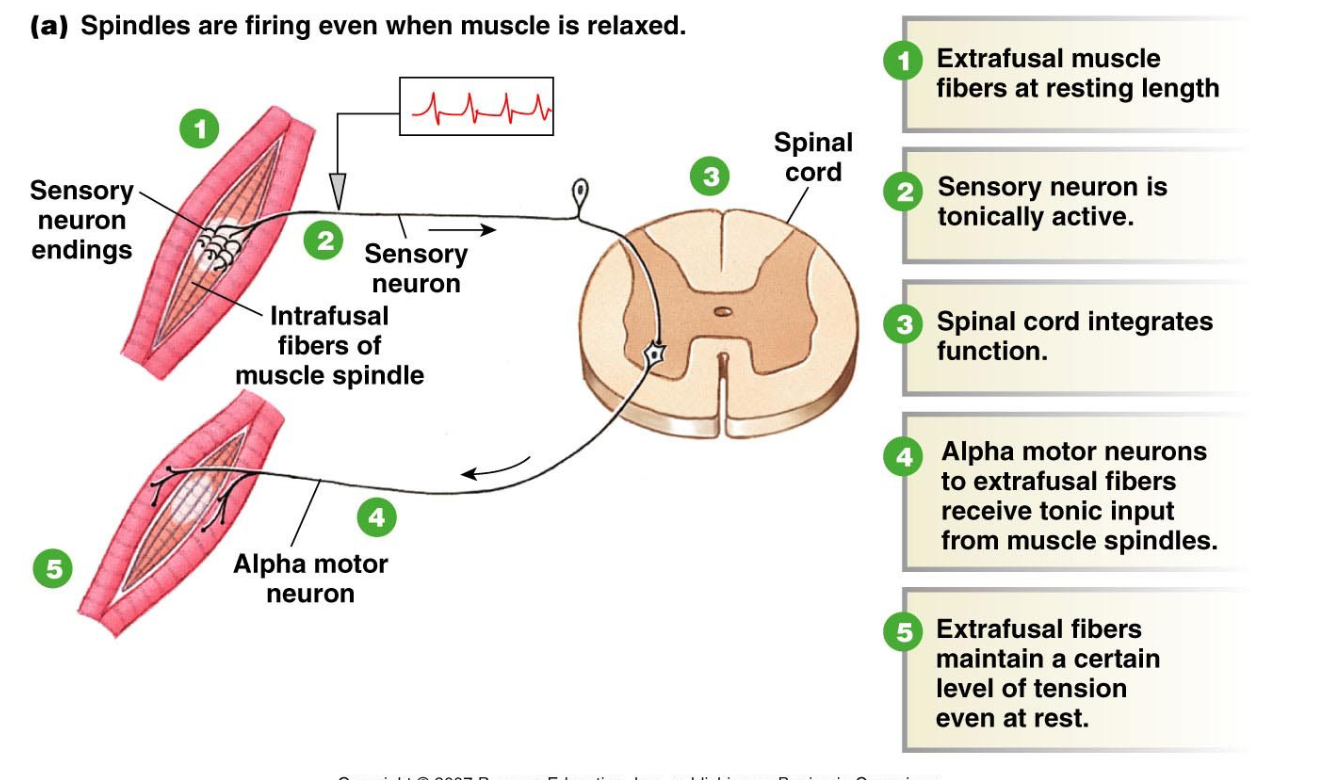
What helps to maintain tone in skeletal muscle?
tonic activity of muscle spindle helps maintain tone in skeletal muscle, spindles are firing even when muscle is relaxed, extrafusal fibres maintain a certain level of tension even at rest
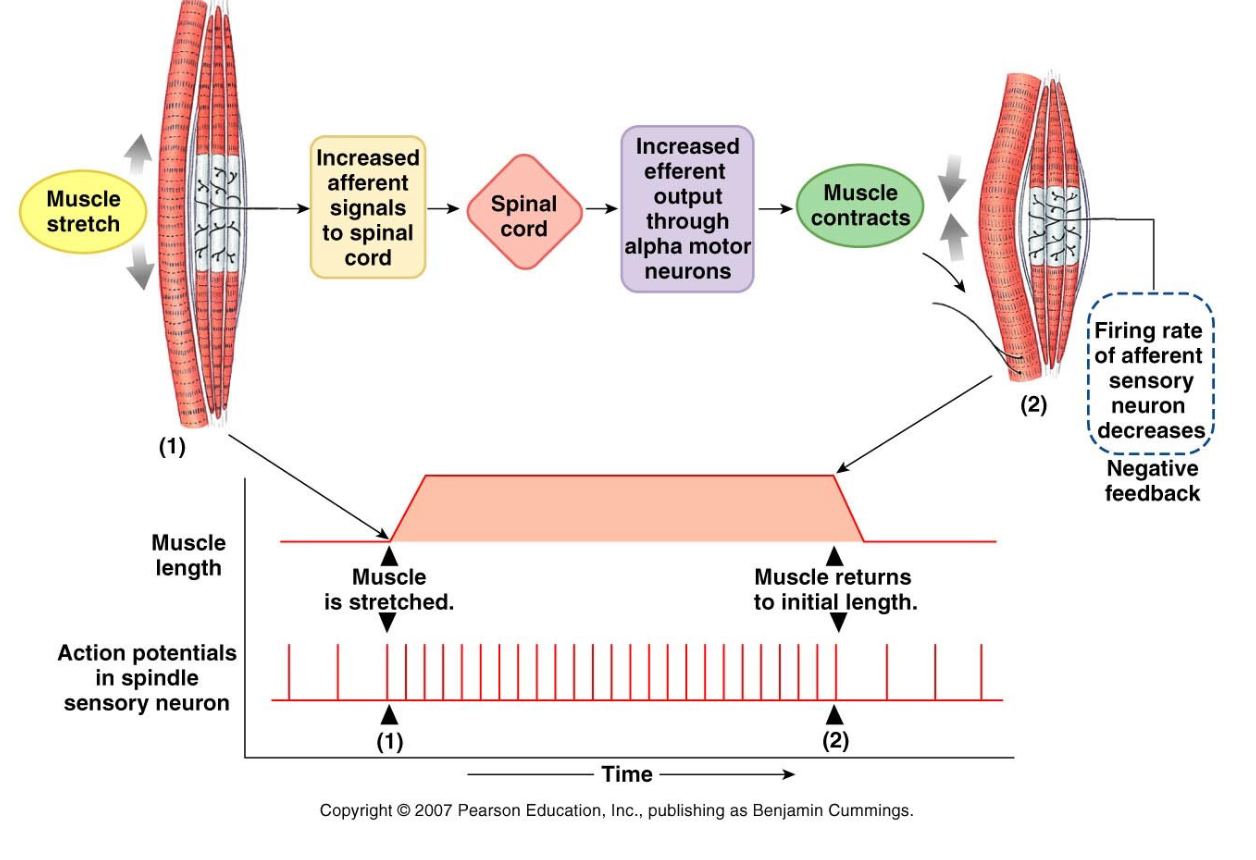
how does muscle stretch trigger a stretch reflex?
1) muscle stretch
2) increased afferent signals to spinal cord
3) increased efferent output through alpha motor neurons causing muscle contraction
firing rate of afferent sensory neuron decreases causing negative feedback
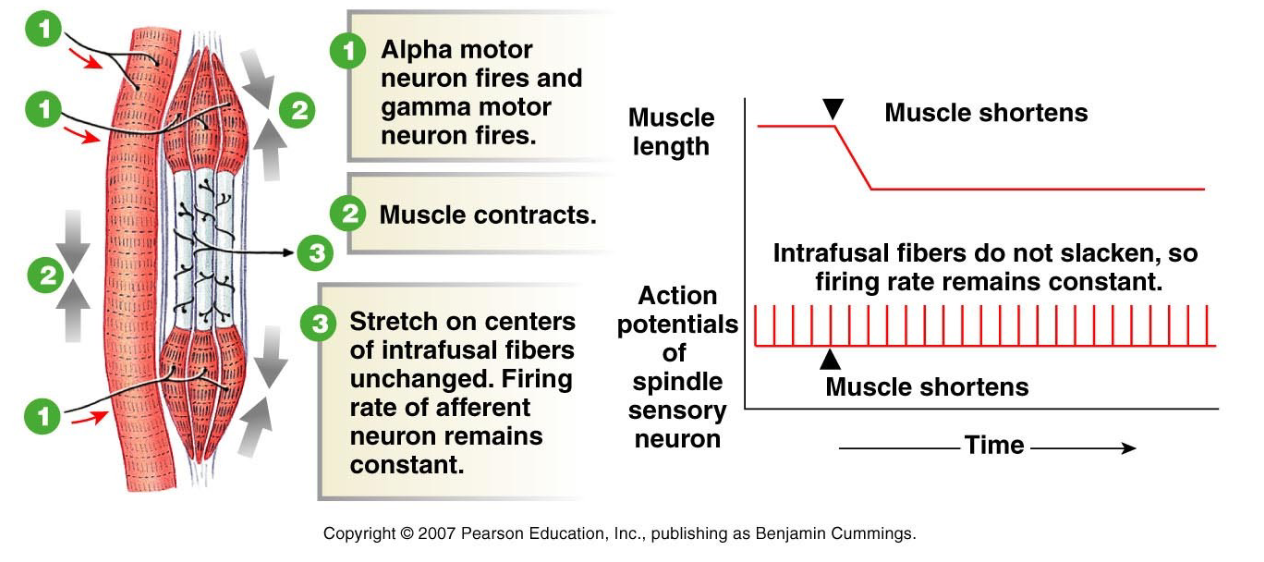
How does alpha-gamma coactivation maintain spindle function during contraction?
1) alpha motor neuron fires and gamma motor neuron fires
2) muscle contracts
3) stretch on centres of intrafusal fibres are unchanged, firing rate of afferent neuron remains constant
ESSENTIAL for maintaining sensitivity of muscle spindle
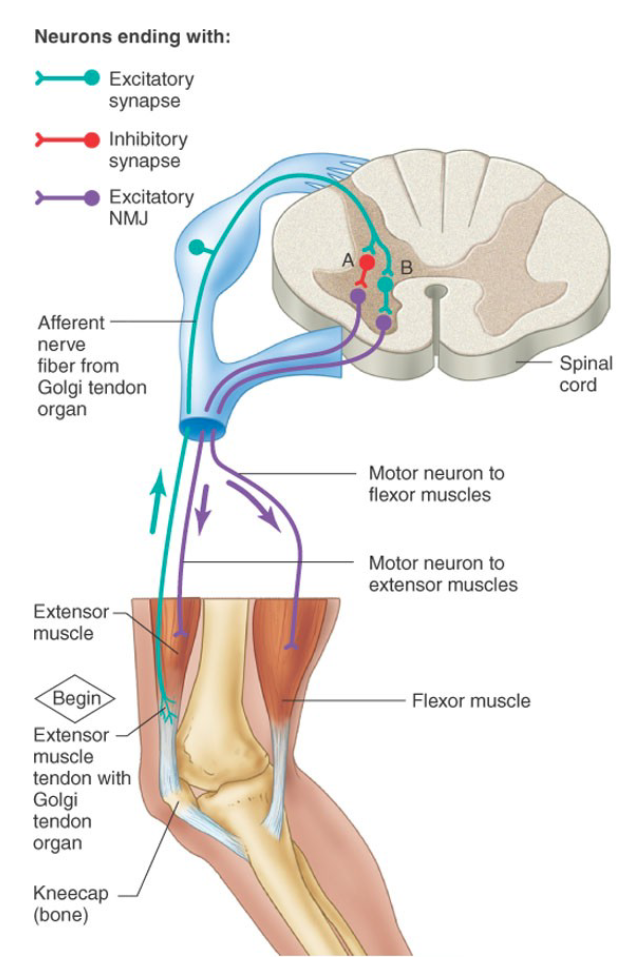
What is the golgi tendon organ?
sensory receptor located at the junction between a muscle and its tendon, detects tension in tendon produced by muscle contraction
NO MOTOR INNERVATION
high threshold response -increases IPSPs (inhibitory) on alpha motor neurons that causes reduction in muscle contraction AND excitation in the opposing flexor’s motor neurons
During normal locomotion, input excites rather than inhibits motoneurons and affects the timing of transitions between the stance and swing phases of locomotion
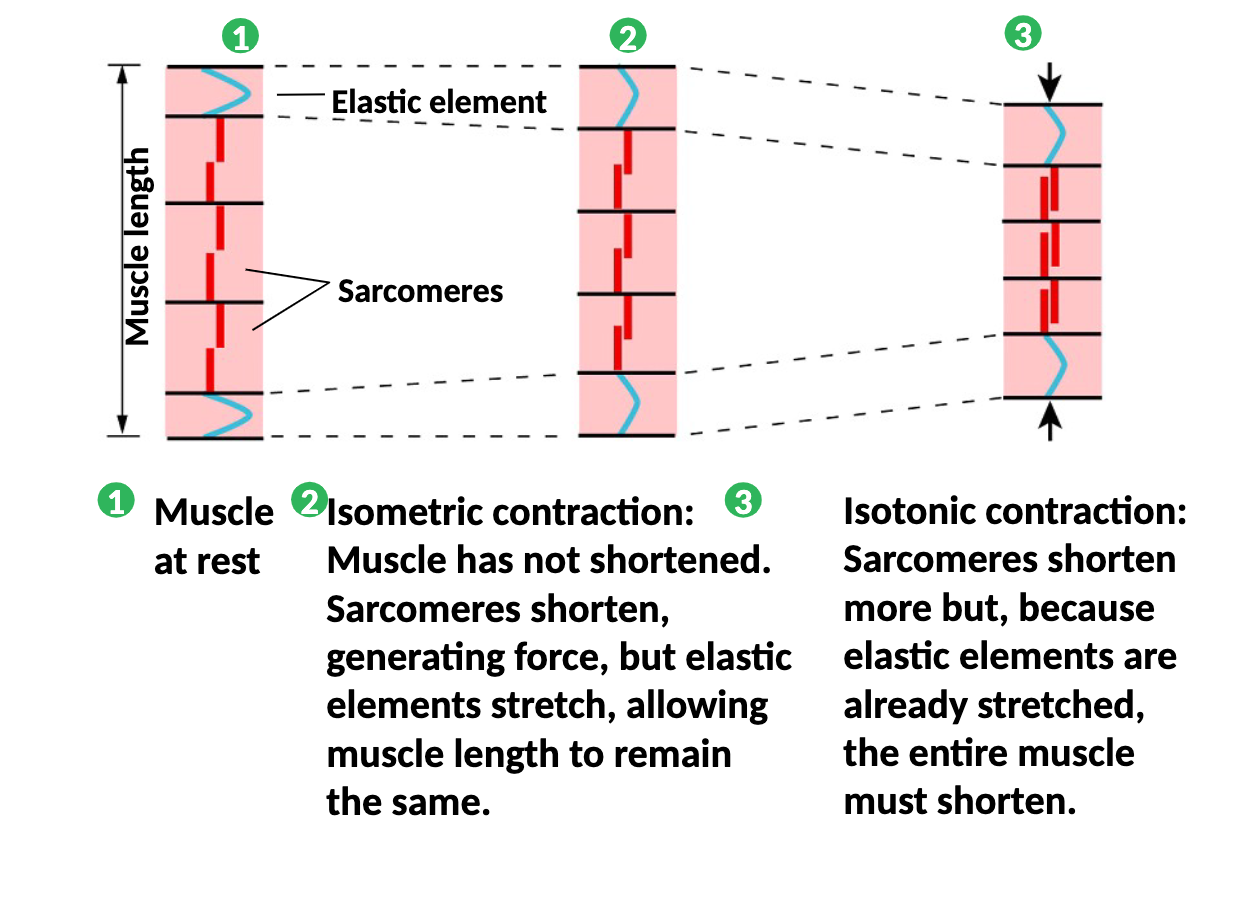
What is the difference between isometric and isotonic muscle contraction?
Isometric contraction - muscle has NOT shortened, sarcomeres shorten generating force but elastic elements stretch allowing muscle length to remain the same
Isotonic contraction - sarcomeres shorten more but becasue elastic elements are already stretch the entire muscle must shorten
what is the only neurotransmitter and what type of receptors does it bind to?
Acetylcholine (Ach), the post synaptic receptors are nicotinic receptors
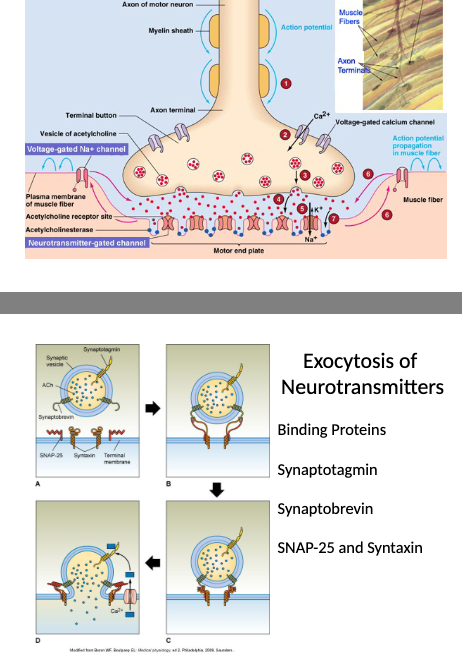
What are the basic steps to a signal moving through the neuromuscular junction?
1) action potential runs dow the motor neuron and reaches the axon terminal
2) the action potential causes the opening of Ca2+ voltage gated channels allowing the influx of calcium, presynaptic ACh filled vesicles line up at active zones
3) vesicle exocytosis - The binding proteins Synaptobrevin on the vesicle intertwine with binding proteins located on the inside of the terminal membrane , SNAP-25 and Syntaxin, to dock the vesicle at the membrane. The calcium binds to other vesicle bound protein synaptotagmin, and results in the fusion of the vesicle and terminal membranes and releases ACh into the synaptic cleft by exocytosis
4) ACh binds to nicotinic receptors on the postsynaptic muscle fibre
What happens to acetylcholine?
normally very rapidly broken down in the synaptic cleft or in the plasma/body by acetylcholine esterase (AChE) into choline and acetic acid
Choline CAN be reused
what are some clinical uses of neuromuscular blockers in vet med?
used in anaesthesia to achieve muscle relaxation, orthopedics, repair diaphragmatic hernia, delicate intra-ocular procedures (still eye), facilitate intra-tracheal intubation in large animals, hypoxemic animals resisting mechanical ventilation, capture of certain exotic animals
what are neuromusclular blockers and what do they do?
structural analogues of ACh that bind nicotinic receptors on motor end plate, two types of blockers:
1) Non-depolarising blockers - prevent ACh binding to motor end plate, competitive antagonists (ie: Tubocurarine, atracurium)
2) Depolarusing muscle relaxants - bind to ACh receptor and cause an initial depolarization (ie: succinylcholine)
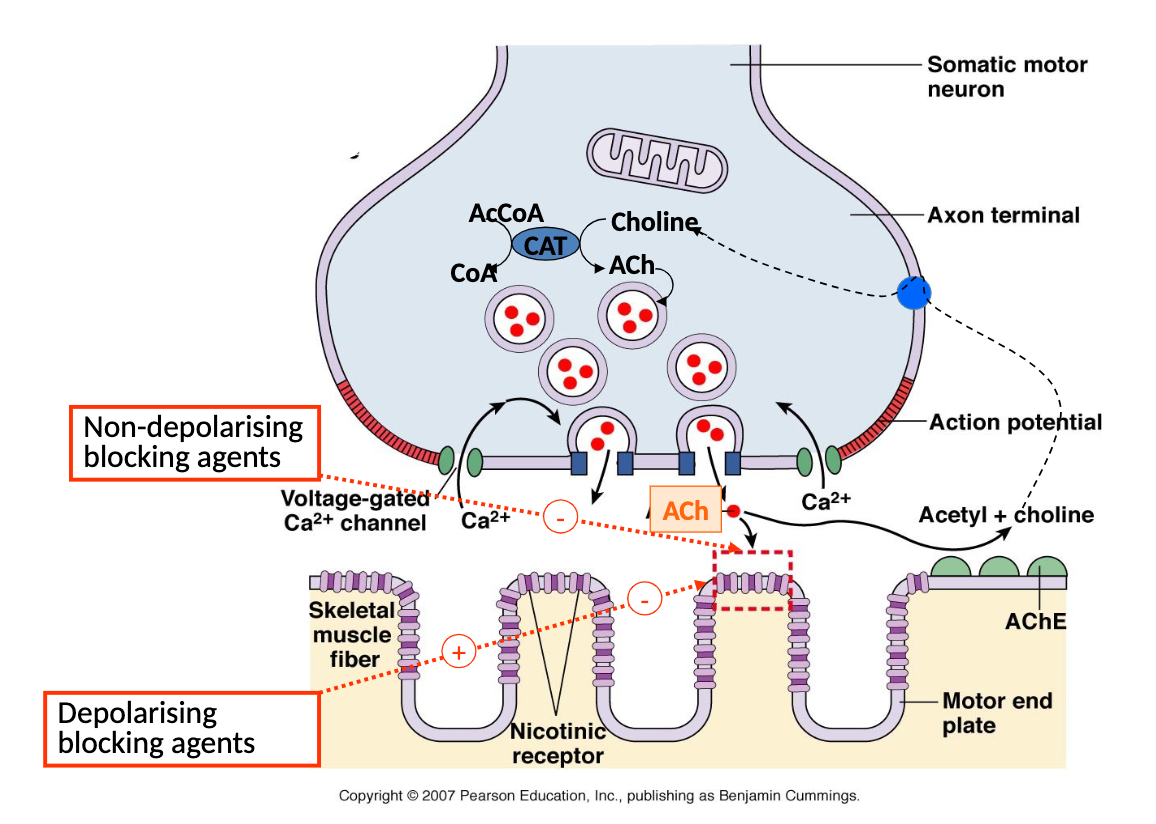
What is tubocurarine and how does it work?
non depolarizing muscle relaxer, prevents influx of sodium through nicotinic receptor operated channel, administered intravenously
low dose - competes with ACh binding at skeletal muscle and prevents muscle contraction, block requires 95% receptor occupancy
high dose - direct interference with sodium channel, becomes non-competitive and insensitive to ACh concentration
What is succinylcholine and how does it work?
ONLY depolarizing muscle relaxer used clinically, made of 2 back-to-back ACh molecules, acts like Ach at nicotinic receptor except its effect persists for longer, sensitive to plasma acetylcholine esterase
Safety issues (lots of risks) and lack of antagonists (reversal agents)
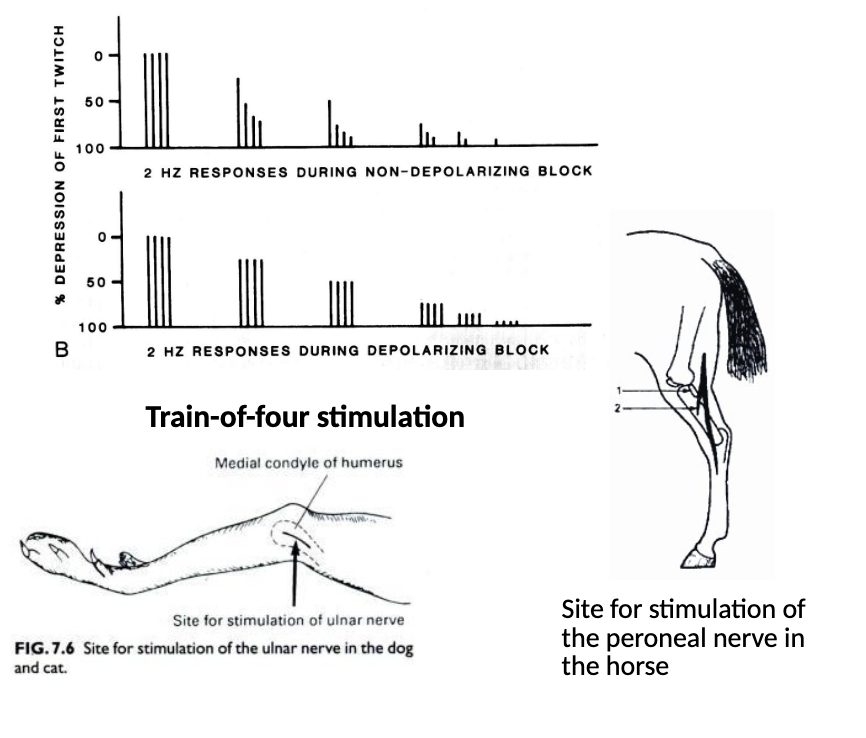
How would you monitor a neuromuscular junction blockade?
impossible to accurately predict depth of blockage in any animal due to large variability in onset times, duration, and depth
monitor by using a Medistim (dogs - ulnar nerve, horse - facial or peroneal nerve)
What are anti-cholinesterases (AKA cholinesterase inhibitors)?
indirectly acting cholinomimetics (anti-AChE, anti ChE)
ACh accumulates at synapse if AChE action is blocked
AChE inhibitors indirectly affect muscarinic and/or nicotinic receptor actions, most commonly used AChE inhibitors DO NOT PASS THE BLOOD BRAIN BARRIER (except physostigmine)
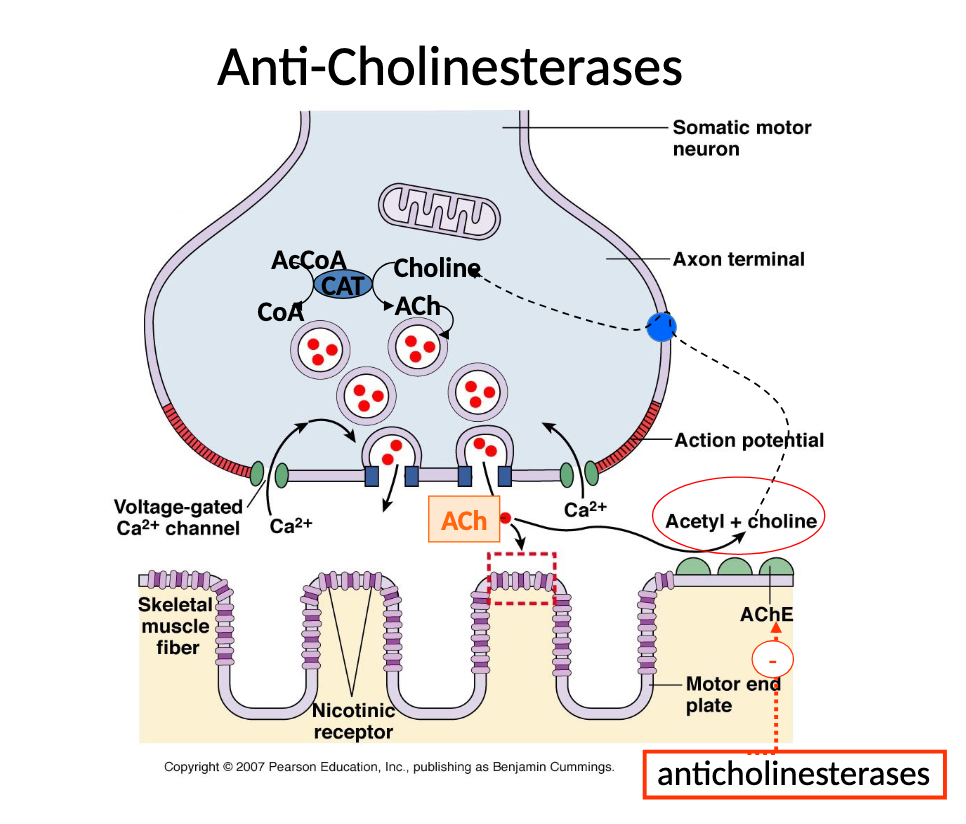
What are some common uses of Cholinesterase inhibitors?
Glaucoma (ectothiophate, demecarium), insecticides (flea collars), reversal of neuromuscular block (neostigmine, edrophonium, pyridostigmine bromide), Myasthenia Gravis (diagnosis and treatment)
What is myasthenia gravis and what is the treatment?
auto-immune disease of the neuromuscular junction where there is a reduction in the number of nicotinic receptors, can be aquired or congenital (rare), diagnose and treat with cholinesterase inhibitors
Tx: requires long acting AChE inhibitor - Pyridostigmine bromide (Mestinon)
What are irreversible AChE inhibitors?
organophosphates - bind AChE covalently and non-competitively, found in nerve gas, insecticides, herbicides, lice and flea treatments, sheep dip
Toxicity = saliva lacrimal urination defection (SLUD) and convulsions
What are lower and upper motor neuron organization?
upper motor neurons - stay in CNS adn control lower motor neurons
lower alpha motor neurons - exit CNS (ventral horn)and innervate skeletal muscles
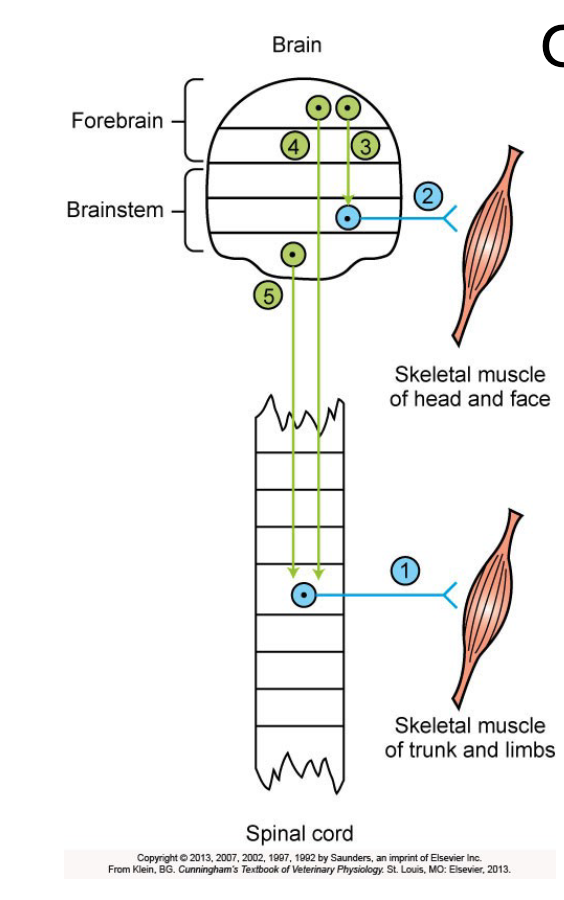
What are signs of lesions of lower motor neurons?
stereotypical clinical signs: paralysis (paresis/flaccid), atrophy (shrinking of skeletal muscle), loss of segmental and intersegmental reflexes, electromyograph (EMG) changes
What are signs of lesions of upper motor neurons?
movement disorders (seizures, rigidity, circling gaits, inappropriate movements), NO atrophy, retained but exaggerated segmental reflexes (hyperreflexia), electromyograph (EMG) is normal (eg. Schiff-Sherrington posture)
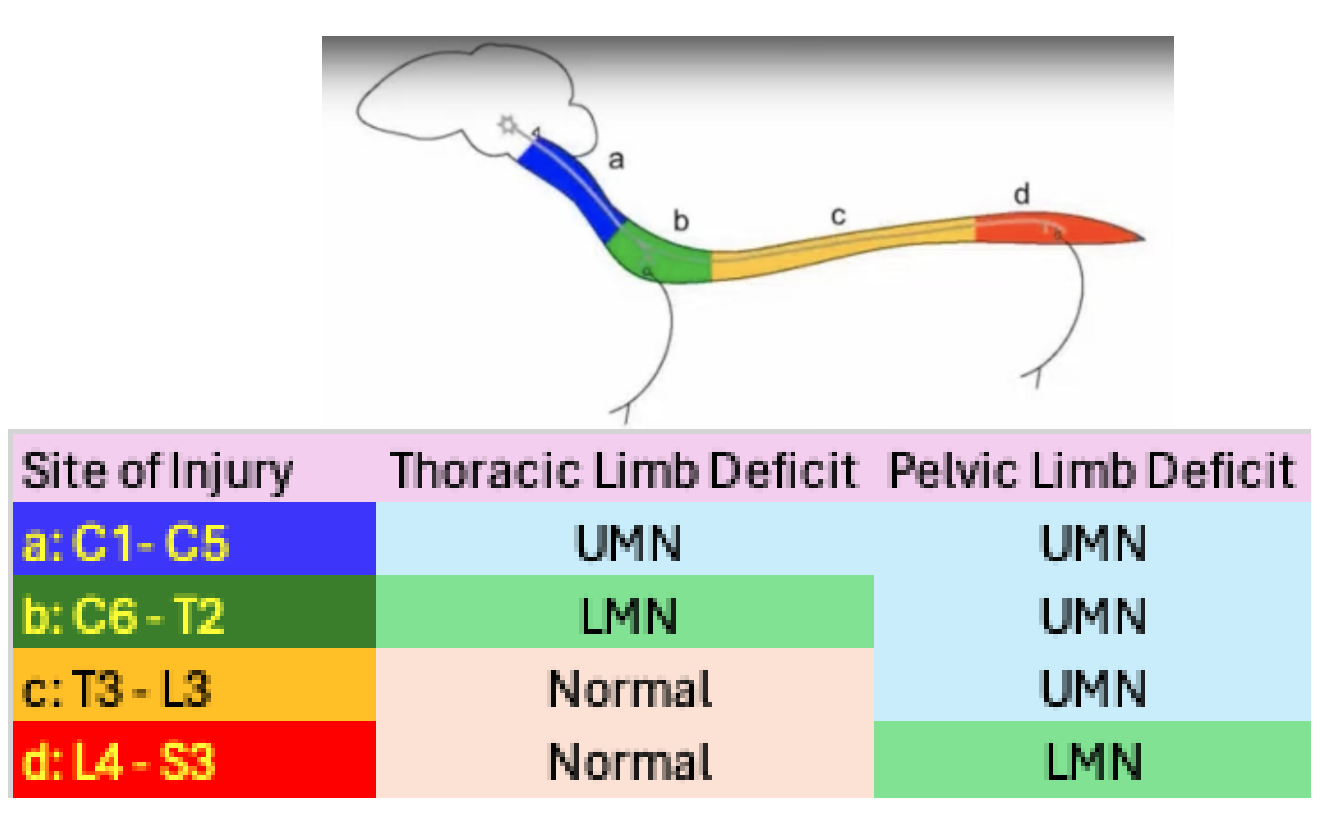
how can you localize the area of the spinal cord that is affected in a upper/lower motor lesion? (in dogs)
look at this table and the link: Two Dogs Unable to Walk But Very Different Localizations || Lower vs. Upper Motor Neuron Lesions
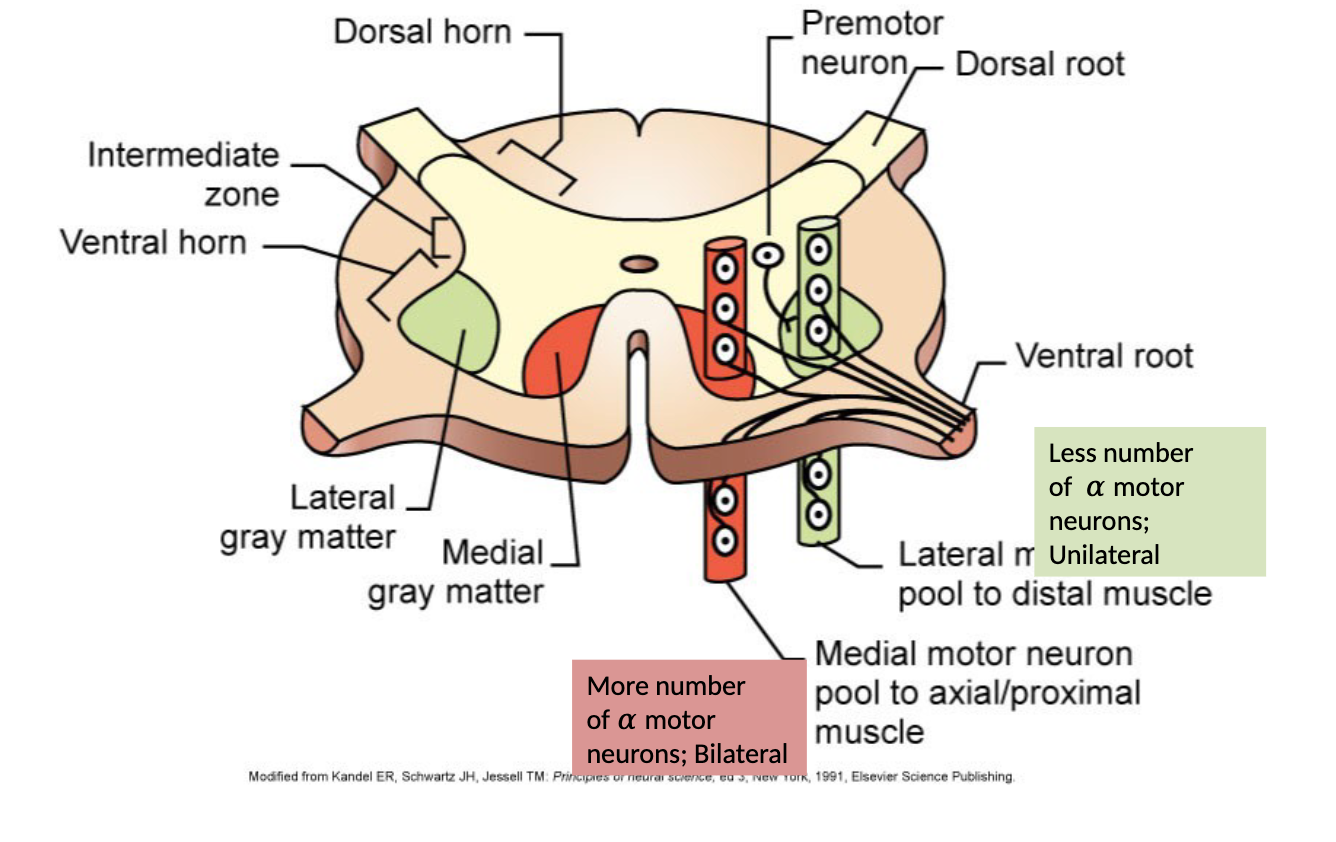
what are the difference between learned and postural movement?
1) learned - voluntary, conscious, skilled, usually mediated by FLEXOR muscles, discrete contraction of few muscle groups usually distal to spinal column, LATERAL grey matter, less number of alpha motor neurons unilaterally
2) postural -anti-gravity muscle tone, involuntary, largely subconscious, mediated by EXTENSOR muscles, maintenace of posture (longer term contraction of larger muscle groups), often closer to spinal column, MEDIAL grey matter, more number of alpha motor neurons bilaterally
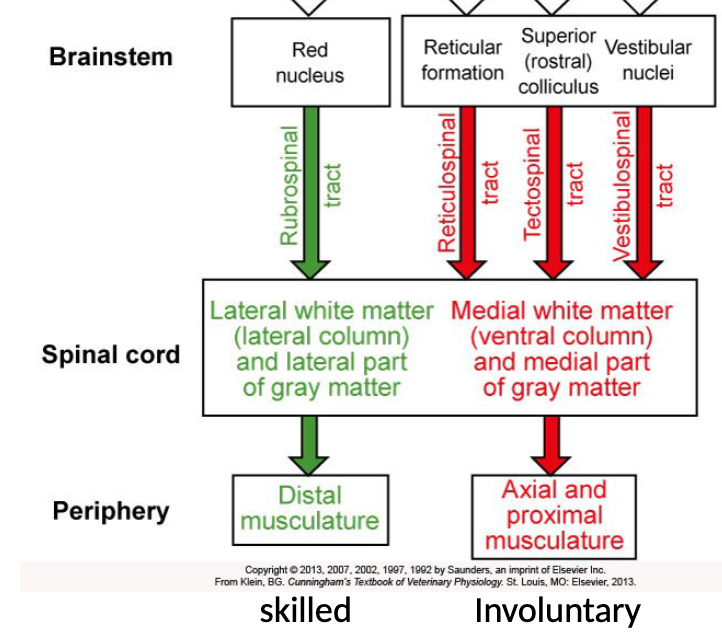
What are the medial and lateral brainstem pathways and what do they do?
1) Reticulospinal, vestibulospinal (involuntary) - most important pathways for maintaining an upright posture
2) tectospinal (involuntary) - principally involved in reflex orientation of the head
3) rubrospinal - involved in skill, manipulative movements of the extrimities
What is the corticospinal/pyramidal tract?
used for elborate and dexterous voluntary movement, tracts:
lateral corticospinal - control the distal limb musculature (75-90%)
ventral corticospinal - control axial and promimal musculatore (10-25%)
In humans the pyramidal system is well developed but in vet species its not well developed and lesions often cause postural response deficits in contralateral limbs and minor alterations to gait
What is the basal ganglia and why is it so important?
it’s a network of different nuclei in the cerebral hemisphere with many different neurotransmitters (mainly ACh, GABA, and dopamine) with an overall effect on the thalamus being INHIBITORY
“brake hypothesis” - to sit still you brake all movements except postural reflexes, to move you brake some postural reflexes
Deficits - presence of extra unwanted movements OR absence/difficulty with intended movements
What happens when there are basal ganglia lesions?
input to basal ganglia diminished and the looping circuit between the basal ganglia, thalamus and sensorimotor cortex is disrupted
results in reduced movement, slow movement, musculature rigidity, tremor at rest → Parkinson’s disease
What are the two main CNS regions involved in planning and execution of movement?
basal ganglia and cerebellum
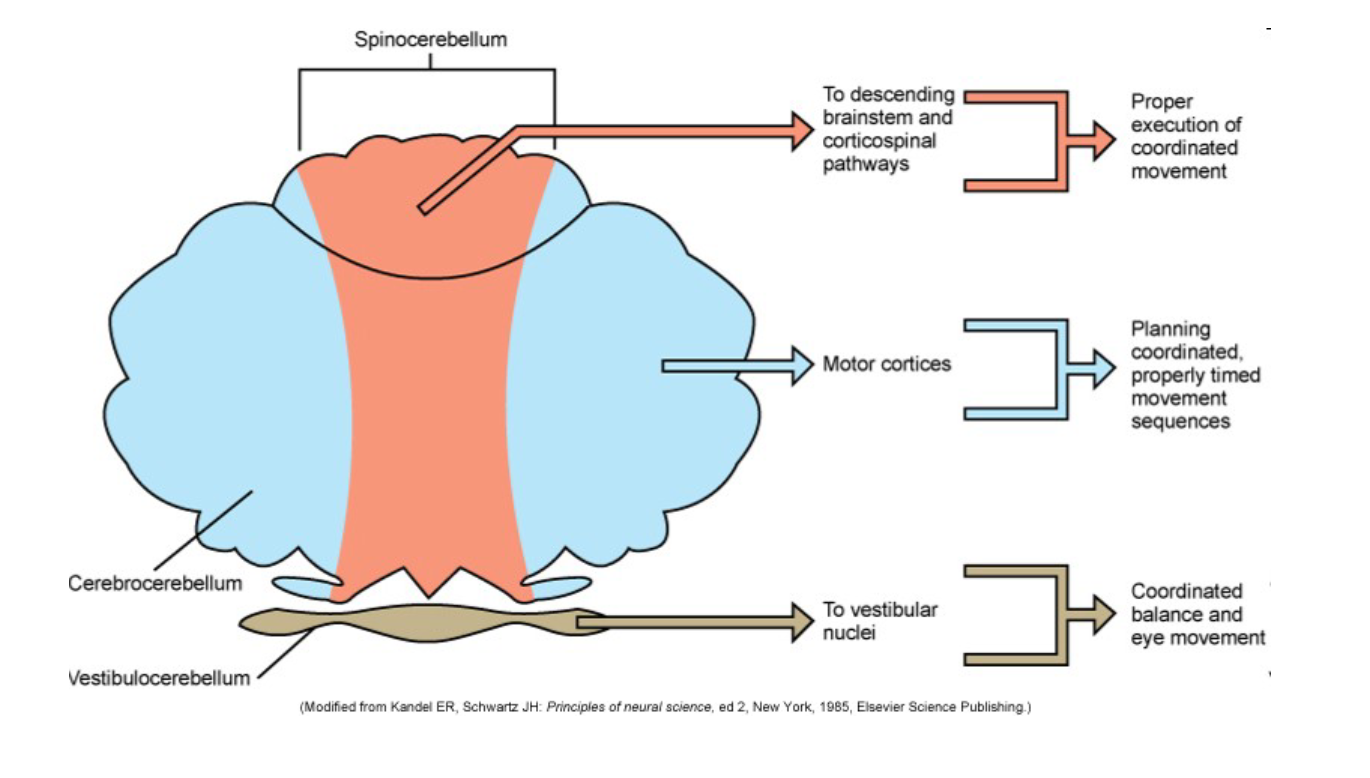
What does the cerebellum influence/do?
1) influences posture and movement indirectly, recieves information from sensorimotor cortex from vestibular system, eyes, ears, skin, joints, and tendons, gives output to all brainstem motor pathways
2) Provides ‘timing’ for precision of execution of movement
3) participated in planning of movement
4) corrects errors in on-going movement
what are the three distinct regions and outputs of the cerebellum?
1) spinocerebellum - proper execution of coordinated movement
2) Cerebrocerebellum - planning coordinated, properly timed movement sequences
3) Vestibulocerebellum - coordinated balance and eye movement
What are some diseases of the cerebellum and their clinical signs?
viral induced feline panleucopenia, BVD, hereditary cerebellar diseases, occipital dysplasia, infectious disease, demyelination disease
typical sign = intention tremor (intended movements performed with distinct tremor BUT no tremor at rest)
other typical sign = ataxia (unstable posture and awkward gait)
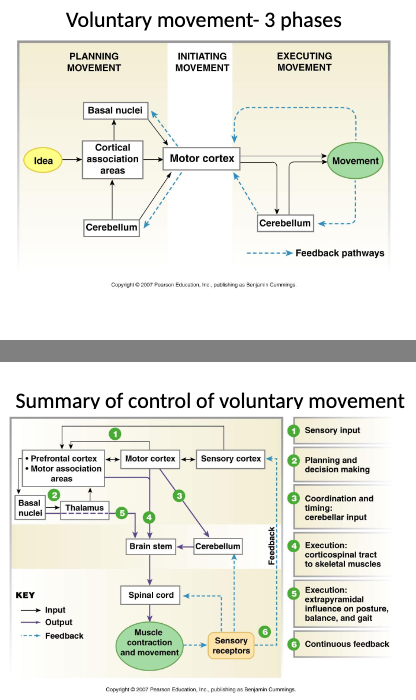
What are three three phases of voluntary movement?
1) planning movement - sensory input
2) initiating movement - planning and decision making, coordination and timing (cerebellar input)
3) executing movement - execution through corticospinal tract to skeletal muscles, execution through extrapyramidal influence on posture, balance, and gait
feedback in continuous
What is a SNP and how do they relate to performance?
SNP = single nucleotide polymorphisms
at a SNP locus different variants are present that can gave different effects on performance
How has genomic technology been harnessed for animals?
1) improving performance - food animal performance, athletic performance (speed in racehorses)
2) disease prediction - allows genetic rather than phenotypic selection of desirable traits, sequence-based genetic tests for specific loci (eg. scrapie resistance in sheep) AND/or whole genome sequencing or multi-locus testing for complex resistant traits (eg. Bovine tuberculosis resistance)
What is the performance example of genomic technology being used on animals?
Myostatin gene - negative regulator of muscle mass development
1) food animals - inhibition of myostatin = more muscling (double muscling) causing increased meat yield, leaner carcasses, and improved meat tenderness, can also have negative effects on calving difficulty, milk production, and female fertility
2) athletic animals - differences in myostatin SNP used to predict race distance in horses, C:C are short distance runners, C:T are middle distance runners, T:T are middle/long distance runners
What are the disease example of genomic technology being used on animals?
1) scrapie resistance - polymorphisms at 3 loci on PRNP gene for CLASSICAL scrapie: ARR/ARR genotype is most resistant and VRQ/VRQ are most susceptible, animals most resistant to classical are more susceptible to ATYPICAL scrapie
2) tuberculosis resistance in cattle - multi-SNP, many genes govern susceptibility to TB in cattle, greater difficulty in selecting animals for resistant phenotype BUT one paper said could be possible for Holstein breed
What is physical therapy?
treatment of physical dysfunction or injury using therapeutic exercise and modalities intended to restore or facilitate normal function or development (aka physiotherapy)
how many muscles are in the dog?
around 640 muscles, 40% of total body weight
What is the purpose of the connecting tissue surrounding muscular tissue?
1) subcutaneous/hypodermis composed of: areolar tissue- fibroblasts and collagen, adipose tissue - stores tryglycerades, insulates reducing heat loss and protechs muscles from trauma
provides pathway fro nerved, blood vessels and lyphatics to enter and exit muscles, separates muscle from skin, protection
2) fascia - dense sheet or broad band of CT that lines body wall and limbs, supports and surrounds muscles and organs, holds muscles with similar functiosn together, allows free movement of muscles, carries nerves, blood vessels and lymph, fills space between muscles, VERY IMPORTANT IN PHYIOSTHERAPY (myofacial work)
WHat do mechanoreceptors in skeletal muscle do?
sense changes in joint movement, muscle tension, and muscle length, send information to CNS which response with muscle contraction or inhibition of muscle contraction
What are muscle spindles?
small elongated structures scattered among the contractile extrafusal muscle fibre, respond to muscle stretch and responsible for muscle tone
What and where are joint receptors?
found in capsule and ligaments around every joint, stimulated by mechanical distortion that accompanies changes in the relative position ing of bones linked by flexible joints
what are the different classifications of movement?
1) reflex movements- lest complex, integrated primarily in spinal cord
2) postural reflexes - integrated in brain stem, require continuous sensory input from visual and vestibular sensory systems
3) voluntary movements - most complex, integrated at cerebral cortex, initiated at will without external stimuli
4) rhythmic movements - combination of reflex movements and voluntary movements (ie: walking, running), initiated and terminated by input of cerebral cortex but once initiated can be sustained without further input from brain
What are some methods and techniques for physiotherapy?
1) manual - massage, passive range of motion (PROM), MET, Mobs
2) Therapeutic exercise - stretching, assisted exercise (sling/towel), active assisted exercise (slow walk, stair/incline, pole weaving, etc.)
3) Thermotherapy - used to heat or cool body, superficial heat (local and large areas), cryotherapy (ice and commercial packs)
4) Electrotherapy
5) Hydrotherapy - water therapy, hot, cold, steam, ice, treadmill vs free swimming
What are the 3 tissue healing phases that help decide when to do physiotherapy?
1) Acute phase - early (acute): inflammatory response for 2-4 days, late (subacute): continue inflammatory phase and completed in 2 weeks, protect rest ice compression and elevation (PRICE)
2) Tissue formation (proliferation) - rebuilding takes 2-3 weeks, does not include chronic inflammation, increase ROM, restore or increase strength, reestablish neuromuscular control
3) Remodeling phase - adapt to original tissue, continues for up to 1 year post injury, ultimate goal of returning to activity, continued collagen realignment
What is conformation?
physical appearance and outline of a horse as dictated primarily by bone and muscle structures, varies according to purpose of horse
what is soundness?
horse is free of lameness and is suitable for a particular purpose (racing, jumping, etc.), important to differentiate ‘blemishes’ from ‘unsoundness’ - blemishes are scares or irregularities that have no effect on serviceability of horse BUT unsoundness causes a horse to be lame or otherwise unserviceable
Does poor conformation mean unsoundness?
no, but poor conformation can lead to lameness (see overgrown foot as example) and good conformation does not guarantee good performance
Does the dam or sire contribute more to faulty conformation?
Dam may contribute more - fillies with faulty conformation may be retired for breeding if they develop lameness BUT most stallions are proven performers with good conformation
What are some heritable conditions relating to bad conformation?
toeing in and toeing out, back-at-the-knee, offset knee, tied in below the knee, sickle hock, and straight behind
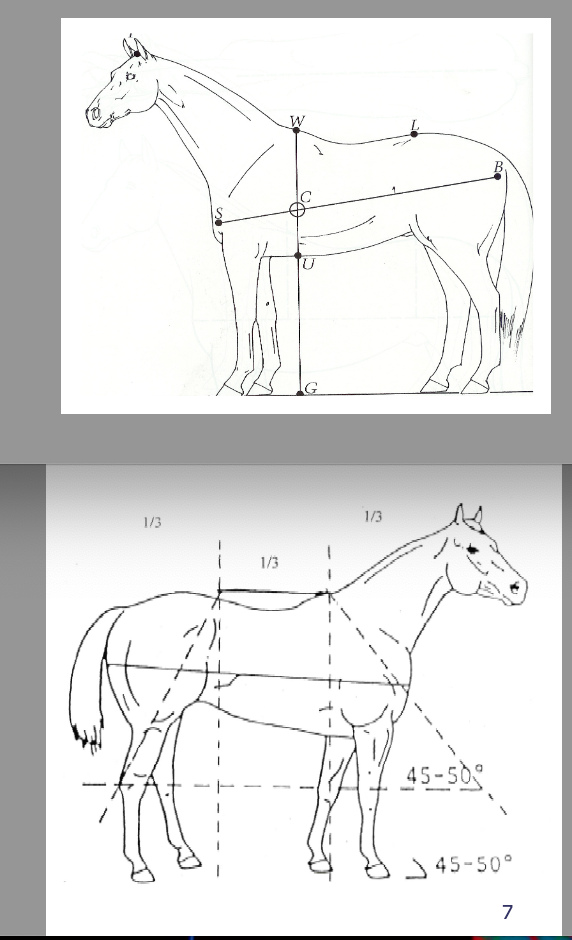
What are the 4 main components to conformation analysis?
1) Balance - relationship between forehand and hindquarter, between limbs of body, and between left and right halves of body
2) Assessment of lengths, angles, and heights
3) Muscling
4) Limb Conformation
What are the components to balance in a conformation analysis?
relationship between forehand and hindquarter, between limbs of body, and between left and right halves of body
Horse can be divided in 3 equal parts (length) = front (muzzle to girth), middle (girth to rear flank), hind (rear flank to tuber ischii)
1) body length (shoulder to tuber ischii) should be equal or slightly longer than withers height
2) withers height should be same as rump height
3) centre of gravity located at intersection of vertical line dropped from withers and line drawn from shoulder to tuber ischii
what is the result have having a short or long back in the horse?
short = horse may have short strides which may cause interference
long = horse may have trouble engaging the hind limbs
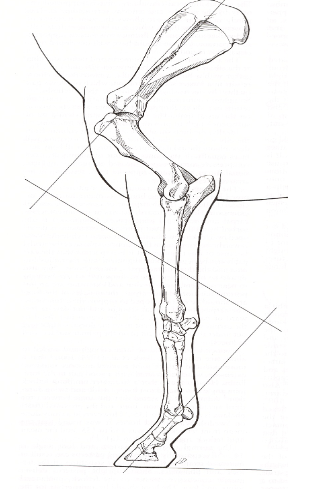
What are the components to length, angles, and heights in a conformation analysis?
line down the scapula should be at the same angle as the pasterns
1) Shoulder length and angle are related to stride length - long sloping shoulders = long strides
2) ideal shoulder angle is 45 degrees, with steep shoulders (ie. >50 degrees) you can see upright pasterns
3) ways long strides can be produced = long radius and short metacarpus, long gaskin and short metatarsus, flat and long rump
4) short steep rump (goose rump) predisposes to hindlimb lameness
5) taller behind than front predisposes to forelimb lameness
What are some specific conformation faults of the forelimbs?
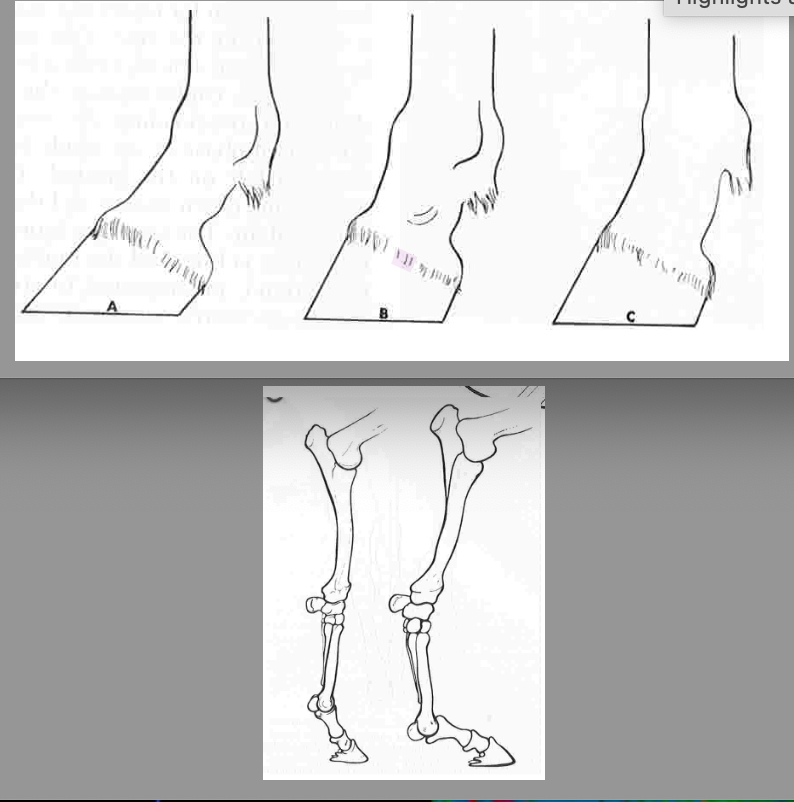
1) upright pasterns - shorter the pastern angle = shorter stride, angle usually similar to angle of shoulder (48-55 degrees), increases concussion on fetlock and other joints, affected horses are prone to navicular disease and ringbone, risk of fetlock effusion increases with increased dorsal hoof angle
2) long sloping pasterns - pastern appears too long for length of limb, predisposes to injury of flexor tendons, sesamoid bones, and suspensory ligament, osteoarthritis of the fetlock, and fractures in P1
What are the components to muscling in a conformation analysis?
muscles are powerhouse and add support to skeleton and joints, length, thickness and distribution of each muscle group vary with age and sport activity, aim for symmetry
What are the components to limb conformation in a conformation analysis?
Ideal conformation front to rear = when view directly from front or back plumb line dropped from shoulder or tuber ischii divides the leg in 2 symmetrically
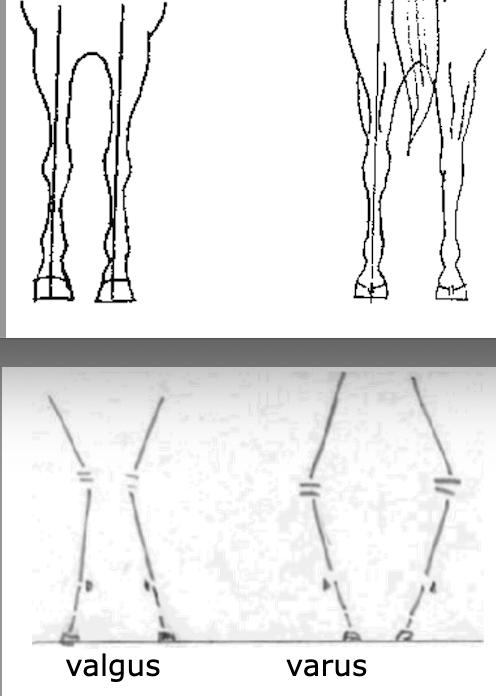
observe 2 main characteristics: 1) Base (wide/narrow), 2) Limb Axis (straight, outward turning=valgus deformity, inward turning=varus deformity)
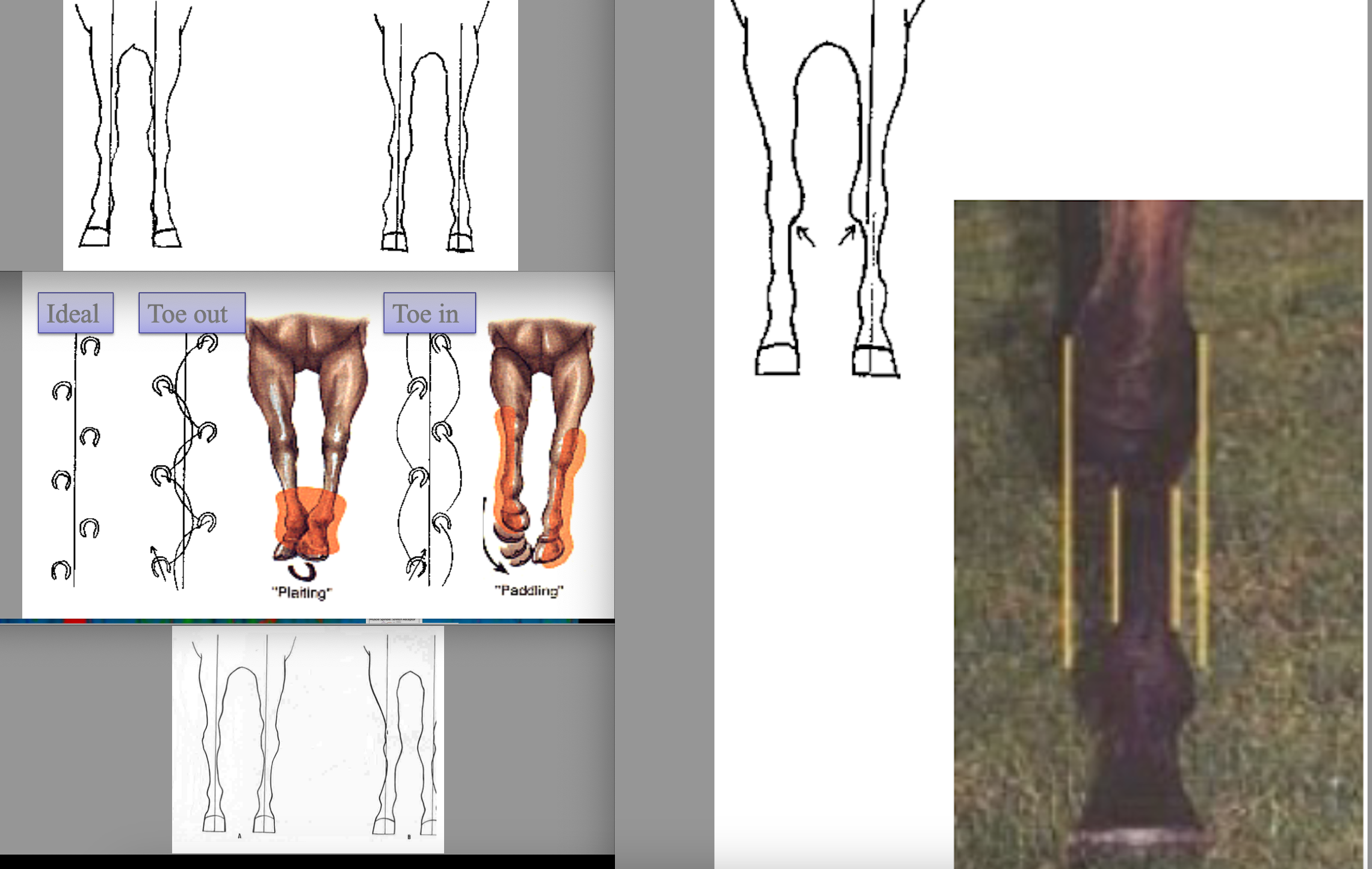
What are some “front the front” deviations from ideal leg conformation?
1) Base deviations - base wide=inside foot is weight bearing, base narrow=outside foot is weight bearing
2) Toe deviations - toe out (splay footed) and toe in (pigeon toed)
toe direction influences how the foot moves and lands - toe out swings inwards (plaiting) and tow out swings outward (paddling)
3) Knee deviations - out at the knee=bow legged, most affected are also toe in, in at the knee=may predispose to splints
4) Bench knee/offset knee - MCIII offset, medial aspect of joint bears abnormal weight and joint is no longer balanced
What is the definition of angular limb deformity?
deviation of the limb from its normal axis in the frontal plane, poorly understood but likely multifactorial, can be congenital or acquired
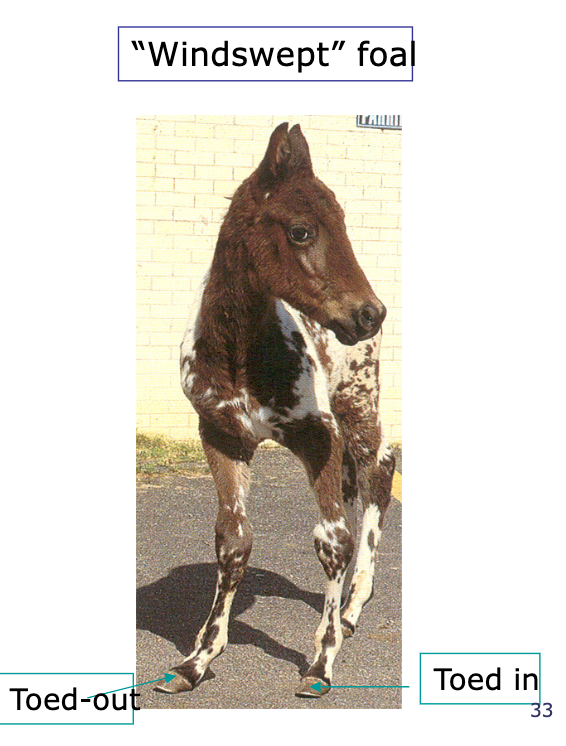
1) valgus - lateral deviation of limb distal to location of deformity, often also splay footed or toed out
2) varus - medial deviation of limb distal to location of deformity, also often pigeon toed
most common site of angular limb deformity is the CARPUS (also seen in fetlocks and tarsus)
What is a windswept foal?
valgus and varus deformities with both rotational deviation
what are some congenital forms/reasons of angular limb deformity?
1) malformation in utero
2) laxity of collateral ligaments of carpus - tissues not strong enough to support carpus in newborns, improves when muscle tone increases
3) hypolasia of cuboidal carpal bones - defective/incomplete ossification
what are some aquired forms/reasons of angular limb deformity?
1) foal born with straight limb but develops angulation - asynchronous growth of limb due to asymmetrical loading of growth plate (trauma, rapid growth due to over nutrition, mineral imbalances)
What are treatment options to angular limb deformity in a foal?
4 main options:
1) confinement and altered nutrition
2) splints, braces, casts
3) surgical growth retardation
4) surgical growth stimulation/acceleration
sometimes in minor cases treatment may not be necessary as it will correct within first week of life
What is the timing for growth plate closures?
1) distal metacarpus/tarsus = 3-6 months, rapid growth peak around 6 weeks
2) distal radius and tibia = 2 years, rapid growth peak around 3-4 months
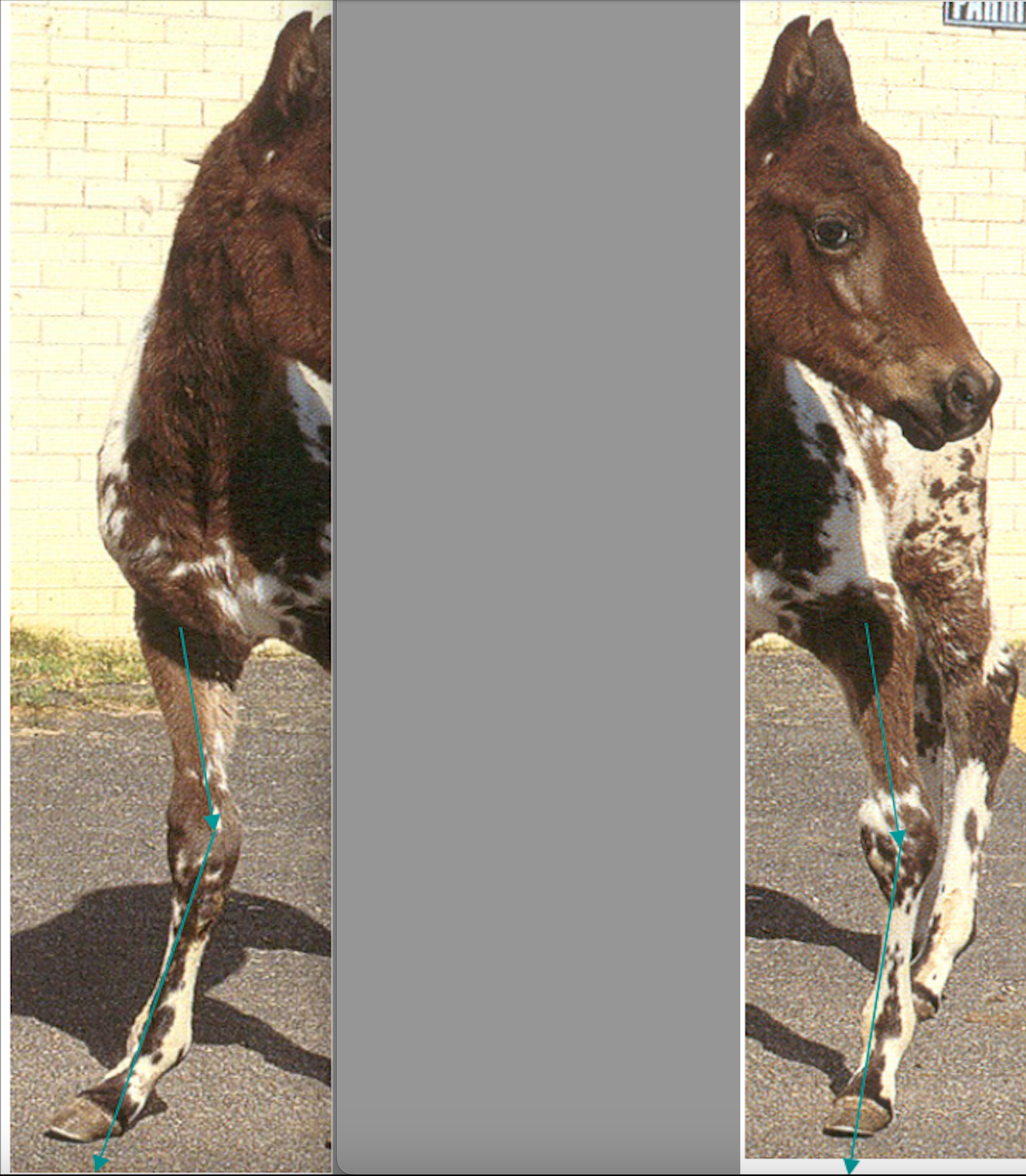
What are rotational deformities in the limb?
temporary rotation of the limb from the elbow is not uncommon in narrow chested foals and will self correct as the chest widens
permanent rotation develops when a bone is abnormally loading in both frontal and sagittal planes leading to rotation of the limb around the overloaded axis point
identified by: radiology, clinical observation at rest, and clinical observation at exercise
What are treatment options to rotational deformities in the limb?
no clear guidelines available, care is needed with manipulation of foot balance in young foal (<6 weeks); abnormal loading of growth plates could lead to additional deformities particularly in the fetlock
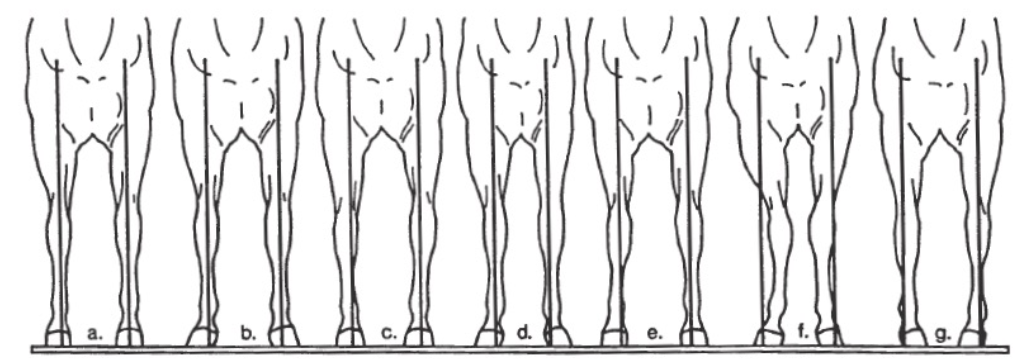
Label this image
a) ideal
b) base wide and toed-out (splay footed)
c) carpal varus (bow kneed)
d) base narrow and toed-out
e) bench knee
f) carpal valgus (knock knee)
g) toed-in (pigeon toed)
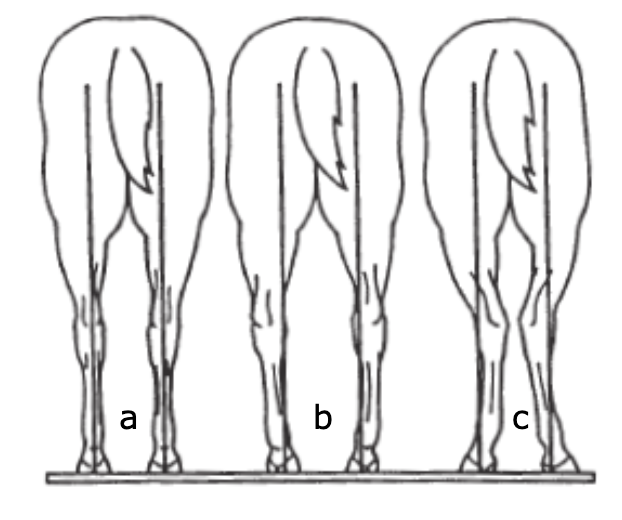
label this image
a) ideal
b) tarsus varus (bow leg)
c) tarsus valgus (cow hock)
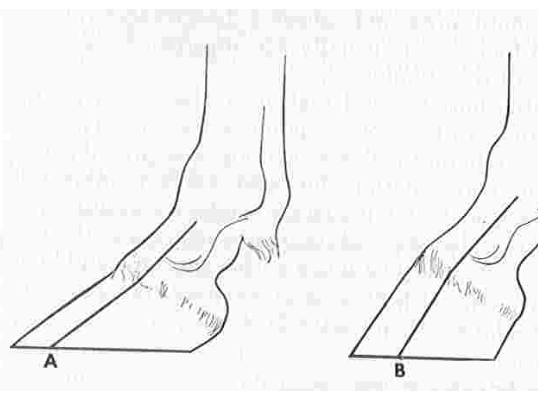
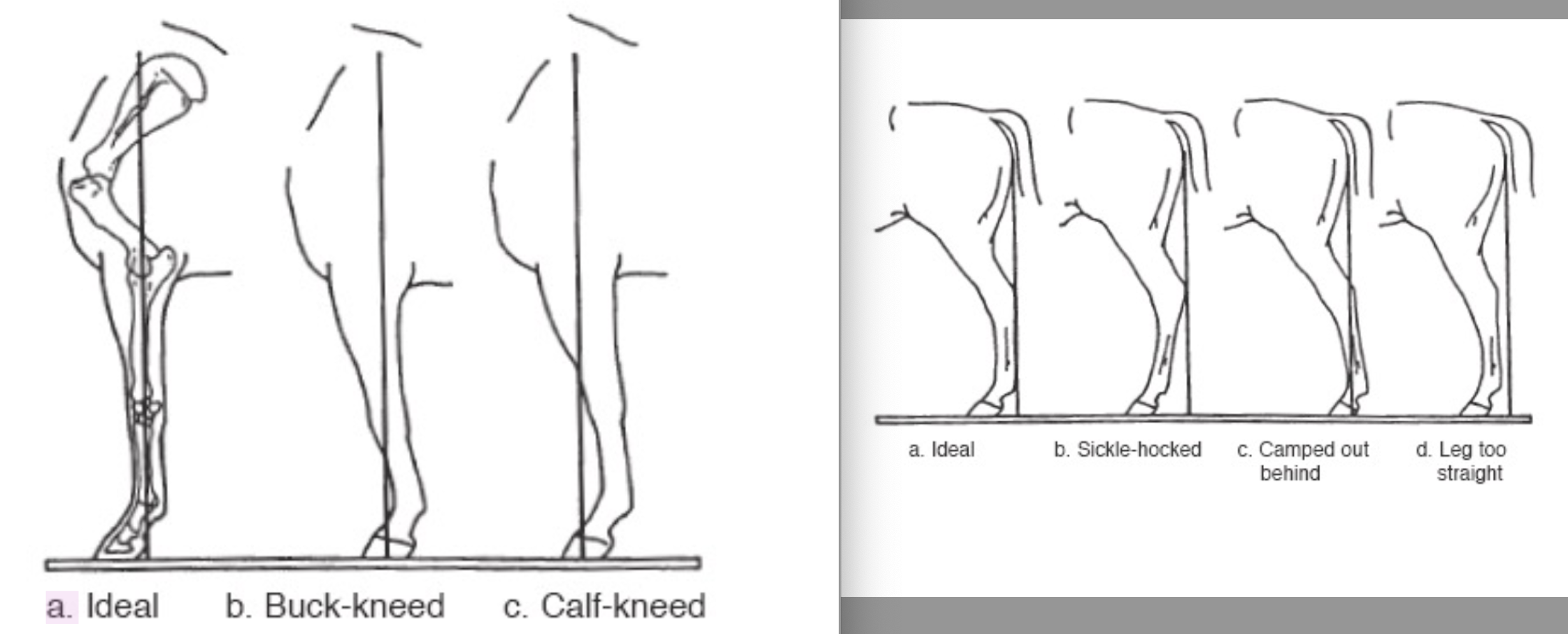
What is ideal conformation from the side?
Forelimb: line bisecting the elbow joint, carpus and fetlock joints and on ground ~5cm from heel, straight column from elbow joint to fetlock, fetlock angle about 125-135 degrees
Hindlimb: line dropped from tuber ischii should touch point of hock and plantar metatarsus and intersect the ground 7.5-10cm behind heel
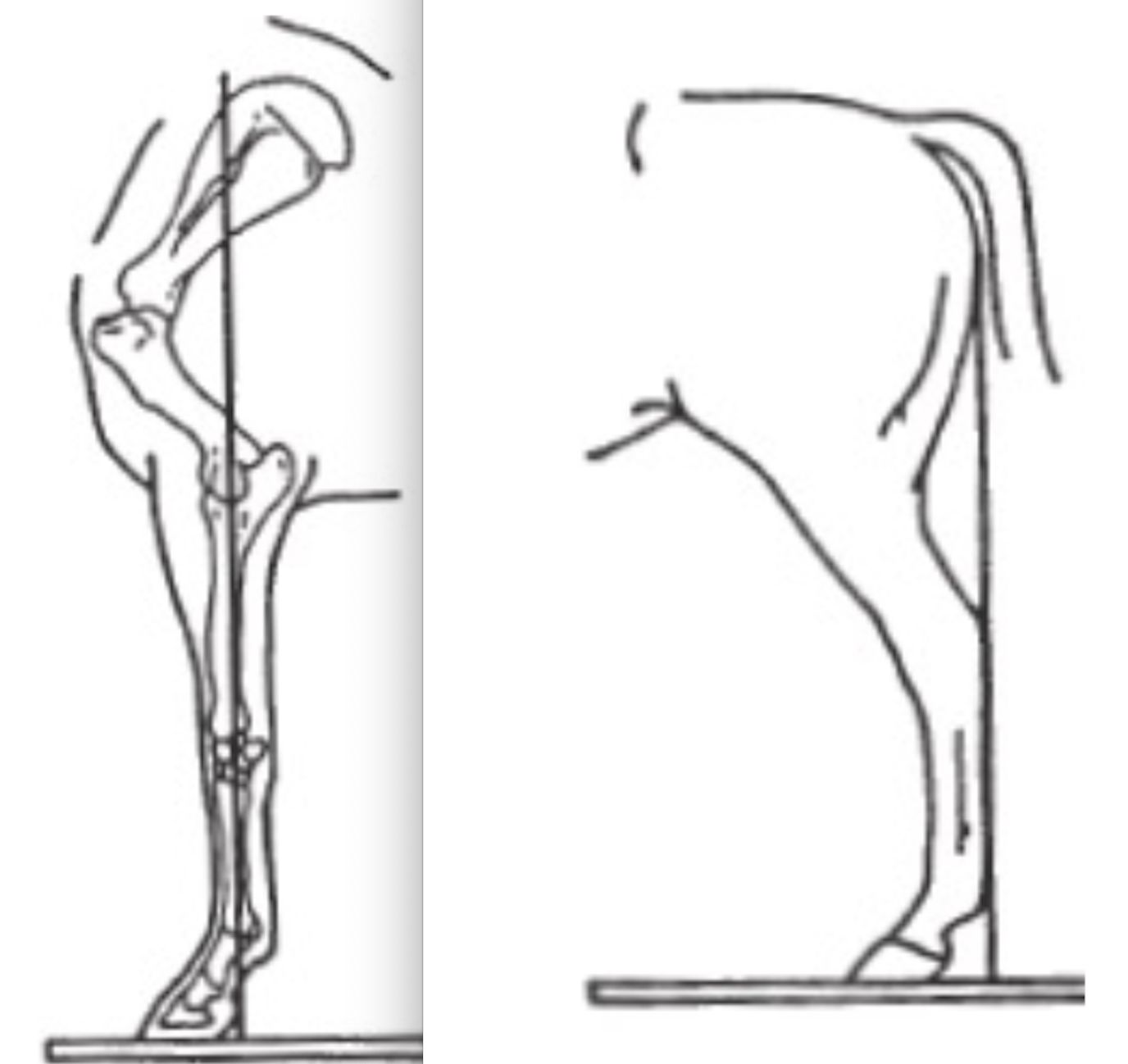
what are some from the side deviations from ideal?
1) buck-kneed (forelimb) - knee inclines forward in front of plumb line, causes increased stress on the flexor tendons/suspensory ligaments
2) calf-kneed (forelimb) - knee inclines backward behind plumb line, carpal hyperextension overloads the dorsal carpus and can lead to carpal fractures
3) sickle-hocked (hindlimb) - hock tilted in front of and away from plumb line
4) camped out behind (hindlimb) - hock tilted behind and into the plumb line, causes inefficiency in propulsion, may lead to spavin and curb
5) leg too straight (hindlimb) - hock sits untilted in front on plumb line
What is hoof balance and when does it become imbalance?
well balanced foot = even distribution of forces throughout the foot
distortion usually caused by uneven loading of pressure from above, many hoof imbalances are caused by poor leg conformation
examination: static hoof balance, static dorsopalmer hoof balance (angle of line through pastern axis should be 55-58 degrees), mediolateral hoof balance (vertical axis through centre of MCIII should bisect hoof in two equal halves), coronary band symmetry, solar views (trimmed frog, length of foot should be approximate width) DYNAMIC hoof balance (foot landing and weight bearing)

What are some hoof balance deformities?
1) Club foot - hoof angle >60 degrees, caused by coffin joint flexion, increased strain on suspensory ligament and SDFT, increased pressure on heel

What is lameness?
clinical sign or manifestation of signs of inflammation (including pain) or a neurological disease, or mechanical defect, that results in a gait abnormality characterized by limping
lameness usually caused by pain/inflammation, super important because it accounts for 67% of lost training days!
What is the load distribution ratio on a horse and how does that contribute to lameness?
60:40 front to hind, with a rider its 70:30
95% of forelimb lameness problems occur distal to the carpus
What are the stages of the lameness exam?
1) history - age, use, onset of lameness (sudden?), duration of lameness, progression of lameness (improvement?), clinical signs of lameness (severe? mild? continuous? intermittent?), training, previous injuries
2) physical exam - asses conformation especially of limb (defects may ID site of lameness as they predispose injuries), observe posture of limbs (resting of forelimb is uncommon while alternating hind limbs in normal), examine muscular symmetry (atrophy? swelling?), foot size, fetlock height, examine soft tissue areas for thickness or increased temperature, manipulate joints and palpate foot
3) evaluate gait - walk and trot (symmetric gait), most lameness amplified by hard surface, look for head nod (down=sound, horse dips its head and neck when sound limb contacts ground), listen to sound created by feet (normal limb=louder strike than lame limb), fetlocks (sound limb drops further than lame), placement of hoof (should be heel first), cranial phase of stride, arc of flight, can use lunge line
forelimb - easier to see when horse trotting towards you, hindlimb-easier when horse is moving away
*hindlimb = observe tuber coxae (lame limb has greater rise and fall)
4) diagnostic analgesia - perineural analgesia (start at foot and work proximally), intrasynovial analgesia (selective), direct infiltration over suspect superficial lesions, look for improvement in lameness, DONT use with severe lameness
5) imaging - after source of lameness has been localized
6) other tests - flexion tests can exacerbate a subtle lameness and can attempt to differentiate lameness associated with distal or proximal limb (grade the change in lameness AFTER flexion, not lameness itself)
What are the gradings of lameness by the AAEP?
0 = no lameness
1 = lameness difficult to detect and inconsistent
2 = lameness difficult to detect but consistent under certain conditions
3 = lameness can be seen consistently in trot in straight line
4 = lameness is obvious at the walk
5 = reluctant to bear weight/minimal weight-bearing in motion and/or at rest
What are the 2 main metabolic pathways for energy creation by the muscles?
1) anaerobic
2) aerobic
energy substrates = fatty acids and glucose
influx of substrate into muscle depends on exercise intensity and duration
lactic acid formed by glycolysis is transported to liver and converted to glucose and glycogen
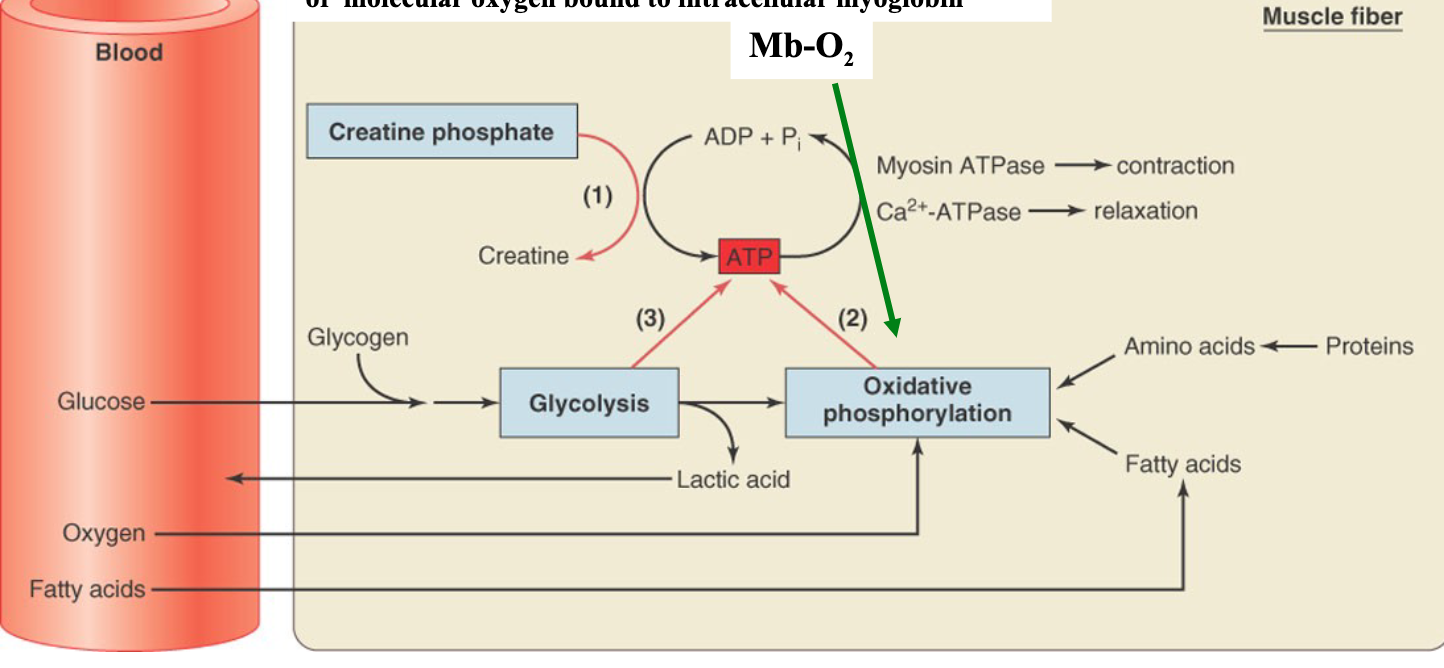
What is the role of creatine phosphate (CP) in skeletal muscle energy formation?
phosphorylates ADP and makes creatine, provides rapid formation of ATP in reversible reaction, anaerobic pathway catalyzed by creatine kinase
during rest creatine phosphate builds up (5x that of ATP) and ATP formation from it is favoured at the start of contraction but limited by initial CP concentration
what is the timing of energy usage with oxidative phosphorylation in the muscles?
initial 5-10 minutes = breakdown of muscle glycogen to glucose for fuel
next 30 mins - blood borne substrates (glucose, Fatty acids) are the main fuel
after another 30 mins fatty acids are the main fuel
(O2 availability is the limiting factor)
When is glycolysis used to form energy in the muscles?
high intensity (>70% max) short duration (2-3 minutes) exercise is when degradation of muscle glycogen to lactate is the main pathway for ATP
produces only small amounts of ATP (3mol) so inefficient but rapid, no O2 needed but lactic acid needs to be cleared by the liver (forms glycogen)
What occurs during skeletal muscle recovery?
after activity creatine phosphate and glycogen must be replaced which required energy so muscles continue to consume O2 after muscular contraction has stopped (also required to metabolize lactic acid) = elevated O2 consumption
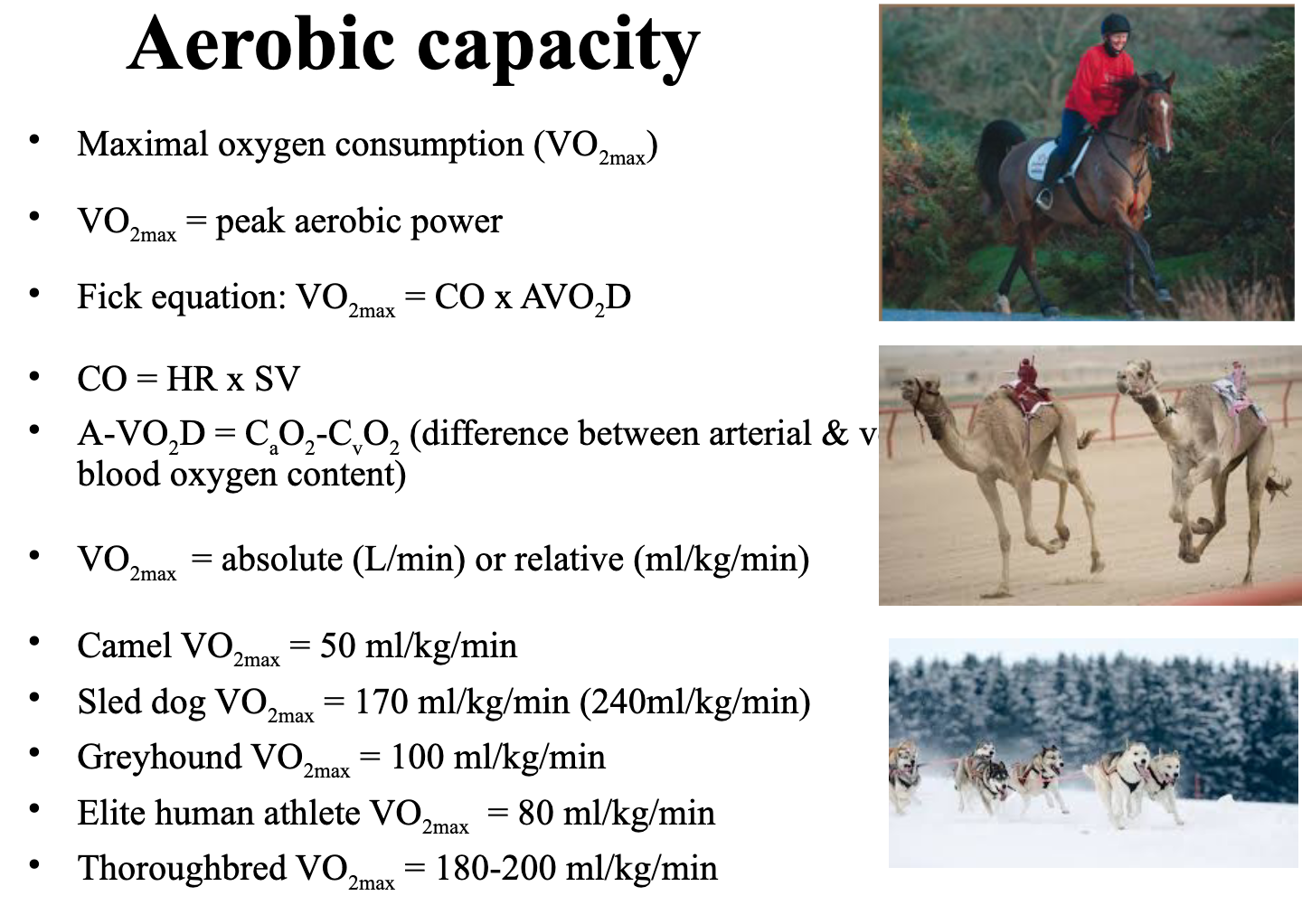
What would you use to assess physical/aerobic capacities?
VO2max is the gold standard, represents the maximal oxygen consumption (peak aerobic power), can be absolute (L/min, doesn’t account for weight) or relative (ml/kg/min)
Fick equation:
VO2max = CO x AVO2D
CO = HR x SV
AVO2D = CaO2 - CvO2 (difference between arterial and venous blood oxygen content)
What is the oxygen uptake of the horse at rest?
2.5 l/min
3.5 ml/kg/min
What is the oxygen uptake of the horse at maximal intensity?
60 l/min
160 ml/kg/min
(increase in CO, HR, and SV)
What are the cardiovascular responses to exercise?
conductive transport=O2 movement from lungs to muscle, depends on cardiac output and arterial oxygen which depends on Hb concentration, binding capacity, and % Hb saturation
diffusive transport=O2 movement within muscle
80-90% cardiac output goes to skeletal muscles during high intensity exercise (vs 10-20% at rest), resistance to flow from muscular arterioles
how much blood is the equine spleen capable of releasing?
up to 12 L RBC
What is so special about the microcirculation in a horse??
diffusing capacity determines the level to which CvO2 falls during max exercise (extraction), capillaries are main site for blood tissue exchange
horse muscle may have 400-800 capillaries per square millimetre containing >80% of intramuscular blood volume
during exercise increased pulmonary aterial pressure leads to recruitment and distension of the vascular bed which reduces vascular resistance and increases capillary conductance and volume