HSCI 130 - Final Exam
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
What are the parts of the Canadian Health Act?
C - Comprehensiveness
U - Universality
P - Portability
P - Public Administration
A - Accessibility
Explain the principles of the Canadian Health Act
Comprehensiveness - provide all medically necessary services are provided; medical necessity is determined by the government
Universality - care is delivered on universe terms to all insured people
Portability - If you travel/move, your health care will come with you, if going abroad it will cover you at the rate it would cost if incident happened at home
Public Administration - system is operated on a non for profit basis by a public authority that is accountable to the government
Accessibility - health care is accessible to all Canadians with insurance without financial or other barriers
What are the Whitehall Studies led by Micheal Marmont?
A series of studies investigating the relationship between social class, employment conditions, and health outcomes among British civil servants, emphasizing how socioeconomic status impacts health disparities.
Discovers the Social Gradient
What is the number one reason people seek professional health care?
chronic pain
What are the five paradigms of health?
Sociology of the Body
Symbolic Interactionist
Conflict
Feminist
Structural-Functionalist
What is “The Condition of the Working Class in England“ published by Engels
A foundational text in social criticism that examines the living conditions and health of the working class during the Industrial Revolution, highlighting issues of poverty, labor exploitation, and social injustice.
What is the social gradient in health?
The concept that health outcomes vary according to an individual's socioeconomic status
those lower on the socioeconomic ladder experience worse health outcomes compared to those higher up
What is Social Inequality?
The unequal distribution of resources, opportunities, and treatment in society, leading to disparities in health, wealth, and social status.
What is social inequity?
not just describing the differences: you are saying they are wrong. Placing a moral stance.
unfair, avoidable differences arising from. poor governance, corruption, social exclusion, discrimination
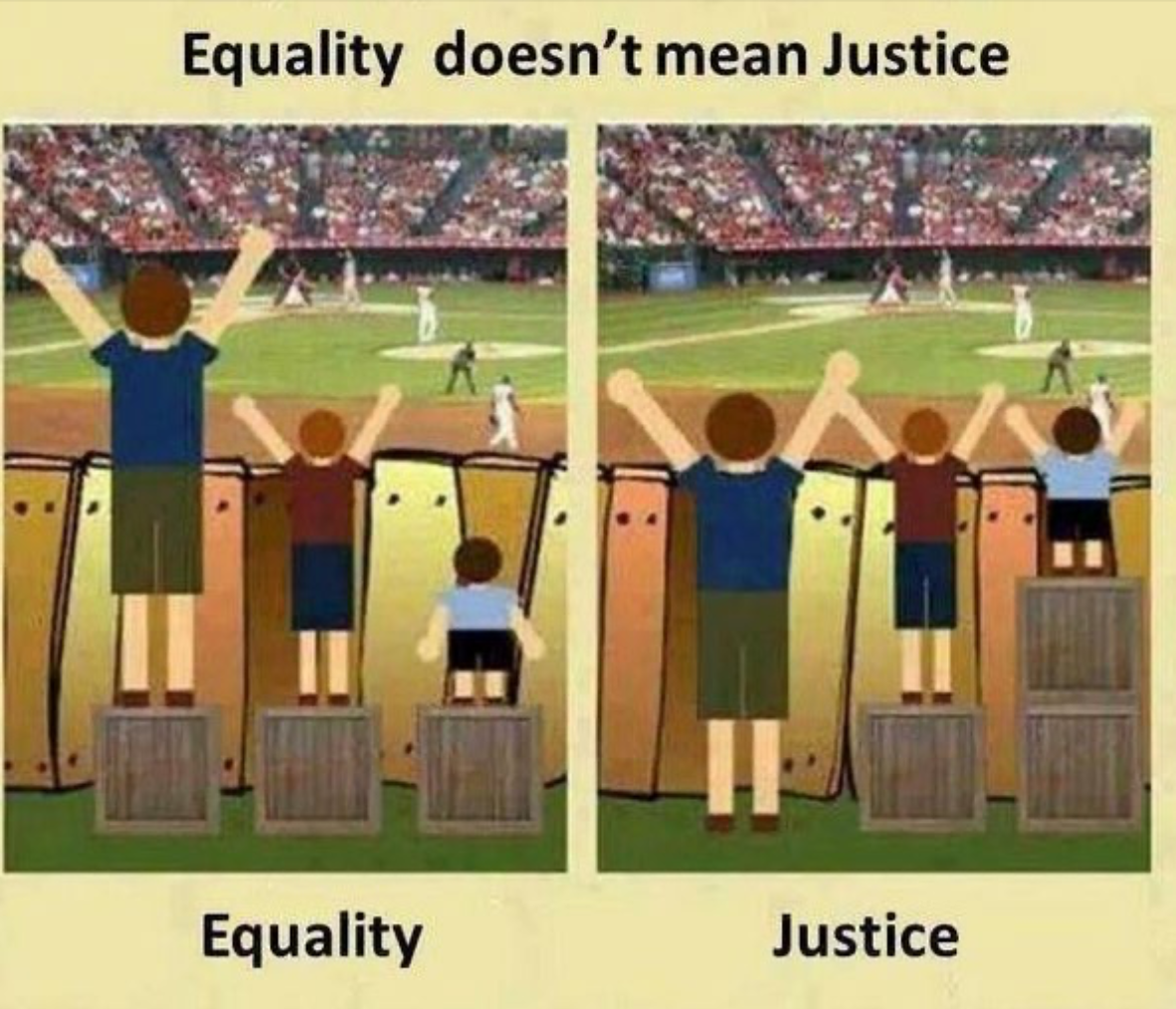
Why doesn’t equality = justice?
Equality fails to account for the unique needs and circumstances of individuals or groups.
Justice requires addressing systemic inequalities and ensuring equitable outcomes for all.
Example: Some people might need more assistance than others to reach an “equal“ status, as they face additional barriers or challenges.
What are the Explanations of the Social Gradient?
Materialist & Neo-Materialist Explanations
Cultural Behavioural Explanations
Psychosocial Explanations
What is the Materialist Explanation?
Differential Exposure hypothesis: greater exposure to psychosocial stressors from financial problems, neighbourhood issues and social isolation
People exposed to positive and negative exposures over a lifetime are indicators of advantages and disadvantages & differences in exposure to stress — that stress can then influence health outcomes
Social Inequality leads to more stressful life experiences, and the consequence of this exposure: worse health
Material advantages/disadvantages (housing neighbourhood conditions, employment) accumulate and contribute to negative/positive health results
What is the Cultural Behavioural Explanation?
Differential vulnerability hypothesis: all have stressors but the position in the social gradient can make some worse than others
How we learn to behave in society
Problem is that people in lower socio-economic positions have developed coping strategies and behaviours (like smoking, drinking, etc,) that may worsen health inequalities
What is the Psychosocial Explanation?
What matters is how people interpret the hierarchy
Where people see themselves in the socio-economic gradient compared to other people
Sense of shame and envy when people feel others have more
That is what influences health outcomes
What is the impact of stress on health?
Life stress can contribute to the development and impact the maintenance of several major mental and physical health conditions
What are the implications of Hans Selye’s path to discovery for health science students
Research on stress
Importance of understanding how stress affects health (increased risk for diseases/impacted treatment effectiveness)
Health science students should recognize the many impacts of stress
and therefore the need for comprehensive stress management strategies.
What are the biological responses to stress?
Fight or flight
Increased blood pressure/heart rate
Sweating
Constriction of blood vessels
Cognitive decline
How is stress measured in current health science literature?
Stress is typically measured through physiological markers (such as cortisol levels), psychological assessments (like surveys and scales), and behavioural observations, allowing researchers to assess its impact on health.
Why are gender/sex considered a social determinant of health?
Gender VS Sex
Sex
Biological characteristics enabling human reproduction
Encompasses anatomy, physiology, genes, hormones
Gender
Social construct/human invention
Socially prescribed ideas of “maleness“ and “femaleness“
Separates people into differentiated gendered statues
What is “Gendering”?
Characterizing things as “masculine“ or “feminine“
What are the four hypotheses that explain gender differences in health and illness?
The role-accumulation hypothesis
The role-strain hypothesis
The social acceptability hypothesis
The risk-taking hypothesis
What is The Role-Accumulation Hypothesis?
Suggests that taking on multiple roles leads to positive health effects
What is the Role-Strain Hypothesis?
States that women’s multiple roles are harmful to health
What is the Social Acceptability Hypothesis?
Suggests that women have been socialized into accepting the sick role
What is the Risk-Taking Hypothesis?
Suggests that men engage in risky behaviour because they are socialized to do so
What does Chan & Saewyc’s study examine/find?
Examined the relationship between the experiences of discrimination based on race and physical appearance and their relationship to aspects of health
Findings:
Experiences of violence associated with self rated health, self harm, suicidality, foregone mental health care
differential vulnerability vs exposure
Differential Exposure: Greater exposure to psychosocial stressors influence health
Differential Vulnerability: Everyone has stressors; but position in social gradient can make some worse than others
Whitehall Studies
A series of studies investigating the health inequalities among British civil servants, highlighting the impact of social class on health outcomes.
What are the different explanations to explain the Occupation Gradient?
The Demand-Control Model
The Effort-Reward Imbalance Model
What is the Demand Control Model?
The psychological demands on the working person (How demanding is the work/what is happening at work)
The degree of control the person has over work schedules and job conditions
Lower level of control + high job strain = negative health outcomes
What is the Effort-Reward Imbalance Model?
Emphasizes the importance of social reciprocity in our work lives
adverse side effects on health if:
Time and effort devoted to work are not matched by adequate rewards:
Income
Career advancement
Job security
What is a possible effect of Effort-Reward Imbalance?
“Individuals with effort-reward imbalance at work have an increase risk or coronary heart disease independent of any job strain experienced”
What is Precarious Employment? How does it impact health?
Jobs that are unstable, low-paid, and lack benefits
Seen as a social determinant of health
Can lead to increased stress and anxiety, negatively impacting mental and physical health.
What is Income Inequality?
The uneven distribution of income within a society or community
How is Income Inequality measured?
Gini Coefficient
Ranges from 0-1
0 = perfect equality
1 = hypothetical situation with 1 person holding ALL income
Problem: Different distributions of inequality can lead to the same Gini
Robin Hood Index - Measuring the amount of income that would need to be redistributed to achieve equality.
Decile Measures - income earned by the top 10% / income earned by the bottom 10%
Proportion of Income Earned By top% of population
What is the relationship of Income Inequality and health?
hypothesis that greater income inequality leads to a stronger gradient in health
Does evidence indicate that the social gradient in health is changing?
Yes, research suggests that the social gradient in health is becoming becoming steeper due to socio-economic statuses and inequality
Is it possible to reduce social class disparities?
Policy initiatives strongly emphasize the importance of making th ongoing struggle against inequalities a higher priority
Race vs Racialization vs Racism
Race - classification of humans into groups based on physical traits, ancestry, genetics, or social relations
Racialization - refers to processes where people are systematically categorized & sorted into inferior social statuses according to perceived racial differences
Racism - prejudicial treatment of groups & individuals according to subjective understandings of race
How does ethnicity affect healthcare?
Perception and understanding of symptoms
Willingness to express symptoms (like pain)
Health care behaviour
Willingness to adopt sick role / use health-care services
Social determinants of health
unequal distribution of wealth/power and privilege
What are the explanations of ethnic differences in health and illness?
biomedical model examines differences in biophysical traits
Believed that biological differences increase risks — discredited
cultural behavioural perspective argues that culture shapes behaviour, which shapes health
People’s lifestyle determines health
socio-economic perspective believes the differences are due to social class
access to care, physical environment, chronic stress
Who is Brian Sinclair?
An Indigenous man who died in a hospital waiting room in Canada in 2008 after being ignored by staff for hours, highlighting systemic racism in healthcare.
What is Cultural Competence?
recognizing behaviours, attitudes, and policies that enable effective cross-cultural communication and understanding in healthcare settings.
Cultural Sensitivity
the awareness and consideration of cultural differences and the impact on patient care and communication.
Cultural safety
acknowledges power imbalances, institutional discrimination, colonization as they apply to health
What is the healthy immigrant effect?
When immigrants arrive to Canada they typically arrive in better average health than those born in Canada, but over time (typically after 4-10 years) their health deteriorates
What are the explanations for the deterioration in Healthy Immigrant Effect?
Converging lifestyles
Acculturation theory - as immigrants integrate they adopt Western diet and practices like smoking, fast food, and alcohol use
Resettlement Stress
New added stress from moving to a new place and facing discrimination
Proficiency in the official language
Differential access to health care
Language and cultural barriers that prevent access to health care upon arrival; with integration, more recognition of previously undiagnosed conditions
little evidence on there being less access to care
What are the main findings of De Maio & Kemp (2010)
Both self rated health and self-rated emotional health deteriorated over time
Visible minorities and people who experienced discrimination more likely to report decrease in self-rated health status
How does structure impact individual behaviours?
Lower socio-economic status can lead to poorer health outcomes
The social structure of people having less access to resources and education
Affects future employment and income
This impacts ability to access care, treatment, and healthy lifestyle choices (foods, support programs)
This is why it is important to recognize that individual agency, although important in maintaining health, it is also impacted by the structural components in society
Inhibit a person’s ability to making healthy choices and engaging in healthy behaviours
What are user fess?
Asking people to make a small co-payment every time they sought health care
What are issues affecting the Canadian Health care system?
Training (Med school spots, residency spots)
Healthcare worker shortage (Doctors and nurses)
Spending coverage - what we consider “necessary” healthcare
Long wait times specifically for specialist care
Quality of care
Price of drugs
What was the first province to have medical insurance plans?
Saskatchewan
How is Healthcare funded in Canada?
50/50 with federal and provincial government
Provincial responsibility and delivery but federal government shares the cost
What year was medicare implemented?
1972
What year was the Canada Health Act implemented?
1984
What is the Canada Health Act?
principles and criteria for provinces to receive federal support; prohibitions of extra billing and user fess added to existing components
What are the key features of the Canadian Health Care System?
Health care delivery is the responsibility of the PROVINCES
Privately delivered (doctors are privately owning their practice) but publicly financed (by government)
Private providers and public not-for-profit hospitals
Fee-for-service funding and global budgets - government decides how much each service will pay a doctor
Choice of practitioner - can choose family doctor/ask for another specialist
Universal coverage applies to less than ½ of total health care expenditures
What is Canada’s Health Spending in 2023?
12.1% of GDP
about $300 billion
What is the largest spending categories for healthcare?
25.6% Hospitals, 14% drugs, 14% physicians
How much are we spending on Public Health in Canada?
5% on public health
not large category
How does aging contribute to overall growth in health spending?
Aging is only a relatively modest contributor to overall growth in health spending
Depends on location
Aging is contributing, but EVERYONE is using more healthcare
What percentage of BC’s budget do we spend on healthcare?
43%
Why has the proportion of spending on healthcare gone up in Canada?
There has been a decrease in revenue - Taxes going down
But an increase in the desire of services
less money coming in but people still want them to spend the same amount of money on healthcare
What country spends the most money on on healthcare?
United States
What provinces have the highest shortage of doctors?
Nunavut and Northwest Territories
Males vs Females in medical specialties?
50-50 - Family Med
57 Male - 43 Female - Med Specialties
66 Male - 34 Female - Surgical Specialties
What percentage of the population does not have a family doctor?
20% - 1/5 do not have a family doctor
What are some of the driving factors of the doctor shortage?
Changes in practice patterns
Limits on how many hours can work
Limited patient encounters
Physician working ½ the amount of time, but the population and number physicians being trained stays the same
Retirement
Burnout
What are possible solutions for the doctor shortage?
opening new medical schools - especially centred on FM
Better payment models for GPs
System reform - have practices that are operated by the government that physicians can work in without dealing with owning and operating a practice
Incentives to work to rural areas - loan forgiveness, set up practice, better pay, housing, and finding work for their spouses