N470: Arterial lines
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
indications for an A-line
- BP monitoring (vasoactive meds)
- blood sampling (ABGs or frequent blood draws)
What do we never do with an A-line?
NEVER infuse anything into it
Which arteries can an A-line be placed in?
- radial (most common)
- brachial
- femoral
Who can insert an A-line?
MD, RT, certified RN
Equipment for an A-line insertion
- pressure bag
- 500 ml bag NS
- pressure tubing with transducer
- occlusive dressing
- immobilizer prn
- pressure cable
- monitor
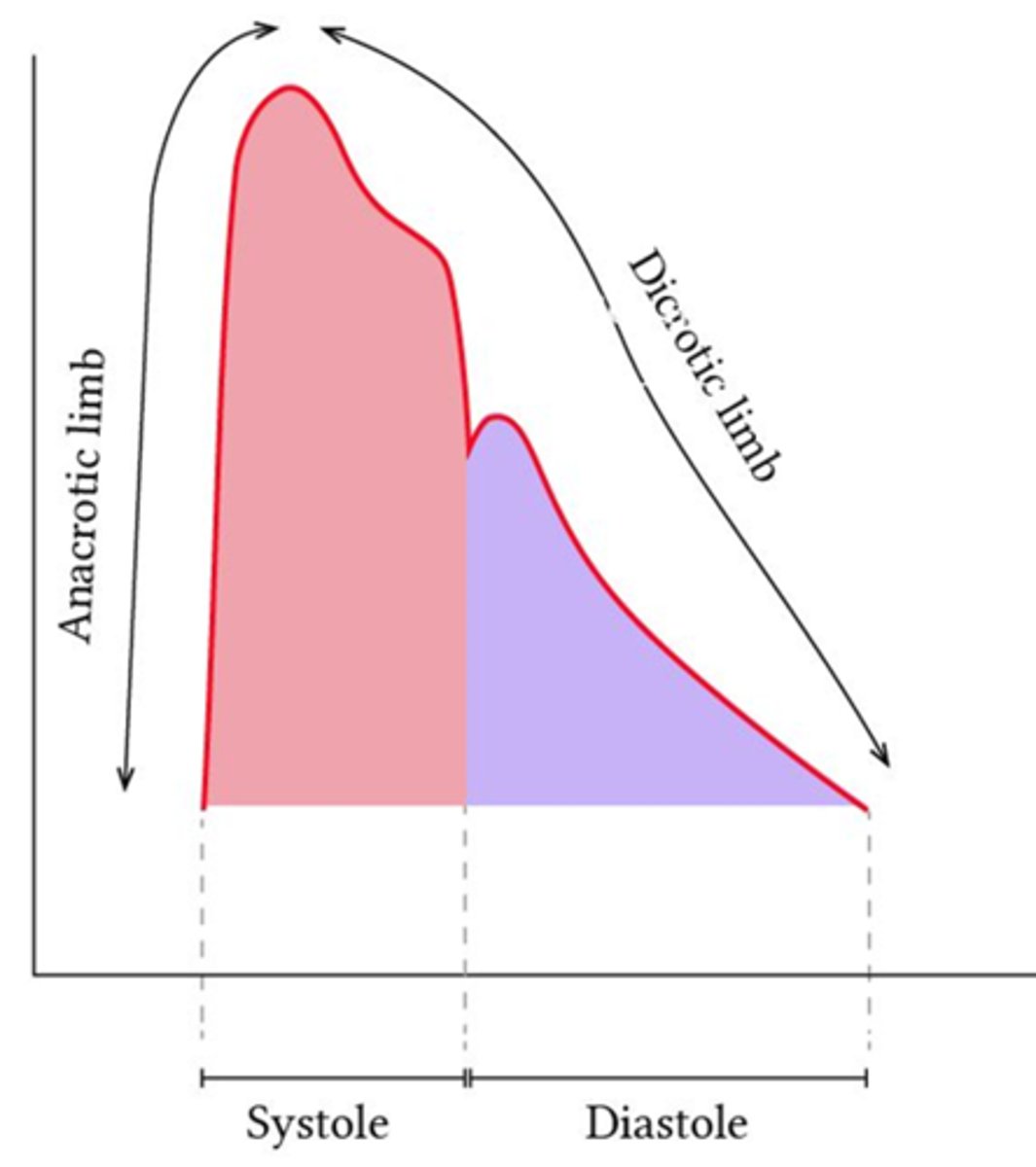
A-line waveform basics*
should have:
-swift systolic uptake (S1)
- diastolic runoff (S2)
- dicrotic notch on diastolic runoff
where is the transducer placed?
at the level of the R atrium aka the phlebostatic axis
- 4th ICS
- midclavicular line (R atrium)
- midaxillary line (transducer)
What occurs if the transducer is above the level of the R atrium?
BP reading falsely low
What occurs if the transducer is below the level of the R atrium?
BP reading falsely high
Purpose of zeroing the A-line
to eliminate gravitational forces affecting pressure readings from the transducer
When should an A-line be zeroed?
- upon insertion
- questionable readings
- when there is a disconnect
square wave test
pulling the flush valve opens it and the transducer reads the 300mmhg pressure from the pressure bag. This creates a sharp rise and a plateau in the wave form that drops off sharply when the valve is closed
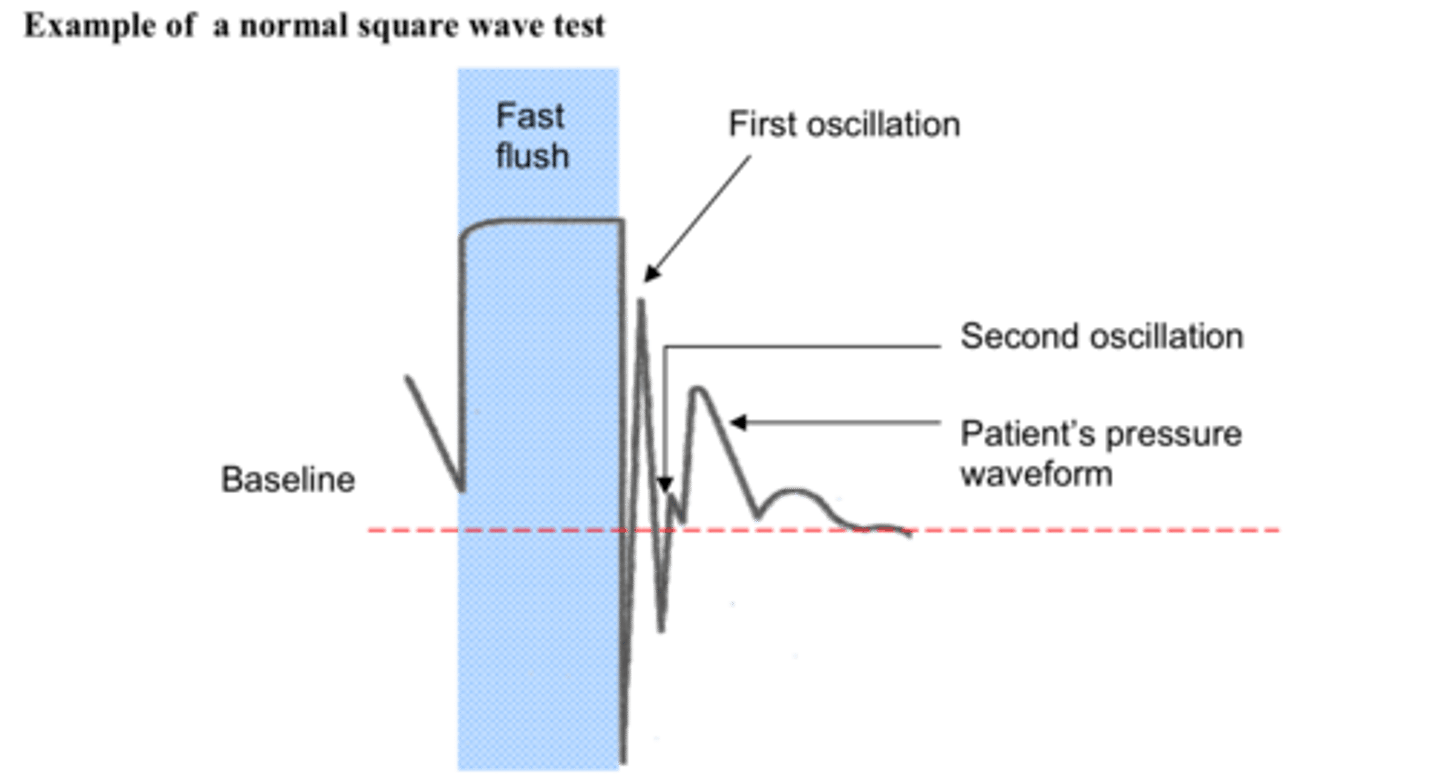
What is a normal square wave test (indicates accurate BP reading)? *
2 oscillations only
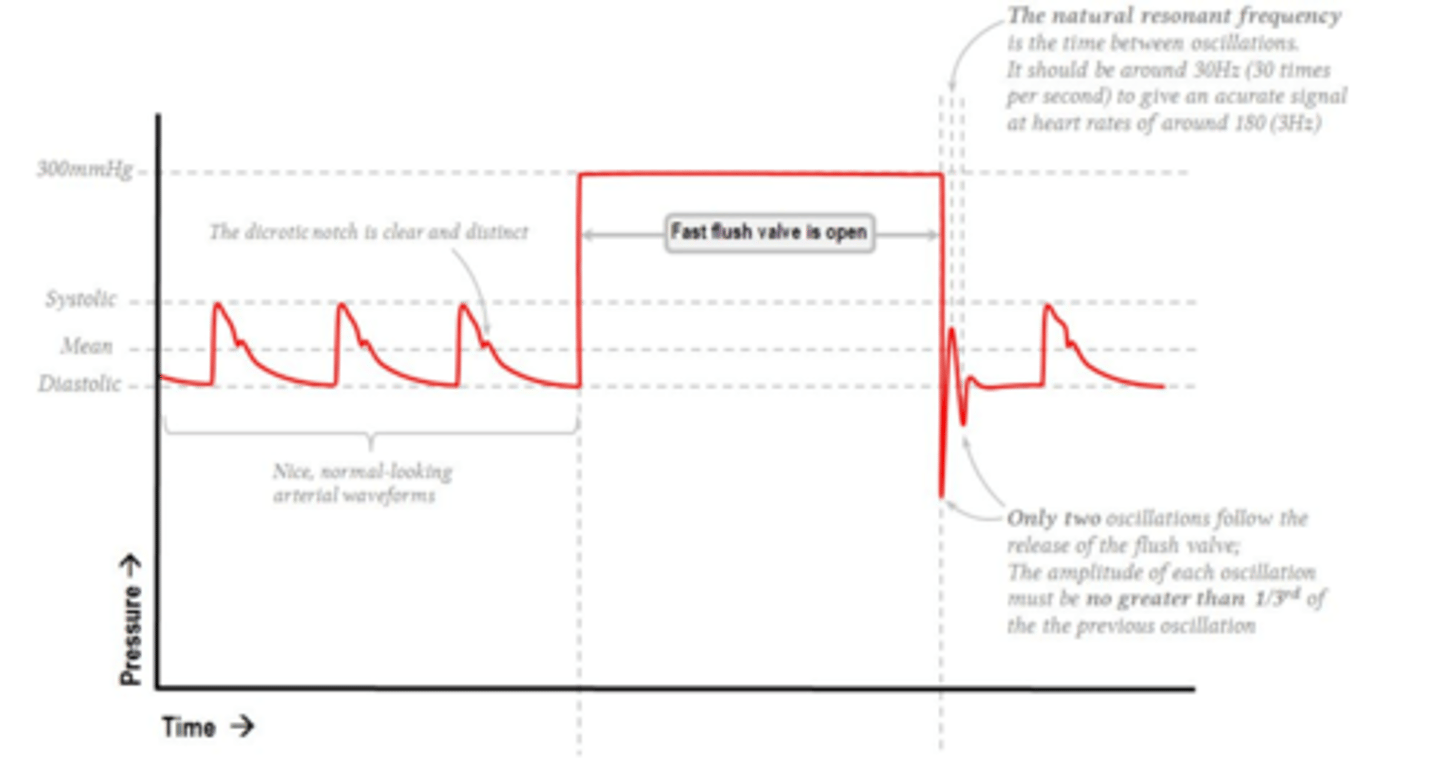
What indicates under-dampening?*
more than two oscillations on the square wave test
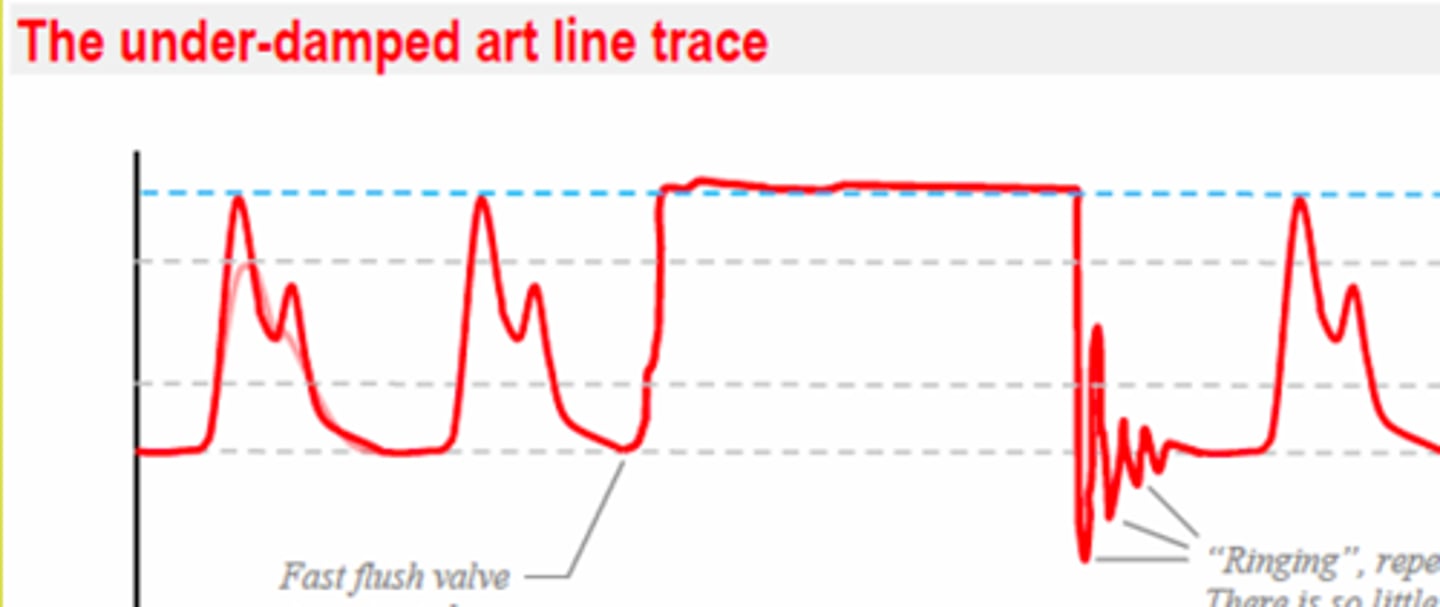
What can under-dampening do the the A-line reading?*
make BP falsely high
causes of under-dampening* (4)
- turbulent flow
- catheter whipping in artery
- too many connections/extensions
- pressure tubing overly stiff
What indicates over-dampening?*
one oscillation only
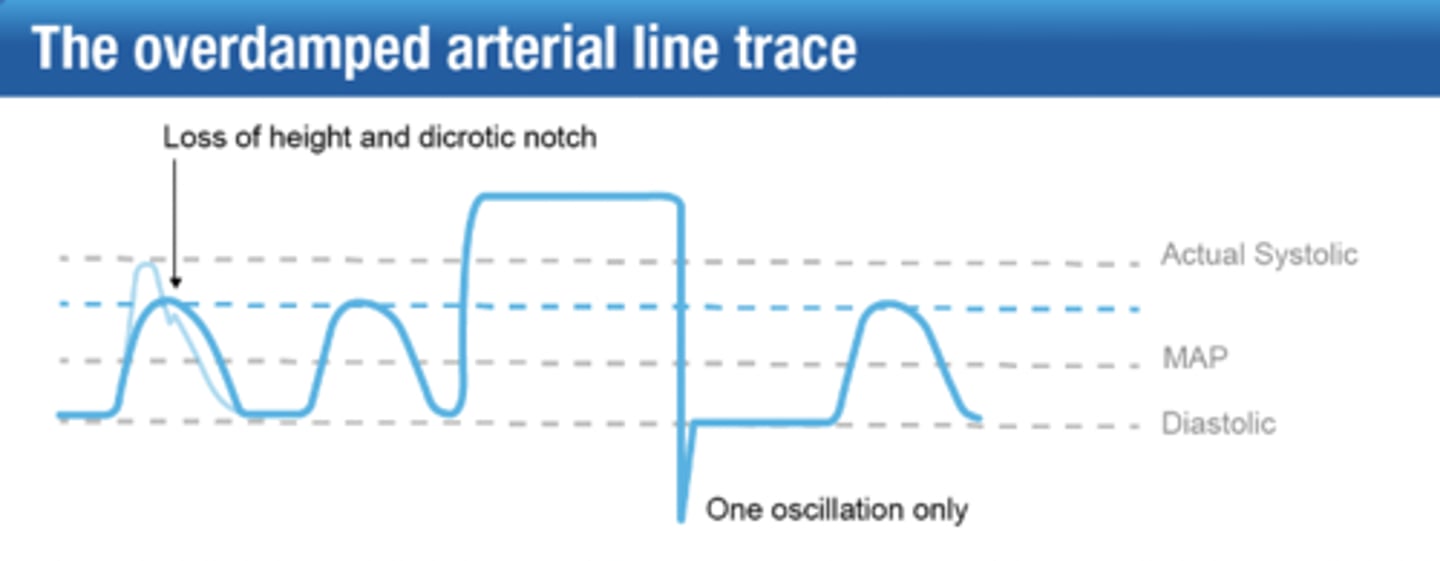
What can over-dampening do the the A-line reading?*
make BP falsely low
causes of over-dampening* (5)
- loose connections
- bubbles in tubing
- kinked tubing
- overly-compliant pressure tubing
- catheter tip occlusion (clot/stuck against artery wall)
5 Ps of assessing A-line*
1) pain
2) pallor
3) paresthesia (numbness)
4) paralysis
5) pulses (cap refill)
Assessment pieces for A-line equipment (4)
- connections tight
- pressure bag filled to 300 mmHg
- flush bag has enough fluid
- tubing not expired (Q96H)
Describe the VAMP system on an A-line
- closed system=reduced infection risk
- 5 ml reservoir holds "waste" during blood sampling
- needless port used for sampling (pt blood sample "waste" cannot be returned to pt)
