Week 12: GU and Kidney Disease
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
Normal urine output (mL/kg/hr)
0.5 mL/kg/hr (0.5 cc)
30 cc/hr
Oliguria urine output volume
< 0.5 cc’s per hour
< 400 mL/day
Anuria urine output volume
< 50-100 mL per day
Kidney function
maintenance of fluid balance, electrolyte balance, and acid-base balance
BP regulation
Excretion of waste product
Regulate RBC production, vitamin D activation, and secretion of prostaglandins
How do the kidneys regulate BP?
renin
Acute Kidney Injury (AKI)
rapid decrease in renal function d/t damage to the kidneys that can result in potentially life-treatening metabolic complications and fluid and electrolyte imbalances
Acute kidney injury (AKI)
Onset?
Reversible?
Length?
% of nephrons involved?
Rapid onset
Often reversible
Lasts 2-4 weeks
50% nephron involvement
End-stage kidney disease (ESKD)
Onset?
Reversible?
% nephron involvment
Prognosis?
Gradual onset
Permanent
90-95% nephron involvement
Poor prognosis — chronic condition that requires a lot of medical treatment
Stage 1 AKI
Creatinine
Urine output
Creatinine: 1.5-1.9 x baseline or an increase > 0.3 mg/dL
Urine output: : < 0.5 mL/kg/hr for 6–12 hr
Stage 2 AKI
Creatinine
Urine output
Creatinine: 2.0-2.9 x baseline
Urine output: < 0.5 mL/kg/hr for ≥ 12 hr
Stage 3 AKI
Creatinine
Urine output
Creatinine: 3 × baseline or ≥ 4.0 mg/dL OR Initiation of renal replacement therapy
Urine Output: < 0.3 mL/kg/hr for ≥ 24 hr OR anuria ≥ 12 hr
Intrarenal AKI
damage to the structure within the kidney
Prerenal AKI
reduced blood flow to the kidneys
Postrenal AKI
obstruction of urine outflow for the kidney
Prerenal AKI causes
Volume depletion (ie hypovolemia)
Impaired cardiac output: Shock, HF, MI
Renal artery stenosis or occlusions (thrombi)
Systemic vasodilation: Sepsis, anaphylaxis, certain meds
NSAIDs a reduce renal blood flow; dilate the afferent arteriole
◦ACE inhibitors/ARBs impair auto-regulation; dilate the efferent arteriole
How is prerenal AKI corrected?
by correcting hypovolemia, increasing BP and cardiac output, and improving renal blood flow
restore BF ASAP, or else AKI will become intrarenal AKI!!!
Intrarenal (AKI) causes (3)
Glomerular obstruction and inflammation
Immune mediated microvascular diseases
Nephrotoxic agents: Contrast dye, Aminoglycosides, Penicillins, NSAIDS
What kidney tissues may be damaged that are r/t intrarenal AKI?
Glomeruli
Tubules
Interstitium
Acute Tubular Necrosis
damage to renal tubules = the major pathologic mechanism
Injured cells slough off into the tubular lumen and forms occlusions, leaving to increased intertubular pressure and reduced GFR
Ischemic Acute Tubular Necrosis (ATN)
Prolonged prerenal states
tubular cells die from lack of O2 – which is how prerenal turns into intrarenal
Causes of Ischemic ATN
Shock
sepsis
prolonged hypotension
hypovolemia
How can NSAIDs cause prerenal AKI?
Inhibit prostaglandins, which normally dilate the afferent arteriole
Without prostaglandins → the afferent arteriole constricts → ↓ renal blood flow
Acute Interstitial Nephritis (AIN)
NSAIDs are a classic cause of drug-induced allergic interstitial nephritis, which is another form of intrarenal AKI
How can NSAIDs cause intrarenal AKI?
If prerenal hypoperfusion is prolonged because of NSAID-induced vasoconstriction, the kidney becomes ischemic → ischemic ATN
Postrenal AKI obstruction causes
Urinary calculi
Tumors
Benign prostatic hyperplasia (BPH)
Strictures
Blood clots
Stage 1 of AKI: Onset or initiating phase
Begins hours to days after triggering event
May begin to see increase in BUN and creatinine
Stage 2 of AKI: Olliguric (anuric) phase
Urine output < 400 ml/day
Increase in BUN and creatinine levels
Electrolyte disturbances: K+, PO4-, Mg+,Ca+
Metabolic acidosis: HCO3-
Fluid overload
Uremic symptoms
Duration usually 1-2 weeks but may be longer
longer oliguria = worse prognosis
Stage 3 AKI: Diuretic phase
Gradual increase in urine output to > 400 ml/day; increased diuresis (up to 10 L/day)
Start to see electrolyte losses/changes bc of how much they are urinating
Stage 3 AKI characteristics
BUN and creatinine stabilize
Renal function remains impaired
Uremic symptoms persist
Potential dehydration
Potential hypokalemia
Duration usually 1-2 weeks
Stage 4 AKI: Recovery Phase
GFR
return of GFR to 70-80% of normal
Stage 4 AKI characteristics
Decreased edema
Normalization of fluid and electrolyte balance
Decreased energy level and stamina, but is significantly improved
AKI diagnostic studies
X-rays
Renal ultrasound
Nuclear imaging
CT scan
MRI
Cystoscopy and retrograde pyelography
Renal biopsy
What should be held when doing AKI diagnostic studies?
Contrast dye because the kidneys can’t filter it out well
What drug should be held when a patient is getting an AKI diagnostic study?
Metformin and other nephrotoxic drugs
AKI management
Identify and correct the underlying cause
Fluid therapy — maintain fluid balance and avoid fluid excess
Nutritional therapy
Renal replacement therapy
Assessment for fluid therapy
Strict I&O
Vital signs
Daily weights — must be measured same way each time
Fluid therapy for prerenal AKI
fluid bolus for hypovolemia and hypotension
Fluid therapy for oliguric phase
fluid restriction
Fluid therapy for diuretic phase
patient may loose up to 10 L/day
may need to increase fluids to prevent dehydration d/t diuresis
Hyperkalemia management
Monitor EKG
Eliminate K+ intake
Increase K+ output
Reverse cardiac cell membrane effects of increased K+ by administering IV Ca2+ gluconate
Dialysis in patients with persistent hyperkalemia
Nutrition and fluid therapy in AKI
Calories, carbs, and protein
Electrolytes
Fluids
High calorie and carb diet
Protein varies with treatment
Electrolyte restriction as indicated
Fluid needs vary by phase
Nutritional consult
Indications for renal replacement therapy in AKI (4)
fluid volume overload
persistent hyperkalemia
metabolic acidosis
uremia
Uremia
increased nitrogenous wastes in the blood d/t the kidneys being unable to excrete it because of AKI
Uremia symptoms
Metallic taste in mouth
Anorexia
N/V
Muscle cramps
Itching
Dry, flakey skin
Fatigue/lethargy
Hiccups
Edema
Parenthesias (sensation of pins and needles)
Continuous renal replacement therapy (CRRT) indication
meant for patients who are hemodynamically unstable and cannot tolerate quick fluid shifts and intermittent dialysis
Continuous Venovenous Hemofiltration (CVVH)
uses ultrafiltration to drag solutes across a membrane - no dialysate, requires replacement fluid
CVVH indications
fluid overload
septic shock
multisystem organ failure
Continuous Venovenous Hemodialysis (CVVHD)
uses diffusion to clear toxins via concentration gradient, less aggressive than CVVH
CVVHD indications
metabolic derangements like acidosis or hyperkalemia
rising BUN/Cr
Continuous Venovenous Hemodiafiltration (CVVHDF)
combines diffusion and convection, provides broadest solute clearance
CVVHDF indications
severe metabolic instability
septic shock
multisystem ICU patients
Slow Continuous Ultrafiltration (SCUF) and use
pure fluid removal only, minimal solute clearance
used for volume overload
Temporary dialysis access location
Subclavian vein
Internal jugular vein
Femoral vein (last choice)
Most important AKI nursing considerations
Strict I&O, daily weights (most accurate fluid indicator)
Monitor urine output hourly (oliguria < 0.5 mL/kg/hr)
Avoid nephrotoxic agents (NSAIDs, contrast, aminoglycosides)
Manage hemodynamics (optimize perfusion, MAP > 65)
AVOID HYPOTENSION***** — especially prolonged hypotension
Chronic Kidney Disease (CKD)
A progressive and irreversible loss of kidney function where they can't effectively remove waste and extra fluid from the body
Present for >3 months
Most common risk factors for CKD
Diabetes — most common
Hypertension — 2nd most common
CAD
Obesity
Recurrent AKI episodes
Nephrotoxicity medications
What 2 ways can CKD be diagnosed? (via labs)
Decreased GFR
< 60 mL/min/1.73 m²
OR
Evidence of kidney damage, regardless of GFR:
Albuminuria ≥ 30 mg/day
Structural abnormalities
History of kidney transplant
Electrolyte abnormalities d/t tubular disorders
What disease is at high risk for developing d/t CKD?
Cardiovascular disease
Complications associated with CKD (3)
Anemia
Bone/mineral disorders
Fluid/electrolyte imbalances
Early stages of CKD are often _____
asymptomatic
Normal GFR (mL/min)
> 90 mL/min
CKD stage 1
GFR
Kidney damage?
Symptoms
Albuminuria
Normal GFR
Evidence of kidney damage with normal function
Usually asymptomatic
Albuminuria may be present
CKD stage 2
GFR
Kidney damage?
Albuminuria
Urine changes
Mild decrease in GFR = 60-89 mL/min
Evidence of kidney damage — nephron damage with normal labs
Albuminuria
Subtle urine changes — increase urine output with dilute urine
CKD stage 2: Why is there an increase in urine output and dilute urine?
Kidneys lose ability to concentrate urine and get the excess electrolytes out
which is why people will get hyperkalemia
CKD stage 3A
Mild-moderate decrease in GFR = 45-59 mL/min
**Turning point in diagnosis — progression accelerates
CKD stage 3B
GFR
Nephron function
Kidney filtration
Fluids, proteins, and electrolytes?
Moderate-severe decrease in GFR = 30-44 mL/min
Remaining nephrons do not function properly
Kidney cannot manage metabolic wastes, fluid balance, or electrolyte balance
Restriction of fluids, proteins, and electrolytes instituted
CKD stage 4
GFR
Restrictions
Complications of CKD
Severe decrease in GFR = 15-29 mL/min
Unable to manage metabolic wastes, fluid balance, or electrolyte balance
Restrictions of fluids, proteins, and electrolytes required
Complications of CDK (CV issues, anemia, HTN, bone disease) likely
CKD stage 5: End Stage Kidney Disease (ESKD)/Chronic RF
GFR
What builds up in the blood?
What is particularly imbalanced?
GFR < 15 mL/min Remaining
Severe uremia: excessive amounts of urea and creatinine buildup in blood
Uncontrolled fluid and electrolyte imbalances
CKD stage 5 requirements for survival
dialysis and/kidney transplant
Albuminuria and relationship to CKD
a measurement of how much protein is leaking into the urine
More albumin = more kidney damage and faster CKD progression
Body systems affected by End Stage Kidney Disease (ESKD)
Systemic disease!
Metabolic
CV
Respiratory
Hematologic
GI
GU
Neurologic
Musculoskeletal
Integumentary
CKD complications: Cardiovascular
HTN — bc patient’s kidneys can’t excrete Na+ and H2O very well
HF/hypervolemia
Accelerated alerosclerosis
Pericarditis
CKD complications: Hemotalogic
Anemia — d/t decrease EPO
Bleeding risk — d/t platelet dysfunction
CKD complications: Electrolyte and Acid-Base
Hyperkalemia
Metabolic acidosis
Hyperphosphatemia
Hypocalcemia — contributes to bone disease
CKD complications: Endocrine/Bone d/t hypocalcemia
Secondary hyperparathyroidism
CKD-Mineral Bone Disorder
Renal osterodystrophy
CKD complications: Neurologic
Peripheral neuropathy
Cognitive changes
Restless leg syndrome
Uremic encephalopathy
CKD complications: GI
N/V
Anorexia/weight loss
Uremic factor — ammonia breath
CKD complications: Dermatologic
Pruritus (itchy skin)
Uremic frost — crystallized urea on the skin bc there is so much urea in the body (“overflow”)
CKD complications: Immune System
impaired immunity = increased infection risk
CKD complications: Fluid balance
Edema
Pulmonary congestion
Difficulty diluting or concentrating urine
Nutritional therapy for ESKD
Calories and carbs
Protein recommendations
Na+, K+ and P
High calorie and high carb diet
Protein recommendations — before dialysis = restrict protein, on dialysis = replace protein
Restrict Na+, K+ and P
Fluid therapy in ESKD: Diuretics purpose
symptom control and fluid management
Loop diuretics ESKD contraindications
Anuria!
because they work by blocking sodium reabsorption in the kidneys
Severe dehydration
Hypovolemia
Severe electrolyte abnormalities
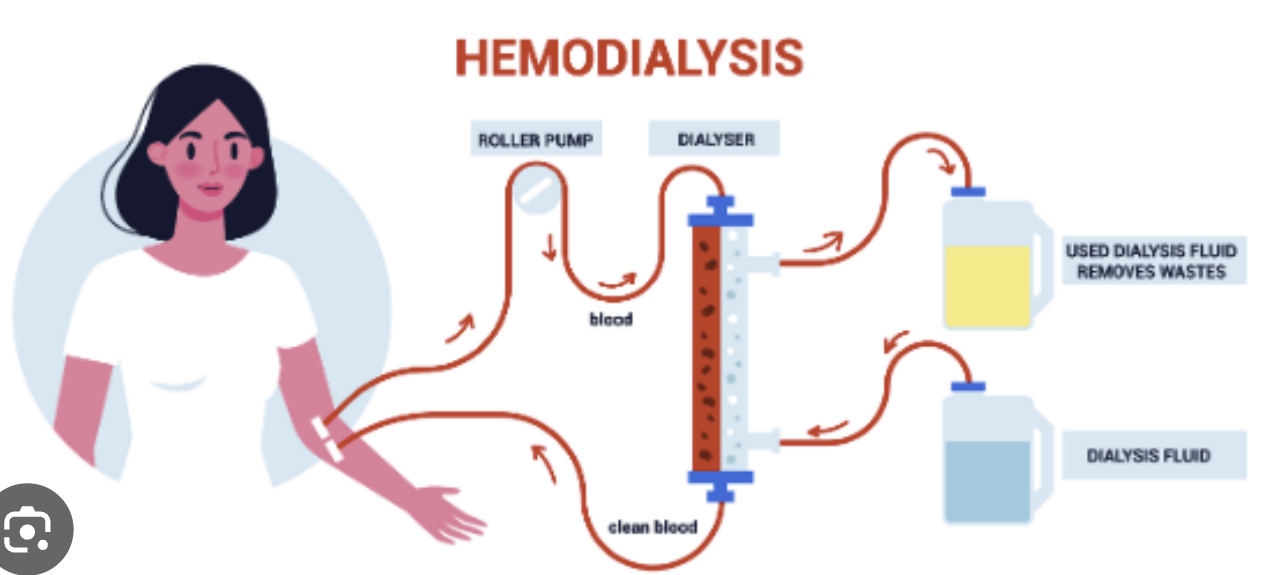
Hemodialysis
Life-sustaining treatment that uses an artificial kidney (dialyzer) to filter waste, extra fluid, and chemicals from the blood when kidneys fail, essentially acting as an external kidney to clean the blood and manage blood pressure
Small solutes that hemodialysis removes via diffusion (3) (hint — they are the most concerning ones for body function!)
Urea
Creatinine
K+
*Hemodialysis indications (AEIOU)
Acid-base imbalance
Electrolyte abnormalities (esp K+)
Intoxication (certain toxins)
Overload (fluid)
Uremia
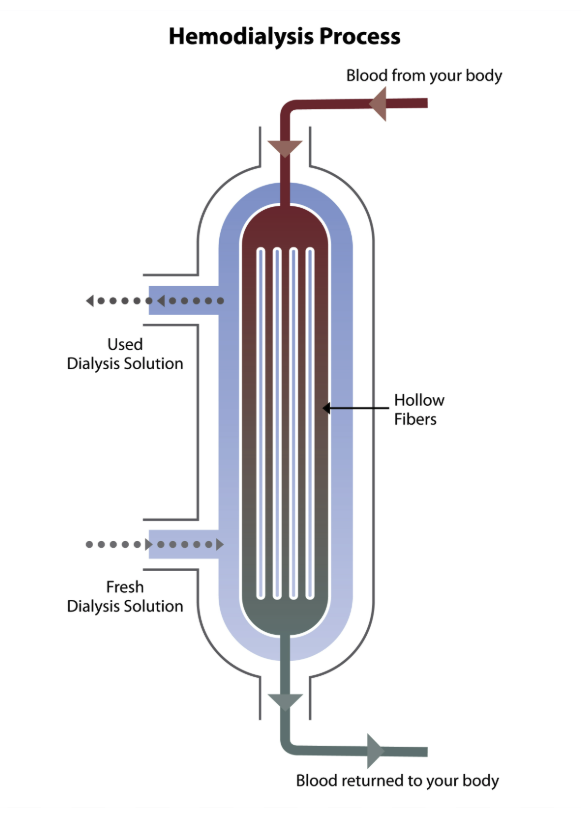
Dialyzer
2 compartments separated by a semipermeable membrane in which blood and dialysate flow in opposite directions, allowing for waste products and excess fluid to be removed from the blood
AV fistula vs AV graft
AV fistula connects an artery directly to a vein — 1st choice bc less invasive
AV graft connects an artery to a vein using a synthetic tube — external
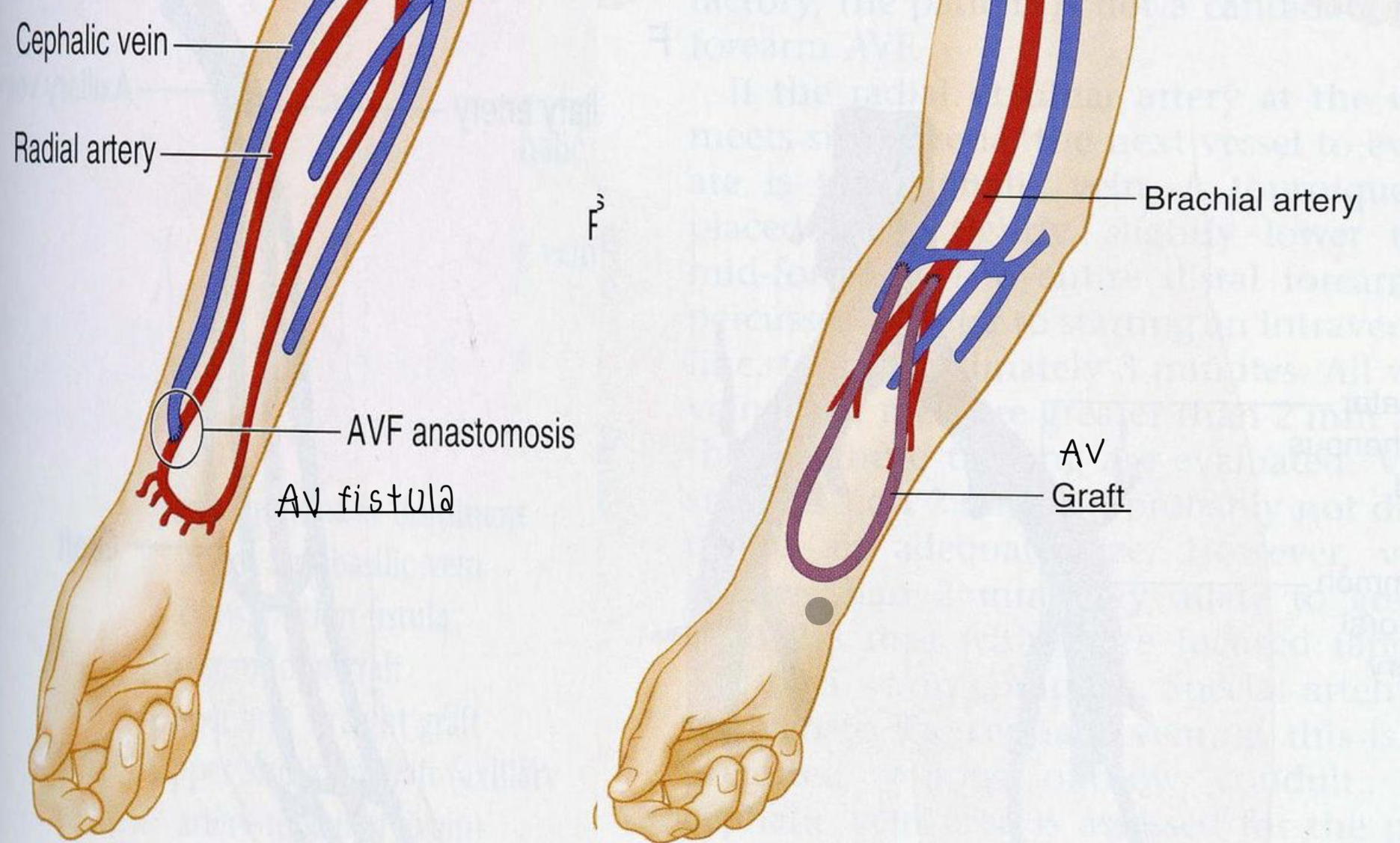
AV fistula precautions
Do not take BP in extremity
No venipunctures or IV access allowed
Assessment includes palpating for thrill and auscultating bruit — turbulent BF bc the connection of an artery and vein
Assess distal pulses
Assess for infection and bleeding
Patient instruction
No heavy lifting or activity that would compress access
Do not sleep on access arm
Hemodialysis complications
***Hypotension
Hypovolemia
Dialysis disequilibrium
Muscle cramps
Hemmorage
Air embolus
Hemodynamic changes
Cardiac dysrhythmias (d/t fluid and electrolyte shifts)
Infectious disease
Hemodialysis: Assessment at vascular access
Bruit and thrill — we WANT this because the hemodialysis is making the vessels abnormal
No BP/IV/lab draws on fistula arm
Intradialytic hypotension
hypotension that occurs during dialysis
most common complication of dialysis
Peritoneum
the serous membrane lining the cavity of the abdomen and covering the abdominal organs
Peritoneal Dialysis
exchange of wastes, fluids, and electrolytes via peritoneum by placing a catheter into the peritoneal cavity
Additives to peritoneal dialysis
Heparin — prevent clots blocking catheter
K+ — prevent hypokalemia
Antibiotics
Continuous Ambulatory Peritoneal Dialysis (CAPD)
infused 4-5 exchanges in 24 hours, dwells for 4-6 hours
Continuous Cyclic Peritoneal Dialysis
over 8-10 hours at night, allows patient to be dialysis free during the day
Peritonitis
Peritoneum becomes inflamed d/t connection site contamination
**must use sterile technique for prevention
Peritonitis symptoms
Fever
Abdominal tenderness + pain
Malaise
N/V
**Cloudy effluent
Peritoneal Dialysis nursing care
Use aseptic technique for dressing changes
Maintain accurate I & O and obtain dry weight when empty
Check BG and be aware of sneaky calorie load of dialysate — high glucose content in dialysate = increased “indirect” caloric intake
Warm dialysate to body temp (reduce discomfort and improve solute transfer)