Comprehensive Review of Hematologic and Lymphoid Neoplasms
1/248
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
249 Terms
What are the two main categories of disorders affecting white blood cells?
Proliferative disorders (reactive and neoplastic) and leukopenias.
What is found in peripheral smears for CML
proliferation of myeloid cells, in all stages of development
Describe the appearance of a Reed Sternberg cell
owl eyes, bilobed and binucleated
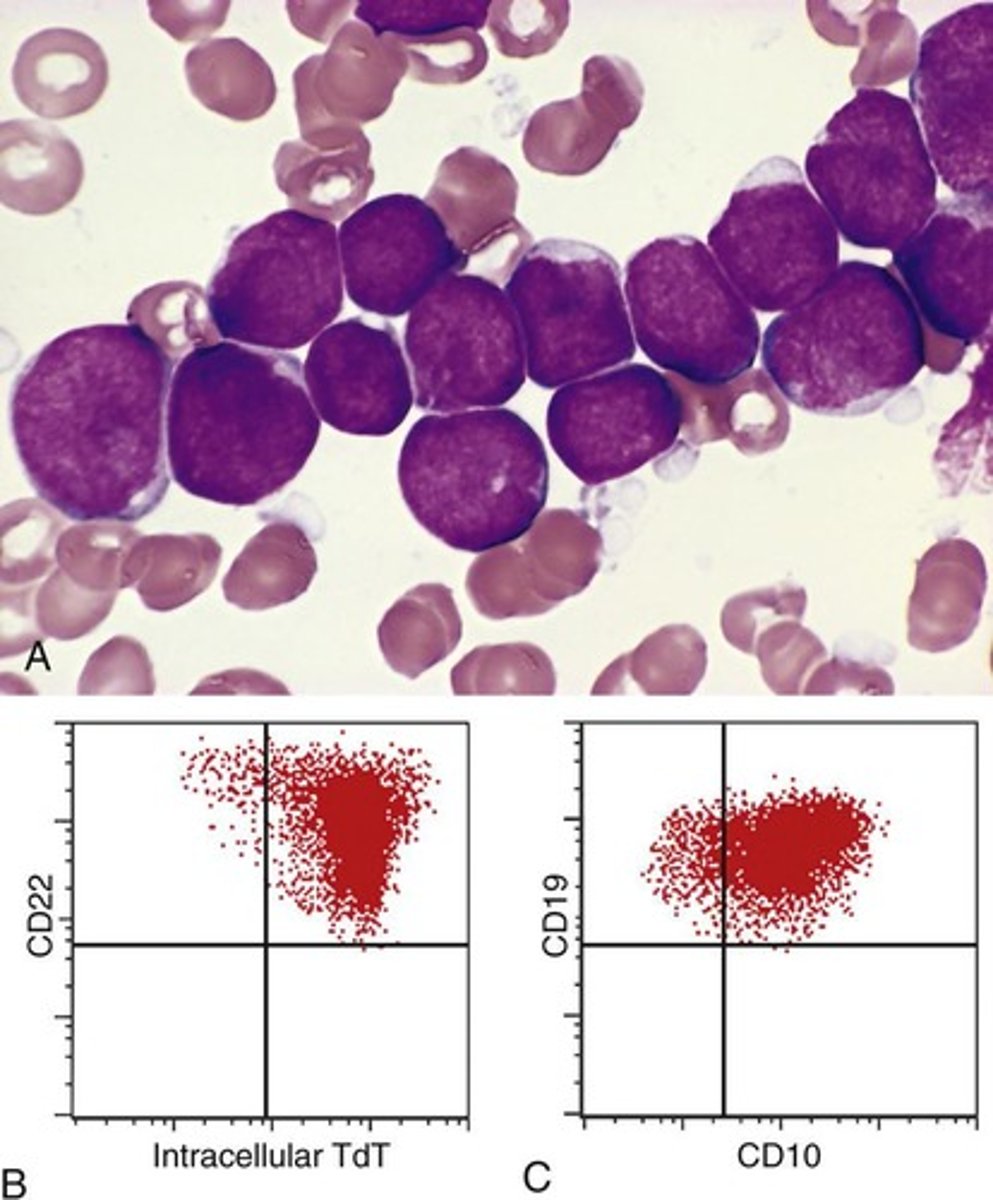
What diagnosis is MPO negative, Tdt positive, and PAS positive?
ALL
What is acute myeloid leukemia
an accumulation of immature myeloid forms in the bone marrow that suppress normal hematopoiesis
what is Myelodysplastic syndrome
defective maturation of myeloid progenitors, giving rise to ineffective hematopoiesis, leading to cytopenias
what is a myeloproliferative neoplasm
increased production of one or more types of blood cells
what was the diagnostic criteria for acute myeloid leukemia?
More than 20% blast cells in bone marrow, OR 10% in the periphery
What is a common comorbidity with AML?
DIC (which involves t(15:17) aka the PML-RARa translocation)
What are the numbers for serum Ig and Bence Jones associated with Multiple myeloma?
usually, more than 3 g/dL serum Ig, and 6 mg/dL Bence Jones protein in the urine
plasma cell neoplasms mechanism
the level of free light chains is elevated and skewed toward one light chain at the expense of the other.
What is leukopenia?
A decrease in white blood cells, which can include neutropenia and agranulocytosis.
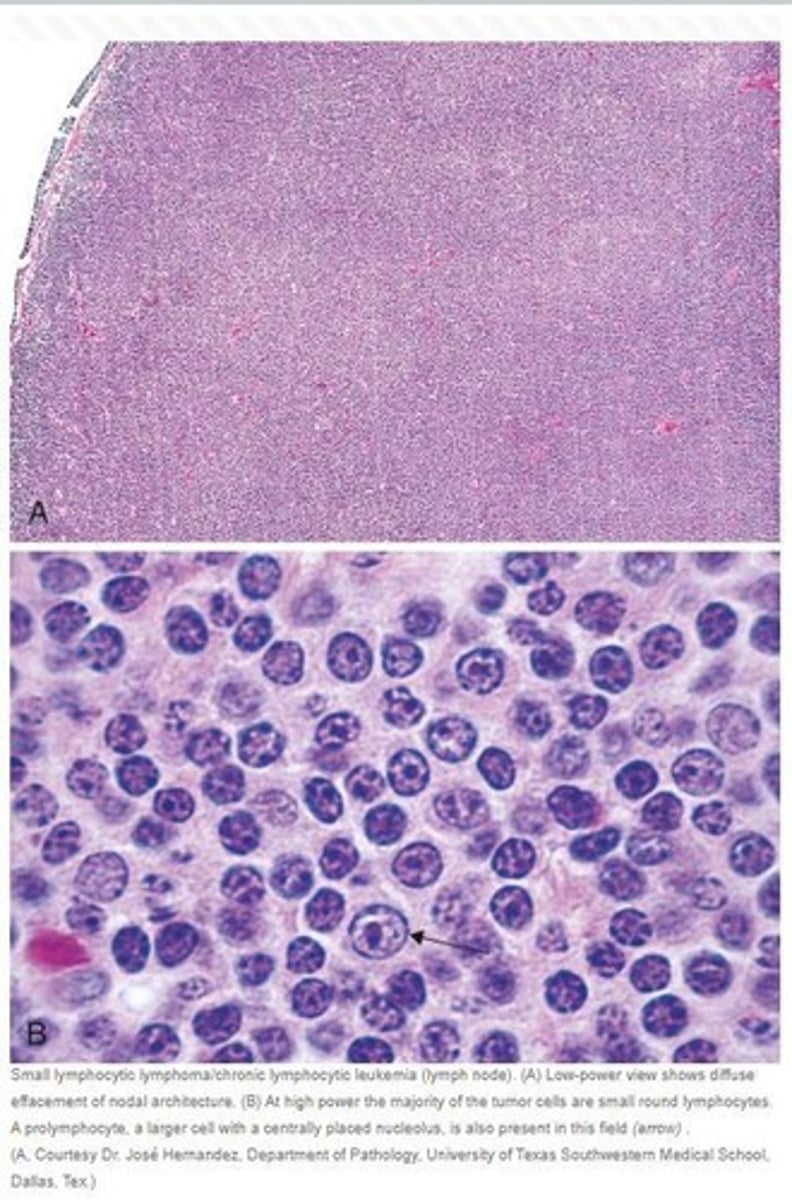
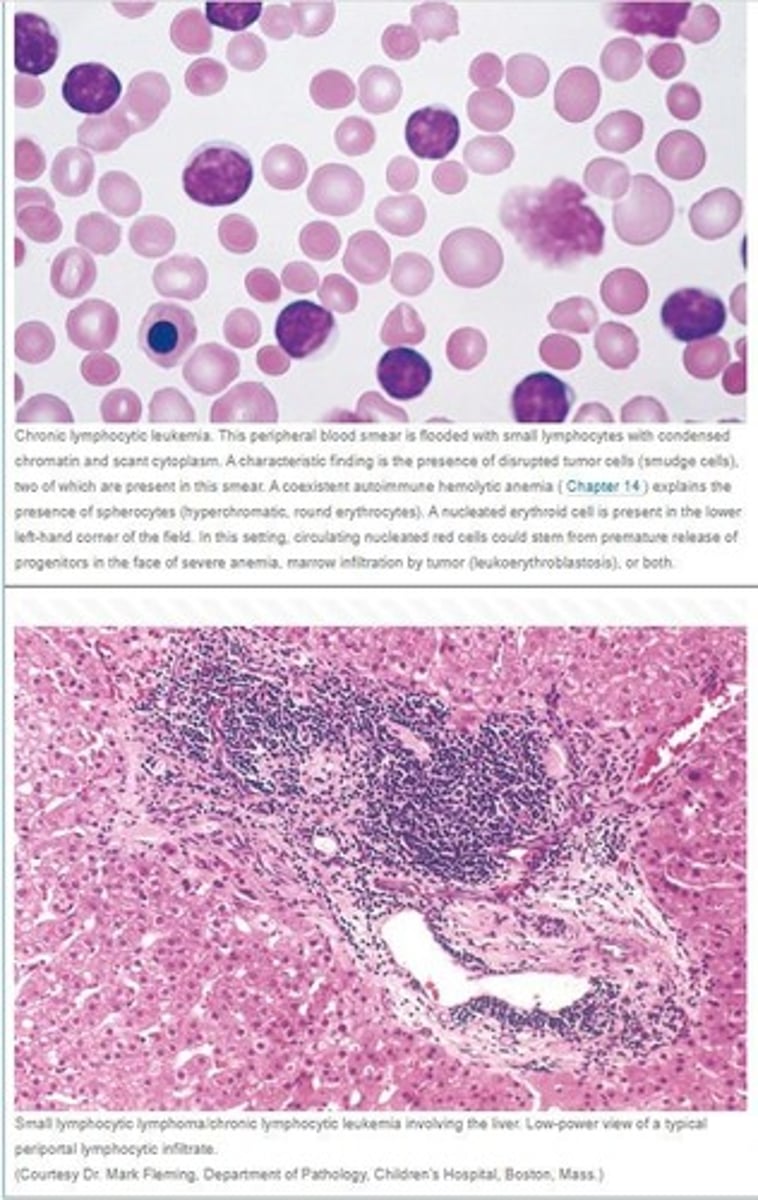
What are the characteristics of chronic lymphocytic leukemia (CLL)?
Most common adult leukemia, shows small, crushed lymphocytes in smears called smudge cells. CD19+, CD20+, CD23+, AND CD5+
What markers are typically expressed in chronic lymphocytic leukemia (CLL)?
CD19, CD20, CD 23 and CD5.
What is the most common form of non-Hodgkin's lymphoma?
Diffuse large B cell lymphoma.
What is Richter syndrome?
the transformation of CCL to diffuse large B-cell lymphoma. involves a rapidly enlarging mass within a lymph node or spleen
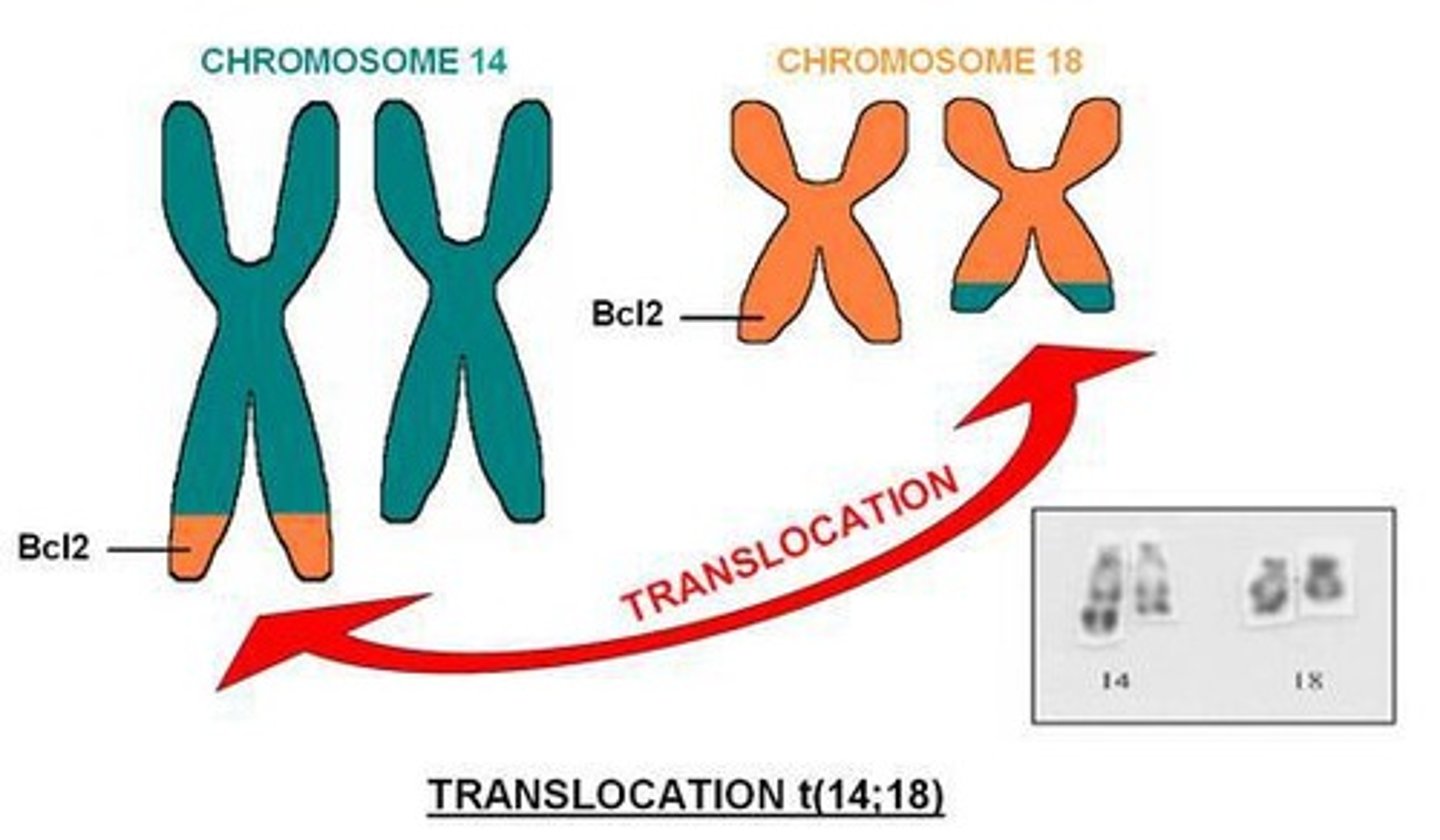
What are the key things to know about follicular lymphoma?
translocation (14:18) on BCL2 locus
expresses CD19, CD20, CD10, BCL6, and BCL2
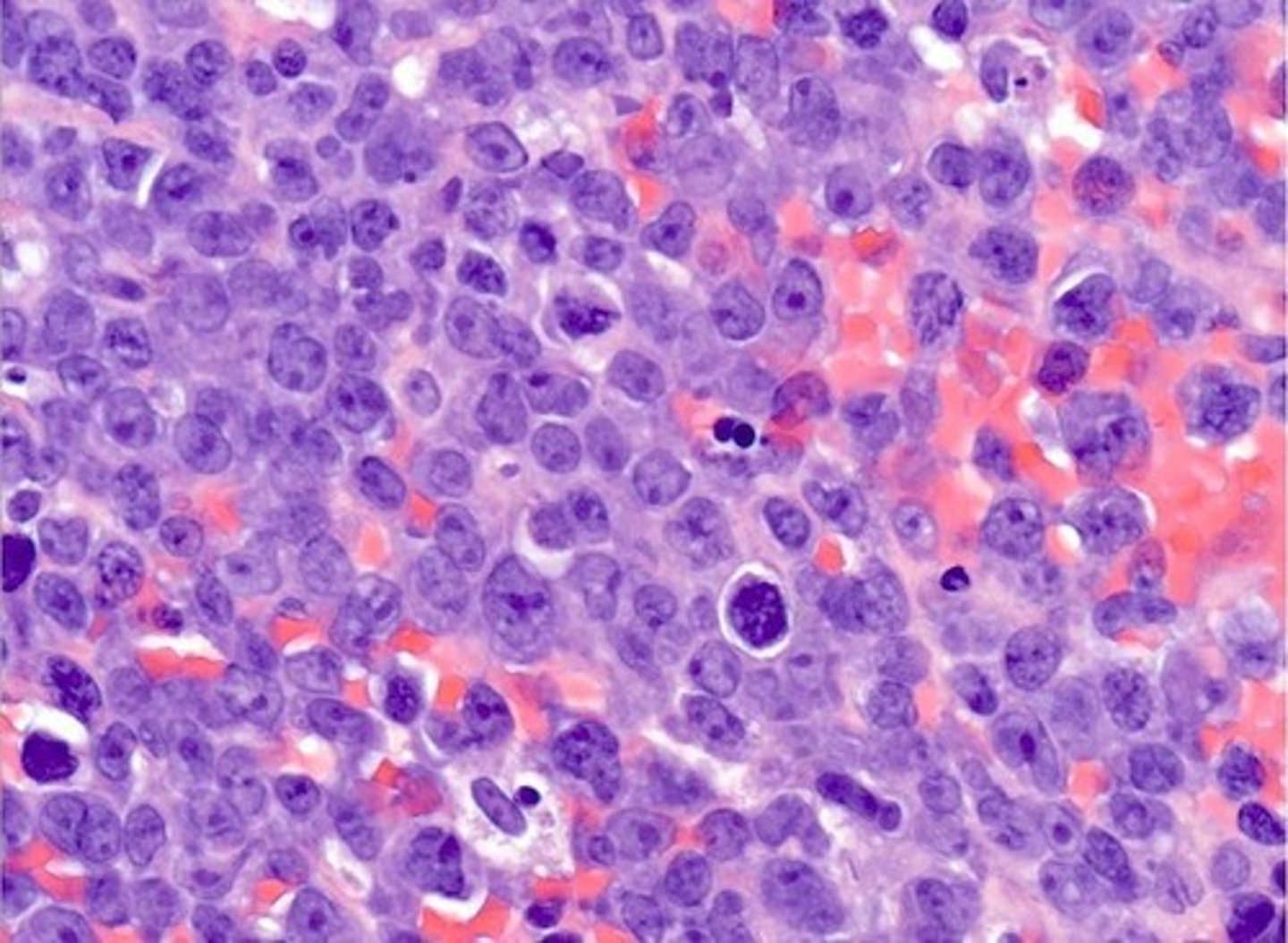
What genetic alterations are often associated with diffuse large B cell lymphoma?
dysregulation of BCL6
expresses CD10, CD19, CD20, and BCL6
What is the significance of the 'starry sky' morphology in Burkitt lymphoma?
It indicates the presence of macrophages in the tissue, typically associated with EBV infection.
What are the characteristics of marginal zone lymphoma (MALToma)?
Arise in tissues with chronic inflammation
Can remain localized for a long time
May regress if the inflammatory agent is eradicated.
What are the defining features of multiple myeloma?
End organ damage (CRAB: hypercalcemia, renal failure, anemia, lytic bone lesions) and neoplastic plasma cells secreting excess light chains.
What is the diagnostic significance of the presence of Reed-Sternberg cells?
They are required for the diagnosis of Hodgkin lymphoma. They induce accumulation of reactive lymphocytes
What is the role of JAK2 mutation in myeloid neoplasms?
It is commonly associated with myeloproliferative disorders and can lead to increased blood cell production.
What is the Philadelphia chromosome and its significance?
It is associated with chronic myeloid leukemia (CML) and results from a translocation between chromosomes 9 and 22.
What are the typical findings in acute myeloid leukemia (AML)?
Presence of blasts in the marrow and various genetic aberrations.
What is the clinical significance of 'CRAB' symptoms in multiple myeloma? What does CRAB stand for?
They indicate end organ damage due to the disease.
hyperCalcemia
Renal failure
Anemia
lytic Bone lesions
What are the common markers for Pre-B ALL?
CD19 and CD10.
What are the characteristics of histiocytic disorders?
They involve neoplastic proliferation of histiocytes and can present with aggressive symptoms.
What is the significance of light chain proteins in plasma cell neoplasms?
Excess light chains in urine can indicate multiple myeloma.
What is the typical presentation of lymphoid neoplasms?
They can present as enlarged lymph nodes, spleen, or liver, and may involve bone marrow.
What are the common symptoms associated with leukemias?
Fatigue, increased susceptibility to infections, and bleeding tendencies.
What is the role of cyclin D in lymphomas?
Overexpression of cyclin D is associated with certain aggressive lymphomas.
What are the characteristics of reactive proliferative disorders of white blood cells?
They involve expansion of leukocytes due to infection or inflammatory processes.
What defines neoplastic proliferative disorders of white blood cells?
They are less frequent and more serious than reactive disorders.
What are the two types of leukopenia?
Neutropenia and agranulocytosis.
What is the pathogenesis of leukopenia?
It can be due to ineffective granulopoiesis, which may involve suppression of hematopoietic stem cells.
What is diffuse large B-cell lymphoma?
A rapidly enlarging mass within a lymph node or spleen, often involving MYC genes.
What is Burkitt lymphoma characterized by?
translocation with MYC gene on chromosome 8 (typically t(8:14))
Starry sky morphology and association with EBV infection.
All endemic Burkitt lymphomas have EBV infection
What is the typical clinical presentation of marginal zone lymphoma (MALToma)?
Localized growth in tissues with a history of chronic inflammation.
What is the Philadelphia chromosome associated with?
Chronic myeloid leukemia (CML) and its characteristic findings.
What is the significance of CD138 in plasma cell neoplasms?
It is a marker used to identify neoplastic plasma cells.
What is the most common subtype of Hodgkin lymphoma?
Nodular sclerosis.
What is the typical presentation of acute myeloid leukemia (AML)?
Presence of myeloid blasts in the marrow and associated genetic aberrations.
What is the treatment for acute promyelocytic leukemia (APL)?
It is treated with retinoic acid and arsenic.
What is Langerhans cell histiocytosis characterized by?
Presence of characteristic granules in the cells and expression of CD1a and HLA-DR.
What is the significance of JAK2 mutations in myeloproliferative neoplasms?
They are commonly associated with conditions like polycythemia vera and essential thrombocythemia.
What is the prognosis for patients with high white blood cell counts in acute leukemia?
It is generally poor.
What are the two types of proliferative disorders?
Reactive (due to infection or inflammation) and neoplastic (less frequent, more serious).
What is neutropenia?
A specific type of leukopenia characterized by a low number of neutrophils.
What can cause leukopenia?
Ineffective granulopoiesis, suppression of hematopoietic stem cells, or exposure to drugs.
What is chronic lymphocytic leukemia (CLL)?
The most common adult leukemia, characterized by lymph node enlargement and small, crushed lymphocytes in smears.
What markers are expressed by tumor cells in chronic lymphocytic leukemia?
CD19 and CD20.
What is diffuse large B cell lymphoma?
A rapidly enlarging mass within a lymph node or spleen, often associated with MYC gene involvement.
What are flame cells and Russell bodies?
Cells seen in multiple myeloma; flame cells are plasma cells with a distinct appearance, and Russell bodies are abnormal immunoglobulin accumulations.
What is the significance of the Philadelphia chromosome in myeloid neoplasms?
It is associated with chronic myeloid leukemia (CML) and indicates a specific genetic abnormality.
it is BCR-ABL due to reciprocal (9:22)(q34:q11) translocation
What is the role of JAK2 mutation in myeloproliferative disorders?
It is commonly associated with disorders like polycythemia vera and essential thrombocythemia, leading to increased blood cell production.
What are the typical findings in the bone marrow of patients with myelodysplastic syndromes?
Dysplastic changes in blood cells, ineffective hematopoiesis, and possible cytopenias.
What is the common presentation of T cell lymphomas?
Aggressive tumors that may present with skin lesions and can spread to the blood.
What is the role of macrophages in the histology of lymphomas?
Macrophages may be present in the tumor microenvironment and can indicate certain types of lymphoma.
What is the typical cytological finding in chronic lymphocytic leukemia?
Crushed little lymphocytes in blood smears.
What is the treatment approach for lymphoid neoplasms?
Varies based on the type and stage of the disease, often involving chemotherapy or targeted therapies.
What is ineffective hematopoiesis and name two conditions associated with it?
Ineffective hematopoiesis refers to the impaired production of blood cells, associated with conditions such as megaloblastic anemia and myelodysplastic syndrome.
What is Kostmann syndrome?
Kostmann syndrome is a rare congenital disease characterized by severe neutropenia.
What is leukopenia and what are its two main forms?
Leukopenia is a decrease in white blood cells, with neutropenia and agranulocytosis being the two main forms.
What is the most common cause of agranulocytosis?
The most common cause of agranulocytosis is drug toxicity, particularly from alkylating agents and antimetabolites.
How does neutropenia manifest and what can it lead to if severe?
Neutropenia manifests as increased susceptibility to infections and, if severe, can lead to death.
At what absolute neutrophil count (ANC) do serious infections typically occur?
Serious infections occur when the ANC is below 500/mm3.
What is the treatment for neutropenia?
Treatment for neutropenia includes broad-spectrum antibiotics and granulocyte colony-stimulating factor (G-CSF).
What causes acute nonspecific lymphadenitis?
Acute nonspecific lymphadenitis is caused by infections and is usually painful.
What are the characteristics of chronic nonspecific lymphadenitis?
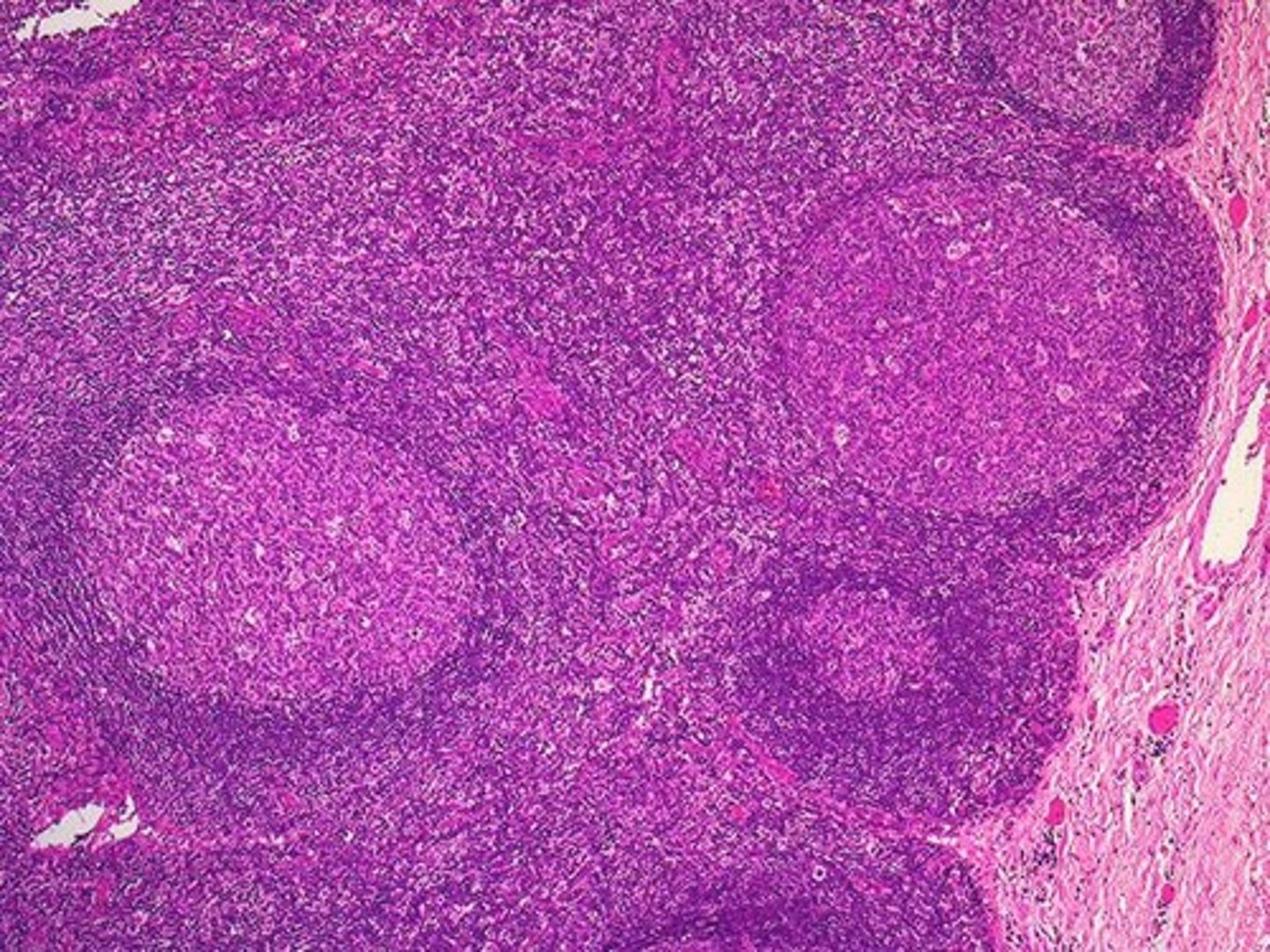
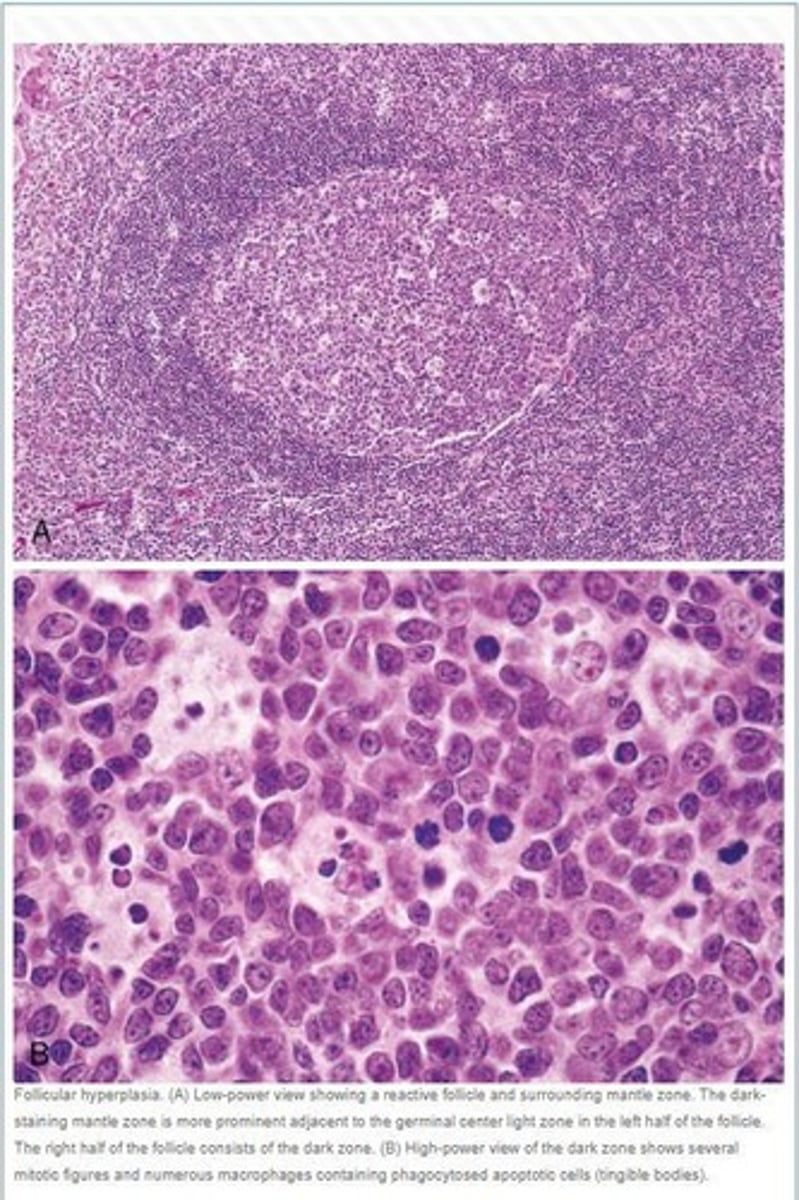
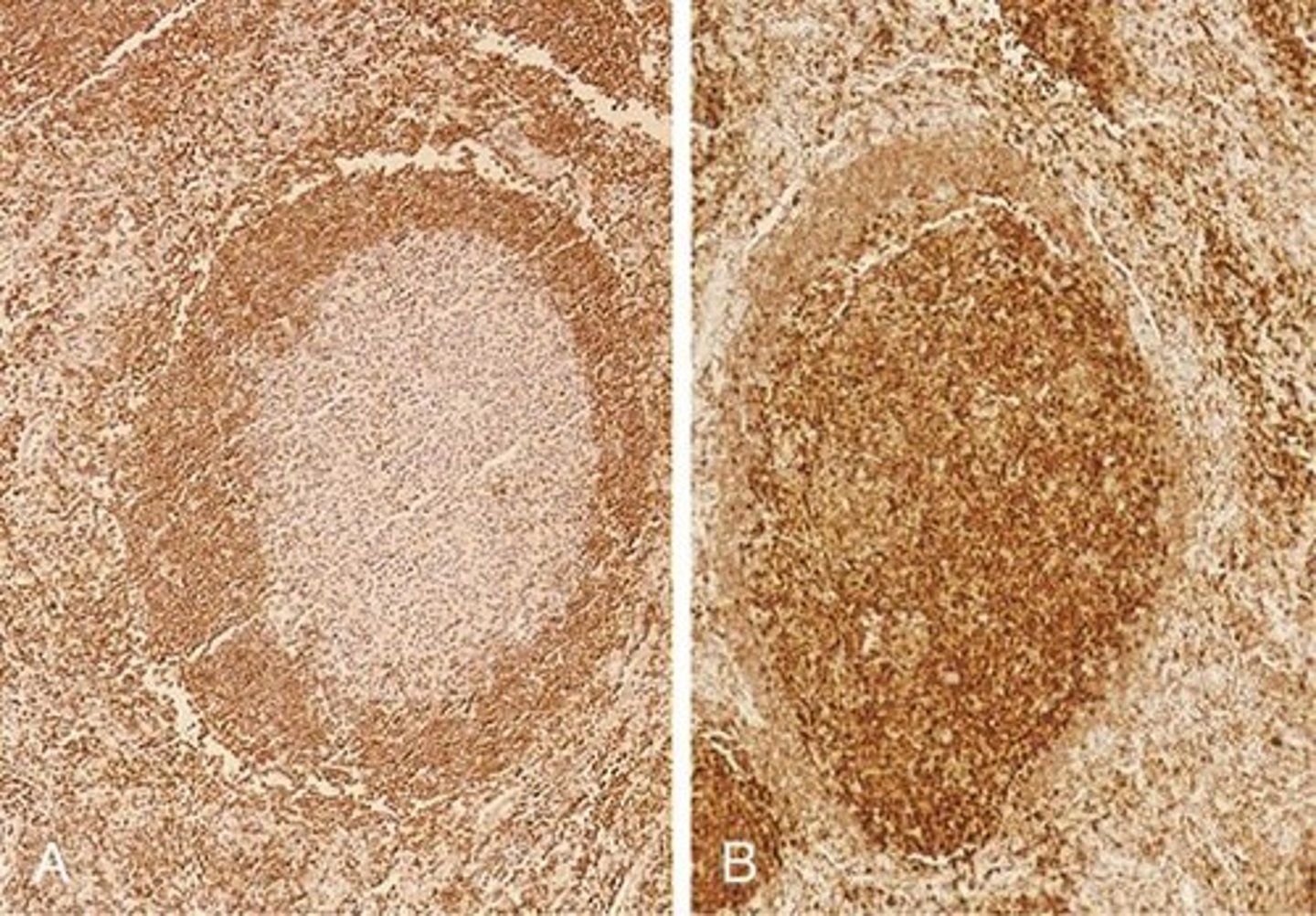
Chronic nonspecific lymphadenitis features follicular hyperplasia due to stimuli activating humoral immune responses.
What are the two distinct regions of germinal centers in lymph nodes?
The two regions are the dark zone, containing proliferating blast-like B cells (centroblasts), and the light zone, composed of B cells with irregular or cleaved nuclear contours (centrocytes).
What are some causes of follicular hyperplasia?
Causes of follicular hyperplasia include rheumatoid arthritis, toxoplasmosis, and early HIV infection.
What features favor a reactive (nonneoplastic) hyperplasia in lymph nodes?
Features include preservation of lymph node architecture, variation in follicle shape and size, and presence of phagocytic macrophages.
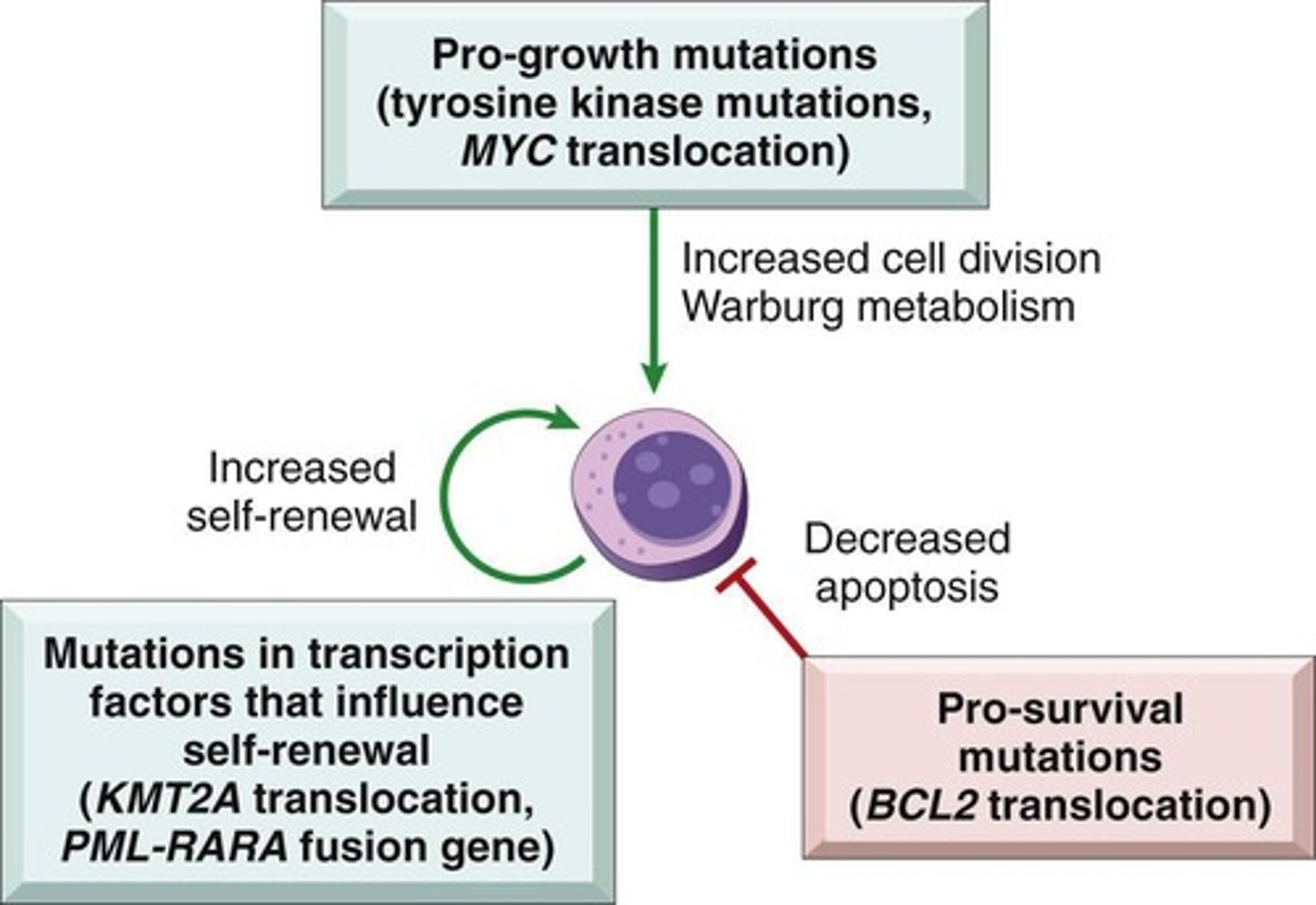
What are some pathogenetic factors in white cell neoplasia?
Pathogenetic factors include chromosomal translocations, acquired mutations, inherited genetic factors, viral infections, chronic inflammation, iatrogenic factors, and smoking.
Which viruses are associated with specific types of white cell malignancies?
HTLV-1 is associated with adult T-cell leukemia/lymphoma, EBV with Burkitt lymphoma and Hodgkin lymphoma, and HHV-8 with Kaposi sarcoma.
How does smoking affect the incidence of acute myeloid leukemia (AML)?
Smoking increases the incidence of AML twofold due to exposure to benzene.
What is the role of oncoproteins in white cell malignancies?
Oncoproteins block normal maturation, activate pro-growth signaling pathways, or protect cells from apoptosis, leading to rapid proliferation.
What is the impact of chronic inflammation on lymphocyte malignancies?
Chronic inflammation, such as from H. Pylori infection, can lead to gastric B-cell lymphoma and other lymphocyte malignancies.
What is the significance of genetic diseases like Bloom syndrome and Fanconi anemia in white cell neoplasia?
These genetic diseases promote genomic instability, increasing the risk of developing white cell malignancies.
What are the characteristics of acute lymphadenitis?
Acute lymphadenitis is characterized by swollen, painful lymph nodes, often with redness of the skin.
What is the difference between acute and chronic lymphadenitis?
Acute lymphadenitis is usually painful and caused by infections, while chronic lymphadenitis involves follicular hyperplasia and is often less painful.
What are lymphoid neoplasms derived from?
Lymphocytes (B-cells, T-cells, and NK cells)
What are myeloid neoplasms derived from?
Myeloid cells (granulocytes, monocytes, red blood cells, platelets)
What are the 5 subclasses of Hodgkin lymphomas? Which ones are classic?
Classical Hodgkin lymphomas include Nodular sclerosis, Mixed cellularity, lymphocyte-rich, and lymphocyte-depleted.
Nodular Lymphocyte predominant is the non-classic form
What is the significance of monoclonality in lymphoid neoplasms?
All daughter cells derived from the malignant progenitor share the same antigen receptor gene configuration and sequence.
What percentage of lymphoid neoplasms are of B-cell origin?
80-90%.
What is the role of flow cytometry in lymphoid neoplasms?
It is used for detection of lymphoid neoplasms.
Which antigen is associated with all leukocytes?
CD45, also known as leukocyte common antigen (LCA).
What does CD19 indicate in lymphoid neoplasms?
It is associated with pre-B cells and mature B cells, but not plasma cells.
What is the function of CD30 in lymphoid neoplasms?
It is an activation marker present on activated B cells, T cells, and monocytes.
What is the primary characteristic of normal immune responses compared to lymphoid neoplasms?
Normal immune responses are comprised of polyclonal populations of lymphocytes, while lymphoid neoplasms are monoclonal.
What is the role of immunohistochemistry in lymphoid neoplasms?
It is used alongside flow cytometry for the detection of lymphoid neoplasms.
What is the antigen designation for helper T cells?
CD4.
Which antigen is associated with cytotoxic T cells?
CD8.
What is the function of CD21 in lymphoid neoplasms?
It acts as an EBV receptor and is found on mature B cells and follicular dendritic cells.
what are the distinct cell markers on hairy cell leukemias
CD11c, CD25, CD103, and annexin A1.
(along with CD 19 and 20)
What is the significance of CD34 in lymphoid neoplasms?
It is associated with pluripotent hematopoietic stem cells and progenitor cells of many lineages.
What is the primary characteristic of lymphoid neoplasms in terms of antigen receptor proteins?
They synthesize identical antigen receptor proteins.
What is a common feature of white cell proliferations in lymphoid neoplasms?
They present as discrete tissue masses.
What is the typical presentation of leukemia compared to lymphoma?
Leukemia presents with widespread involvement of the bone marrow and peripheral blood, while lymphoma typically presents as tissue masses.