MMD I: Week 4 (Neck CPGs & CPRs)
1/33
Earn XP
Description and Tags
Exam 2 Content
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
20% of the brain’s blood supply is provided by this artery, which travels through the C6-C1 transverse foramina
Vertebral artery
What does the neck disability index (NDI) measure?
Measures how neck pain has impacted everyday life (pain intensity, personal care, lifting, headaches, concentration, work, driving, sleeping, and recreation)
MCID for NDI
5 to 10 points (10% to 20%)
What does the Patient Specific Functional Scale (PSFS) measure?
Patient selects 3 activities they are unable to do/are limited due to their neck pain, and they rank how well they can do said activy on a sclae form 0-10
MCID for the PSFS
2 points average / 3 points per single activity
MCID for the Numeric Pain Rating Scale (like VAS)
2 points
What does the Global Rating of Change (GROC) measure?
A patient's subjective perception of health or functional change over time, typically from their perspective at the start of treatment to their current status.
MCID for GROC
3 points
Moderate: 4 or 5 points
Significant: 6 or 7
What are he 2 highest evidence risk factors for poor prognosis according to the CPG?
Femal sex
Prior history of neck pain
Recovery is the fastes in the first ____ to _____ months. It slows down after ____ months
6 to 12 months / 12 months
Expected physical examination findings for Mobility Deficits classification:
Limited Cx ROM
Passive and active end-range pain
Central and unilateral pain
May have UE pain referral
Pain with segmental provocation
Strength and motor control deficits (subacute - chronic)
Expected physical examination findings for Movement Coordination Impairments classification:
(+) Cranial Cervical Flexion Test (CCFT)
(+) DNF Endurance Test
(+) Pressure algometry
(+) Strength and endurance deficits
MID range pain, worsens at end range
Hx of trauma/whiplash
UE pain referral
TTP trigger points
Sensorimotor impairment
Concentration, memory issues
Hypersensitivity
Expected physical examination findings for Cervicogenic Headaches classification:
(+) Cervical Flexion-Rotation Test
HA with segmental provocation
non-continuous unilateral neck pain + headache
HA triggered by movement or by sustained position
Limited Cx ROM
Restricted upper cervical segmental mobility
Strength, endurance, and coordination deficits
Expected physical examination findings for Radiating Pain classification:
(+) Test cluster: ULTT, Spurling’s, Cervical distraction, and limited Cx ROM
UE sensory, strength or neuro deficits
Dermatomal paresthesia
Myotomal weakness
Tests and measures for Mobility Deficits classification:
ICD: Cervicalgia or pain in the thoracic spine
Cervical AROM
Cervical and thoracic segmental mobility
Tests and measures for Movement Coordination Impairments classification:
ICD: Sprain and strain of cervical spine
Cranial cervical flexion test
DNF endurance test
Deep cervical extensors
Tests and measures for Cervicogenic Headaches classification:
ICD: Headaches or cervicocranial syndrome
Cervical AROM (upper>lower cx spine ROM)
Cervical segmental mobility
Cranial cervical flexion test
Tests and measures for Radiating Pain classification:
ICD: Spondylosis with radiculopathy or cervical disc disorder with radiculopathy
ULTT
Spulring’s Test
Cervical Distraction
Interventions for Mobility Deficits classification (B and C level):
Thoracic manipulation
++Acute and chronic
Cervical manipulation
++Chronic
Cervical mobilization
++Chronic
Cervical ROM
++Acute
UQ Strengthening and Stretching
NM Exercise
++Chronic
DN, intermittent traction
++Chronic
T/F: Manual therapy combined with exercise was proven more effective at reducing neck pain than manual therapy alone
True
Thoracic spine thrust manipulation can be used for reducing pain and disability in patients with ____________ ____ ______
Neck-related arm pain
What is something you should ALWAYS do after manipulation techniques?
Provide ROM exercises (UT & levator stretch, DNF strenghtening)
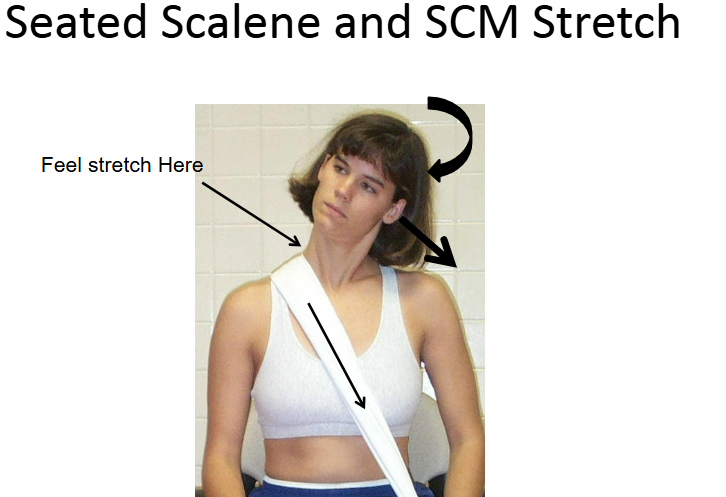
What are the suggested muscles targeted for stretching/flexibility interventions?
Scalenes
OA ext, SB and CL ROT
UT
SB away and ROT towards
Levator Scap
SB + ROT towards + depression
Pecs
Doorway stretch
Interventions for Movement Coordination Impairments classification:
ROM with strengthening + postural exercises
++ Acute
MINIMIZE collar use
++ Acute
Combined Manual Therapy and Exercise
++ Acute, + Chronic
TNMES
Education on prognosis
++Acute, + Chronic
Average recovery for WAD is:
2-3 months
Interventions for Cervicogenic Headaches classification:
Active Mobility
++Acute
Upper cx self glides
Cervical manipulations
++ Subacute and chronic
Thoracic Thrust
++ Chronic
Manual + ST strength and endurance
++ Chronic
Interventions for Radiating Pain classification:
Exercise with mobilizing and stabilizing
++Chronic, +Acute
Low level laser
Possible short term collar
Manual therapy + exercise
++ Chronic
Intermittent traction
++ Chronic
CPR - For identifying individuals with cervical radiculopathy
(+) Spurling’s
(+) Radiating sx relief with cervical distraction
(+) ULTT
ROM <60° on involved side
LR: +30.3 (All 4 variables)
CPR - For identifying individuals with neck pain likely to respond to mechanical cervical traction
Age > 55
(+) shoulder abduction test
(+) ULTT
Symptom peripheralization with lower cervical (C4-C7) PA motion testing
(+) Neck distraction test
> 4 variables present: +LR = 11.7
CPR - For identifying individuals with neck pain likely to respond to thoracic spine manipulation
Symptoms < 30 days
No symptoms distal to the shoulder
Looking up doesn’t worsen symptoms
FABQPA < 12
Diminished upper thoracic kyphosis T3-T5
Cervical Extension ROM < 30
>3 variables present: +LR = 5.5
When does the clinical reasoning pause #1 happen?
After gathering general information → you formulate an initial hypothesis
When does the clinical reasoning pause #2 happen?
After gathering patient goals (end of subjective)→ you modify your hypothesis, establish SINSS, and plan physical exam
Shoulder Abduction Sign (Bakody’s Sign)
Relief of upper extremity radicular sx
Flexed/abducted position
Resting arm on head
Typically C5/6/7 nerve root
What are the regionally specific questions to ask for the SE (Cx Spine)?
Hx of headaches
Vision changes
Referred/radiating sx