Alterations in Hemodynamic Stability: Shock
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
87 Terms
Shock
Life-threatening
- syndrome caused by alteration in tissue perfusion and impaired cellular metabolism
- results in imbalance between supply of & demand of O2 + nutrients
4 Main Categories of Shock
Cardiogenic
Hypovolemic
Distributive
Obstructive
Hypovolemic Shock
Occurs from inadequate fluid volume in the intravascular space
- most common type of shock
How does hypovolemic shock occur?
Loss of blood (most common)
- traumatic bleeding
Fluid losses
- severe burns
- severe diarrhea &/vomiting
- renal losses
- third spacing
Absolute Hypovolemic Shock
Fluid lost through:
- Hemorrhage
- Gastrointestinal (GI) loss (e.g., vomiting, diarrhea)
- Fistula drainage
- Diabetes insipidus
- Diuresis
Relative Hypovolemic Shock
Occurs when fluid volume moves out of the vascular space into the extravascular space
- aka third spacing
- bowel obstruction
- internal bleeding
- ascites
Pt's response to Acute Volume Loss
Depends on several factors:
- extent of injury
- age
- general state of health
Up to 15% of Total Blood Volume Loss (750 mL)
Pt can compensate
Up to 15%-30% Blood Loss
Results in SNS mediated response
- increase in HR, CO, RR and depth
- decrease in SV, CVP & PAWP
> 30% Volume Loss
Compensatory mechanism may fail
- immediate replacement with blood products should be started
> 40% Volume Loss
Loss of autoregulation in microcirculation & irreversible tissue destruction
Early S&S of Hypovolemic Shock
Irritability
Tachycardia
Slight Tachypnea
Pink to Pale Skin change
Dry mucous membranes
Compensation of Early Hypovolemic Shock
Decrease Preload, PAP, PAWP, CO
- increased SVR & afterload --> due to vasoconstriction of vessels
Acid-Base Imbalance --> respiratory alkalosis & metabolic acidosis
Later S&S of Hypovolemic Shock
- Altered mental status
- HypoTN (more profound)
- Rapid, weak, thready pulse & bradycardic
- Cool, clammy skin
- Rapid + shallow respirations
- Hypothermia
- Cold + mottled skin (esp. extremities)
- Anxiety & restlessness
- Oliguria to anuria
Decompensation of Later Hypovolemic Shock
Decreased Preload (CVP)
PAP
PAWP
CO
SVR
Afterload
What is always include in tx plan, no matter the type of shock?
Supplemental O2
Tx of Hypovolemic Shock: Hemorrhagic
1. Supplemental O2
2. Rapid fluid resuscitation
3. Hypertonic - 3% & 6% NaCL
- given via central line
4. Crystalloids (Sodium Chloride [0.9%] or LR)
5. Colloids (will depend on pt)
6. Plasma and albumin
- albumin is hypertonic
7. Polysaccharide (Dextran), Polygeline & hetastarch (Hespan) - synthetic blood products
8. Blood Replacements
9. Repair of the problem
Tx of Hypovolemic Shock: Non-Hemorrhagic
1. Supplemental oxygen
2. Isotonic IV Fluids / Hypertonic Fluids
3. PRBC'S
4. Vasopressin
- will help promote/bring up BP
5. Antiemetics
6. Antidiarrheals
Resuscitation Fluid Requirements for Adults
1-2L isotonic IV fluids as initial bolus
Warm blood & fluids (if appropriate)
Why are cold IV Bags bad?
Can cause vasospasms and drop in BP & body temp
Metabolic Acidosis
Occurs in long standing or severe shock
- do not routinely use sodium bicarb to see if it corrects acidosis
What does a correction of Metabolic Acidosis result as?
Results of improved perfusion and tissue oxygenation
Cardiogenic Shock
Occurs when either systolic or diastolic dysfunction of the heart's pumping action causes:
- reduced CO, SV and BP
- often called "pump failure"
- compromised CO
Systolic Dysfunction
The heart's inability to pump blood forward
Diastolic Dysfunction
↓ filling of the heart resulting in ↓ stroke volume
Causes of Cardiogenic Shock
MI (most common)
HF
Cardiomyopathy
Dysrhythmias
Severe systemic or pulmonary HTN
Pericardial tamponade
Tension pneumothorax
PE
Myocardial depression from metabolic problems
Systolic Dysfunction Pathophysiology
Ineffective forward movement of blood → ↓ SV, ↓ CO → ↓ Cellular O2 supply → ↓ Tissue perfusion → Impaired Cellular metabolism
Diastolic Dysfunction Pathophysiology
Ineffective filling → ↑ Pulmonary pressure → Pulmonary edema → ↓ Oxygenation → ↓ Cellular O2 supply → ↓ Tissue perfusion → Impaired cellular metabolism
Early Manifestations of Cardiogenic Shock
Tachycardia
HypoTN
↑ Myocardial O2 consumption
- ↑ in SVR
Narrowed pulse pressure
Signs and Symptoms of Cardiogenic Shock
- Tachypnea
- Crackles on breath sounds
- ↑ in PAWP, SVV, PVR
- Signs of peripheral hypoperfusion
- Decreased renal blood flow
- Impaired cerebral perfusion
Signs of Peripheral Hypoperfusion
Cyanosis
Pallor
Weak peripheral pulses
Cool and clammy skin
Delayed capillary refill
Decreased Renal Blood Flow
Results in:
- Sodium and water retention
- Decreased urine output
Causes of Impaired Cerebral Perfusion
Anxiety
Confusion
Agitation
Compensation for Cardiogenic Shock
Low BP + HR = Low CO
- so SNS kicks in and creates vasoconstriction
- CVP & wedge pressure will be high
Additional S&S w/ Cardiogenic Shock
Chest Pain
SOB
JVD (due to backup of blood)
Weak/absent pulse
Dysrhythmias
Increased Preload (CVP), PAP, PAWP, SVR + afterload
Decreased CO
Tx for Cardiogenic Shock
Supplemental O2
Inotropic drugs
Vasodilators
Diuretics
Thrombolytic therapy
IABP (balloon pump)
VAD
Heart transplant
Tx for Cardiogenic Shock: Labs
H&H
Electrolytes
BUN
Creatinine
Tx for Cardiogenic: Inotropic Drugs
Dopamine & Dobutamine
Tx for Cardiogenic: Vasodilators
NTG (nitroglycerin)
- vasodilates
- will help decrease backup of blood
Tx for Cardiogenic Shock: Diuretics
Not only decrease blood volume, also decreases workload on heart
- the heart can pump more blood forward & less volume to shift into lungs (no pulmonary edema)
Tx for Cardiogenic Shock: IABP (balloon pump)
- In cardiogenic shock --> no afterload & increased SVR (due to vasoconstriction)
- W/ tx of balloon pump --> decreased SVR due to increased movement of blood
NSG Interventions for Cardiogenic Shock: Limit Myocardial Oxygen Demand & Consumption
- Administer analgesics and sedatives.
- Position the patient in position of comfort.
- can open their lung & be comfortable
- Limit activities.
- Reduce anxiety; calm, quiet environment.
- stress & anxiety increased SNS response
NSG Interventions for Cardiogenic Shock: Enhance Myocardial Oxygen Supply
- Administer oxygen.
- Monitor respiratory status.
- Administer medications as prescribed.
NSG Intervention for Cardiogenic Shock
- Monitor pt's response to tx
- Tx the cause
Anaphylactic Shock
Acute, life-threatening hypersensitivity (allergic) reaction to a sensitizing substance
- drug
- chemical
- vaccine
- food
- insect venom
What does Anaphylactic Shock cause?
Quickly causes:
- massive vasodilation
- release of vasoactive mediators
- increase in capillary permeability (fluid leaking to vascular space)
What can Anaphylactic Shock Lead to?
Can lead to:
- Respiratory distress due to laryngeal edema or severe bronchospasm
- Circulatory failure from the massive vasodilation
2 Major Issues w/ Anaphylactic Shock
Major drop in BP
Fluid vascular shift
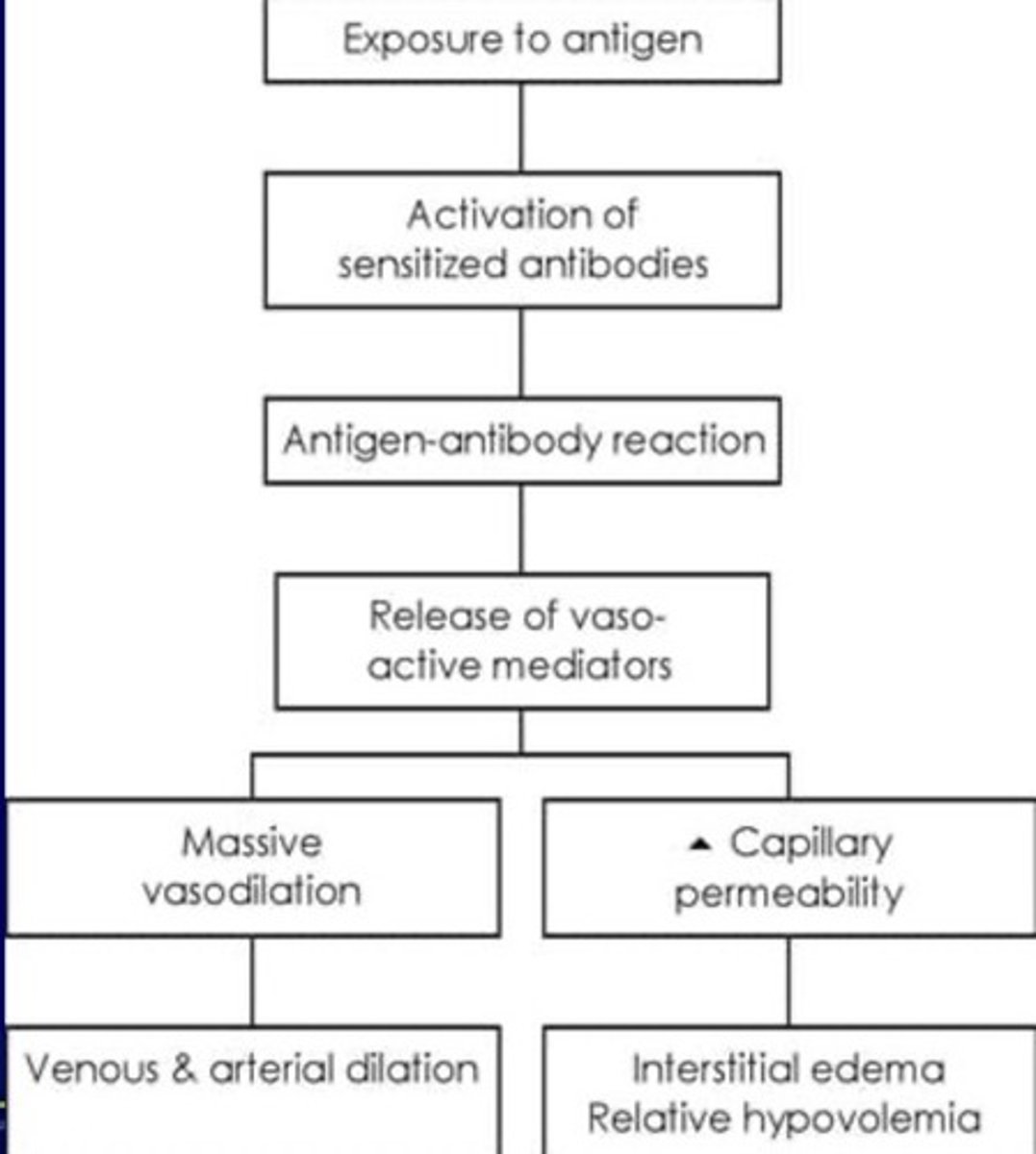
Patho of Anaphylactic Shock
Anaphylactic Shock S&S: Skin Changes
Skin eruptions and hives
Flushing of skin
Pruritus
Urticaria
Angioedema
Anaphylactic Shock S&S: Other S&S
Dizziness
Chest pain
Incontinence
Swelling of lips & tongue
Wheezing
Stridor
Weak & rapid pulse
Localized edema (esp. around face)
Breathlessness & cough (due to bronchoconstriction)
Anaphylactic Shock S&S: Hemodynamic
Decreased:
- preload (CVP)
- PAP
- PAWP
- CO
- SVR
- afterload
Tx for Anaphylaxis Shock
1. Airway management & supplemental O2
2. Administer Catecholamines (Epi), Antihistamines (Benadryl), Bronchodilators, Corticosteroids
Use of Catecholamines (Epinephrine) for Anaphylaxis Shock
Will be an increase in HR and vasoconstriction
- make sure to teach pts this is a normal response
Sepsis
Severe illness in which the bloodstream is overwhelmed by bacteria
Common Sepsis Sites
- Bowel (peritonitis)
- Kidneys (UUTI or pyelonephritis)
- Lining of brain (meningitis)
- Lungs (bacterial pneumonia)
- Skin (cellulitis)
- Bone (osteomyelitis)
- Any opening in barrier of skin
Stages of Sepsis
1. Infection (fever)
2. System inflammatory response syndrome (SIRS)
3. Sepsis (SIRS + infection on culture)
4. Severe sepsis/Septic Shock (organ dys, hypoTN or hypoperfusion)
Septic Shock
An overwhelming systemic infection
- 70% of septic chock causes are due to HAI (prevention is key)
- characterized by persistent hypoTN and inadequate tissue perfusion that results in tissue hypoxia
Organisms causing septic shock
- Gram negative bacteria (ex: E. coli, Proteus species, Klebsiella coli, etc.)
- Some Gram positive bacteria (strep or pneumococcal)
- Also can be caused by yeasts, fungi, parasites, protozoa, mycobacteria, rickettsia
3 Pathophysiologic Effects of Septic Shock
Vasodilation --> leads to hypoTN
Maldistribution of blood flow
Myocardial depression
- decreased EF
- ventricular dilation
Phases of Septic Shock: Hyperdynamic Phase
Increased CO
Decreased SVR
Moderate tachycardia + normal BP
Widened pulse pressure
Pyrexia (fever)
Warm, dry, flushed skin
Moderate alteration in sensorium (early sign)
Normal cap refill
Tachypnea (early indicator)
Phases of Septic Shock: Hypodynamic Phase
S&S are similar to uncompensated and irreversible shock
- Significant tachycardia changing to bradycardia
- Dysrhythmias
- Profound hypotension
- Decreased pulse pressure
- Decreased SVP, PAP, PAWP, CO, SVR + afterload
CMs of Septic Shock
- Tachypnea/hyperventilation
- results in respir. alkalosis
- occurs due to backup in blood
- ↓ Urine output
- Altered neurologic status
- GI dysfunction, GI bleeding, paralytic ileus
- not getting blood flow to gut
Tx for Septic Shock
1. Supplemental O2
2. Fluids (for vasodilation)
3. Antibiotics (start within 1st hr of dx)
4. Inotropic drugs
5. Vasopressor drugs
Antibiotics Tx for Septic Shock
Culture pt first before starting antibiotics
- will culture the sputum, blood, urine
Stages of Shock: Initial Stage
Occurs at a cellular level
- usually not clinically apparent
- metabolism changes from aerobic to anaerobic = lactic acid buildup
What is lactic acid?
Waste product that is removed by liver
- process requires O2 --> which is unavailable due to decrease tissue perfusion in shock pts
Stage of Shock: Compensatory Non-Progressive Stage (1st Part)
1. Body activates neural, hormonal and biochemical compensation to try to maintain homeostasis
- respiratory alkalosis
- baroreceptors in arteries detect hypoTN
- catecholamines are released
- RAAS is activated
- Vasopressin (ADH)
Release of Catecholamines in Compensatory Non-Progressive Stage
Norepinephrine
- causes predominately vasoconstriction w/ mild increase in HR
Epinephrine
- predominately causes an increase in HR w/ small effect on vascular tone --> results in increase in BP
Release of Vasopressin (ADH) in Compensatory Non-Progressive Stage
Conserves fluids via kidney & GI tract
- causes vasoconstriction of kidneys, GI tract, and other organs → divert blood to heart, lungs and brain
- lack of blood to renal system → causes characteristic low urine production
Stages of Shock: Compensatory Non-Progressive Stage (2nd Part)
2. SNS stimulation increases myocardial O2 demands
3. Shunting blood from lungs increases physiologic dead space, causing:
- V/Q mismatch
- decreased arterial O2 levels
- increase in rate/depth
4. Impaired GI motility
- causing slowed peristalsis & risk for paralytic ileus
5. Decreased blood flow to skin
- pt feels cold & clammy
Is the body able to compensate during the Compensatory Stage of Shock?
Yes, the body is able to compensate for changes in tissue perfusion
- if correct --> pt recovers w/ little or no effects
- if not corrected --> pt enters progressive stage
Stages of Shock: Progressive (Decompensating)
Begins as compensatory mechanisms fail
- Na+ builds up as K+ leaks out
- Anaerobic metabolism continues = worsening metabolic acidosis
Stages of Shock: Progressive - Cardiovascular System
CO begins to fall
- decrease in BP, coronary artery, cerebral and peripheral perfusion
Altered capillary permeability occurs
- fluids & proteins leak into interstitial space causing anasarca (profound edema)
Myocardial dysfunction = dysrhythmias, MIs
Pt is at higher risk for DIC
- consumption of PLTs and clotting factors = increased bleeding
Stages of Shock: Progressive - Pulmonary System
WILL SHOW CRITICAL DYS FIRST!!
Results in:
- impaired gas exchange
- decreased compliance
- worsening ventilation-perfusion mismatch
Blood flow to lungs is reduced
Fluid moves from pulmonary area into interstitial space
- causing edema and bronchoconstriction
Fluid moving into alveoli = alveolar edema & decrease in surfactant products (ARDS!)
What would the pt have CLINICALLY in the progressive stage of shock (pulmonary system)?
Tachypnea
Crackles
Increased WOB
Stages of Shock: Progressive - GI System
Affected by prolonged decreased tissue perfusion
Mucosal barrier becomes ischemic
- increases risk of ulcers and GI bleeding and bacteria migration
- decreased ability to absorb nutrients
Stages of Shock: Progressive - Liver
Los of liver function leads to failure to metabolize drugs and waste products (ex. lactate, ammonia)
1. Jaundice results from increased bilirubin
2. As liver cells die = increased liver enzymes
3. No more immune function
- cannot destroy bacteria from GI tract = increased risk of bacteremia
Stages of Shock: Progressive - Kidneys
Causes renal tubular ischemia & leads to an AKI
- can be worsened by nephrotoxic drugs
- metabolic acidosis occurs from decreases ability to excrete acids and reabsorb bicarbonate
What can be seen CLINCIALLY in a pt who is in the progressive stage of shock (kidneys)?
Decreased urine output
Increased BUN & serum creatinine
Stages of Shock: Refractory (Irreversible)
Decreased perfusion worsens anaerobic metabolism
- caused by peripheral vasoconstriction and decreased CO
- vital organs have FAILED
What will be seen in a pt in the refractory stage of shock?
- Profound acidosis
- Profound hypoTN & hypoxemia
- Tachycardia worsen (decreased O2 to heart)
- Brain damage and cell death occurred
- Organ systems are in failure
RECOVERY IS UNLIKELY
Obstructive Shock
Develops when physical obstruction to blood flow occurs with decreased CO
- associated w/ obstruction of the big vessels or the heart
What is Obstructive Shock caused by?
1. Restricted diastolic filling of right ventricle from compression
2. Abd. compartment syndrome
- abd. pressure compressing IVC
3. PE and right vent. thrombi
- causes decreased blood flow to lungs & blood return to LA
Forms of Obstructive Shock
PE
Tension pneumothorax
Cardiac tamponade
Symptoms of Obstructive Shock
Rapid assessment and immediate tx = important!!!
- Decreased CO
- Increased Afterload
- Variable LV filling pressure
- JVD
- Pulsus paradoxus (abn. decrease in BP during inspiration)
Interprofessional Care for Obstructive Shock
Having early recgnitina tx
- echa ial therapy
- yjt