exam style questions[CVS; NEURO(41,43,44)]
1/107
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
108 Terms
A 75-year-old woman is brought to the clinic by her daughter, who reports that her mother has been experiencing progressive memory loss, disorientation, and difficulty performing daily tasks over the past two years. On neurological examination, the patient exhibits significant cognitive impairment, including problems with short-term memory and executive functions. An MRI of the brain shows generalized cortical atrophy, particularly in the medial temporal lobe. A brain biopsy reveals the following microscopic findings:
Neuro-Fibrillary Tangles (NFTs): Paired helical filaments forming basophilic fibrillary structures in the cytoplasm of neurons.
Abnormally hyper-phosphorylated tau protein: Major component of paired helical filaments.
Localization: Entorhinal cortex, hippocampus, amygdala, basal forebrain.
Which of the following is the most likely diagnosis?
alzheimers
A 75-year-old male presents with his daughter, who reports that he has been experiencing progressive forgetfulness, difficulty finding words, and occasional disorientation over the past two years. His past medical history is significant for hypertension and hypercholesterolemia. On examination, he is oriented to person but not to time or place. Neuroimaging shows marked atrophy of the cerebral cortex, particularly in the frontal and parietal lobes, with evidence of hydrocephalus ex vacuo. A brain biopsy shows:
Diffuse Plaques: Αβ deposits lacking the surrounding neuritic reaction.
Localization: Cerebral cortex, basal ganglia, cerebellar cortex.
What best describes the stage of plaque development in this patient?
early stage
(neuritic plaques are in the late stage)
(pt has alzheimer disease)
A 72-year-old woman is evaluated for progressive memory loss, difficulty in language, and changes in behavior. Her family notes that she has become increasingly confused and has difficulty performing familiar tasks. Neurological examination shows moderate cognitive impairment and disorientation. MRI shows marked cortical and hippocampal atrophy. Genetic testing reveals a mutation in the PS1 gene. A brain biopsy reveals the following microscopic findings:
Neurofibrillary Tangles (NFTs): Paired helical filaments in the cytoplasm of neurons, composed of abnormally hyper-phosphorylated tau protein.
Localization: Entorhinal cortex, hippocampus, amygdala, basal forebrain.
Which genetic factor is most likely associated with this patient's condition?
Variant of Apolipoprotein E called ε4 (Apo E4)
A 68-year-old man presents to the clinic with his wife, who reports that he has had increasing difficulty remembering recent events and handling daily activities over the past year. He has also become more withdrawn and sometimes exhibits sudden mood changes. On examination, he shows significant disorientation and mild aphasia. MRI reveals cortical atrophy, particularly in the temporal and parietal lobes. A brain biopsy shows the following microscopic findings:
Neuritic Plaques: Focal, spherical collections of tortuous, silver-staining neuritic processes around a central amyloid-beta (Aβ) core, with microglia and reactive astrocytes at their periphery.
Localization: Hippocampus, amygdala, and neocortex.
What is the most likely diagnosis?
ALzheimer disease
A 58-year-old woman presents with progressive difficulty in finding words and understanding language over the past two years. Her family notes that she also shows some changes in behavior, such as becoming more irritable and less empathetic. However, her memory remains relatively intact. Neurological examination reveals prominent language deficits. MRI shows significant atrophy of the temporal lobes. A brain biopsy reveals the following microscopic findings:
Microscopic Findings: Presence of neuronal inclusions.
Forms of FTLD:
FTLD-tau: Defining inclusions contain tau; Subtype of FTLD-tau is Pick disease, which has characteristic smooth, globular, pale basophilic inclusions (Pick bodies).
FTLD-TDP43: Aggregates contain TDP43; Predominantly frontal lobe cognitive impairment.
What following is the most likely diagnosis?
fronto-temporal lobe degeneration
A 62-year-old man presents with his wife, who reports that he has undergone significant personality changes over the past year. He has become more disinhibited, socially inappropriate, and apathetic. On examination, the patient shows notable behavioral changes but relatively preserved memory. MRI of the brain reveals marked atrophy of the frontal and temporal lobes. A brain biopsy reveals the following microscopic findings:
Microscopic Findings: Presence of neuronal inclusions.
Forms of FTLD:
FTLD-tau: Defining inclusions contain tau; Subtype of FTLD-tau is Pick disease, which has characteristic smooth, globular, pale basophilic inclusions (Pick bodies).
FTLD-TDP43: Aggregates contain TDP43; Predominantly frontal lobe cognitive impairment.
Which is the most likely diagnosis?
fronto-temporal lobe degeneration
A 70-year-old man presents with a history of progressive asymmetric limb rigidity, tremor, and difficulty with fine motor tasks over the past 3 years. His family notes that he has developed apraxia and cortical sensory deficits. Neurological examination reveals marked rigidity, akinesia, and cortical sensory loss. MRI of the brain shows asymmetric cortical atrophy and basal ganglia involvement. A brain biopsy reveals tau-containing inclusions in neurons and glia.
Which condition is most likely associated with the findings in this patient?
Cortico-Basal Degeneration
A 65-year-old man presents with a history of progressive difficulty in speaking and swallowing over the past 4 years. His family notes that he has developed stiffness in his neck and trunk, and difficulty with eye movements. Neurological examination reveals axial rigidity, dysphagia, and vertical gaze palsy. MRI of the brain shows atrophy of the midbrain. A brain biopsy reveals α-Synuclein aggregates in oligodendrocytes.
Which condition is most likely associated with the findings in this patient?
Multiple System Atrophy
[this is a disease associated with Parkinsonism]
(differential diagnosis:
Progressive Supranuclear Palsy (PSP): Characterized by vertical gaze palsy and axial rigidity, but it usually shows tau protein aggregates rather than α-Synuclein.
Parkinson's Disease: Typically involves Lewy bodies (α-Synuclein aggregates) in neurons, not oligodendrocytes, and does not usually present with midbrain atrophy early on.
Lewy Body Dementia: Also involves α-Synuclein but primarily affects cortical and subcortical neurons, presenting with cognitive decline and fluctuating attention rather than prominent autonomic dysfunction or midbrain atrophy.)
A 68-year-old man presents with a history of progressive stiffness, slowness of movements, and a resting tremor that started on one side of his body and gradually involved both sides. He also reports difficulty maintaining balance and frequent falls. On examination, he exhibits cogwheel rigidity, bradykinesia, and a resting tremor. MRI of the brain shows pallor of the substantia nigra and locus coeruleus. A brain biopsy reveals the following microscopic findings:
Microscopic Findings: Loss of pigmented neurons and gliosis in the substantia nigra and locus coeruleus.
Presence of Lewy Bodies: Intra-cytoplasmic, eosinophilic, round inclusions with a dense core and a peripheral pale halo, composed of α-Synuclein, Neurofilaments, and Ubiquitin.
Clinical Syndrome: Tremor, rigidity, bradykinesia, and instability.
Which of the following is the most likely diagnosis?
parkinson’s disease.
A 55-year-old woman presents with a 2-year history of progressive difficulty in walking and frequent falls. She reports stiffness and slowness in her movements, along with a resting tremor that started on one side and now affects both sides. Neurological examination reveals cogwheel rigidity, bradykinesia, and a resting tremor. MRI of the brain shows pallor of the substantia nigra and locus coeruleus. A brain biopsy reveals the following microscopic findings:
Microscopic Findings: Loss of pigmented neurons and gliosis in the substantia nigra and locus coeruleus.
Presence of Lewy Bodies: Intra-cytoplasmic, eosinophilic, round inclusions with a dense core and a peripheral pale halo, composed of α-Synuclein, Neurofilaments, and Ubiquitin.
Clinical Syndrome: Tremor, rigidity, bradykinesia, and instability.
Which of the following is the most likely diagnosis?
Parkinson’s disease.
A 40-year-old man presents with a 3-year history of progressive involuntary movements, including choreiform movements of the limbs and face. His family reports that he has also become increasingly forgetful and irritable. On examination, he exhibits prominent chorea, impaired cognition, and affective disturbances. MRI of the brain shows atrophy of the caudate nucleus and enlargement of the lateral ventricles. A brain biopsy reveals severe loss of neurons in the striatum and intra-nuclear inclusions composed of ubiquitinated Huntingtin.
Which of the following is the underlying genetic mutation associated with this patient's condition?
Trinucleotide repeat expansion in the HTT gene
A 50-year-old woman presents with a history of progressive choreiform movements and cognitive decline over the past 5 years. She reports difficulty with balance and frequent falls. Neurological examination reveals choreiform movements of the limbs and face, along with rigidity and dystonia(Twisting movements of the extremities). MRI of the brain shows marked atrophy of the caudate nucleus and putamen. A brain biopsy reveals severe loss of neurons in the striatum and fibrillary gliosis.
Name another (microscopical) pathological finding characteristic of Huntington's disease
Intra-nuclear inclusions composed of ubiquitinated Huntingtin
A 45-year-old man presents with a 4-year history of progressive involuntary jerky movements, memory loss, and mood swings. His family notes a history of similar symptoms in his father and paternal grandmother. On examination, he demonstrates choreiform movements and cognitive impairment. MRI of the brain shows prominent atrophy of the caudate nucleus and dilation of the lateral ventricles. A brain biopsy confirms severe loss of neurons in the striatum.
Which of the following is the most likely prognosis for this patient?
Persistently progressive disease course
A 55-year-old woman presents with a 2-year history of progressive choreiform movements and difficulty with coordination. She reports frequent falls and increasing forgetfulness. Neurological examination reveals prominent chorea, along with impaired executive function and memory deficits. MRI of the brain shows marked atrophy of the caudate nucleus and putamen. A brain biopsy reveals severe loss of neurons in the striatum and fibrillary gliosis.
Which brain region is secondarily affected due to atrophy of the caudate nucleus in Huntington's disease?
globus pallidus
A 60-year-old man presents with a 5-year history of progressive choreiform movements and memory problems. He also experiences frequent mood swings and irritability. Neurological examination reveals involuntary jerky movements of the limbs and face, along with cognitive impairment. MRI of the brain shows prominent atrophy of the caudate nucleus and dilatation of the lateral ventricles. A brain biopsy reveals severe loss of neurons in the striatum and intra-nuclear inclusions composed of ubiquitinated Huntingtin.
What is most likely to be the diagnosis?
huntington’s disease.
A 72-year-old woman presents with progressive memory loss and subtle behavioral changes over the past few months. Her family reports that her condition has deteriorated rapidly. Neurological examination reveals cognitive impairment and myoclonus. MRI of the brain shows no significant atrophy. A brain biopsy reveals the following microscopic findings:
Microscopic Findings: Spongiform changes in the cerebral cortex and deep gray matter structures, with microscopic vacuoles of variable size within the neuropil and neuronal perikaryon. Severe neuronal loss and reactive gliosis are noted.
What is the most likely diagnosis?
Creutzfeldt-Jakob disease (CJD)
A 65-year-old man presents with a 4-month history of rapidly progressive dementia and myoclonic jerks. His family notes significant changes in his memory and behavior. An MRI of the brain shows spongiform changes without significant atrophy. A brain biopsy reveals severe neuronal loss, reactive gliosis, and status spongiosus.
Which of the following epidemiological features is most consistent with this patient's diagnosis?
A) Autosomal dominant inheritance
B) Sporadic form constitutes 85% of cases
C) Incidence rate: 10 per million
D) Most common in individuals under 50 years of age
E) Slow progression over several years
B
A 68-year-old woman presents with rapidly progressive dementia, personality changes, and involuntary movements over the past six months. Her condition has worsened significantly, leading to severe cognitive impairment. MRI of the brain shows little or no atrophy, but a brain biopsy reveals spongiform changes and numerous microscopic vacuoles within the neuropil and neuronal perikaryon.
Mention 2 micro findings characteristic of severe cases of the disease likely affecting this patient?
Severe neuronal loss and status spongiosus
A 55-year-old man presents with behavioral changes, cognitive decline, and involuntary movements that have progressed over the past year. He has a family history of a similar disease. MRI of the brain reveals no significant atrophy. A brain biopsy shows spongiform changes, abundant cortical amyloid plaques, and reactive gliosis.
Given the patient's age and clinical presentation, which variant of Creutzfeldt-Jakob disease is most likely?
Variant CJD
A 38-year-old woman presents with a progressive history of unsteady gait and difficulty with coordination. She also reports muscle stiffness and weakness in her extremities. Neurological examination reveals cerebellar ataxia, spasticity, and diminished sensation in a glove-and-stocking distribution. Genetic testing confirms a trinucleotide repeat expansion mutation.
Which microscopic finding are most likely to be observed in a biopsy of this patient's nervous tissue?
Degeneration of neurons without characteristic histopathologic changes
reactive astrogliosis
A 16-year-old boy presents with difficulty walking, frequent falls, and clumsiness of the hands. Physical examination reveals pes cavus, kyphoscoliosis, and gait ataxia. He also has dysarthria. Genetic testing reveals a GAA trinucleotide repeat expansion in the gene encoding frataxin.
Which primary pathophysiological mechanism is the underlying cause of this patient's condition?
Decreased levels of frataxin leading to mitochondrial dysfunction and increased oxidative damage.
(Stems from GAA trinucleotide repeat. )
A 45-year-old man presents with progressive gait instability, muscle stiffness, and loss of sensation in his hands and feet. Neurological examination confirms cerebellar ataxia, spasticity, and peripheral neuropathy. Genetic testing identifies a trinucleotide repeat expansion mutation.
How likely is it for kyphoscoliosis to be associated with this condition?
Not likely. The scenario described charactic findings of spinocerebellar ataxia - not friederich ataxia.
A 12-year-old girl presents with progressive gait ataxia, hand clumsiness, and slurred speech. Her family history is significant for a similar disorder in her older brother. On examination, she has pes cavus and kyphoscoliosis. Genetic testing confirms an autosomal recessive disorder with a GAA trinucleotide repeat expansion.
Name an additional finding most likely to be present in this patient?
Sensorimotor peripheral Neuropathy
A 55-year-old man presents with progressive muscle weakness, atrophy, and fasciculations. Neurological examination reveals hyperreflexia and spasticity. Genetic testing identifies a mutation in the SOD-1 gene.
What pathophysiological mechanism is most likely responsible for this patient's condition?
Accumulation of misfolded SOD-1 protein leading to neuronal apoptosis
A 62-year-old woman presents with muscle weakness, atrophy, and difficulty swallowing. Physical examination shows fasciculations and spasticity. She has a family history of similar symptoms in her father. Which of the following genetic mutations is most likely associated with her condition?
A) α-Synuclein
B) TDP-43
C) Amyloid precursor protein
D) Frataxin
E) Huntingtin
TDP-43
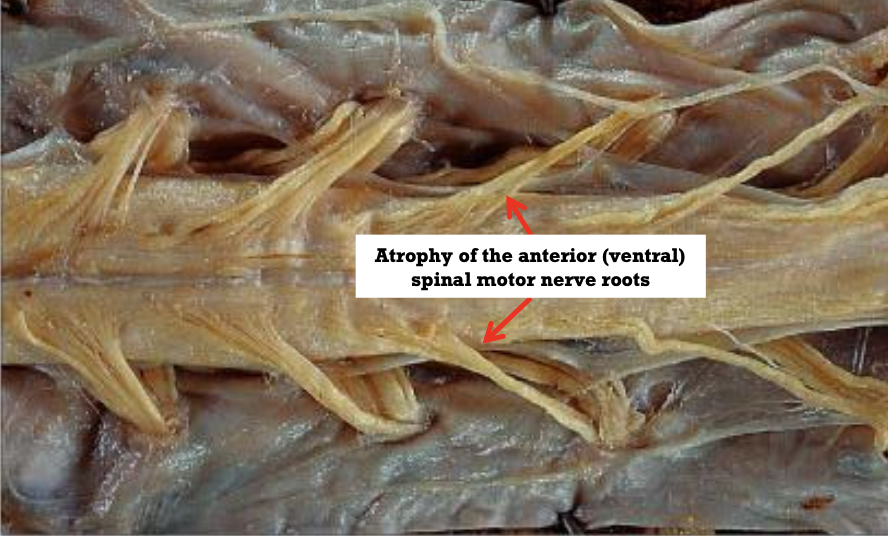
A patient diagnosed with ALS presents with severe muscle weakness, hyperreflexia, and spasticity. Which of the following microscopic findings is most likely to be observed in this patient's spinal cord?
Reactive gliosis and loss of anterior root myelinated fibers
A 58-year-old man with a diagnosis of ALS has progressive muscle atrophy and fasciculations. What is the most common cause of death in patients with this disease?
Respiratory muscle involvement leading to recurrent pulmonary infections
A 60-year-old woman with ALS has developed significant weakness and spasticity. On examination, there is atrophy of the tongue muscles and hyperreflexia in the limbs. Which of the following macroscopic findings is most likely to be seen in her spinal cord?
A) Enlarged anterior roots
B) Enlarged pre-central gyrus
C) Thin and gray anterior roots
D) Atrophy of the substantia nigra
E) Enlargement of the lateral ventricles
▪ Thin and gray anterior roots of the spinal cord
▪ Mildly atrophic pre-central gyrus (severe cases)
A 45-year-old man with a history of chronic alcoholism presents with confusion, abnormal eye movements, and ataxia. On physical examination, he is found to have memory disturbances. MRI reveals foci of hemorrhage and necrosis in the mammillary bodies and periventricular regions.
What is the most likely diagnosis?
wernicke’s encephalopathy
A patient with chronic alcoholism presents with confusion, ophthalmoplegia, and ataxia. Microscopic examination of brain tissue reveals dilated capillaries with prominent endothelial cells and hemorrhages.
Which findings are most likely to be seen in the chronic phase of this condition?
Gliosis with perivascular accumulation of haemosiderin-laden macrophages
Shrunken and centrally rarified mamillary bodies
A 55-year-old woman with a history of gastric carcinoma presents with confusion, ataxia, and eye movement abnormalities. She is diagnosed with Wernicke’s encephalopathy.
Which macroscopic features are most likely to be observed in this patient’s brain?
Foci of hemorrhage and necrosis in the mammillary bodies and around the 3rd and 4th ventricles
Atrophy of mammillary bodies
A 70-year-old man presents with progressive numbness and tingling in his lower extremities, along with slight ataxia. He also has pernicious anemia. Laboratory tests reveal a deficiency in vitamin B12.
Which of the following is the most likely diagnosis?
Early subacute combined degeneration of the spinal cord
A patient presents with memory disturbances, confusion, and ataxia. Imaging reveals shrunken mammillary bodies with central rarefaction. Histology shows gliosis and perivascular accumulation of haemosiderin-laden macrophages.
What is the most likely underlying condition?
Chronic Wernicke’s encephalopathy
A 50-year-old man with a history of poorly controlled diabetes mellitus presents with confusion, stupor, and eventually slips into a coma. His lab results indicate severe hyperglycemia.
Which of the following complications is most likely responsible for his condition?
A) Diabetic ketoacidosis
B) Hypoglycemia
C) Hepatic encephalopathy
D) Global hypoxia
E) Subacute combined degeneration of the spinal cord
diabetic ketoacidosis
A patient presents with confusion and altered mental status. Histological examination of brain tissue shows astrocytes with swollen, pale nuclei, particularly in the cortex and basal ganglia.
what is the most likely diagnosis and cause?
hepatic encephalopathy due to elevated levels of urea + inflammation + hyponatriaemia
A 35-year-old man is brought to the emergency room with symptoms of severe confusion, tremors, and muscle atrophy. He works in an industrial environment with potential exposure to heavy metals.
Which of the following toxins is most likely responsible for his symptoms?
A) Arsenic
B) Lead
C) Mercury
D) Organophosphates
E) Methanol
mercury
A 60-year-old chronic alcoholic presents with truncal ataxia, an unsteady gait, and nystagmus. An MRI shows atrophy in the anterior cerebellar vermis.
Which of the following microscopic findings is most likely to be observed in his brain tissue?
A) Extensive white matter necrosis
B) Thinning of the molecular layer and patchy loss of Purkinje cells
C) Foci of hemorrhage and necrosis
D) Spongiform changes
E) Dilated capillaries with prominent endothelial cells
Thinning of the molecular layer and patchy loss of Purkinje cells
mild loss of granule cells
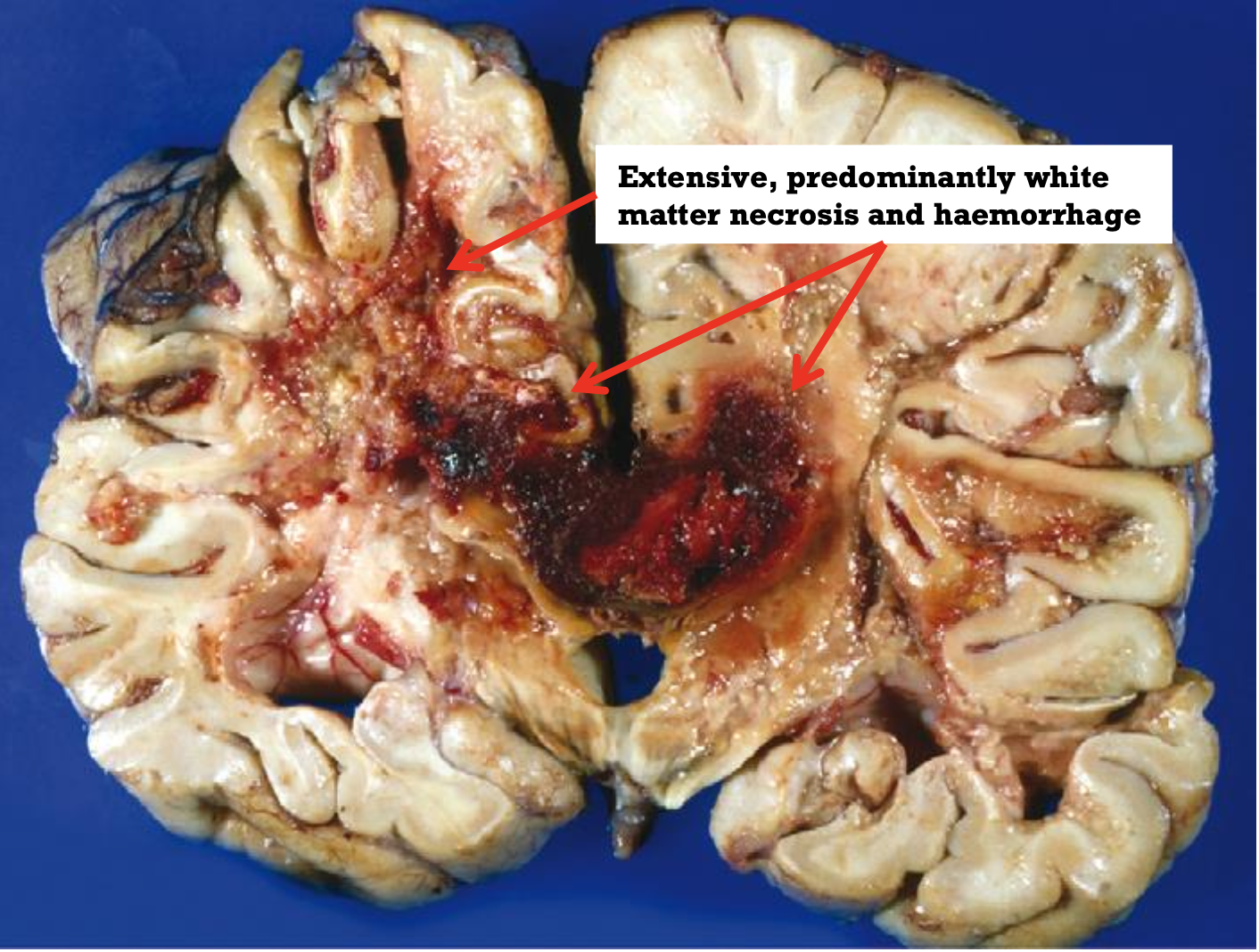
A patient presents with headache, nausea, vomiting, and papilledema. He has a history of exposure to ionizing radiation.
Which of the following histological findings is most likely to be observed in his brain tissue?
A) Reactive astrogliosis
B) Cystic spaces with haemosiderin-laden macrophages
C) Extensive white matter necrosis and haemorrhage
D) Spongiform changes in the cortex
E) Fibrillary gliosis
Extensive white matter necrosis and haemorrhage
A patient presents with acute onset blindness after ingesting a suspicious substance. Further testing reveals severe metabolic acidosis.
Which of the following toxins is most likely responsible for his symptoms?
A) Lead
B) Mercury
C) Methanol
D) Ethanol
E) Organophosphates
methanol
A 28-year-old woman presents with episodes of blurred vision, weakness in her legs, and difficulty walking over the past year. MRI of her brain reveals multiple, well-circumscribed, slightly depressed, gray-tan lesions in the periventricular regions. Histological examination shows active plaques with abundant macrophages and perivascular cuffs of lymphocytes and macrophages. What is the most likely diagnosis?
MS
A 4-year-old child presents with developmental delays and progressive deterioration in motor skills. Physical examination reveals spasticity and ataxia. MRI shows diffuse gray and translucent appearance of the white matter with brain atrophy and ventricular enlargement. Histological examination shows myelin loss and lipid-stuffed macrophages. What is the most likely diagnosis?
leukodystrophy
A 32-year-old man presents with acute onset of headache, lethargy, and coma, two weeks after recovering from a viral illness. MRI reveals multiple foci of inflammatory demyelination with diffuse edema in the adjacent white matter. Histological examination shows perivascular neutrophil infiltrates and scattered petechial hemorrhages. What is the most likely diagnosis?
Acute Hemorrhagic Leukoencephalitis (AHL)

A 45-year-old man with chronic alcoholism develops rapidly evolving quadriplegia (paralysis of all 4 limbs) after undergoing rapid correction of hyponatremia. MRI of the brain shows symmetric demyelination in the center of the pons. Which of the following is the most likely diagnosis?
central pontine myelinolysis
A 38-year-old woman presents with recurrent episodes of optic neuritis and transverse myelitis. She tests positive for antibodies against aquaporin-4. Which of the following is the most likely diagnosis?
Neuro-myelitis Optica (NMO)
Which of the following is characteristic of leukodystrophies?
A) Inflammatory demyelination with perivascular neutrophil infiltrates
B) Abnormal myelin synthesis or turnover
C) Sharp margins with abundant macrophages in active plaques
D) Autoimmune response against aquaporin-4
E) Severe electrolyte imbalance causing demyelination
Abnormal myelin synthesis or turnover
A patient presents with myelin loss and lipid-stuffed macrophages in the white matter. This condition typically manifests with progressive deterioration in motor skills and spasticity starting in early childhood. Which of the following conditions is most likely?
Leukodystrophy
Which of the following is a characteristic feature of multiple sclerosis on histological examination of active plaques?
Lipid-stuffed macrophages
A 10-year-old boy presents with fever, joint pain, and involuntary movements. He recently recovered from a sore throat. Physical examination reveals erythema marginatum on his trunk and subcutaneous nodules over his elbows. Which of the following is the most likely causative agent of his condition?
A) Group A β-haemolytic Streptococcus
B) Staphylococcus aureus
C) Streptococcus pneumoniae
D) Neisseria meningitidis
E) Mycobacterium tuberculosis
Group A β-haemolytic Streptococcus
(pt has rheumatic fever)
A 12-year-old girl with a history of rheumatic fever presents with shortness of breath and fatigue. Echocardiogram reveals mitral valve stenosis. What best describes the pathological changes in her mitral valve?
Thickened, fibrotic, and deformed valve with fusion of cusps
A 14-year-old boy presents with joint pain that migrates from one joint to another. Laboratory tests reveal elevated ESR and positive anti-streptolysin O (ASO) titers. Which of the following cardiac manifestations is most likely to develop in this patient if his condition progresses?
A) Aortic valve stenosis
B) Mitral valve stenosis
C) Pulmonic valve stenosis
D) Tricuspid valve stenosis
E) Patent ductus arteriosus
Mitral valve stenosis
mitral valve>aortic valve>tricuspid valve
A pathologist examines a myocardial biopsy from a patient with rheumatic fever and notes focal interstitial myocardial inflammation with fragmented collagen and fibrinoid material. Large cells with prominent nuclei are also seen. These findings are most consistent with what microscopic feature?
Aschoff nodules.
During an autopsy of a patient who had rheumatic heart disease, the examiner finds map-like areas of thickened, roughened endocardium in the left atrium. Microscopic examination reveals subendocardial fibrosis with mixed inflammatory cell infiltrate. These findings are most consistent with what?
MacCallum plaques
(arises from damage to posterior wall of left ventricle)
A 9-year-old girl presents with a sudden onset of bizarre grimaces and purposeless muscular movements. She has a history of a recent streptococcal throat infection. What is the most likely neurological manifestation of her condition?
Sydenham Chorea
A biopsy from the myocardium of a patient with acute rheumatic fever shows focal interstitial inflammation with Aschoff cells and Anitschkow cells. What stage of the disease is indicated by these histopathological findings?
granulomatous stage (Arises 1-2 months after the onset of clinical
symptoms)
A patient with a history of rheumatic fever presents with signs of congestive heart failure. Echocardiography shows pericardial effusion and thickened mitral valve leaflets. Which of the following findings is least likely to be associated with his condition?
A) Aschoff bodies in the myocardium
B) Red and swollen valve leaflets
C) Multinucleated giant cells in myocardial lesions
D) Calcifications of the mitral valve leaflets
E) Hemorrhagic pericardial effusion
Hemorrhagic pericardial effusion
Myocarditis → Cardiac failure → Death
another anatomic change due to rheumatic fever.
• Red and swollen valve leaflets
• Tiny, warty, rubbery, but non-friable vegetations (verrucae) along the lines of closure of the valve leaflets
early stage of endocarditis due to rheumatic fever.
A 45-year-old woman with a history of rheumatic fever presents with dyspnea and fatigue. Physical examination reveals a diastolic murmur best heard at the apex. Echocardiography confirms mitral valve stenosis. What is the most common cause of her condition?
Post-rheumatic or post-inflammatory disease
A 50-year-old man with a history of rheumatic heart disease presents with worsening shortness of breath. Echocardiography reveals a "fish mouth" appearance of the mitral valve. Which of the following microscopic features is most likely to be absent in this patient’s mitral valve?
A) Fibrosis and calcification
B) Aschoff bodies
C) Neovascularisation
D) Chronic inflammatory cell infiltrate
E) Superimposed sterile vegetations
Aschoff bodies
A 12-year-old girl presents with symptoms of heart failure. She has a history of rheumatic fever. Physical examination reveals a diastolic rumbling murmur at the apex. Which of the following macroscopic features is most characteristic of acute rheumatic valvulitis affecting the mitral valve?
A) Fibrous thickening and retraction of the leaflets
B) Tiny flat vegetations along the lines of closure
C) Fusion and shortening of the chordae
D) "Fish mouth" orifice
E) Calcification with or without ossification
Tiny flat vegetations along the lines of closure
A) Fibrous thickening and retraction of the leaflets (would be right if she already had rheumatic heart disease as these are present in fibrosing stage)
B) Tiny flat vegetations along the lines of closure
C) Fusion and shortening of the chordae (fibrosing stage)
D) "Fish mouth" orifice (fibrosing stage)
E) Calcification with or without ossification (microscopic feature of fibrosing stage)
A pathologist examines a mitral valve biopsy from a patient with chronic rheumatic heart disease. The specimen shows fibrosis, calcification, and neovascularisation but lacks Aschoff bodies. What stage of the disease is indicated by these findings?
fibrosing stage of rheumatic heart disease
A patient with a history of rheumatic fever develops severe aortic stenosis. Echocardiography reveals thickened, inflexible aortic valve leaflets with a triangular orifice. Which macroscopic findings would most likely be observed in this condition?
fusion of the commissures
(calcification less than what is seen tricuspid aortic stenosis)
A 55-year-old woman with a history of rheumatic fever presents with symptoms of heart failure. Echocardiography reveals thickened and calcified mitral valve leaflets with a narrow, oval-shaped orifice. What is the most likely microscopic finding in her mitral valve?
A) Platelet-fibrin thrombi
B) Aschoff bodies
C) Fibrosis and neovascularisation
D) Acute inflammatory cell infiltrate
E) Myxomatous degeneration
Fibrosis and neovascularisation
A 60-year-old man presents with progressive dyspnea and a history of rheumatic fever. Physical examination reveals a systolic ejection murmur at the right upper sternal border. Echocardiography shows thickened aortic valve leaflets with a triangular orifice. Which of the following complications is he at risk for?
A) Myocardial infarction
B) Infectious endocarditis
C) Cardiac tamponade
D) Pulmonary embolism
E) Aortic dissection
Infectious endocarditis
A 14-year-old boy with a history of rheumatic fever develops mitral valve stenosis. During surgery, the mitral valve is found to have fusion of the commissures and thickened leaflets. Microscopic examination reveals fibrosis and chronic inflammatory cells but no Aschoff bodies. Which phase of rheumatic heart disease does this represent?
fibrosing phase
A 65-year-old man with a history of hypertension and myocardial infarction presents with progressive shortness of breath and orthopnea. On physical examination, you note bilateral crackles at the lung bases. What is the most likely cause of his condition?
left sided heart failure
A 55-year-old woman presents with worsening dyspnea and peripheral edema. She has a history of untreated hypertension. Which of the following clinical manifestations is least likely associated with her condition?
A) Dyspnea and orthopnea
B) Pleural effusion with hydrothorax
C) Pitting edema of the ankles
D) Cerebral anoxia
E) Distention of the neck veins
Distention of the neck veins is characteristic of right sided heart failure.
(along with hepato/splenomegaly and pitting edema)
e in this case is more correct than option c
A 70-year-old man with a history of chronic obstructive pulmonary disease (COPD) presents with peripheral edema and distended neck veins. Echocardiography shows right ventricular hypertrophy and dilation. Which of the following is the most likely cause of his condition?
A) Left-sided heart failure
B) Mitral valve stenosis
C) Pulmonary hypertension
D) Tricuspid valve disease
E) Acute myocardial infarction
Pulmonary hypertension caused by cor pulmonale.
A 60-year-old woman presents with severe shortness of breath and orthopnea. Physical examination reveals bilateral crackles, and an S3 heart sound is heard on auscultation. Which of the following pathophysiological mechanisms is most likely responsible for her symptoms?
A) Activation of the renin-angiotensin-aldosterone system
B) Pulmonary embolism
C) Peripheral vasoconstriction
D) Left ventricular hypertrophy
E) Increased cardiac output
Activation of the renin-angiotensin-aldosterone system
A 50-year-old man presents with ascites, peripheral edema, and an enlarged, congested liver. He has a history of mitral valve stenosis and left-sided heart failure. What is the most likely diagnosis?
right sided heart failure
A 45-year-old woman with a history of systemic hypertension and mitral valve disease presents with shortness of breath and fatigue. Physical examination reveals rales in the lung bases and mild peripheral edema. Laboratory tests show increased serum creatinine. What best explains the increased serum creatinine in this patient?
Reduction in renal perfusion → Activation of Renin-Angiotensin-Aldosterone system → Retention of NaCl and H2O
A patient with a history of extensive myocardial infarction presents with dyspnea and orthopnea. Physical examination reveals bilateral lung crackles and an S3 heart sound. Which of the following best describes the primary mechanism behind his respiratory symptoms?
A) Increased pulmonary capillary hydrostatic pressure
B) Reduced systemic vascular resistance
C) Increased cardiac output
D) Decreased left atrial pressure
E) Pulmonary embolism
Increased pulmonary capillary hydrostatic pressure
LV is unable to pump blood out to body; blood backs up to left atrium and right side(pulmonary ‘side’); increased pressure in pulmonary side causes fluid leakage hence edema.
A 60-year-old man presents with fatigue, dyspnea, and peripheral edema. He has a history of diffuse myocarditis. On examination, you note distended neck veins and hepatomegaly. Which of the following findings would be most consistent with right-sided heart failure?
A) Bilateral lung crackles
B) Ascites
C) Pleural effusion with hydrothorax
D) Orthopnea
E) Increased cerebral perfusion
Ascites
Asthma, Acute Coronary Syndrome, COPD, Pulmonary Embolism
differential diagnosis for congestive heart failure.
A 45-year-old man with a history of chronic alcoholism presents with symptoms of heart failure. Echocardiography shows a globular-shaped heart with biventricular dilatation and normal left ventricular wall thickness. Which microscopic findings are most likely to be observed in his heart biopsy?
Interstitial and perivascular fibrosis with myocyte hypertrophy
A 30-year-old man collapses during a soccer game and is found to have asymmetric septal hypertrophy on echocardiography. His father died suddenly at age 40. What is the most likely genetic cause of his condition?
Autosomal dominant mutation in sarcomeric proteins
(cardiomyopathy here is hypertrophic cardiomyopathy)
A 50-year-old woman with a history of breast cancer treated with radiation therapy presents with symptoms of heart failure. Echocardiography shows normal left ventricular wall thickness and reduced ventricular compliance. Which condition is most likely contributing to her heart failure?
Restrictive cardiomyopathy
A 28-year-old man presents with palpitations and fainting after physical activity. Physical examination reveals hyperkeratosis of the palms and soles. An ECG shows ventricular arrhythmias, and an echocardiogram reveals right ventricular dilatation. Which genetic condition is most likely associated with his symptoms?
Naxos syndrome
(associated with arrhythmogenic right ventricular cardiomyopathy- also explains the hyperkeratosis seen)
A 40-year-old woman presents with progressive dyspnea and peripheral edema. She has a history of sarcoidosis. Echocardiography shows a thickened ventricular wall with reduced compliance. Which of the following best describes the pathogenesis of her condition?
condition is restrictive cardiomyopathy(infiltrative cardiomyopathy)
Infiltrative processes within heart muscle leads to stiffening of the myocardium → Restriction of the heart to stretch properly → Affects the filling capacity of the heart ventricles → Reduction in blood flow → Blood backs up in the circulation → Heart Failure
A 50-year-old man presents with heart failure symptoms and an echocardiogram shows marked left ventricular hypertrophy with a small left ventricular cavity. Histological examination reveals myocyte disarray and interstitial fibrosis. What is the most likely diagnosis?
A) Restrictive cardiomyopathy
B) Dilated cardiomyopathy
C) Hypertrophic cardiomyopathy
D) Arrhythmogenic right ventricular cardiomyopathy
E) Alcoholic cardiomyopathy
Hypertrophic cardiomyopathy
A 55-year-old man presents with heart failure symptoms and an echocardiogram shows dilated left and right ventricles with thin walls. A biopsy reveals reduced myocytes and interstitial lymphocytic infiltration. What is the most likely cause of his condition?
Alcohol-induced myocardial damage
A 35-year-old woman presents with symptoms of heart failure. She has a history of hemochromatosis. Echocardiography reveals normal ventricular size but reduced diastolic filling. Which of the following findings is most likely to be observed on her cardiac biopsy?
A) Extensive fatty infiltration and fibrosis
B) Marked myocyte hypertrophy and disarray
C) Interstitial deposits of iron
D) Myocyte loss and interstitial lymphocytes
E) Myocardial necrosis with neutrophilic infiltration
Interstitial deposits of iron
A 55-year-old male presents with progressive dyspnea and lower extremity edema. Echocardiography reveals biventricular dilatation and a globular-shaped heart. Biopsy of the heart muscle shows interstitial lymphocytic infiltration and myocyte hypertrophy. Which of the following is the most likely diagnosis?
Congestive (Dilated) Cardiomyopathy
A 45-year-old woman with a history of sarcoidosis presents with signs of heart failure. An echocardiogram shows normal ventricular size with poor diastolic filling. What is the most likely underlying mechanism of her heart failure?
Impairment of compliance (diastolic dysfunction)
(“sarcoidosis” points us to restrictive cardiomyopathy. )
A 30-year-old athlete collapses suddenly during a football match and is found to have a markedly thickened ventricular septum on autopsy. Genetic testing reveals a mutation in the gene encoding beta-myosin heavy chain. Which histological finding is most likely present?
Myocyte disarray and interstitial fibrosis
(Hypertrophic cardiomyopathy is often caused by mutations in genes encoding sarcomeric proteins, such as the beta-myosin heavy chain.)
A 40-year-old man presents with palpitations and syncope. An echocardiogram shows a dilated right ventricle with attenuation of the free wall and fatty infiltration. Genetic testing reveals mutations in desmoplakin and plakoglobin. What syndrome is most consistent with these findings?
Naxos Syndrome
A 60-year-old male with a history of chronic alcoholism presents with fatigue and dyspnea. Echocardiogram shows an enlarged heart with four-chamber dilatation and normal left ventricular wall thickness. What is the primary mechanism of his heart failure?
Impairment of contractility (systolic dysfunction)
Alcoholism is a cause of congestive cardiomyopathy which causes systolic dysfunction.
A 65-year-old woman with a history of hemochromatosis presents with heart failure. Echocardiogram reveals a non-dilated left ventricle with poor diastolic function. Which finding is most likely to be seen on histology?
fibrosis with iron deposits
(restrictive(infiltrative) cardiomyopathy)
A 35-year-old male presents with dizziness and palpitations. Physical examination reveals hyperkeratosis of the palms and soles. Imaging shows right ventricular dilatation. Genetic analysis reveals a mutation in plakoglobin. What is the primary pathological finding in this patient’s right ventricle?
Fatty infiltration and fibrosis
(naxos syndrome associated with Arrhythmogenic right ventricular Cardiomyopathy )
A 28-year-old man with a family history of sudden cardiac death presents with exertional dyspnea. Echocardiography shows asymmetric septal hypertrophy/”whorled’ appearance of septum. Which genetic mutation is most likely responsible for his condition?
Sarcomeric protein mutation
(hypertrophic cardiomyopathy)
A 55-year-old woman dies suddenly from a myocardial infarction. Histological examination of the heart reveals numerous neutrophils, loss of nuclei in myocardial cells, and karyorrhexis. What is the most likely time frame post-infarction when these findings are observed?
1-3 days
A 48-year-old man presents with chest pain and his ECG shows ST-segment elevation. Which of the following cardiac markers would be expected to return to normal levels within 48-72 hours?
CK-MB
Which of the following ECG findings is most characteristic of a non-ST-segment elevation myocardial infarction (NSTEMI)?
A) ST-segment elevation
B) Pathological Q-wave formation
C) T-wave inversion
D) J-point elevation
E) Tall, peaked T-waves
T-wave inversion
A patient with a history of myocardial infarction presents with signs of heart failure. Echocardiography reveals a ventricular aneurysm. What is the most likely underlying cause of this complication?
A) Arrhythmia
B) Myocardial rupture
C) Mural thrombosis
D) Extensive myocardial fibrosis
E) Transmural infarction
Transmural infarction
What is the primary pathological finding in a myocardial biopsy taken from a patient who died of an acute STEMI?
coagulative necrosis; transmural
A 60-year-old woman with chest pain and dyspnea is found to have subendocardial ischemia on an echocardiogram. Which laboratory finding would you expect to be delayed compared to ST-segment elevation myocardial infarction (STEMI)?
A) Troponin I levels
B) White blood cell count
C) CK-MB levels
D) ESR
E) CRP
Troponin I levels
(you’ll expect this to be elevated in STEMI thus most likely to be delayed here.)
(NSTEMI leads to subendocardial infarctions)
Which cellular component is least likely to be prominent in the acute phase of myocardial infarction?
Myocytes
(the first thing that happens is, they die(myocyte necrosis), hence they will be scarce)
A 68-year-old male presents with severe chest pain radiating to his left arm. His ECG shows ST-segment elevation in multiple leads, and laboratory tests reveal elevated Troponin I and CK-MB. Which type of myocardial infarction is most likely?
STEMI (transmural infarction)
Mention a long-term complication of thrombo-phlebitis that can result in chronic venous insufficiency and ulceration (especially of the lower extremities)
stasis ulcer
A patient with chronic venous insufficiency develops ulceration of the skin in the lower third of the leg. Which macroscopic feature is commonly associated with this condition?
Brawny (strapping) edema and dermal fibrosis
• Cutaneous pigmentation
• Dermal and subcutaneous fibrosis
• Extensive secondary varicosities
• Ulceration of the skin in the lower 1/3 of the leg