Archer: Critical Care Concepts
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
46 Terms
Ventilators terminology
continue to next following flashcards
peak inspiratory pressure (PIP)
highest level of pressure in lungs during inhalation
(pressure going in)
positive end expiratory pressure (PEEP)
amount of pressure in the alveoli at the end of expiration
(pressure at the end)
fraction of inspired oxygen (FiO2)
how much oxygen the patient is getting (21%-100%)
tidal volume (TV)
the amount of air that is inhaled during one respiratory cycle
end-tidal carbon dioxide (ETCO2)
partial pressure of CO2 at the end of exhalation (35-45)
if it is low then retaining CO2 thus making them acidotic
if it is high then releasing CO2 thus making them alkalotic
CO2 is acid
room air
atmospheric air we breathe under normal circumstances. has FiO2 of 21%
Ventilator modes
-volume controller: there is certain volume of air delivered to the pt. with each breath
-pressure controlled: the lungs are inflated to a certain pressure (looks at PIP and PEEP)
-CPAP: continuous positive airway pressure; continuous positive airway pressure, occurring, while pt controls their respiratory rates and volumes
-BiPAP: bilevel positive airway pressure; there is positive airway pressure, set at diff pressures for inspiration and expiration
high pressure alarms are activated by
pressure in the circuit that is too high
-anything that blocks, kinks, occludes, pushes
causes:
-pt. coughing
-gagging
-bronchospasm
-fighting the ventilator
-ETT occlusion
-kink in tubing (clogged)
-increased secretions
-thick secretions
-water in ventilator circuit
low pressure alarms
pressure in circuit is too low
-leaklike, disconnection, something came apart
causes:
-tubing is disconnected
-loose connections
-leak
-extubation
-cuffed ETT or trach is deflated
-poorly fitted CPAP or BiPAP mask
-pt. pulls out tube
Hemodynamic monitoring
terminology for hemodynamic monitoring; continue in following cards
preload
amount of blood returning to right side of the heart (deoxygenated blood from body coming back)
afterload
pressure against which the left ventricle must pump to eject blood out to body
compliance
how easily the heart muscle expands when filled w blood
contractility
strength of contraction of the heart muscle
stroke volume
volume of blood pumped out of each ventricles with each contraction (measured in a percentage)
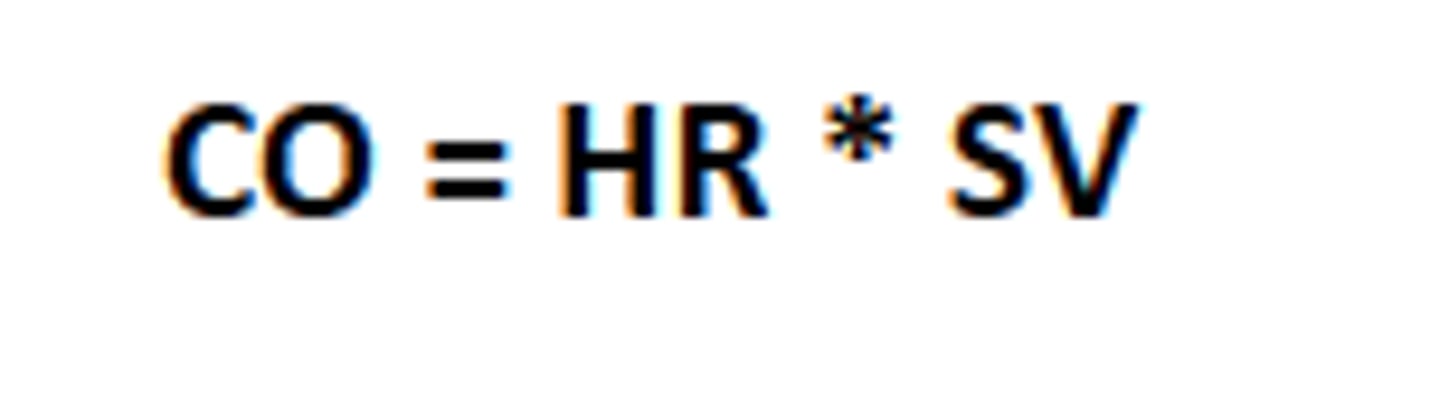
cardiac output
amount of blood pumped out by cardiac system every MINUTE
formula is for CO is SV x HR
why cardiac output so important?
-tissue perfusion
-delivery of oxygen and nutrients to each and every cell in body
-for organ function
poor cardiac output?
-brain: decr. LOC
-heart: chest pain, weak peripheral pulses
-lungs: SOB, crackles, rales
-skin: cool, clammy, mottled extremities
-kidneys: decr. UOP
CO = Stroke volume x heart rate
incr in preload leads to what with CO?
incr in CO (more blood coming back to heart then more blood coming out per min)
incr. in afterload leads to what with CO?
decr. in CO (incr in afterload makes increase in pressure so more difficulty pumping blood w heart, so decr CO)
incr in compliance leads to what in CO?
incr. CO (more expansion)
incr in contractility leads to what in CO?
incr CO (the muscle can contract stronger to pump out blood incr CO)
incr. in stroke volume leads to what in CO?
incr. CO (more blood pumped with each contraction means more blood pumped per min)
causes of dec. CO
-bradycardia (slow HR)
-arrhythmias (pulseless V-tach, V fib, asystole, supraventricular tachycardia)
-hypotension
-myocardial infarction
-cardiac muscle disease
causes of incr. CO
-incr blood volume
-tachycardia
-medications (ace inhibitors = cause vasodilation and decr. afterload, ARBs = decr afterload, nitrates = decr afterload)
-inotropes = incr. contractility
cardiac output
4-8 L/min
cardiac index
2.5-4.0 L/min/M^2
when do you need vasoactive infusions
-cardiac arrest
-hypotension
-shock refractory to fluid resuscitation
-cardiac disease (acquired or congenital)
-decr. cardiac output
Inotropes:
act on force of myocardial contractility (incr. contractility)
vasopressors
mimic sympathetic nervous system to cause vasoconstriction = squeeze veins to incr. BP
-for pt w low BP
adrenergic receptors
receptor sites that sit in vascular smooth muscle, heart, all thru body monitoring to create diff reactions based on what occurs
alpha 1 receptor
found in vascular smooth muscle
-veins
-monitor BP
-when BP goes down = causes vasoconstriction to incr BP
beta 1 receptor
in heart
-monitor BP
-when it goes down it incr. contractility
-incr. SV, HR, and CO
beta 2 receptor
in lungs
-how well dilated the bronchi and vasculature leading to lungs are ok
-are lungs getting enough blood
-causes bronchodilation
epinephrine
-most often used in cold shock
-low doses act on beta 1 receptors: incr contractility, thus incr. CO
-high doses act on alpha 1 receptors: incr. vasoconstriction, incr. BP
norepinephrine
-most often used in warm shock
-acts on alpha 1 receptors: incr. vasoconstriction, thus increasing BP
-incr. cardiac output
dopamine
-used in trauma pt. and cold shock
-low doses used in kidney failure to incr. renal blood flow (renal dopa) :: low doses incr. contractility => incr. CO
-higher doses cause vasoconstriction => incr. SVR => incr. BP
phenylephrine
-used for anesthesia-induced hypotension
-second line agent in some shock pt.
-only acts on alpha 1 : incr. vasoconstriction thus leading to incr. BP
milrinone
used in pt. with cardiogenic shock, decr. cardiac output, congenital/acquired heart defects
-causes systemic vasodilation, pulmonary vasodilation, decr. afterload, incr. contractility
-doesnt incr. oxygen consumption
vasopressin
-antidiuretics hormone (ADH)
-less diuresis => hold onto water => more volume thus more pressure => raises BP
-second line in vasodilatory shock
-third line in septic shock
complications and side effects of vasoactive infusions
-arrhythmia: due to stim. of beta 1 receptors
-hypoperfusion to extremities, kidneys, and GI tract: due to excessive vasoconstriction
-peripheral tissue necrosis: due to hypoperfusion of the skin
-myocardial ischemia (obstructed blood flow to heart): due to incr. myocardial oxygen demand secondary to incr. chronotropy
unconscious pt.
1. try to wake pt, yell and shake them & sternal rub
2. check their pulse (adult: carotid) (infant: brachial) - for no longer than 10 sec.
3. press the code bell and yell for help
priority intervention if they have no pulse
-start chest compressions (100-120 bpm); depth of 2 inches, allow full chest recoil
-have someone get crash cart
CPR cycles
-30 compressions: 2 breaths
-2 minutes
-at 2 min mark: check rhythm and pulse
-if pt. still pulseless, switch compressors and resume compressing
-never stop compressions for more than 10 secs.
shock
-allow AED to analyze rhythm
-follow prompts
-if shock advised, resume compression while device charge
-clear pt. when AED advises
-ensure pt is cleared and administer shock
-immediately resume compressions
infant CPR
2 rescuer: compression to breath ratio is 15:2
1 rescuer: 30:2
use 2 fingers for compression
-compress a depth 1/3 of chest to back diameter