Craniofacial, inflammatory, and vasculopathic disorders of the orbit
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
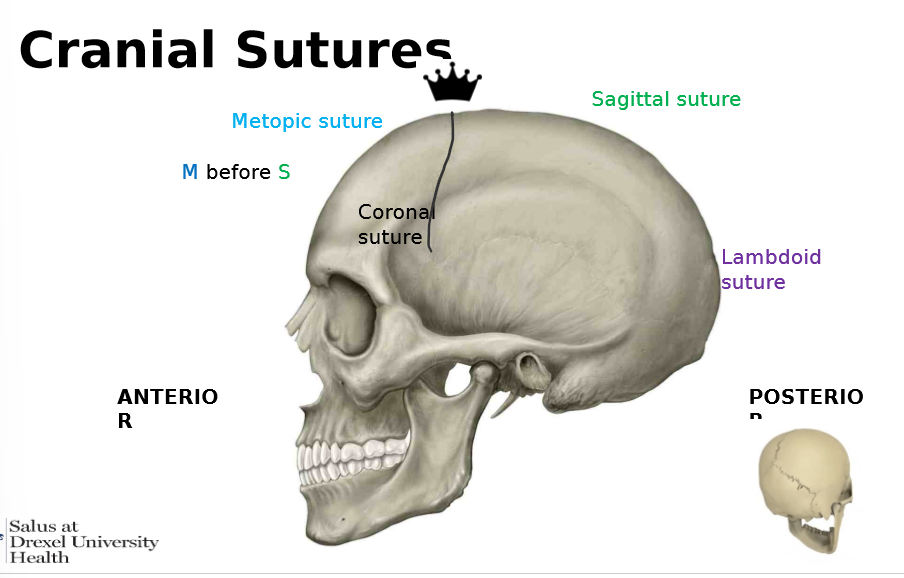
cranial suture
fibrous joints btw the bones of the vault and face
important for cranial vault growth and brain growth (allows for expansion)
once they fully ossify, further expansion is impossible
what are the cranial sutures from anterior to posterior
mesopic suture
sagittal suture
lambdoid suture
craniosynostosis
the premature fusion of the cranial vault suture
results in abnormal skull and brain development
intracranial pressure can be elevated due to brain growht in a confined space
virchows law
the premature fusion of teh cranial vault suture inhibits normal skull growth PERPENDICULAR to the fused suture
a COMPENSATORY growth occurs at the open sutures
the general direction of growth after craniosynctosis is PARALLEL TO THE FUSED SUTURE
what are the ocular manifestations of craniosynostosis
proptosis
papilledema
bilateral ONH swelling due to inc intracranial presure
optic nerve head atrophy
EOM paresis
what are the types of craniosynostosis
scaphelocephaly
trigonocephaly
brachycephaly
oxycephaly
positional plagiocephaly —- NOT a true craniosynotosis
scaphelocephaly cause
premature fusion of the saggital suture
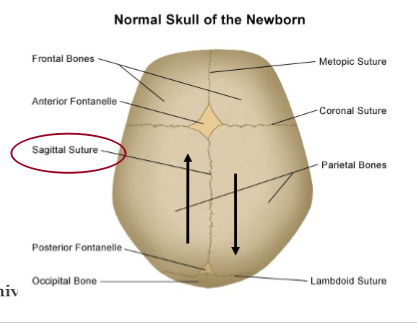
scaphelocephaly appearance
elongation of the cranium anterior to posterior
resembles an inverted boat/ football
scaphelocephy tx
sx
trigonocephaly cause
premature fusion of the metopic suture
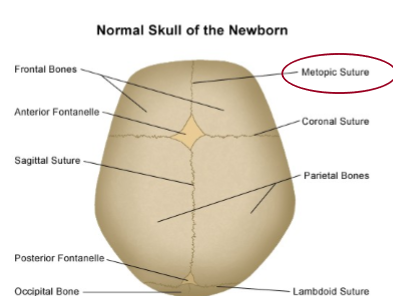
trigonocephaly appearance
high retreating forehead, V shaped
triangle
trigonocephaly tx
sx
brachycephaly caus e
premature fusion of BOTH coronal sutures
can have fusion of one coronal suture
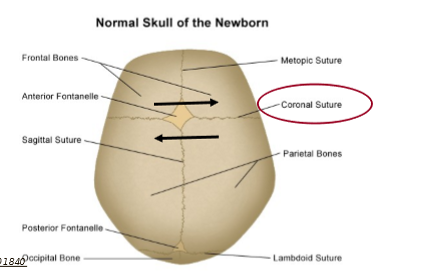
brachycephaly appearance
shortened front to back diameter of the skull
head disproportionately wide
pumpkin?

oxycephaly cause
premature fusion of teh coronal and saggital AND/OR lamdoid sutures
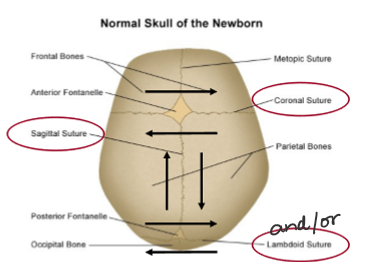
oxycephaly appearance
tower skull or high head syndrome

positional plagiocephaly cause
all sutures are open
most common cause of misshapen head during infancy
back of head is often flatter on one side due to position in womb during pregnancy
more common in twins, triplets, etc
treatment of positional plagiocephaly
ionce the infant has better control of their head
deformity decreases
SO NO TX (maybe a baby helmet)
orbital roof
lesser wing of the sphenoid bone
frontal
THE ROOF IS FRONT-LESS
orbital floor
maxillary
could be involved in blow out fracture
palatine
zygomatic
MY PAL LEFT HIS Zs on the floor
medial wall of the orbit
maxillary
lacrimal
ethmoid
the lamina papyracea of the ethmoid is the thinnest bone and can erode in ethmoid sinusitis infections
sphenoid
SLEM like Slime bc youre near your nose
lateral wall
greater wing of the sphenoid
zygomatic
Greater Z
syndromic craniosynostosis cause
inherited or genetic condition characterized by a collection distinct facial and body abnormalities
can be mild to severe
limb and hand abnormalities can be telling
often have related health and developmental issues
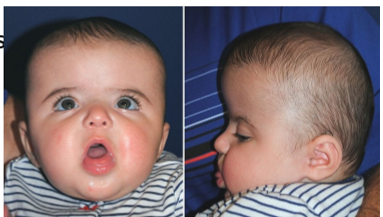
syndromic craniosynostosis diseases (5)
apert syndrome
crouzon syndrome
muenke syndrome
pfeiffer syndrome
saethre - chotzen syndrome
apert syndrome is also called
acrocephalosyndactyly
apert syndrome inheritance
autosomal dominant
apert syndrome appearance
flat elongated forehead
proptosis
underdeveloped midface
fusion of the digits
brachycephaly and/or oxycephaly

crouzon syndrome inheritance
autosomal dom
appearance of crouzon syndrome
wide set proptotic eyes
beaked nose
underdeveloped jaw
dnetal issues - possible cleft lip and palate
no associated hand and feet anomalies
brachycephaly

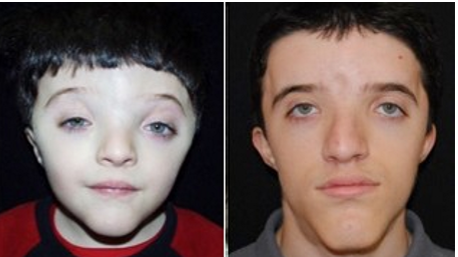
muenke syndrome INHERITANCE
autosomal dom
muenke syndrome appearance
abnormally shpaed head
wide set eyes
flattened cheek bones
mild hand/feet abnormalities
MOST HAVE NORMAL INTELLECT
brachycephaly
pfeiffer syndrome inheritance
autosomal dom
pfeiffer syndrome appearance
abnormally shaped head
wide set eyes
beaked nose
underdeveloped upper jaw
thumbs and big toes point away from other digits
may hae webbing or fusion
hearing issues D

saethre-chotzen syndrome inheritance
autosomal dom
saethre chotzen syndrome appearance
abnormally shaped head
low frontal ahirline
ptosis
wide spaced eyes
broad nasal bridge
facial asymmetry
small ears
fusion of 2nd and 3rd fingers
normal intellect
what do we do for craniosynostosis?
recognize it
refer to pediatric craniofacial subspecialist
most have proptosis
artificial tears
preservative free if doing more than 4x a day
gel or ointment (ung) at bedtime (QHS)
possible lid taping QHS
what are the eyelid tissues from superficial to deep
eyelid skin
subcutaneous areolar layer
orbicularis oculi
orbital and palpebral portion
CN 7
orbital septum
posterior muscular system
levator and mueller muscle
levator - CN 3
mueller - sympathetics
tarsal plate
whatas the arterial supply and venous drainage of the eyelids
lateral palpebral artery (branch of lacrimal artery) + 2. medial palpebral a (banch of ophthalmic a) ==anastomose==> 3. palpebral arcades
whats above the tendinous annulus
lacrimal nerve
frontal nerve
superior ophthalmic vein
trochlear nerve
LFSTUNALI - Large Fluffy Squirrels Take Unexpected Naps Among Lush Ivy!
whats thru the tendinous annulus annulus
Upper division of CN 3
SR
levator
nasociliary nerve
abducens nerve
lower division of CN 3
Large Fluffy Squirrels Take Unexpected Naps Among Lush Ivy!
whats below the tendinous annulus
inferior opthalmic vein
Large Fluffy Squirrels Take Unexpected Naps Among Lush Ivy!
orbital cellulitis presentation
eyelid edema
erthema - swelling
warmth
tenderness
conjunctival infection, chemosis (swelling of conj)
proptosis
febrile and malaise
restricted EOM/pain w eye movement
orbital cellulitis symptoms
red eye
pain
blurred vision
double vision
eyelid swelling
nasal congestion/discharge
sinus headache, congestion, pressure
tooth pain
infra/suprorbital pain
orbital cellulitis cause
• Direct extension from a paranasal sinus infection (especially ethmoiditis)
• Focal periorbital infection
• Dacryoadenitis
• Dacryocystitis
• Dental infections
• Sequela of orbital trauma
• Sequela of orbital surgery or paranasal sinus surgery
• Vascular extension (seeding from a systemic bacteremia)
• Secondary to orbital venous stasis and inflammation from a septic cavernous sinus thrombosis
• Infection by Staphylococcus (adults), Streptococcus (adults), H. influenzae (children)
• Fungal infection in immunocompromised patients (diabetics, HIV, chemotherapy
• Mucormycosis/zygomycosis
• Aspergillus
orbital cellulitis clinical exam
Ask about trauma, surgeries, ear/nose/throat infections, tooth pain/abscess, stiff neck or mental changes
• Palpation of the affected lid assessing for warmth and tenderness
• May need to open eye to assess for:
• Visual acuity
• Reduced in affected eye
• (+) APD
• Indicates compressive optic neuropathy
• Extraocular motilities/restrictions
• Proptosis
• Resistance to retropulsion
• Conjunctival congestion/chemosis
• Dilated fundus exam
• Swollen optic nerve head
• Check for febrile status
what does the ER do for orbital cellulitis
preform a Ct scan w contrast of the orbits and paranasal sinuses to confirm diagnosis
give IV antibiotics stat
CONCERN FOR INFECTION OF THE CNS AND MENINGITIS
REFER IMMEDIATELY
what are the 4 types of idiopathic orbital inflammation
dacryoadenitis
myositis
dacryoadenitis + myositis
orbital apex syndrome
how does idiopathic orbital inflammation (IOI) present
• Usually unilateral, although bilateral more common in children
• Marked tenderness of the involved region
• Lid edema, erythema
• Lacrimal gland enlargement (dacryoadenitis)
• Limitation of and pain with EOM (myositis)
• Proptosis
• Decreased orbital retropulsion
• Conjunctival chemosis
• Reduced corneal sensation
• Increased IOP
what are the symptoms of IOI
• Acute onset of orbital pain
• Decreased vision
• Binocular diplopia •
Red eye
• Headaches
• Fever, nausea, vomiting
whats teh cause of IOI
• Idiopathic acute or chronic inflammatory disorder of the orbital tissue.
• This condition is a diagnosis of exclusion.
what are the differentials for IOI
• Thyroid related ophthalmopathy
• Orbital cellulitis
• Orbital tumor •
Lacrimal gland tumor
• Orbital vasculitis
• Trauma
• Cavernous sinus thrombosis
• Cranial nerve palsy
• Herpes Zoster Ophthalmicus
what do we do in a clinical exam for IOI
• Ask about trauma, surgeries, ear/nose/throat infections, tooth pain/abscess, stiff neck or mental changes •
Palpation of the affected lid assessing for warmth and tenderness •
May need to open eye to assess for:
• Visual acuity
• Reduced in affected eye
• (+) APD •
Indicates compressive optic neuropathy
• Extraocular motilities/restrictions •
Proptosis
• Resistance to retropulsion
• Conjunctival congestion/chemosis
• Dilated fundus exam
• Swollen optic nerve head
• Check for febrile status
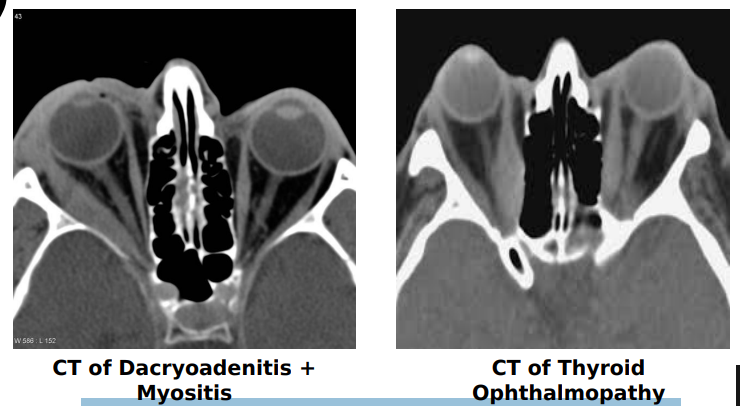
what does the muscle look like in IOI vs thyroid ophthalmopathy
On CT scan, the tendons & extraocular muscles are enlarged in idiopathic orbital inflammation. In thyroid ophthalmopathy, only the muscle belly is enlarged (coke bottle)
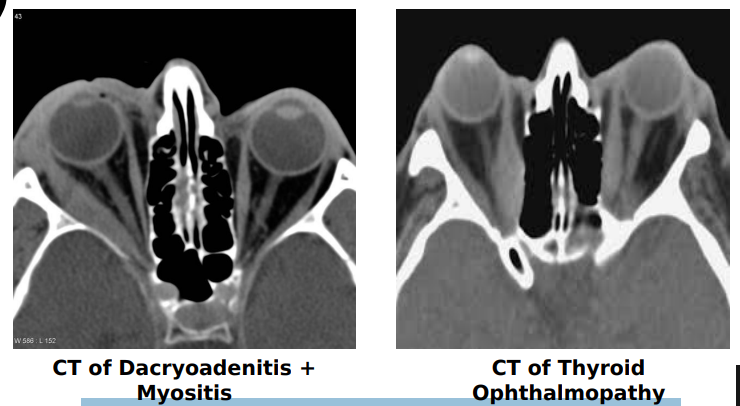
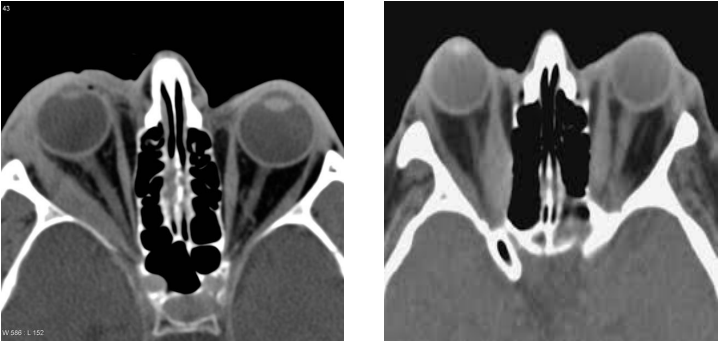
which is Dacryoadenitis + Myositis and which is Thyroid ophthalmopathy
how do we treat IOI
• Admit/refer to ED/hospital for orbital CT scan STAT
• ED to initiate systemic steroids once all other conditions have been ruled out
• ED will run hematology to rule out presence of vasculitis in adults
• (i.e. Wegner’s granulomatosis, Polyarteritis nodosa)
orbital apex syndrome presentation
• Unilateral vision loss with ophthalmoplegia involving multiple cranial nerves
• Vision loss is due to CN II being affected. Optic atrophy can occur weeks to months after initial presentation if no remedied •
Ophthalmoplegia due to involvement of • CN III, IV, VI •
Periorbital facial pain and forehead hypoesthesia due to CNV1 involvement
• Decreased corneal sensitivity
• Mydriasis and ptosis •
Due to CN III involvement
• Proptosis
• Injection/chemosis
orbital apex syndrome symptoms
• Poor vision in affected eye
• Binocular diplopia
• Orbital pain
cause of orbital apex syndrome
• Inflammatory
• Infectious
• Neoplastic
• Iatrogenic/Traumatic
• Vasculopathic
whats the diff diagnosis for orbital apex syndrome
cav sinus syndromes - NO ON involvement
what do we do in a clincial exam for orbital apex syndrom
• Ask about trauma, surgeries, ear/nose/throat infections, tooth pain/abscess, stiff neck or mental changes
• Palpation of the affected lid assessing for warmth and tenderness
• May need to open eye to assess for:
• Visual acuity
• Reduced in affected eye
• (+) APD
• Indicates CN II involvement
• Extraocular ophthalmoplegia
• Proptosis
• Resistance to retropulsion
• Conjunctival congestion/chemosis
• Dilated fundus exam
• Swollen optic nerve head
• Check for febrile status
how do we treat orbital apex syndrome
• Admit/refer to ED/hospital for orbital CT and MRI scan STAT
• ED to initiate systemic steroids once all other conditions have been ruled out
whats the blood supply to the retina
ophthalmic artery —> 2. CRA —> 3. Retina
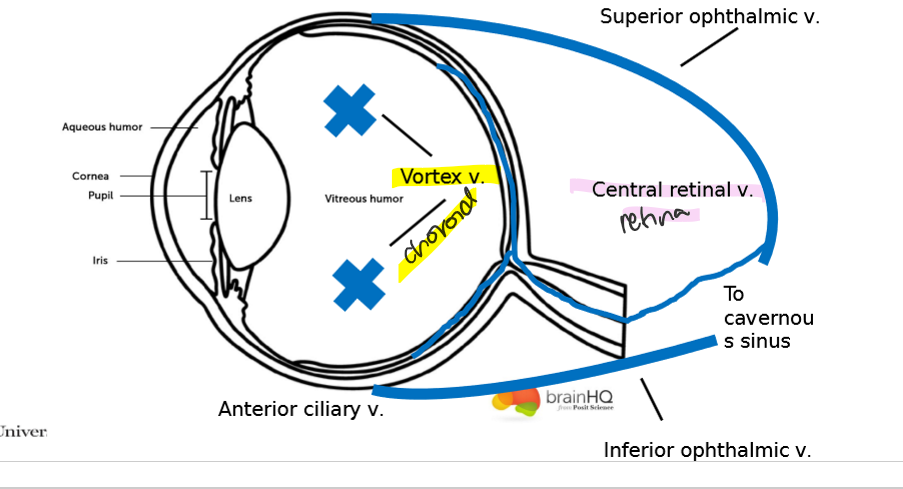
whats the blood flow out of the eye
choroid
vortex vein
retina
central ertinal vein
Sup/
anteiror ciliary vein —> Inf ophthalmic vein
cav Sinus
whats in the cav sinus
3
4
6
V1
V2
sympathetics
ICA
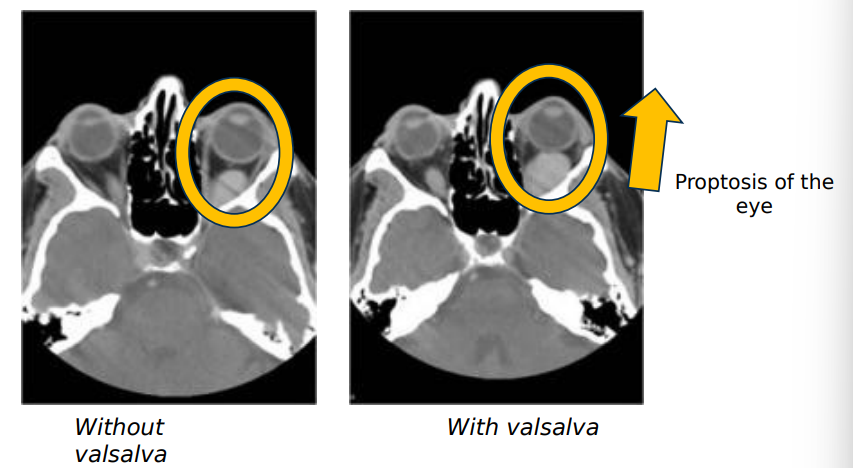
orbital varix presentation
intermittent proptosis of one or both eyes which is non pulsatile and not associated w a brut (rhythmic pattern)
proptosis is precipitated by valsava manuever or compression of jugular veins
inc venous pressure
symptoms of orbital varix
intermittent bulging of eyes on command or w valsalva maneuver
differential diagnosis for orbital varix
carotid cavernous fistula
diagnosis, treatment, management of orbital varix
xray of orbit to rule out mass
pt education
carotid cavernous fistula presentation
• Typically, unilateral presentation
• Red eye
• Chemosis and injection from backup of venous blood
• Pulsatile proptosis
• Orbital bruit
• Decreased visual acuity
carotid cavernous fistula symptoms
• Pulsations of the globe
• Irritated red eye
• Eyelid edema

carotid cavernous fistula diff diagnosis
orbital varix
what does carotid cavernous fistula appearance
pulsatile proptosis
proptosis is beating at the rhythm of the heart
what are the 2 types of carotid cavernous fistulas
high flow or direct fistula
low flow or dural fistula
high flow/ direct fistula
• Characterized by direct connection of internal carotid artery to the cavernous sinus
• 80% of lesions
• Often secondary to closed head trauma
low flow / dural fistula
• Characterized by a connection of the sinus with any of the meningeal branches of the internal carotid
• Often associated with systemic disease (i.e. HTN, connective tissue disorders, atherosclerosis)
diagnosis, treatment, and management of carotid cavernous fistula
• Orbital CT or MRI: enlargement of the superior ophthalmic vein
• Arteriography usually required to identify fistula
• High-flow fistula are closed by surgical repair of the lesion, if possible or embolization with balloon occlusion
• Low-flow fistulas are closed by endovascular balloon occlusion, if possible. May have conservative monitoring with low-flow fistula as some spontaneously resolve.
palliative care (optometrists) for carotid cavernous fistula
we don’t treat the underlying issue
we refer
pt will need to be referred for emergent imaging and initiation of systemic antibiotics/steroids/immunomodulators
proptosis
gel based artificial tears (preservative free) q1hr - PRN
ointments w lid taping QHS
elevated IOP
topical anti hypertensive agent
Alphagan 1 gtt TID in affected eye