Week 5 Homeostasis & Perfusion (CV Care I)
1/58
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
59 Terms
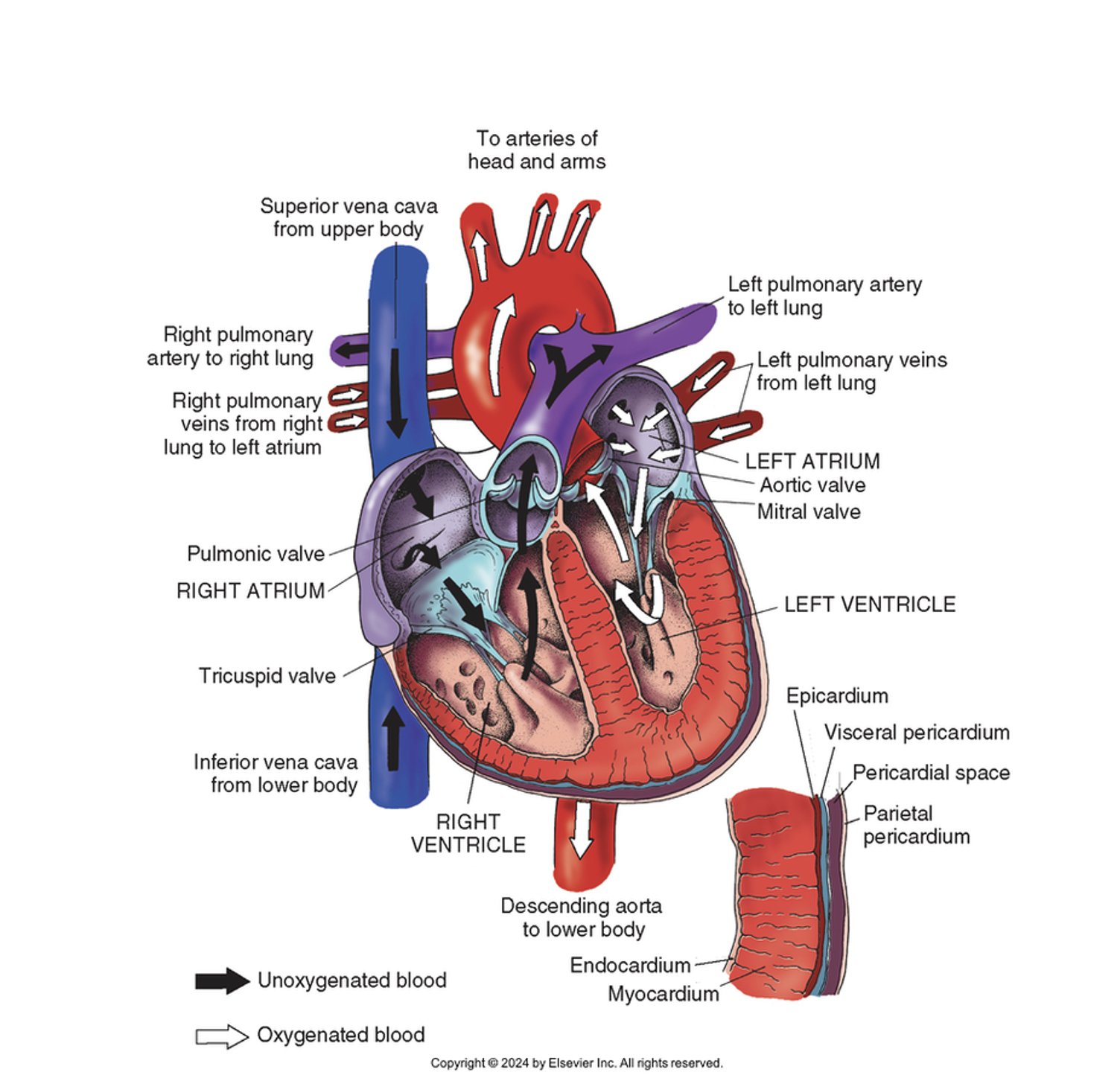
Cardiovascular (CV) System
Responsible for supplying oxygen to organs and other tissues (perfusion) by pumping blood throughout the body
Blood carries oxygen, as well as nutrients/electrolytes/hormones throughout the body, and carries away unwanted CO2 and waste products
All these functions are important, but oxygen is key because cells die quickly without oxygen. All the systems in our body rely on oxygen to function, e.g. moving our muscles, digesting food, and thinking.
Cardiovascular System
Consists of the heart and blood vessels
Heart: myocardium
The heart is a large muscle, the myocardium, which is composed of 4 chambers and valves.
Blood vessels
Arteries: blood vessels that carry oxygenated blood away from the heart
Veins: blood vessels that carry deoxygenated blood back to the heart
Capillaries: small blood vessels that connect your arteries and veins. Facilitate exchange of materials (oxygen, nutrients) between blood & tissues.
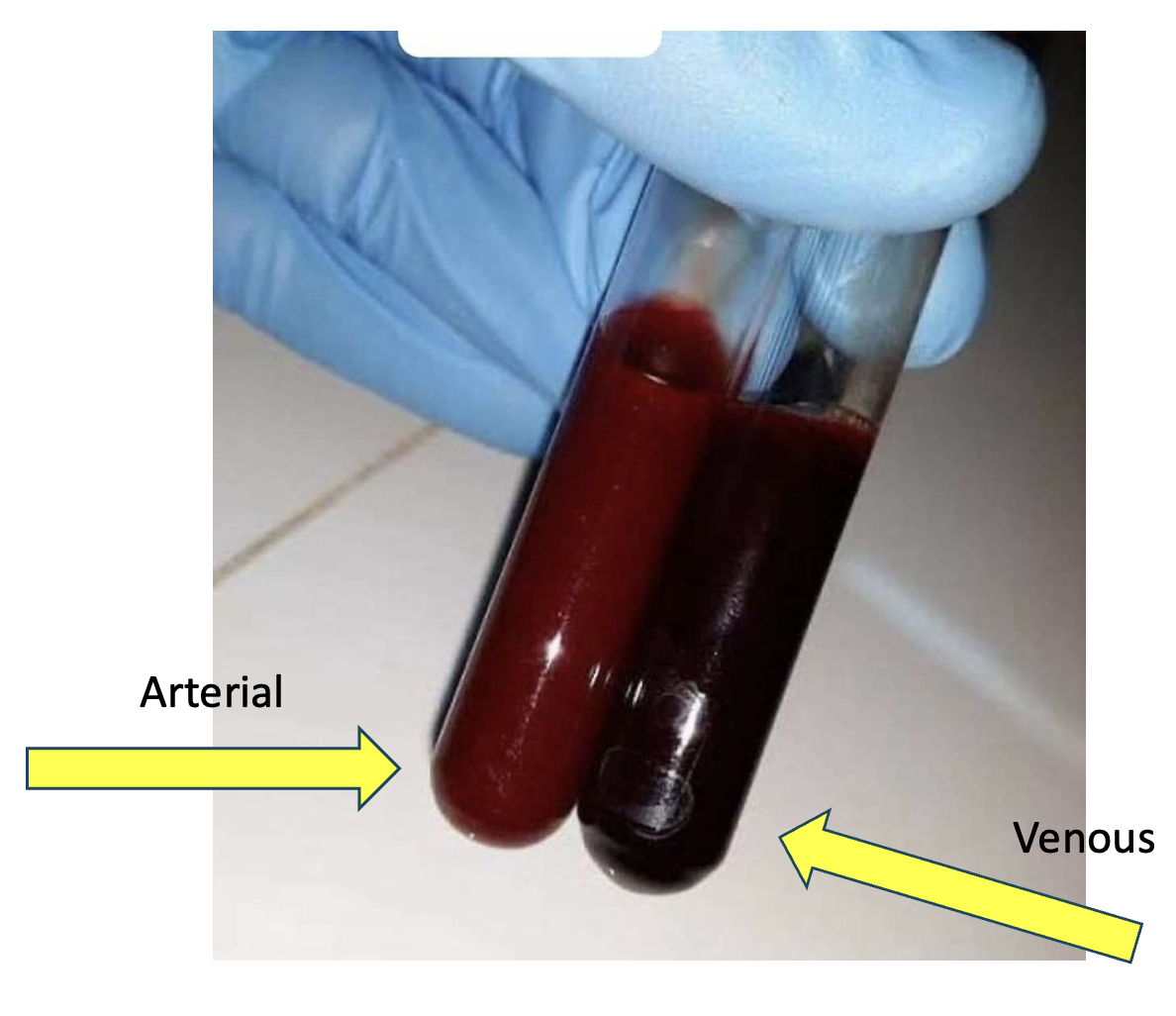
Arterial blood is usually a brighter-red color than venous blood because of the high amt of oxygen in it. In contrast, venous blood has lost a lot of oxygen, so that’s why it looks darker-red.
If you need to get an ABG (arterial blood gas) from your pt, check to make sure the blood is bright red. If it’s really dark, it may be venous blood, which would give you an inaccurate ABG result. Instead, you’d get VBG results (venous blood gas)
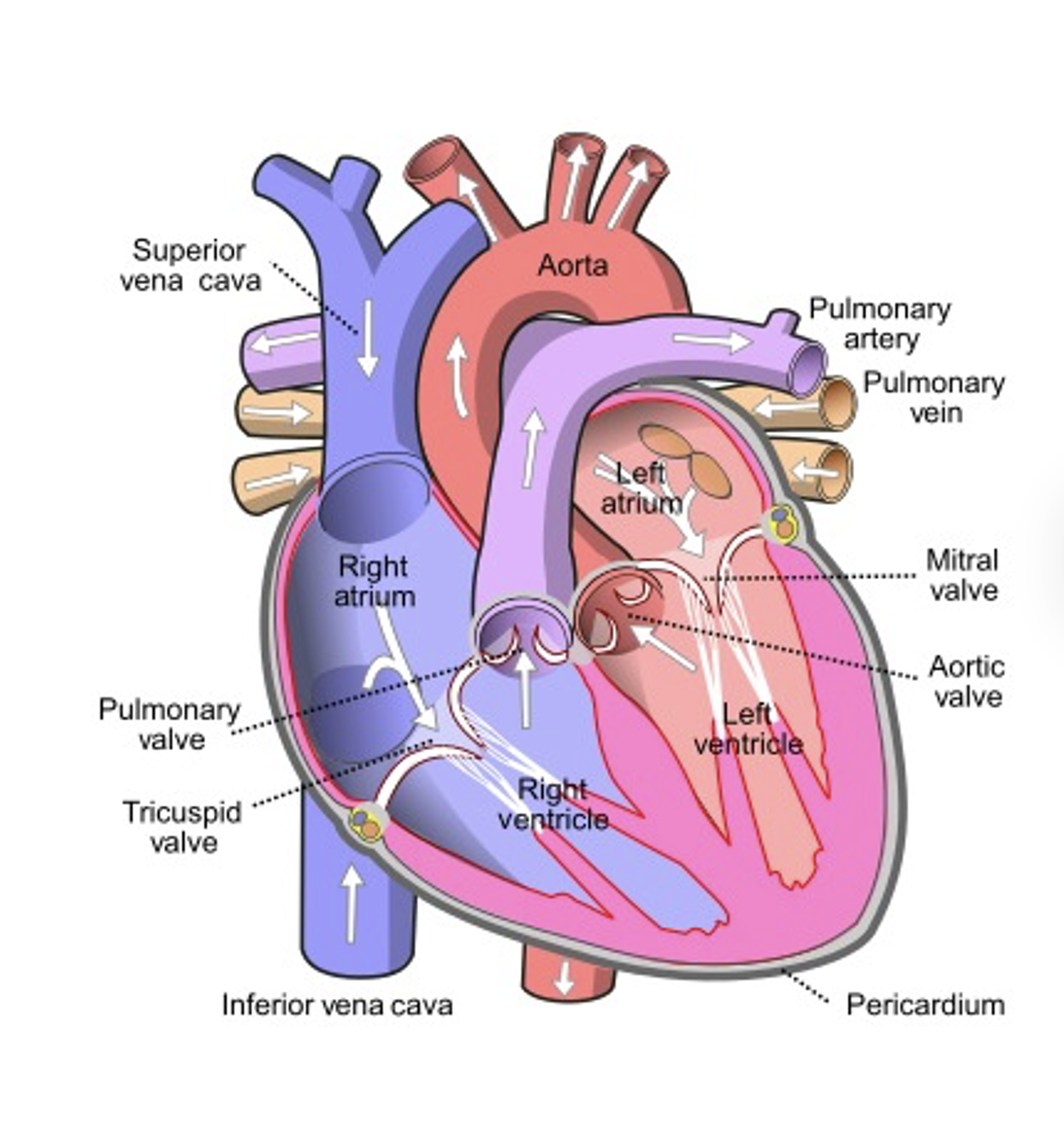
Heart structures
Myocardium (heart muscle)
4 chambers (right atrium, right ventricle, left atrium, left ventricle)
4 valves (tricuspid, pulmonary, mitral, and aortic valve)
Keeps forward flow of blood
S1 heart sound = mitral and tricuspid valves closing
S2 heart sound = aortic and pulmonic valves closing
Pericardium (surrounds & protects heart from trauma & infection)
The heart valves keep blood flowing forward into the next chamber. When the heart valves don’t work efficiently (the valve doesn’t close all the way, or stiff so it doesn’t open/close well) → this can lead to heart murmurs, heart dysrhythmias, blood backing up in your heart, and oxygenated blood mixing w/ deoxygenated blood. Some individuals are born with valve defects, while some develop valve issues later in life from HTN or infection.
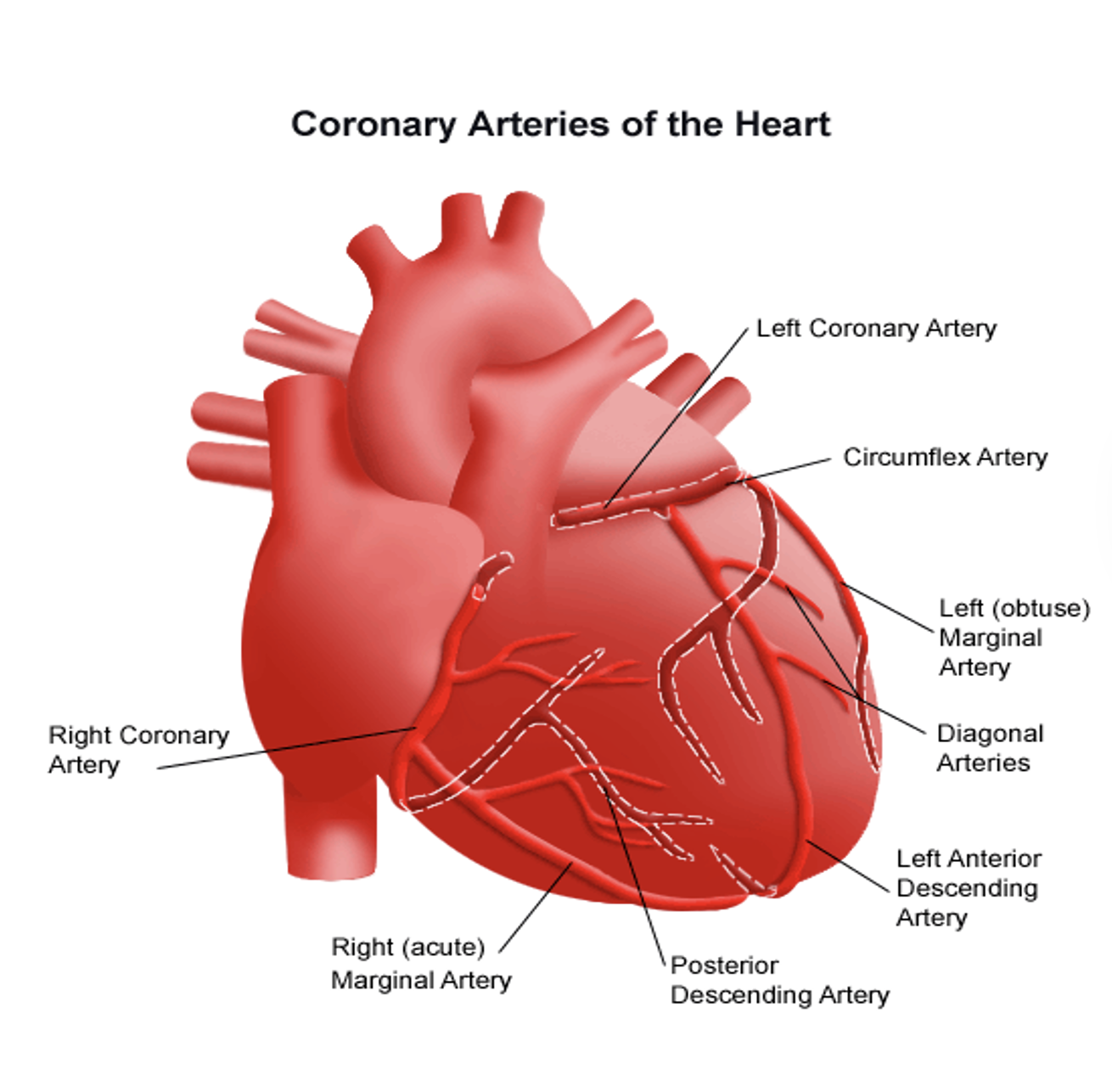
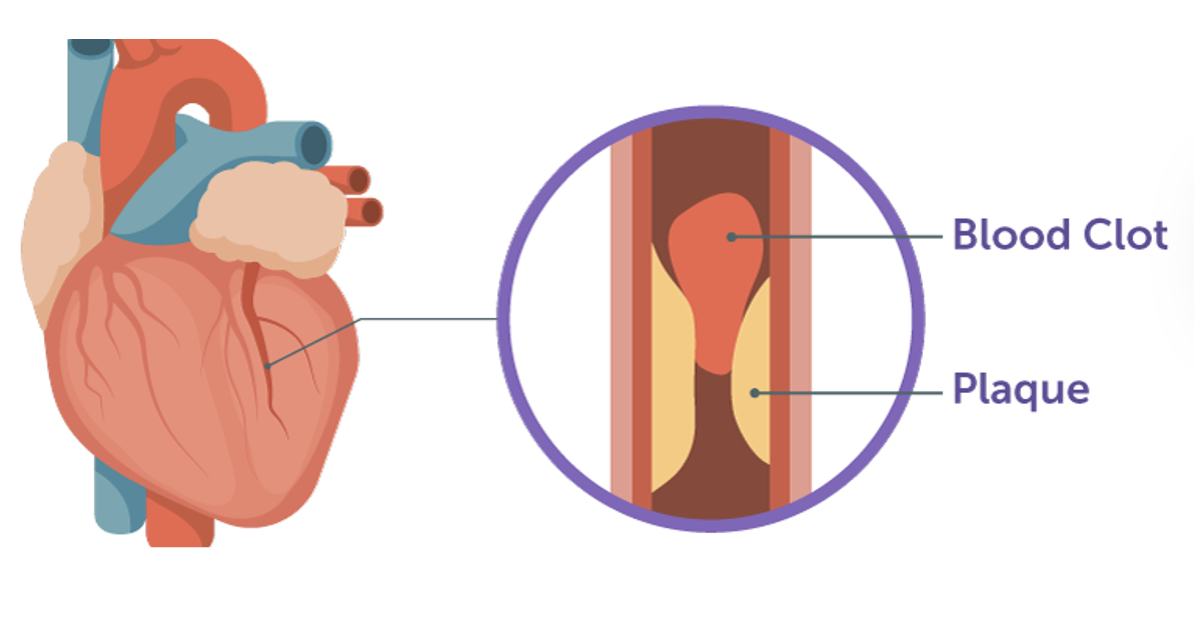
Heart structures - Coronary Arteries
Coronary arteries
Supplies myocardium with blood/oxygen → so myocardium can contract/pump blood/function
Main coronary arteries: right main, left main (left anterior descending & circumflex)
Blockages of coronary arteries → stops blood flow to myocardium → myocardial infarction (aka: heart attack)
There are 2 main coronary arteries:
The right main coronary artery supplies the right atrium and ventricle, the inferior portion of the left ventricle, the posterior septal wall, and the SA and AV nodes.
The left main coronary artery consists of two major branches, the left anterior descending (LAD) and the circumflex arteries.
The LAD artery supplies blood to the anterior wall of the left ventricle, the anterior ventricular septum, and the apex of the left ventricle.
The circumflex artery supplies blood to the left atrium and the lateral and posterior surfaces of the left ventricle.
The coronary arteries supply the capillaries of the myocardium with blood. If blockage occurs in these arteries, the pt is at risk for myocardial infarction (MI).
Cardiac cycle
Cardiac cycle: The beginning of one heartbeat to the beginning of the next one
The phases of the cardiac cycle are: Systole (contraction and emptying of the atria and ventricles) and Diastole (relaxation and filling of the atria and ventricles)
The cardiac cycle begins with atrial systole → ventricular systole (simultaneously w/ atrial diastole) → ventricular diastole
Cardiac muscle contraction (systole) results from the release of large numbers of calcium ions from the sarcoplasmic reticulum (inside each myocardium cell) and the blood. Cardiac muscle relaxes (diastole) when calcium ions are pumped back into the sarcoplasmic reticulum. Basically, calcium released from myocardial cells leads to systole, and calcium going back into myocardial cells leads to diastole
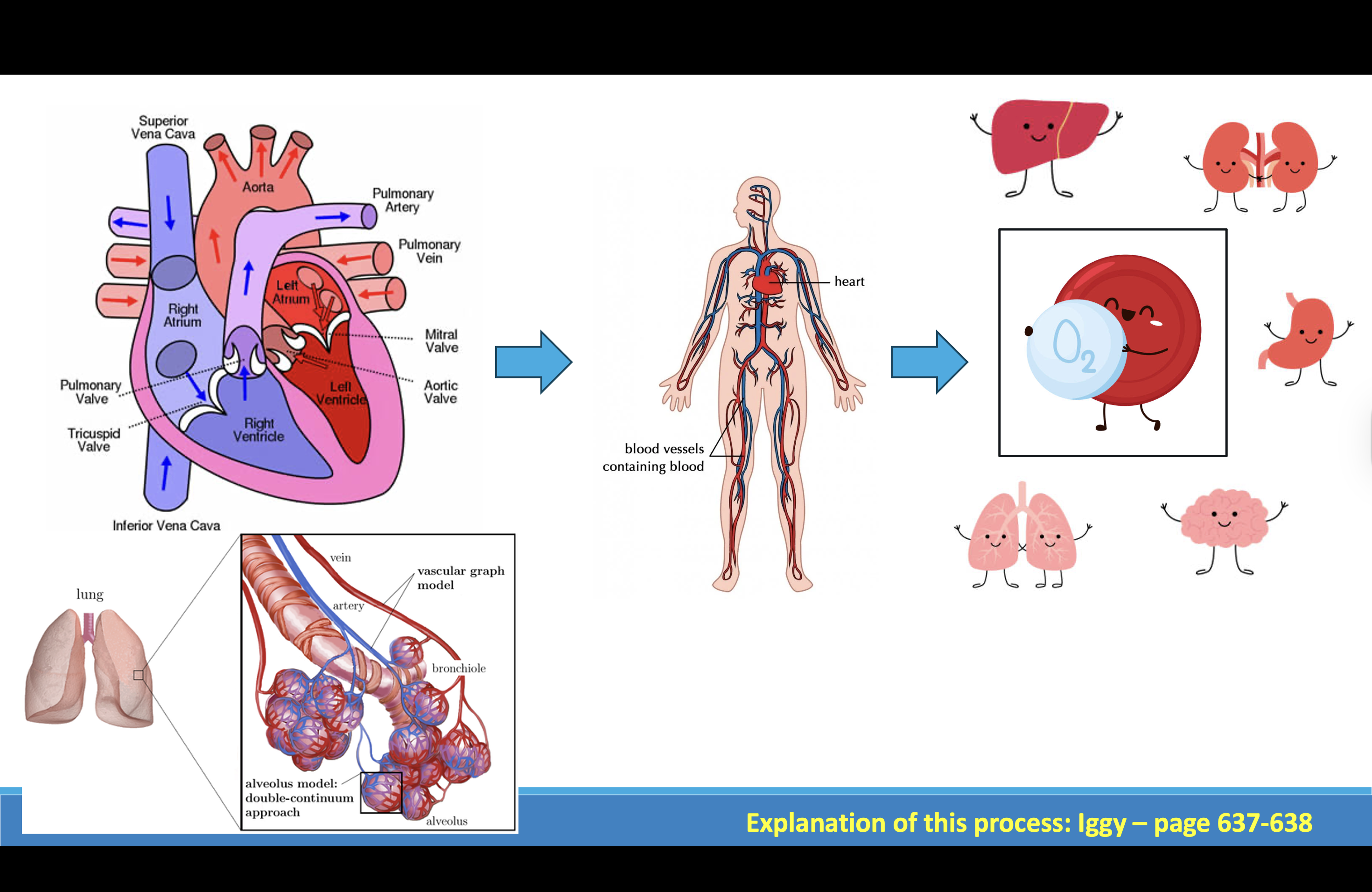
Cardiovascular
We’ve talked about the parts of the cardiovascular system, lets go over how it works as a whole: The main job of the cardiovascular system is to perfuse our body’s cells and organs w/oxygen. The heart receives deoxygenated blood through the IVC/SVC (vena cava). It is then pumped out of the right side of the heart to the lungs, to get oxygenated via the lung capillaries around the alveoli of our lungs (look at picture in the bottom left) where gas exchange happens, the oxygen in the alveoli latch onto a protein, hemoglobin the oxygenated blood travels back to the left side of the heart and is pumped out of the heart via the aorta into our arteries → and then that oxygenated blood travels throughout our body to perfuse our cells, tissues, and organs with oxygen so they can live and function.
Maintaining CV Function
Arteries must be patent so pumped blood can reach rest of the body.
When diseases of the CV system occur gas exchange and perfusion are decreased, which often result in life-threatening events.
CV system works with the respiratory and hematologic systems to meet the human need for gas exchange and tissue perfusion. Any problem in these systems requires the CV system to work harder to meet gas exchange and tissue perfusion needs.
Maintaining CV Function
How can we tell when a patient has decreased gas exchange or decreased perfusion? What are some sx/sx?
Decreased oxygen saturation (lower pulse ox reading)
Tachypneic
Dyspneic
Pale
cyanosis
Cold skin/extremities
Tachycardia
Numbness
Lightheaded
Slow cap refill
Weak pulses
Low BP
Low MAP (< 60 mmHg)
MAP 60-70 mmHg is necessary to maintain perfusion to major organs
-S/S decreased gas exchange: decreased oxygen saturation (lower pulse oximetry reading), might be breathing faster (body is trying to compensate for the lack of O2 – so your autonomic system is telling your lungs to breath more).
S/S of decreased perfusion: cold, pale skin/extremities, slow cap refill, weak pulses, low blood pressure. There’s also another way to assess for decreased perfusion… when you get a pt’s BP: you get 3 kinds of #s: systolic BP, diastolic BP, and the MAP. So the MAP (mean arterial pressure) is a numeric representation of perfusion. A MAP between 60 and 70 mm Hg is necessary to maintain perfusion of major body organs, such as the kidneys and brain.
The official definition of MAP is the arterial blood pressure necessary to maintain perfusion of major body organs.
Limited blood supply going to major organs such as brain
Measuring blood pressure
Blood pressure (BP) - the force of blood exerted against the vessel walls.
BP is determined primarily by cardiac output (the volume of blood ejected by the heart each minute) and by the resistance in the arterioles.
Causes of resistance in arterioles: vasoconstriction (medications, hypothermia, heart failure, stress, shock)
Systolic BP - the amount of force generated by the left ventricle to distribute blood into the aorta with each contraction of the heart. It is a measure of how effectively the heart pumps and is an indicator of vascular tone.
Diastolic BP - the amount of force against the arterial walls during the relaxation phase of the heart.
Mean Arterial Pressure (MAP) - the arterial blood pressure necessary to maintain perfusion of major body organs
BP is regulated by balancing the sympathetic and parasympathetic nervous systems of the autonomic nervous system. Changes in autonomic activity are responses to messages sent by the sensory receptors in the various tissues of the body. These receptors, including the baroreceptors, chemoreceptors, and stretch receptors, respond differently to the biochemical and physiologic changes of the body.
Baroreceptors (in arch of aorta and internal carotid arteries) are stimulated when the arterial walls are stretched by an increased BP. Impulses from these baroreceptors inhibit the vasomotor center in the brain → drops BP
So what that means is these baroreceptors w/in our arteries help keep our BP steady. They can sense when there is an increase in BP in our body, so it sends messages to our brain to inhibit whats called the vasomotor center → which then helps bring our BP back down.
***Unfortunately as we age, these baroreceptors become less sensitive, so they don’t sense changes in BPs as well. So that’s why our elderly pts are at risk of getting dizzy and falling if they get OOB or stand up too fast. Because when you get up too fast, your BP can drop and less blood is going up into your brain due to gravity → but normally your baroreceptors fixes this because it can sense this low BP w/in the artery walls. And it then sends a message to your brain → Your brain tells your blood vessels to tighten up in order to raise your BP. But in elderly pts, that doesn’t happen as efficiently, so their BP may remain low when standing up, so then they get dizzy and fall.
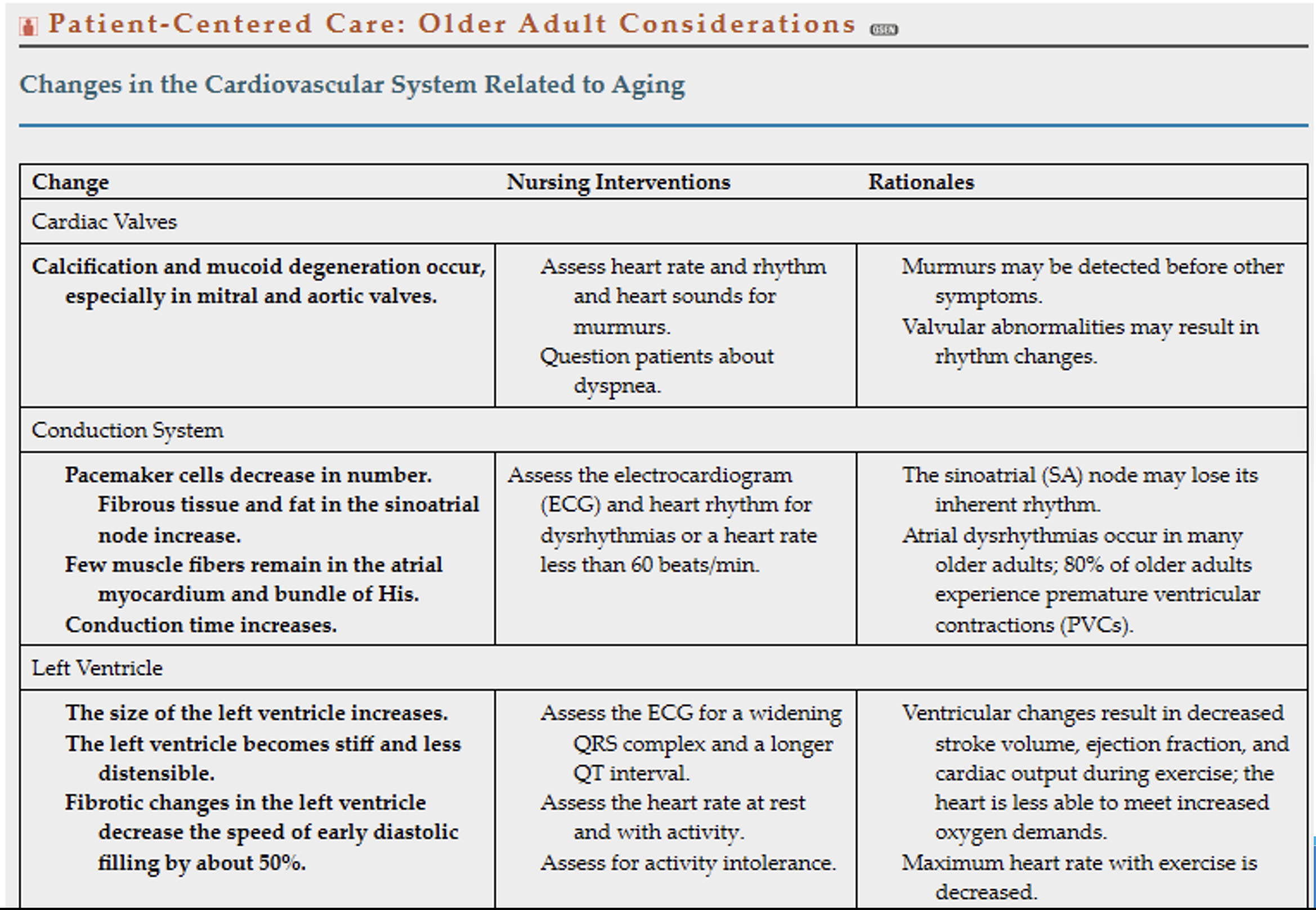
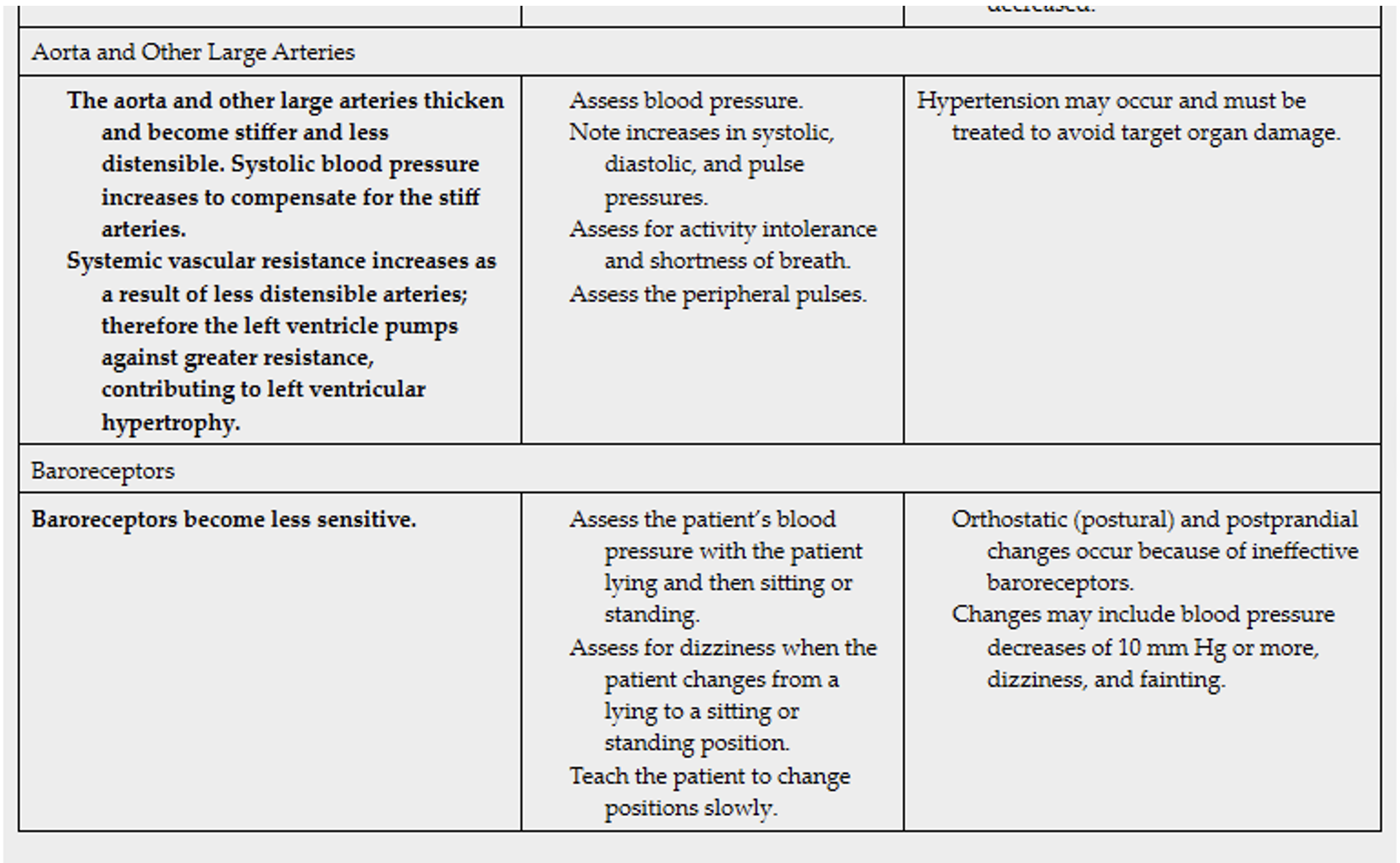
Patient-Centered Care: Older Adult Considerations
Calcification in your mitral and aortic heart valves can develop in older adults → causes the valves to not open and close efficiently so then blood starts to back up in the heart. Thus, the heart needs to work harder to pump sufficient blood through the valve. The harder your heart works to compensate for this loss,
Conduction system is an electrical impulse system that controls how fast our heart beats and the rhythm it beats at. Over time w/ age, the muscle fibers and cells that make up this system start to weaken → this results in a lower HR and heart dysrhythmias. That’s why it’s important to assess our elderly pts for bradycardia (low HR < 60 ) and assess their heart rhythm on their ECG to look for any abnormalities. The time it takes for impulses to go through the heart increases
Left ventricle becomes stiffer w/ age → more at risk of developing ventricular heart dysrhythmias.
Aorta also becomes stiffer with age → and the BP becomes higher to compensate for this (so your heart has to pump even harder to get blood through the aorta which is another reason why so many elderly pts have HTN)
Lastly, baroreceptors get less sensitive w/ age. And we already talked about this. So be sure to maintain fall precautions for this pt population. Teach pts to change positions slowly. Assess for dizziness. Make sure to use a gait belt.
Cardiovascular Disease (CVD)
According to the World Health Organization, cardiovascular diseases (CVDs) are a group of disorders of the heart and blood vessels. They include:
Coronary Heart Disease – a disease of the blood vessels supplying the heart muscle;
Cerebrovascular Disease – a disease of the blood vessels supplying the brain;
Peripheral Arterial Disease – a disease of blood vessels supplying the arms and legs;
Rheumatic Heart Disease – damage to the heart muscle and heart valves from rheumatic fever, caused by streptococcal bacteria;
Congenital Heart Disease – birth defects that affect the normal development and functioning of the heart caused by malformations of the heart structure from birth;
PEs and DVTs – blood clots in the lung; blood clots in the leg veins, which can dislodge and move to the heart and lungs.
Atherosclerosis: thickening or hardening of the arteries caused by buildup of plaque in the inner lining of an artery
Assessing for CVD
Assess nonmodifiable (uncontrollable) risk factors: patient’s age, gender, ethnic origin, and family history of CVD.
Assess modifiable (controllable) risk factors: personal lifestyle habits, including diet, cigarette smoking, physical inactivity, overweight/obesity (BMI > 25), and psychological variables.
Exercise recommendation: 150 mins of moderate exercise or 75 mins of vigorous exercise/ week (or a combination of the two) plus completing muscle-strengthening exercises at least 2 days/ week
Assess past medical history → HTN, hyperlipidemia, and diabetes contribute to CVD
Per AHA & Iggy text, hypertension is SBP > 130 or DBP > 80
Hyperlipidemia - triglycerides: Females > 135 and Males:> 160, cholesterol > 200
Modifiable: personal lifestyle habits (diet high in cholesterol, fat, sodium, sugar)
Psychological variables: emotional stress, anger, depression
Assessing for CVD
CVD signs/symptoms: chest pain or discomfort, dyspnea, fatigue, palpitations, weight gain, syncope, and extremity pain.
Chest pain can arise from a variety of sources, so do thorough pain assessment (use PQRST method)
Ask whether the patient has noticed a weight gain, tightness of shoes, indentations from socks, or tightness of rings.
Assess for pitting edema.
Assess skin for decreased perfusion → skin cold and pale (cyanosis → later sign of decreased perfusion)
Pulses weak, diminished
Carotid artery bruit (turbulent blood flow in narrowed/atherosclerotic arteries)
Assessing for pain: PQRST: P, precipitating or palliative (What brings it on? What makes it better or worse?); Q, quality or quantity (How does it look, feel, or sound?); R, region or radiation (Where is it? Does it spread anywhere?); S, severity scale (How bad is it [on a scale of 0 to 10]? Is it getting better, worse, or staying the same?); T, timing (Onset, duration, and frequency?
Assessing for CVD
Extremity pain may be caused by 2 conditions: ischemia (aka: inadequate blood perfusion) from atherosclerosis & venous insufficiency of the peripheral blood vessels.
Cramping in legs associated with activity (ex: walking) → intermittent claudication r/t decreased arterial tissue perfusion (ischemia) → Resting or lowering the affected extremity to decrease tissue demands or to enhance arterial blood flow usually relieves claudication pain.
Leg pain from prolonged standing or sitting is r/t venous insufficiency from incompetent valves or venous obstruction → Elevating the extremity may relieve pain.
Peripheral edema common in patients with CV problems.
Localized edema in one extremity may be d/t venous obstruction (thrombosis) or lymphatic blockage of the extremity (lymphedema)
Venous insufficiency is when your leg veins have a hard time getting blood to flow back up to the heart.
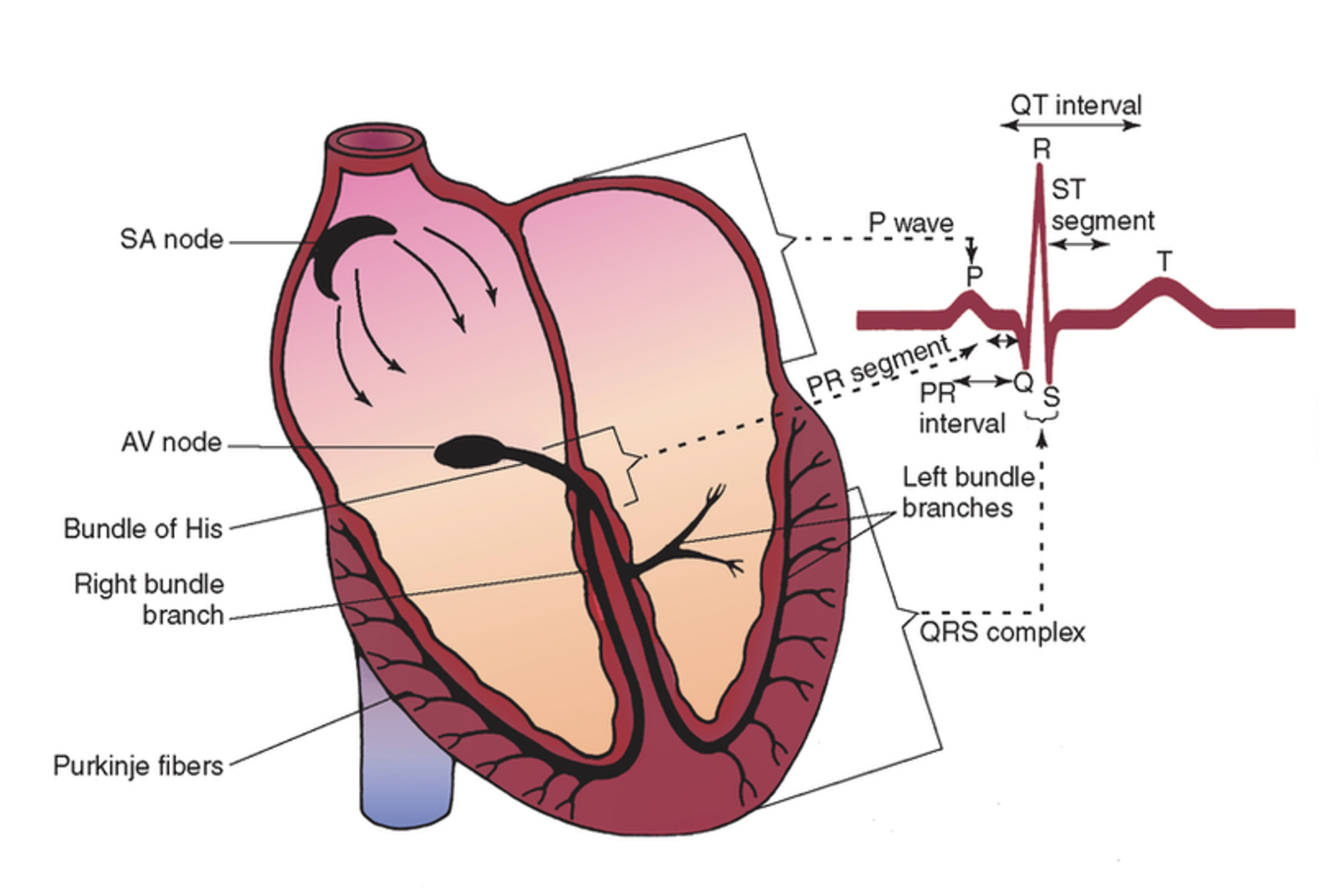
Cardiac Conduction System
The heart conduction (electrical) system is a network of nodes, cells and electrical signals that causes the heart to contract (systole) and expand (diastole) → to produce a heartbeat. For your heart to beat, electrical signals travel through the heart muscle (myocardium). These signals make different parts of your heart contract and expand. To start this process, your brain sends signals to the autonomic nervous system (regulates unconscious body processes) then into the heart. Once it reaches the heart, it sends an electrical pulse through your heart muscle, which makes the chambers of your heart squeeze in a specific order, creating a heartbeat.
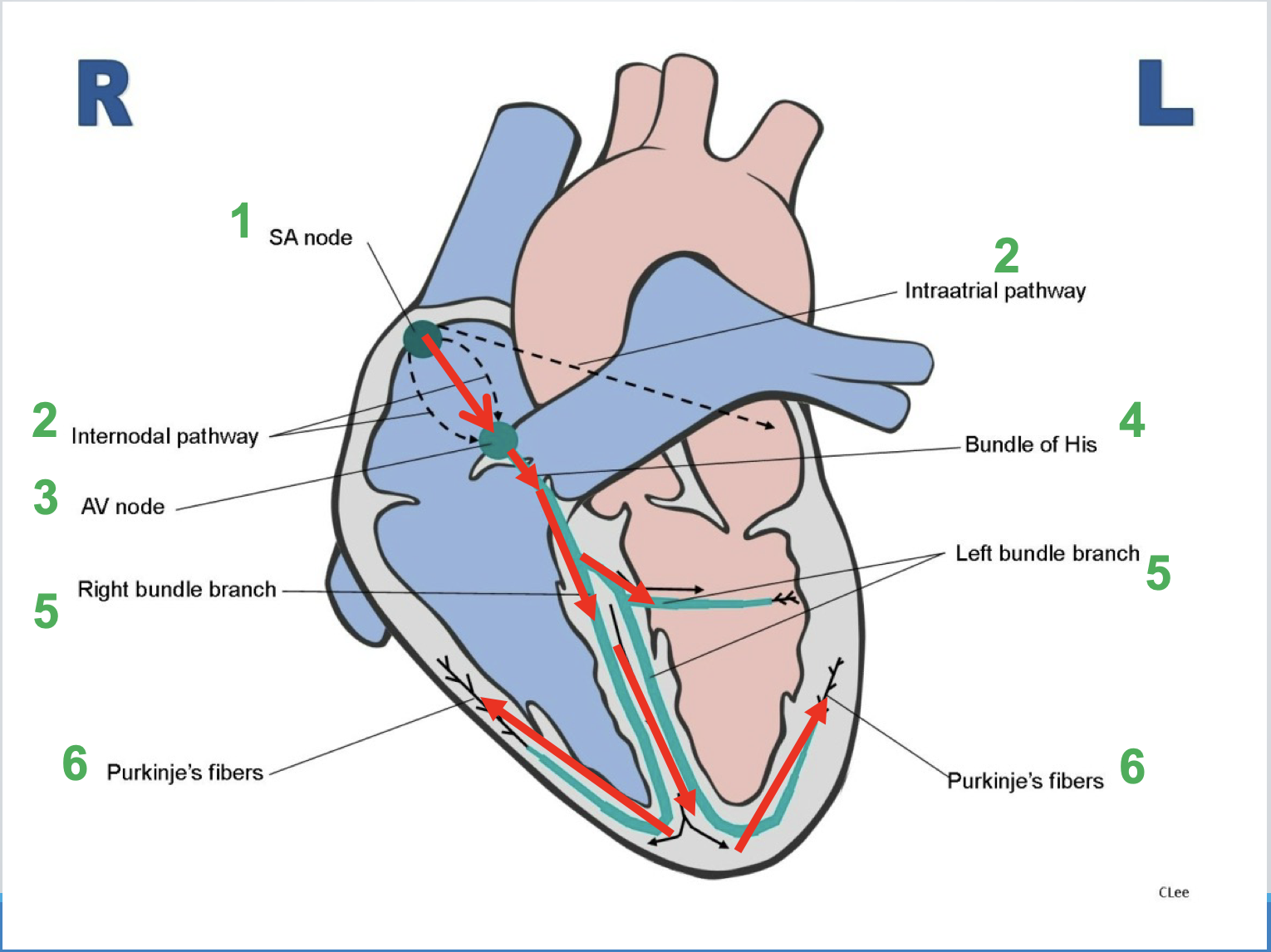
HEART CONDUCTION SYSTEM
SA node: normal pacemaker of the heart
Internodal/intraatrial pathways: transmits impulse throughout the atria → atrial depolarization → atria contract
AV node: relays electrical impulse to ventricles
Bundle of His: muscle fibers the carry impulse through upper part of ventricles
Bundle branches: impulse splits into left and right branches of ventricles
Purkinje fibers: causes rapid conduction of electrical impulses throughout ventricles → ventricular depolarization → ventricles contract
Completion of one cardiac cycle = 1 heartbeat
This is the order in which our heart conduction system works: once the autonomic nervous system sends a signal down to the heart → the Electrical signal starts at a group of cells inside the heart called the: sinus node (SA node) = it’s also known as the heart’s natural pacemaker. In adults, the SA node normally creates an electrical signal 60-100 times/minute → which is why a normal heart rate for adults is 60-100 = called “normal sinus rhythm”
Electrical impulse starts in the SA node and moves across both atria → atrial contract → once at the AV node, the impulse then moves through the ventricles. In the ventricles, the impulse travels through the Bundle of HIS and then splits in the right and left bundle branches. From there it quickly spreads through both ventricles by the Purkinje Fibers, and ventricles contract.
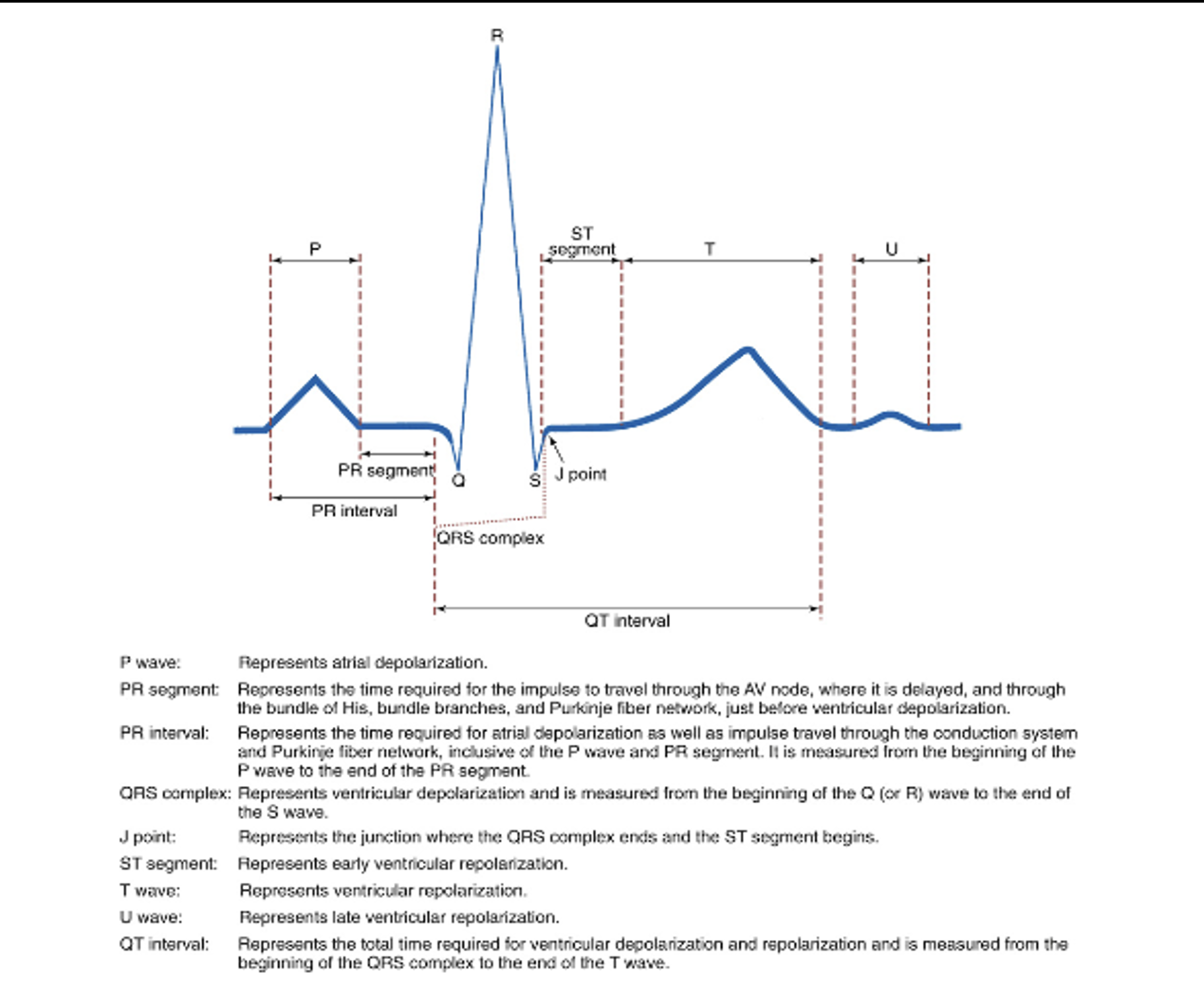
Electrocardiogram (ECG or EKG)
Graphic representation of cardiac electrical activity
Atrial depolarization → atrial contraction (systole)
Ventricle depolarization → ventricle contraction (systole)
Ventricle repolarization → ventricle relaxation (diastole)
Voltage and time it takes for each step of heart conduction to occur
Heart Rate
Electrocardiogram, is the graphic representation of cardiac electrical activity also called ECG or EKG – same thing. EKG is the abbreviation of the German spelling of electrocardiogram b/c that’s where this test was originally invented. Basically, an ECG shows heart conduction in the form of waveforms.
Depolarization is the process by which the membrane potential of a cell becomes more positive, due to the influx of positively charged ions such as sodium (Na+) or calcium (Ca2+). Which then causes the cell to become electrically charged → action potential → causes the heart muscle to contract
Repolarization refers to the process by which the membrane potential of a cell resets itself and returns to a resting state after depolarization.
** Can’t see atrial repolarization on ECG because it occurs so fast and happens simultaneously as depolarization of ventricles
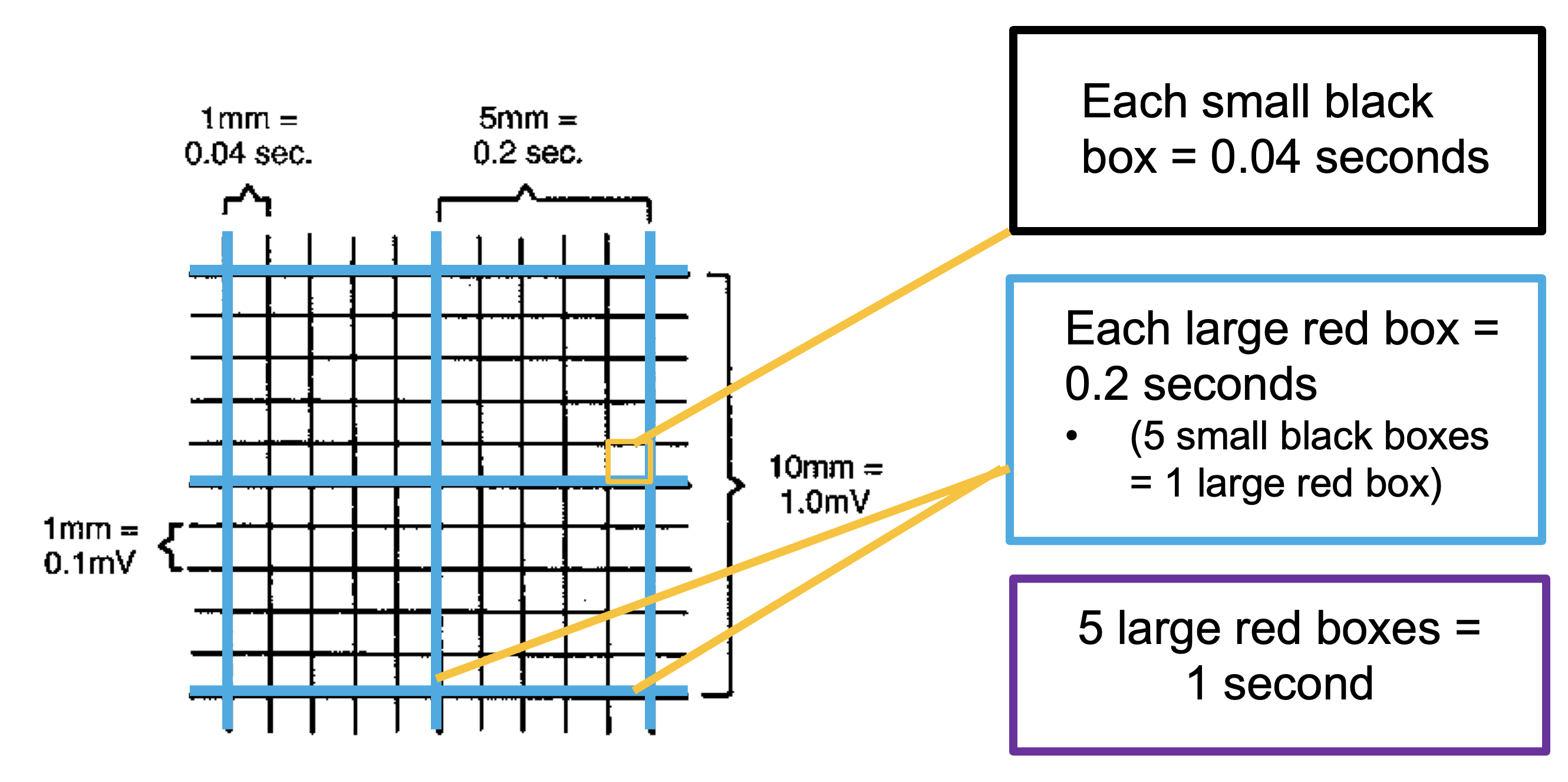
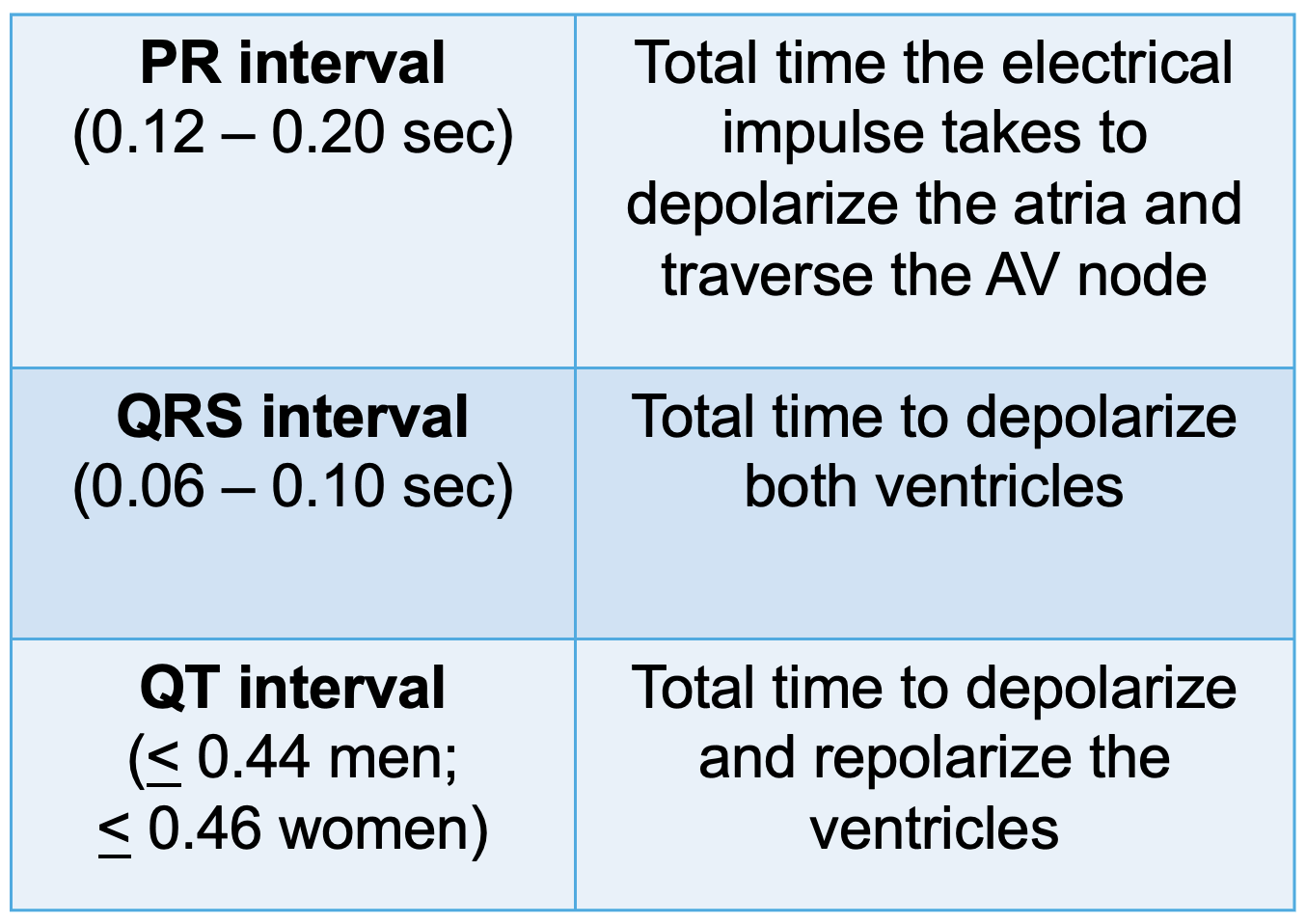
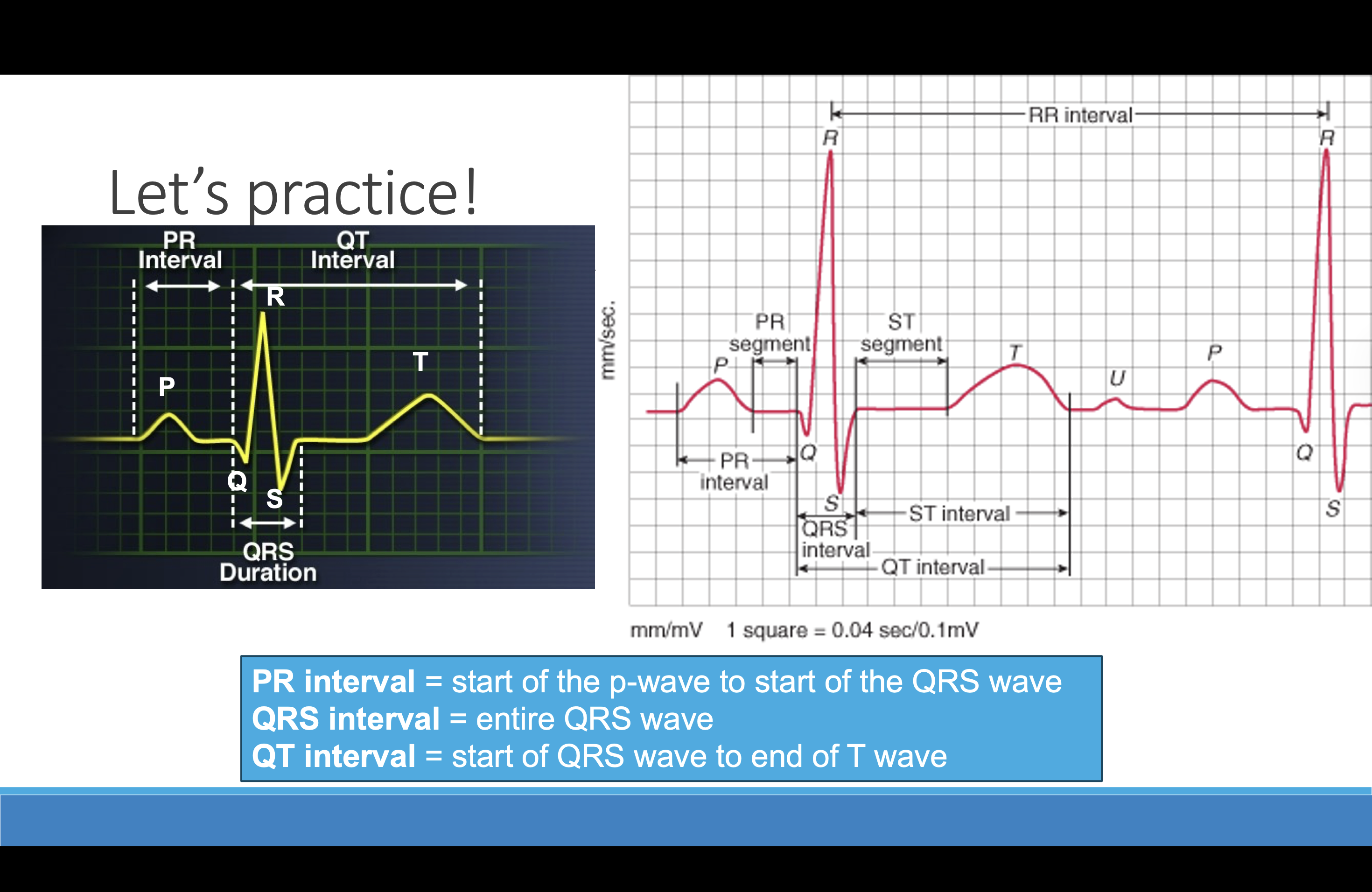
EKG Basics
Each of these boxes represents seconds and amplitude.
By counting the # of boxes, you can calculate how long it takes for each phase of heart conduction to occur and how strong the heart’s electrical current is.
Graph: Millivolts (vertically)
Seconds (horizontally)
* As a nurse, what will be important to you is measuring the seconds it takes for heart conduction to occur because that’s how you identify whether your patient has a regular or irregular heart rhythm.
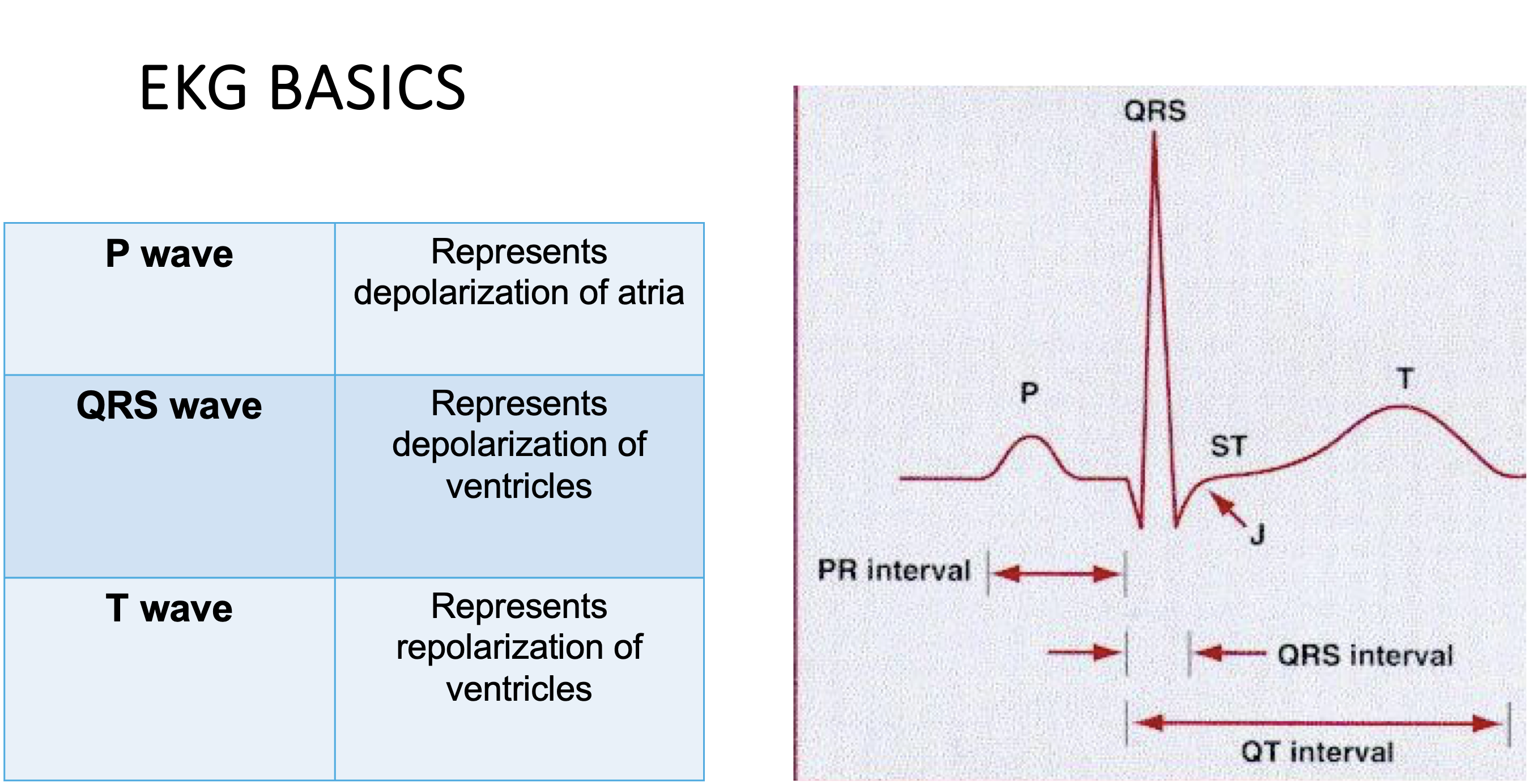
EKG basics
Each heart rhythm consists of several waveforms and intervals. Lets start w/ waveforms. There’s a total of 3 major wave forms: P wave, QRS wave, and T wave.
QT interval: Not used to diagnose a rhythm but used to monitor the affects of antiarrhythmic therapy or as an indicator of potential arrhythmias.
Prolonged QT interval: Means it takes longer than usual for the heart to recharge in between beats (conduction delay in the ventricles). This can upset the normal timing of the heartbeat and cause sudden fast dysrhythmias, which can be lethal. There are certain meds we can’t give if the QT interval is too long, and then for some the docs usually order an EKG first on the pt first before prescribing the med. Ex: Antipsychotics like Haldol. Antiarrhythmics: Amiodarone
EKG Basics
U – wave: not always present. May result from slow repolarization of ventricular Purkinje fibers. May be due to electrolyte abnormality, usually hypokalemia
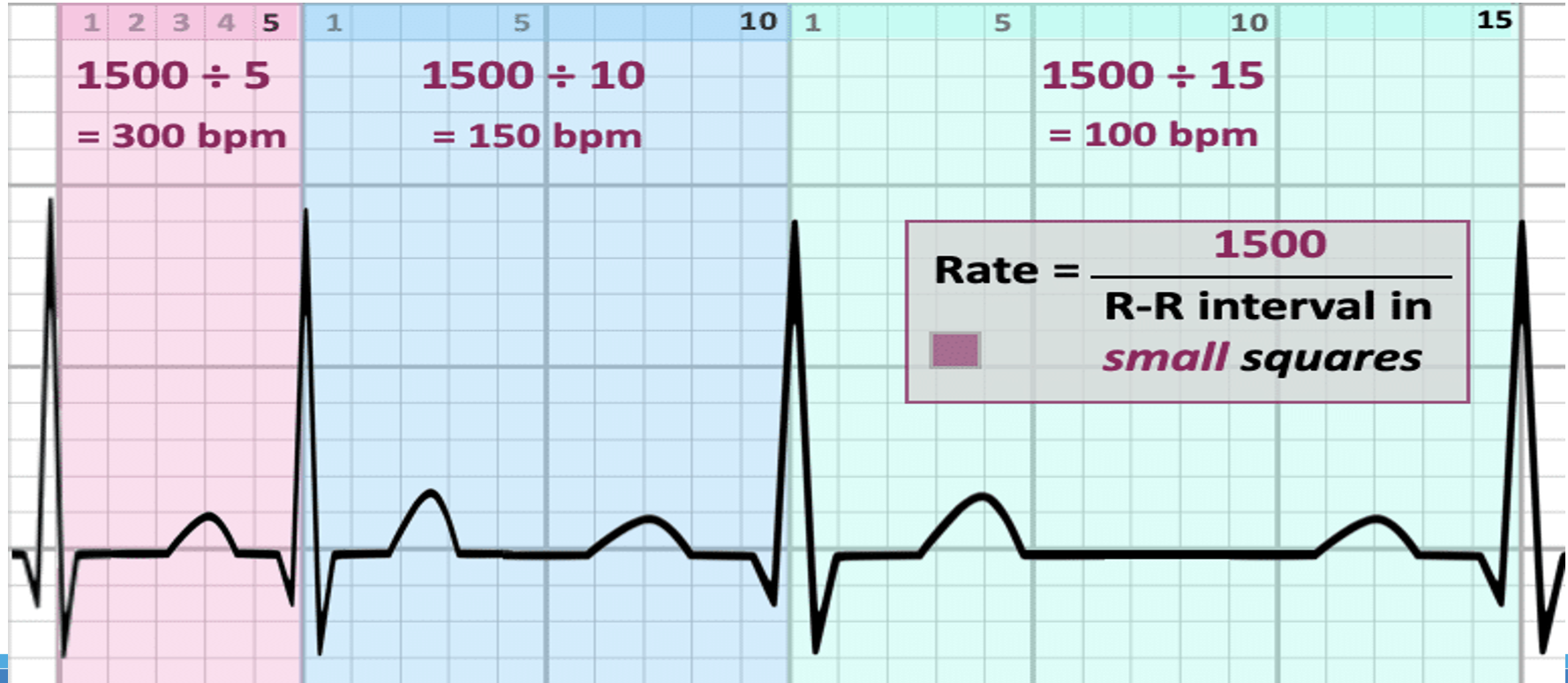
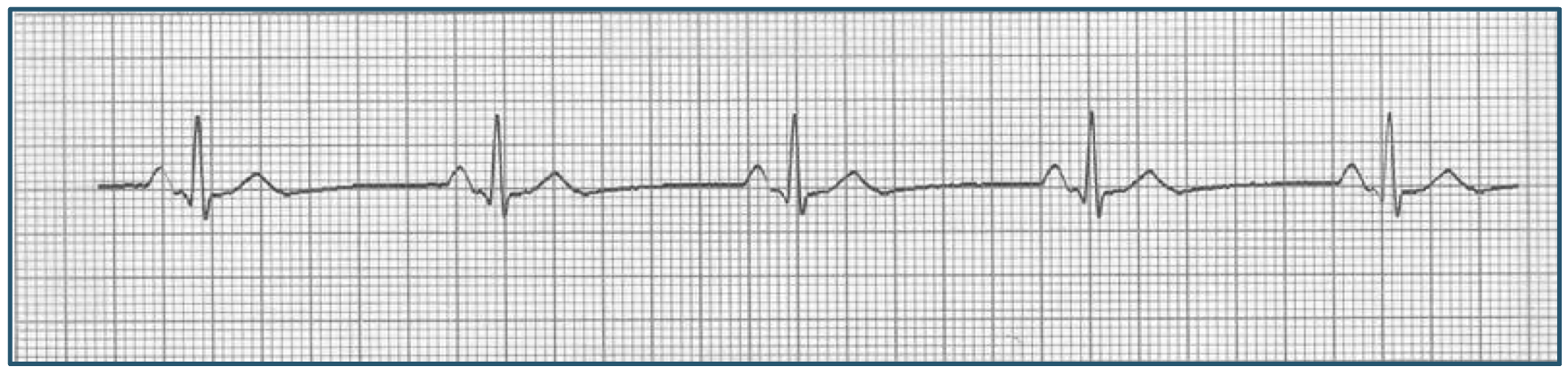
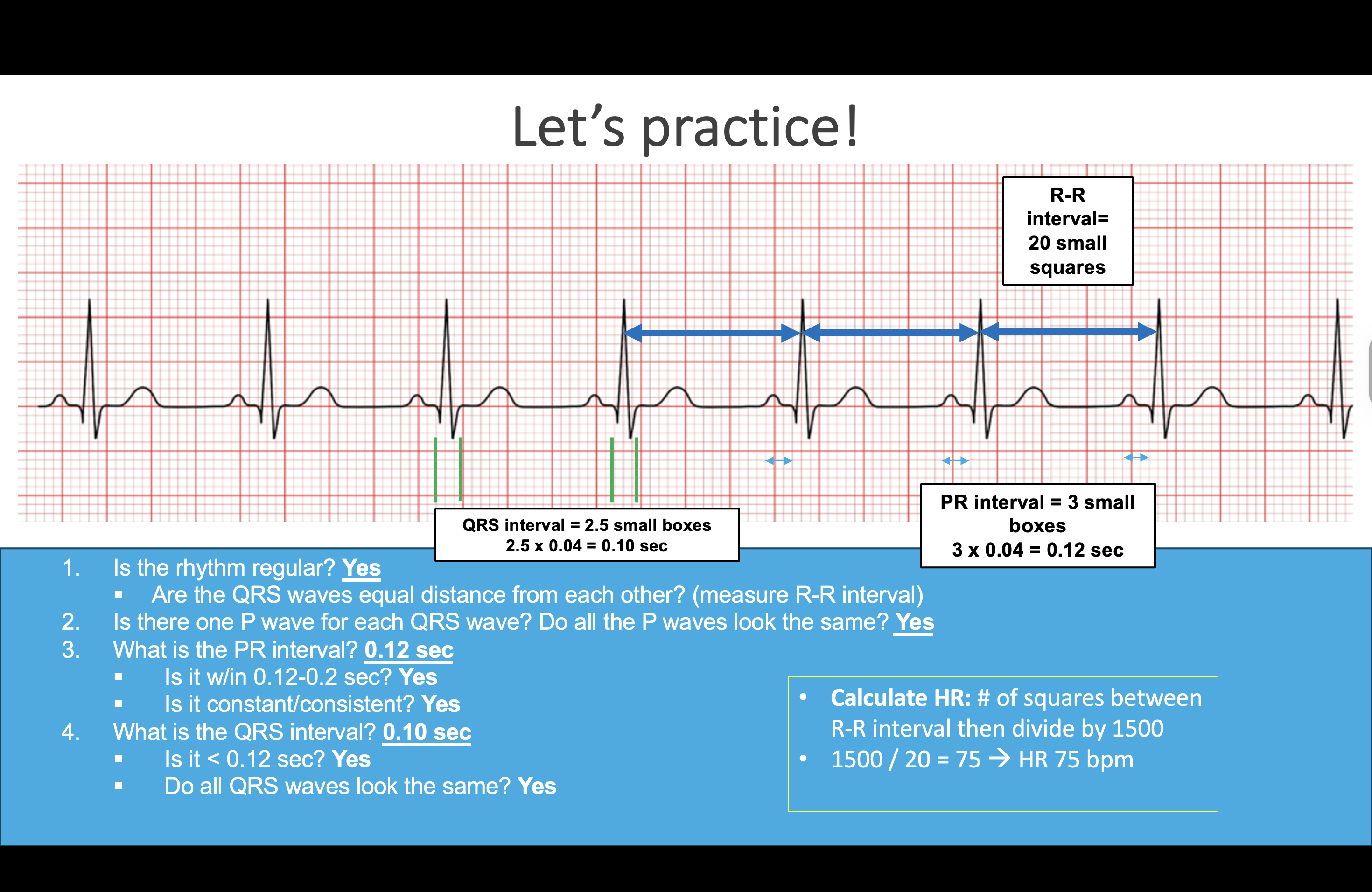
EKG Basics: How to determine a heart rate?
Most accurate: Count the number of small blocks between 2 R waves (tip of the QRS wave). Divide this into 1500.
Estimate: Count the number or R waves in a 6 second strip and multiply by 10. This is the best way for irregular rhythms.
Heart dysrhythmia
Abnormal rhythms of the heart’s electrical system that can affect its ability to effectively pump oxygenated blood throughout the body.
Some dysrhythmias are life threatening - others are not.
Result of disturbances in cardiac electrical impulse formation, conduction, or both. Causes include: CAD, electrolyte imbalances, impaired gas exchange, and drug toxicity (both legal and illicit drugs).
Dysrhythmias can occur in people of any age but occur most often in older adults.
Analyzing Heart Dysrhythmias
Steps to interpret ECG:
Is the rhythm regular?
Are the QRS waves equal distance from each other? (measure R-R interval)
Is there one P wave for each QRS wave? Do all the P waves look the same?
What is the PR interval? Is it w/in 0.12-0.2 sec? Is it constant?
What is the QRS interval? Is it < 0.12 sec? Do all QRS waves look the same?
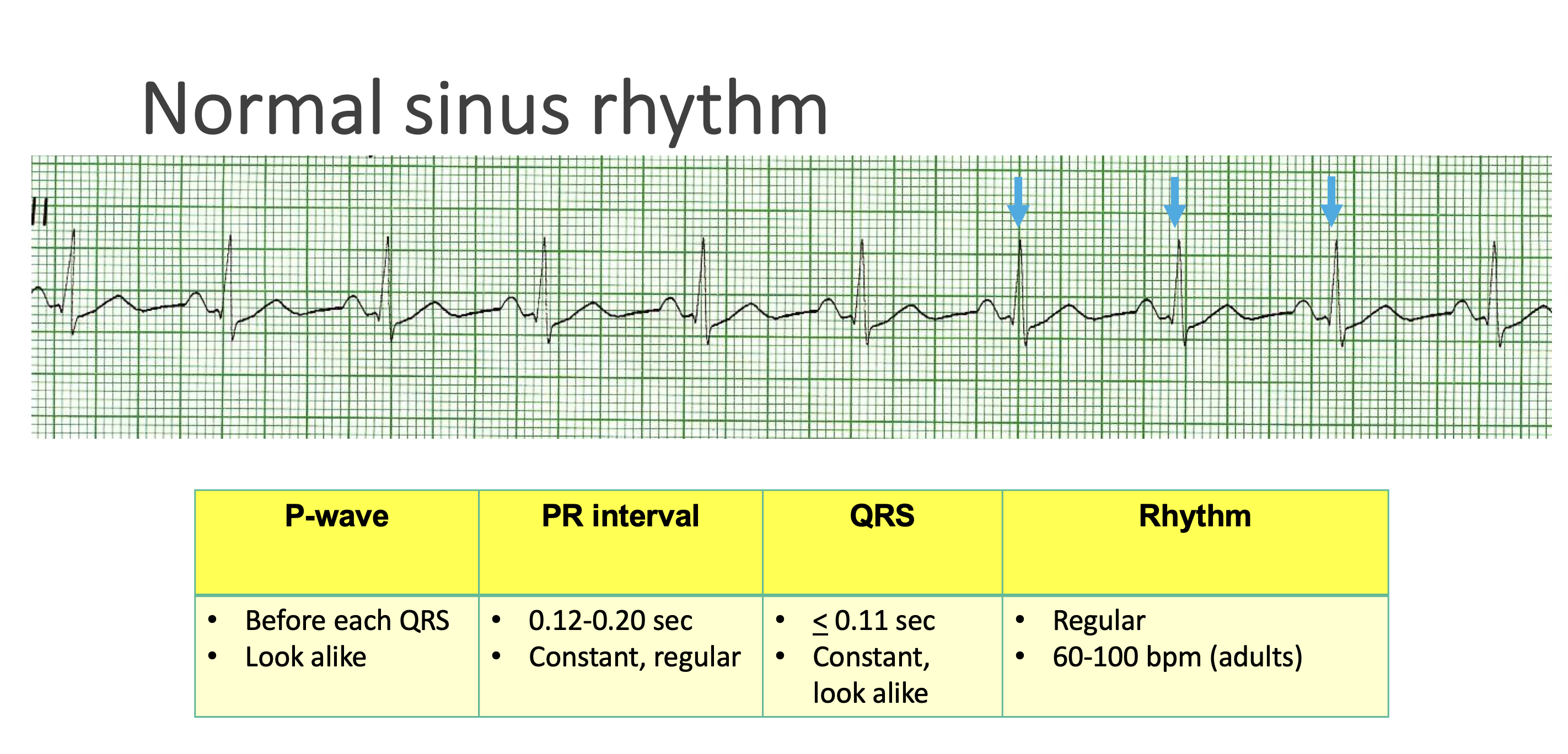
Normal Sinus Rhythm
One P for each QRS, all P waves look the same
Rate < 150
PR normal & constant
QRS =/<.11 and all look the same
Regular appearing rhythm - each wave/interval constant, and similar in appearance across the EKG paper
– P, QRS, T wave present
– Regular R-R interval
– Rate 60-100 bpm (adult)
– Normal/constant PR, QRS, and QT intervals
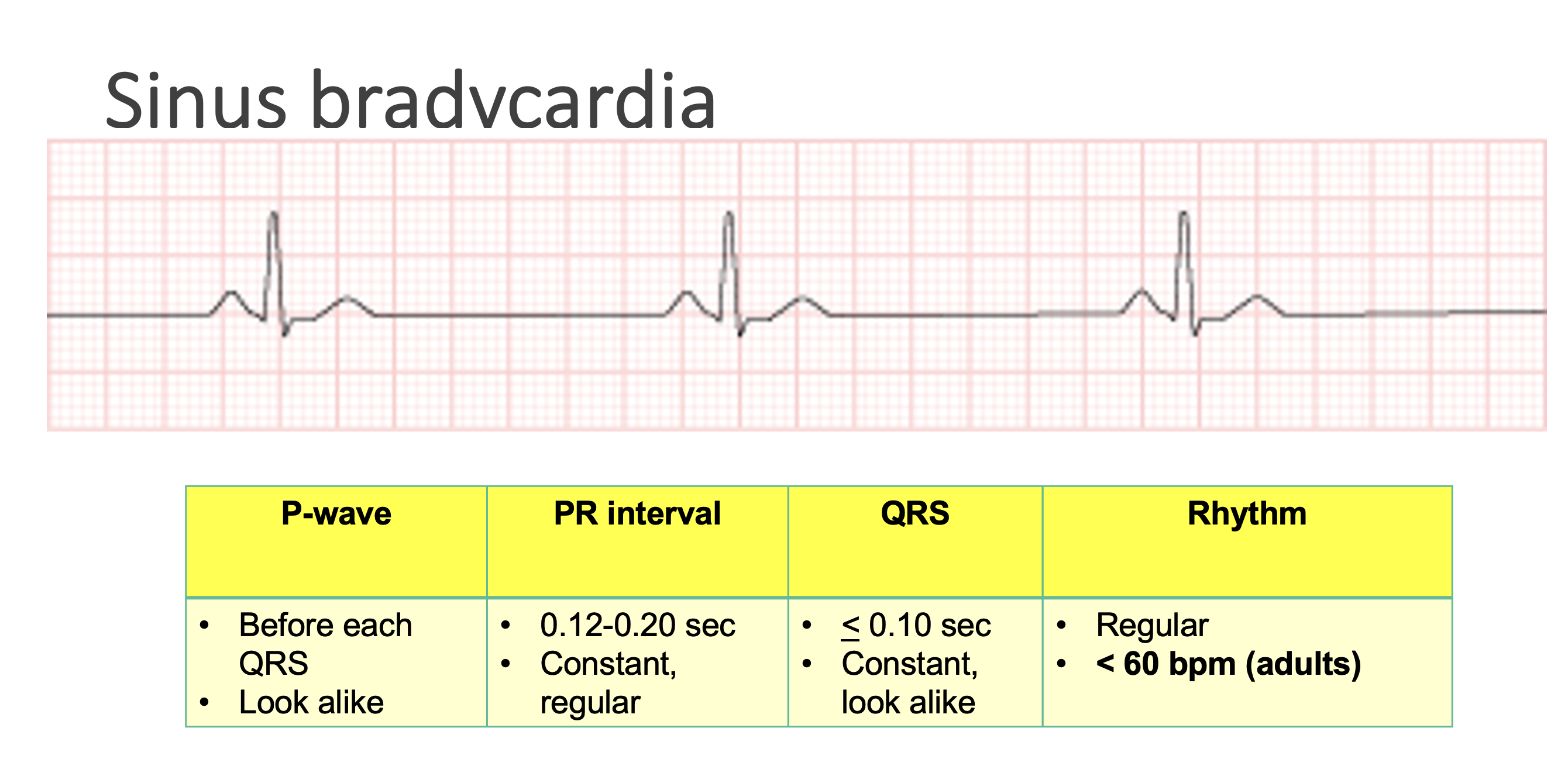
Sinus bradycardia
Regular appearing rhythm - each wave/interval constant, and similar in appearance across the EKG paper
– P, QRS, T wave present
– Regular R-R interval
– Rate < 60 bpm (adult)
Common Causes
Can be normal
Drug-Induced (B-blockers, calcium channel blockers, antiarrhythmics, narcotics, sedatives)
Enhanced vagal tone
Problem with pacemaker of the heart (SA node) → Sick Sinus Syndrome
Hypoxia
Can be normal for some patients (their baseline) → it’s ok as long as they’re asymptomatic
Increased vagal tone (increased activity of the vagus nerve) is generally associated with bradycardia → individuals who exercise a lot and do a lot of endurance training → enhances their cardiac vagal tone resulting in a low resting heart rate. Athletes like long distance runners can have resting heart rates as low as 40. Exercise strengthens the heart muscle, enabling it to pump a greater volume of blood with each heartbeat. More oxygen gets delivered to the muscles, so the heart needs to beat fewer times to pump oxygenated blood to rest of body.
Treatment:
Treatment if symptomatic
Atropine
Pacing (acute at bedside) and then placement of a pacemaker (permanent)
Treatment if asymptomatic
Maybe none!
Adjust medications
Atropine: Anticholinergic/blocks involuntary nervous system. Blocks the vagus nerve from acting on the heart, which will allow the SA node to increase its rate of electrical discharges → increased HR
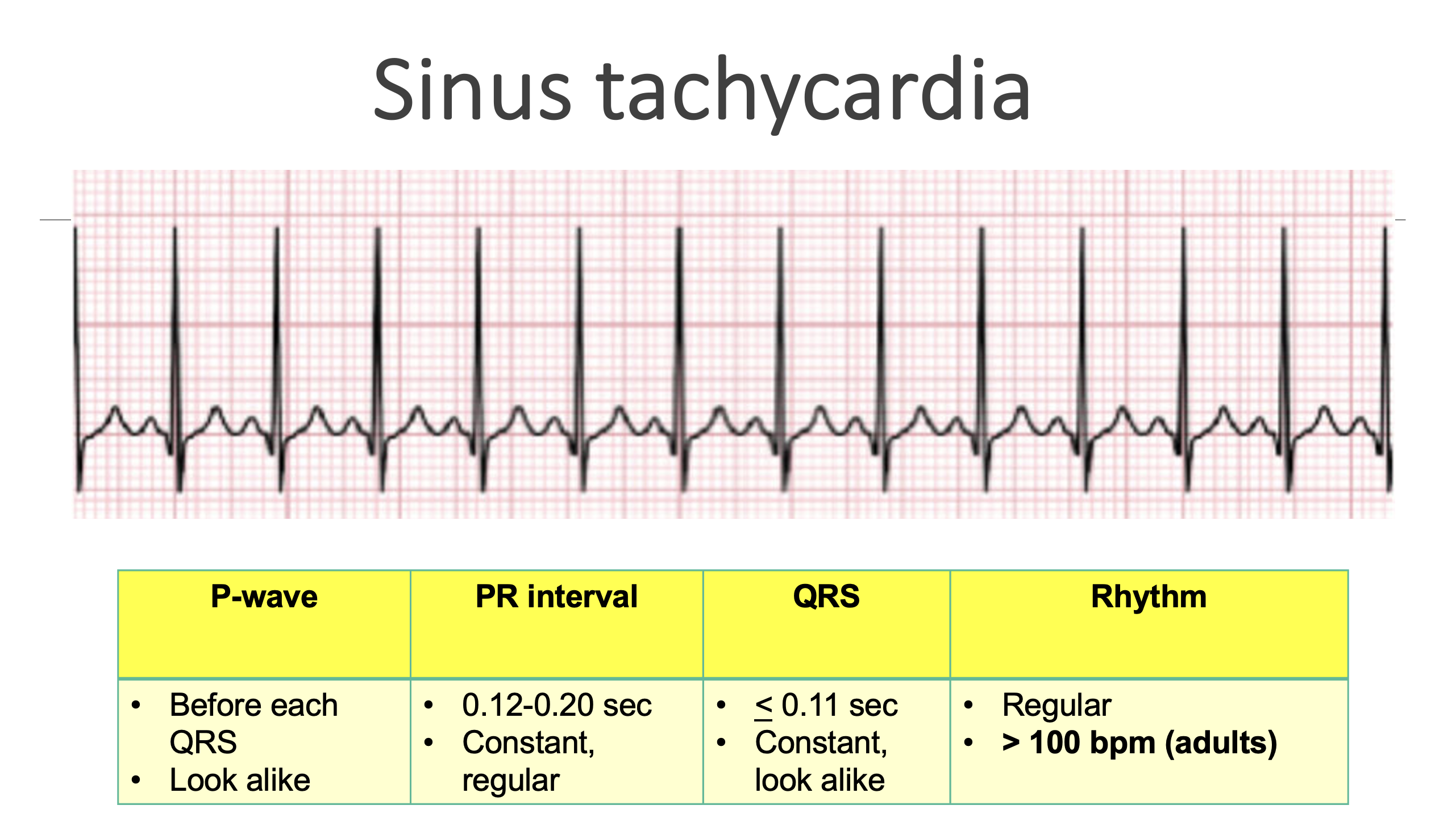
Sinus tachycardia
Regular appearing rhythm - each wave/interval constant, and similar in appearance across the EKG paper
– P, QRS, T wave present
– Regular R-R interval
– Rate > 100 bpm (adult)
SVT is HR >150 still regular rhythm
Common causes:
Pain
Fever
Anxiety
Hypovolemia
Hypoxemia
Activity
Medications
Caffeine
Nicotine
and many more!
Many factors can cause your pt to be tachycardic: Pain, fever, anxiety, deconditioning, activity, hypovolemia, hypoxemia. Medications (steroids, certain breathing txs – albuterol, OTC decongestants) caffeine, nicotine…many more!
Treatment:
Treat underlying cause
Fluid bolus, blood products, anxiolytics, pain relievers
Cardiac medications (beta blockers, calcium channel blockers)
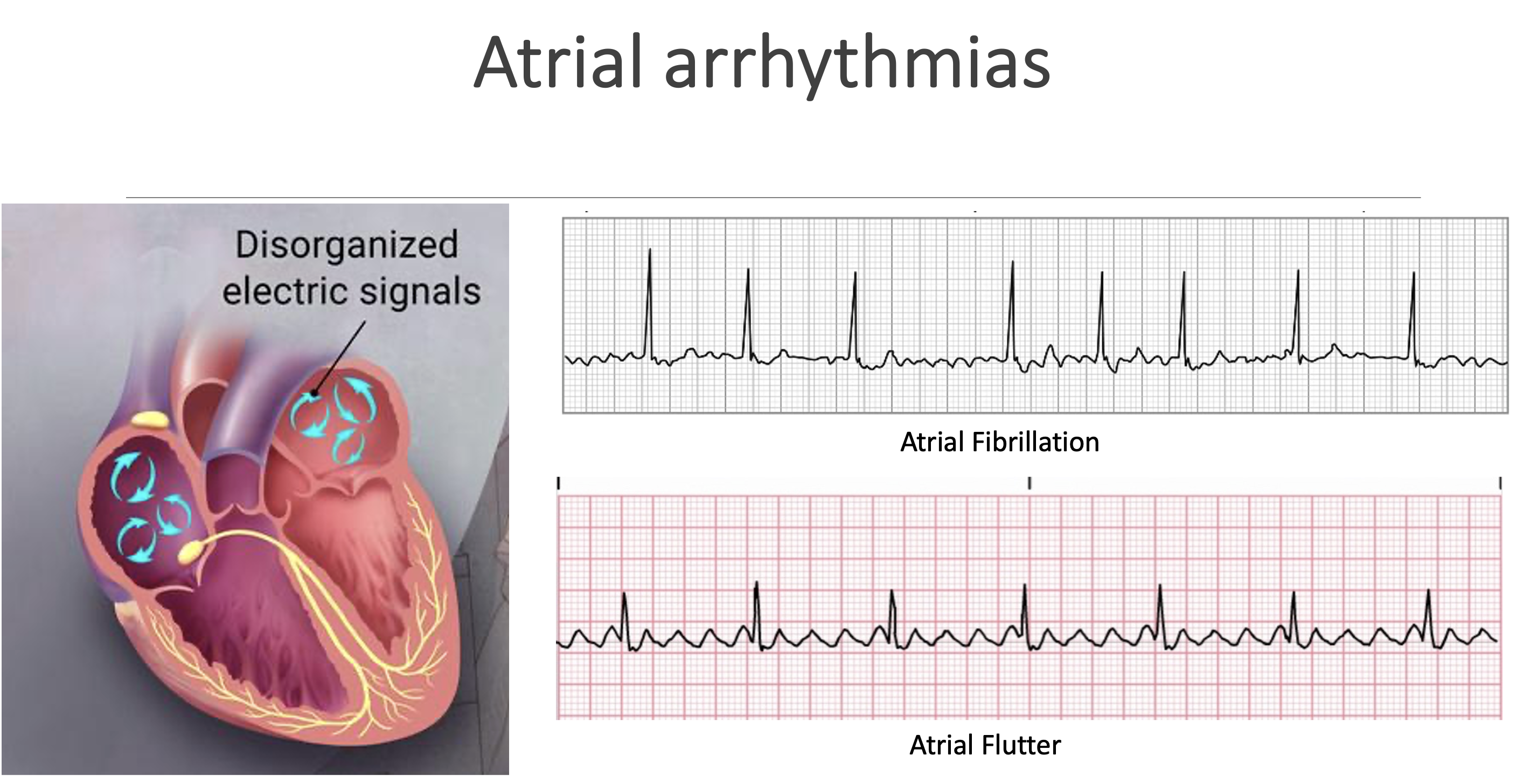
Atrial arrhythmias
Occur when the atria (aka: the upper chambers of the heart) are out of sync. So they’re not contracting and expanding in the order and timing that they should be → which causes several complications including decreased cardiac output and blood clots.
Afib (more irregular)
Aflutter (sawtooth pattern, multiple uniform p-waves)
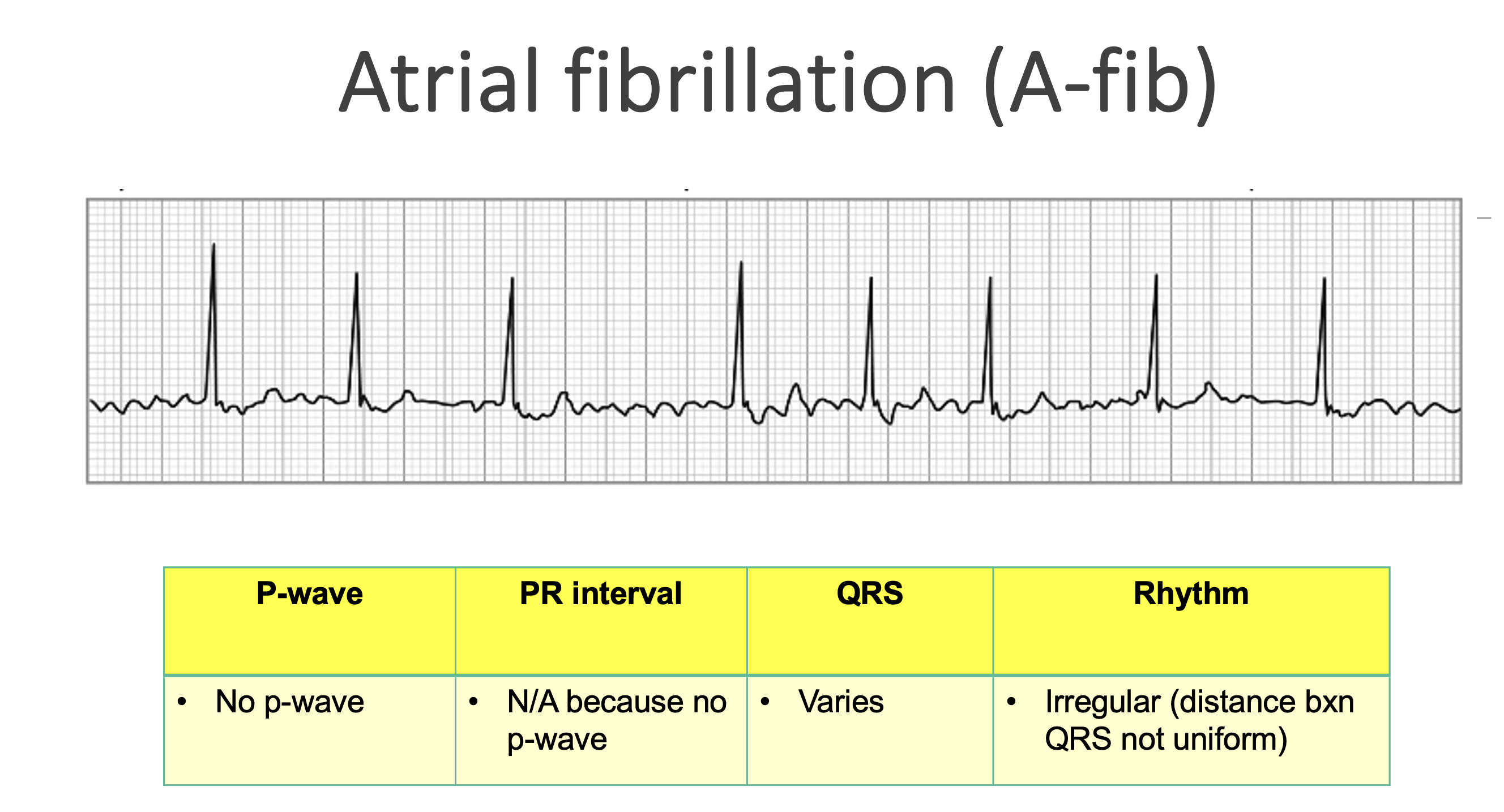
Atrial fibrillation (A-fib)
Common causes:
Mitral valve disease
OSA
HTN
Diabetes
Myocardial infarction
CKD
Heart failure
Obesity
Hyperthyroidism
CAD
Previous ischemic stroke
Excessive ETOH use
Most common adult dysrhythmia. SA node is no longer in control of the heart → impulses are coming from multiple foci in the atria. Afib is associated with atrial fibrosis and loss of muscle mass.
Signs/symptoms of afib: Fatigue, weakness, shortness of breath, dizziness, anxiety, syncope, palpitations, chest discomfort or pain, and hypotension.
Consequences of afib: The loss of coordinated atrial contractions in afib can lead to pooling of blood, resulting in clotting. The patient is at high risk for PE, DVT, embolic stroke. Afib can also lead to tachycardia induced cardiomyopathy if rate uncontrolled → leads to heart failure.
Nursing considerations:
Priority is to prevent embolus formation → administer blood thinner
Monitor patients carefully for signs of stroke and PE. Initiate RRT when suspected.
AMS, slurred speech, unequal movement in extremities, facial drooping
Coughing, including a cough that produces bloody mucus.
Dizziness
Heart palpitations, sensations of your heart racing or pounding.
Leg pain or swelling.
Sharp and sudden chest pain.
Shortness of breath that worsens with exertion
Restore regular blood flow through the atrium. Correcting the rhythm and controlling the rate of the rhythm restore blood flow, which helps prevent embolus formation and increases cardiac output. Meds to give include antiarrhythmics (amiodarone), calcium channel blockers (Diltiazem), Beta blockers (Metoprolol)
Treat with anticoagulation first 48 hours
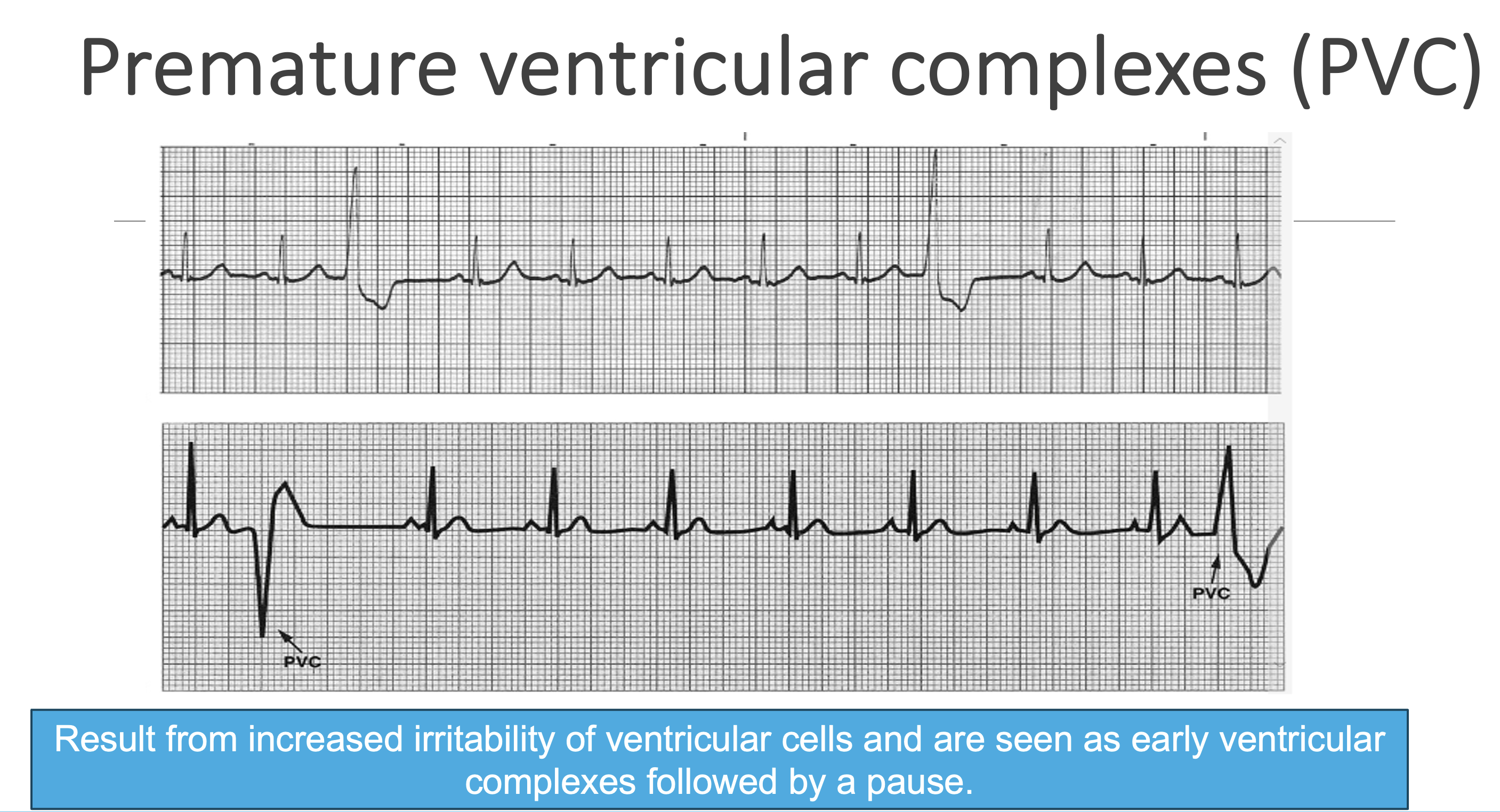
Premature ventricular complexes (PVC)
Result from increased irritability of ventricular cells and are seen as early ventricular complexes followed by a pause.
PVCs are common, and frequency increases with age.
They may be insignificant or may occur with problems such as MI, chronic heart failure, COPD, and anemia.
PVCs may also be present in patients with hypokalemia or hypomagnesemia. Sympathomimetic agents, anesthesia drugs, stress, nicotine, caffeine, alcohol, infection, or surgery can also cause PVCs, especially in older adults.
Sympathomimetic agents – Catecholamines (epi, norepi, dopamine); non-catecholamines (salmeterol, pseudoephedrine, phenylephrine)
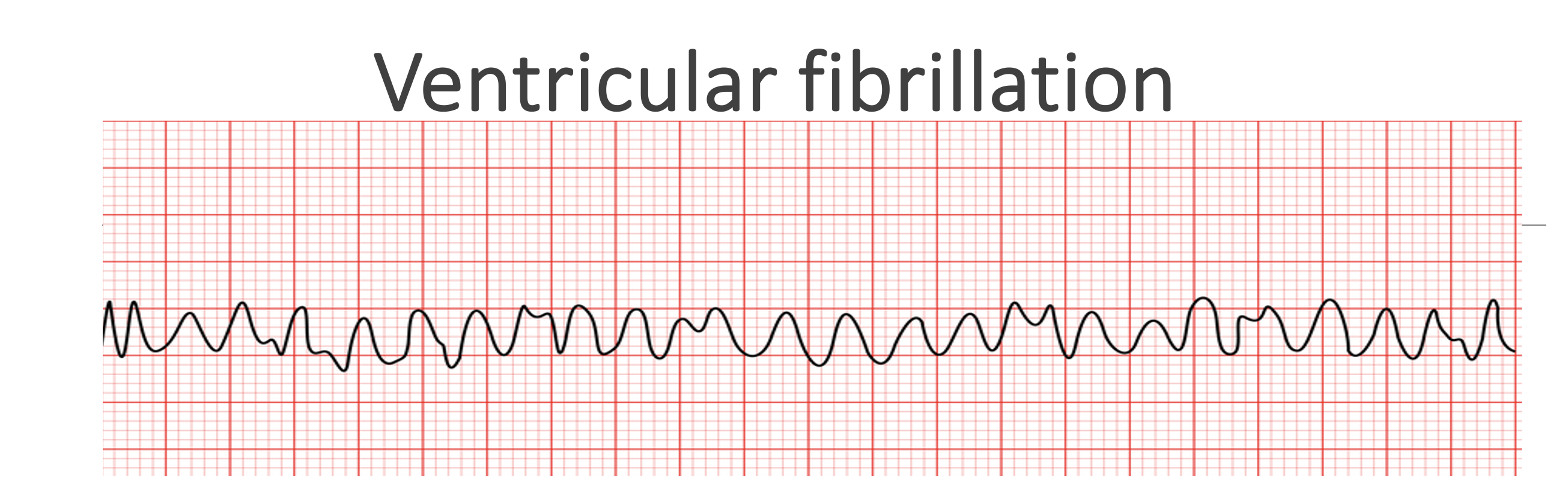
Ventricular fibrillation
Vfib is the result of electrical chaos in the ventricles and is life threatening! Impulses from many irritable foci fire in a totally disorganized manner, so ventricular contraction cannot occur.
The ventricles merely quiver, consuming a tremendous amount of oxygen. There is no cardiac output or pulse and therefore no cerebral, myocardial, or systemic perfusion. This rhythm is rapidly fatal if not successfully ended within 3 to 5 minutes.
Patients with MI are at great risk for Vfib. It may also occur in those with hypokalemia, hypomagnesemia, hemorrhage, drug therapy, rapid supraventricular tachycardia (SVT), or shock.
Surgery or trauma may also cause vfib
Signs and symptoms:
Patient becomes faint, immediately loses consciousness, and becomes pulseless and apneic (no breathing). There is no BP, and heart sounds are absent. Respiratory and metabolic acidosis develop. Seizures may occur.
Nursing Considerations:
Call a code blue / press code blue button on wall
Priority is to defibrillate the patient immediately.
If a defibrillator is not readily available, high-quality CPR must be initiated and continued until the defibrillator arrives.
Defib (shock) + CPR + epi
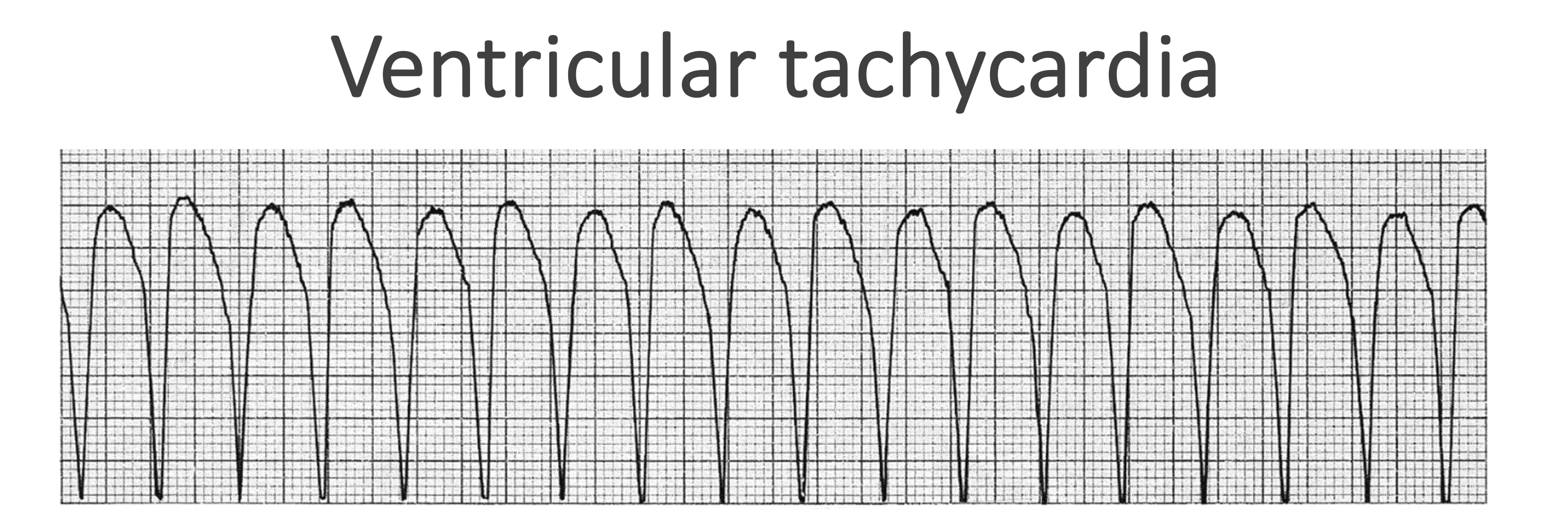
Ventricular tachycardia
V tach occurs with repetitive firing of an irritable ventricular ectopic focus, usually at a rate of 140 to 180 beats/min or more
Wide QRS complex, usually no p-waves present
It may be intermittent or sustained, lasting longer than 15 to 30 seconds.
May occur in patients with ischemic heart disease, MI, cardiomyopathy, hypokalemia, hypomagnesemia, valvular heart disease, heart failure, drug toxicity (e.g., steroids), or hypotension.
Patients who use cocaine or illicit inhalants are at a high risk
Nursing Considerations:
In some patients, vtach causes cardiac arrest → 1st check a pulse when pt is in vtach
Assess the patient’s ABCs and level of consciousness. For the stable patient with sustained vtach, administer oxygen and confirm the rhythm via a 12-lead EKG. Amiodarone or lidocaine may be prescribed.
No pulse: Defib (shock) + CPR + epi
With pulse: amiodarone OR synchronized cardioversion
Vtach is 4 or more PVCs in a row
In patients who go into cardiac arrest, vtach is commonly the initial rhythm before deterioration into vfib as the terminal rhythm!
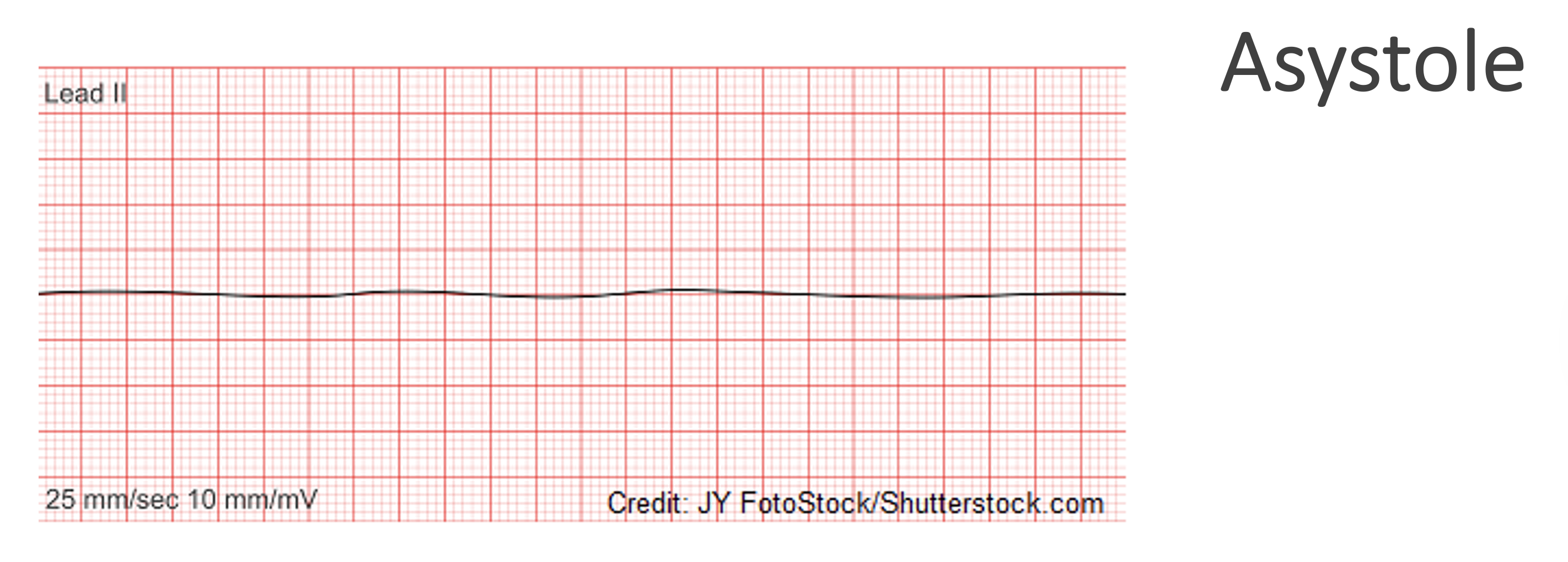
Asystole
Complete cardiac standstill – heart has stopped pumping
Medical emergency
Call a code / press code button
Start chest compressions
An asystolic heart cannot be defibrillated because the heart has no electrical activity to be reset or reorganized by the shock. A defibrillator works by delivering an electrical current to the heart to stop disorganized electrical activity, such as ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT), with the hope that the heart's natural pacemaker will then restart with a normal, synchronized rhythm.
Can’t defibrillate with asystole – shock stops the heart so normal rhythm can take over
Let’s practice!
Hypertension (HTN)
Hypertension, or high BP, is the most common health problem seen in primary care settings
Can cause stroke, MI, kidney failure, and death if not treated early and effectively.
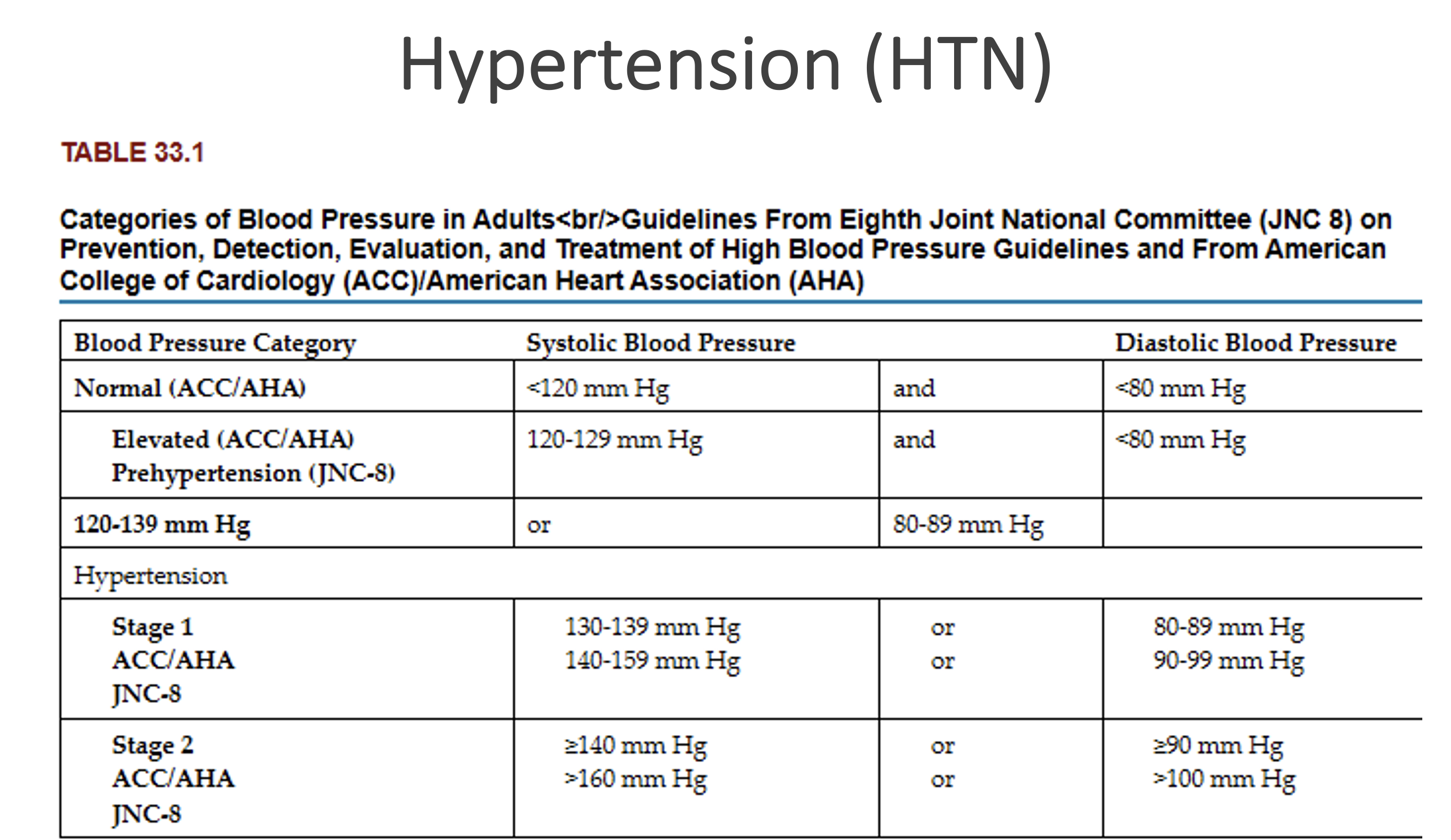
Current guidelines from the American College of Cardiology (ACC) and the American Heart Association (AHA) recommend a BP below 130/80 mm Hg in all people
Per 2017 guidelines from American College of Cardiology (ACC) and American Heart Association (AHA), desired BP is below 130/80.
Per 2023 guidelines from European Society of Hypertension (ESH), desired BP is 130/80 up to age 65, then relaxes the systolic level to 140 (if 130 not tolerated), and 140-150 starting at age 80.
Patients with a BP above these goals should be treated with drug therapy and lifestyle modifications
Hypertension (HTN)
Four control systems play a major role in maintaining blood pressure:
Baroreceptor system - Primarily in the carotid sinus, aortic arch, and left ventricle. They monitor the level of arterial pressure and counteract a rise in arterial pressure through vagally mediated cardiac slowing and vasodilation with decreased sympathetic tone → decrease BP
Regulation of body fluid volume - If there is an excess of sodium and/or water in a person’s body, the BP rises through complex physiologic mechanisms that change the venous return to the heart, producing a rise in cardiac output. If the kidneys are functioning adequately, a rise in systemic arterial pressure produces diuresis and a fall in BP.
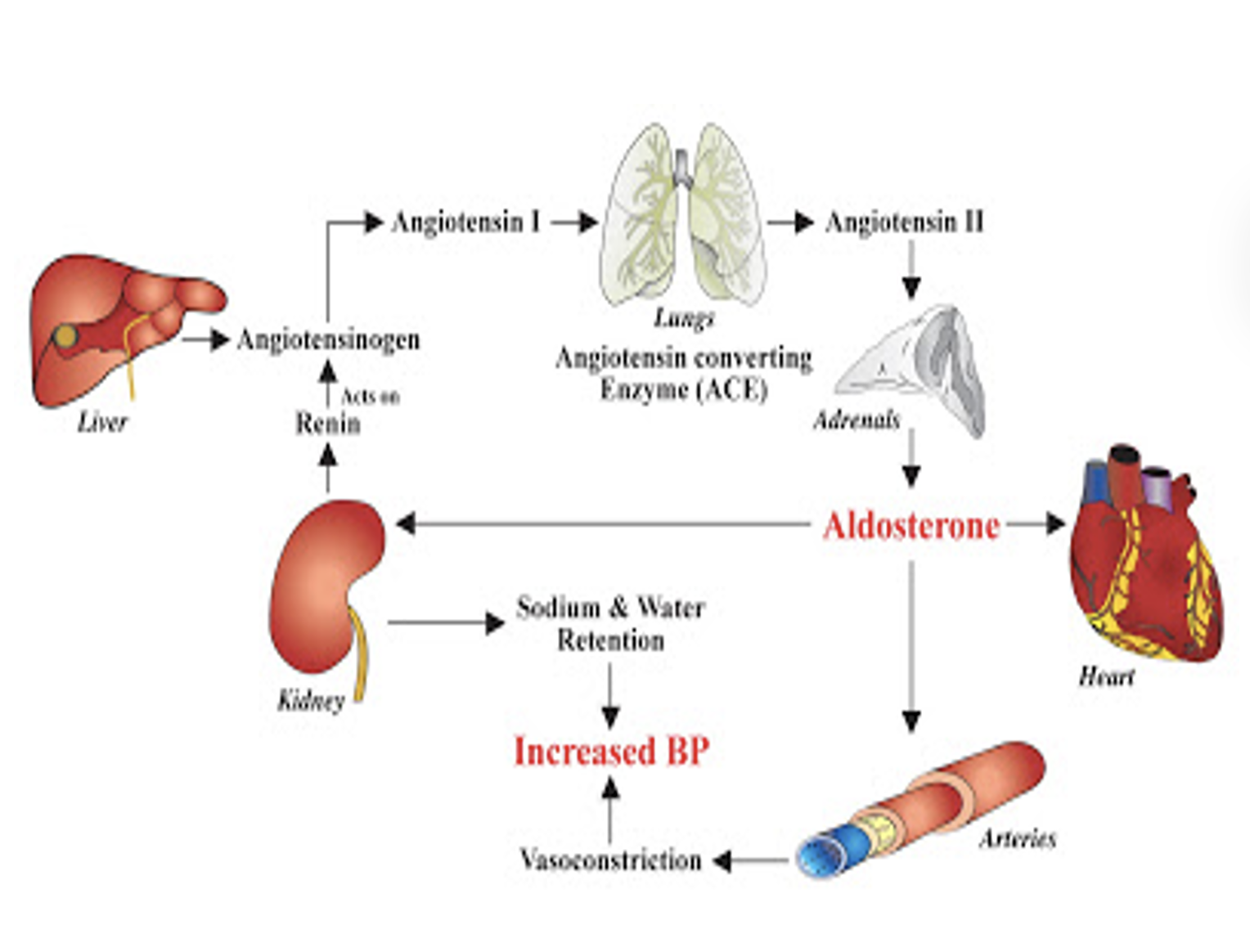
The renin-angiotensin-aldosterone system - The kidney produces renin, an enzyme that acts on angiotensinogen to split off angiotensin I, which is converted by an enzyme in the lung to form angiotensin II. Angiotensin II has strong vasoconstrictor action on blood vessels and is the controlling mechanism for aldosterone release. Aldosterone then works on the collecting tubules in the kidneys to reabsorb sodium. Sodium retention inhibits fluid loss, thus increasing blood volume and subsequent BP.
RAAS system also helps regulate our body’s BP. Renin activates angiotensinogen, which becomes angiotensin I, further activated by angiotensin-converting enzyme (ACE) to produce angiotensin II, a strong vasoconstrictor, which also causes adrenals to secrete aldosterone, thus increasing sodium and water retention. All this leads to increased BP
Vascular autoregulation - Keeps perfusion of tissues in the body relatively constant. Appears to be important in causing hypertension. However, the exact mechanism of how this system works is poorly understood.
Hypertension (HTN)
Blood pressure is categorized into four levels:
Normal
Elevated (or prehypertension)
Stage 1 HTN
Stage 2 HTN
HTN , categorized as stage 1 or stage 2, can be classified as either essential (aka: primary) or secondary HTN
Hypertension (HTN)
Primary (Essential) HTN:
Most common type. Not caused by an existing health problem.
Several risk factors can increase a person’s likelihood.
Continuous BP elevation in patients with primary HTN results in damage to vital organs by causing medial hyperplasia (thickening) of the arterioles.
As the blood vessels thicken and perfusion decreases, body organs are damaged.
These changes can result in MIs, strokes, peripheral vascular disease (PVD), or kidney failure. Dementia?
Secondary HTN
Specific disease states and drugs can increase a person’s susceptibility to hypertension.
Elevated BP due to a specific disease or medication.
Hypertensive crisis (aka malignant hypertension)
Severe type of HTN (> 180/120) that rapidly progresses and is a medical emergency.
Sx/Sx: morning headaches, blurred vision, anxiety, nosebleeds, and dyspnea.
These patients may experience kidney failure, left ventricular heart failure, or stroke.
Hypertension (HTN) - Etiology
Primary
Family history of hypertension
Black race
Hyperlipidemia
Smoking
Older than 60 years or postmenopausal
Excessive sodium intake
Overweight/obesity
Physical inactivity
Excessive alcohol intake
Excessive and continuous stress
Secondary
Kidney disease
Primary aldosteronism
Pheochromocytoma
Cushing syndrome
Coarctation of the aorta
Brain tumors
Pregnancy
Obstructive sleep apnea
Illicit drug use
Drugs:
Estrogen (e.g., oral contraceptives)
Glucocorticoids
Mineralocorticoids
Sympathomimetics
Hypertension (HTN)
Physical Assessment/Signs and Symptoms:
When a diagnosis of HTN is made, most people have no symptoms. However, some patients experience headaches, facial flushing (redness), dizziness, or fainting.
If you notice your pt develops an acute increase in their BP that’s far from their baseline → Reassess/get a repeat BP reading. Try to obtain BP readings in each arm (if no contraindications).
Be sure to take an accurate blood pressure by using an appropriate-size cuff.
This is also the time when you would want to take a manual BP to make sure it is accurate
Management of Hypertension (HTN)
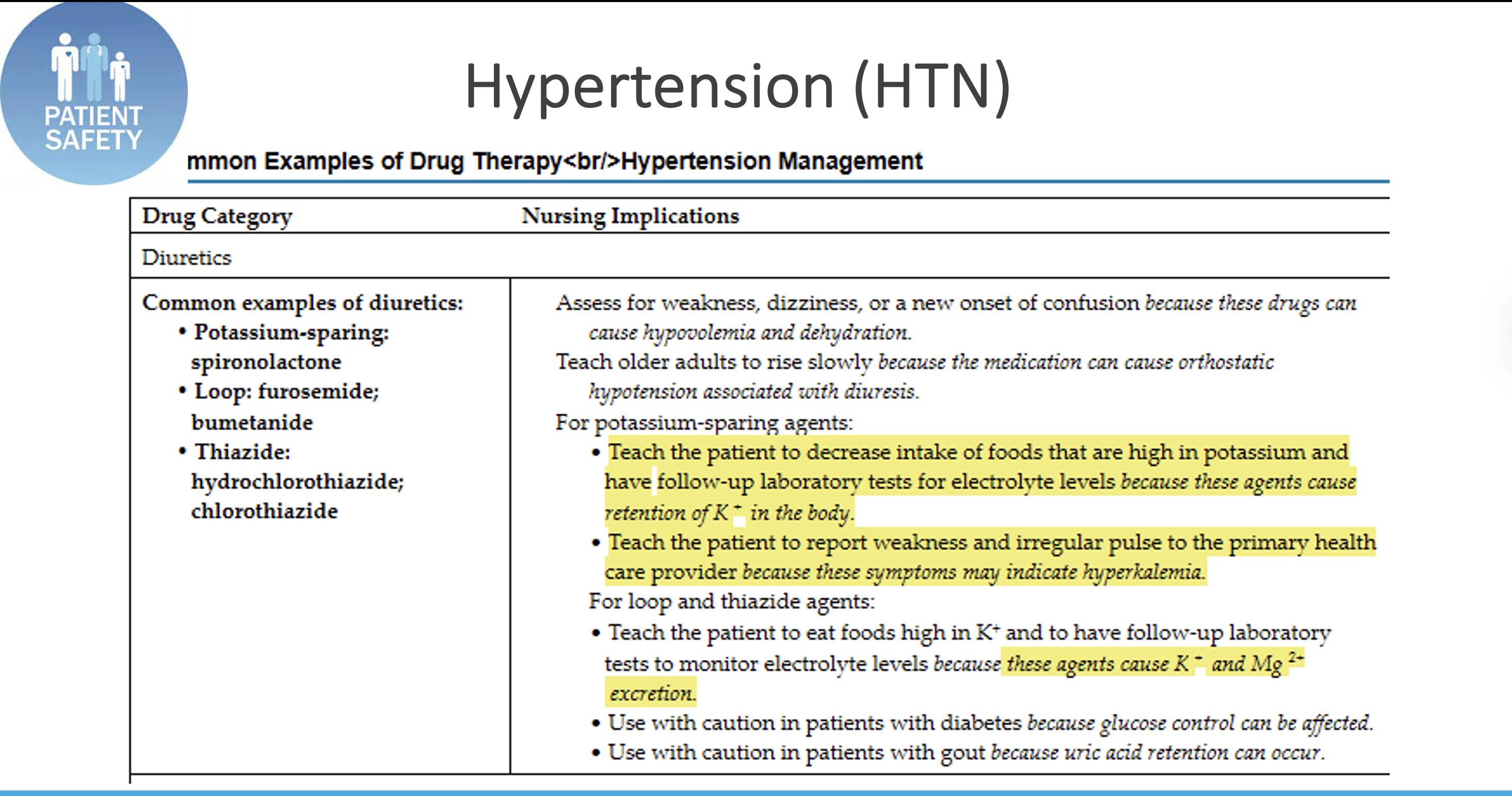
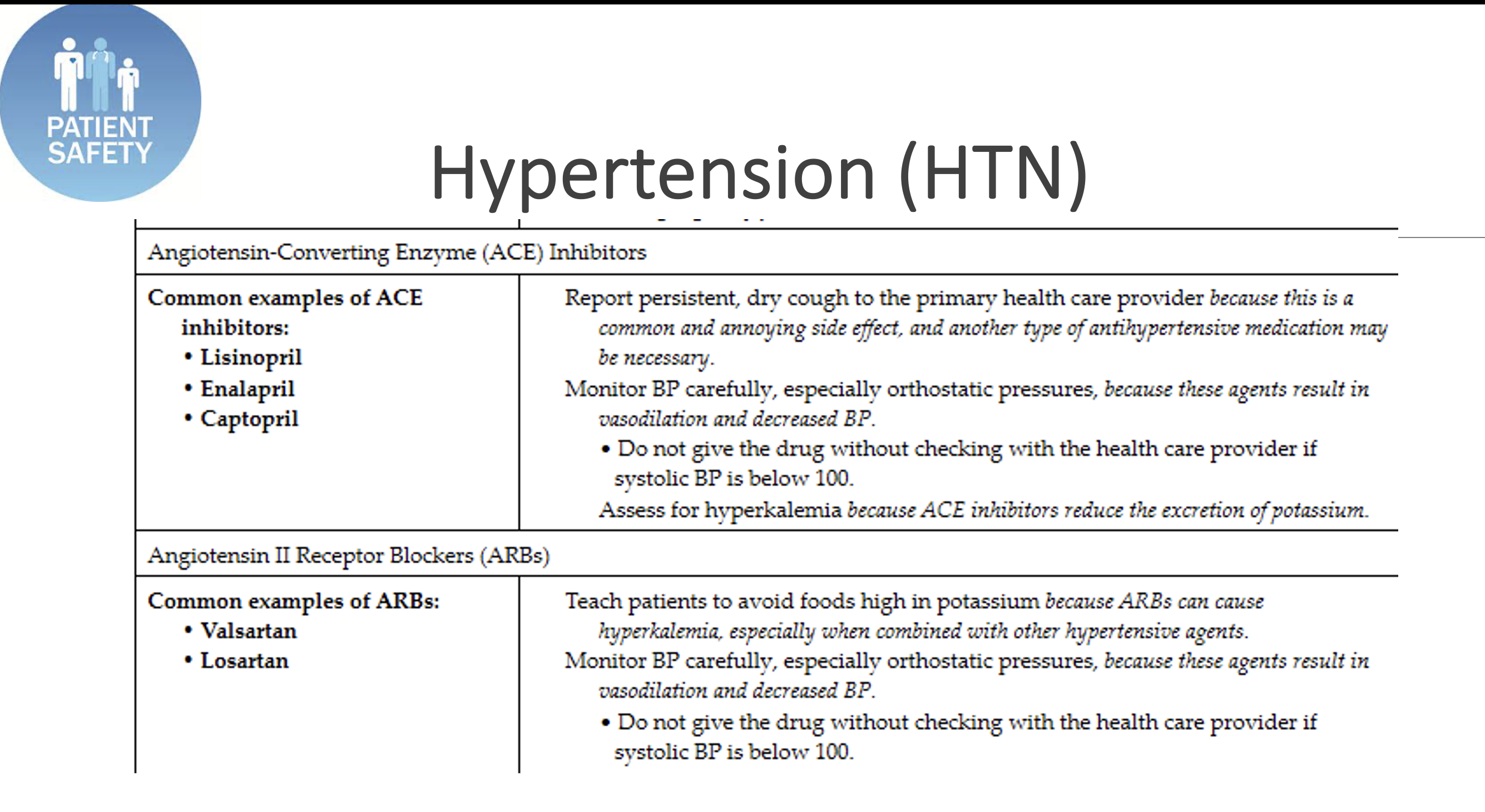
Medications: Current guidelines recommend use of one or more of these five classes of drugs:
Potassium-sparing, loop, or thiazide diuretics,
Beta blockers
Calcium channel blockers (CCBs),
Angiotensin-converting enzyme inhibitors (ACE Inhibitors),
Angiotensin II receptor blockers (ARBs).
In general, it is not recommended to use ARBs and ACEIs together. BB no longer first line treatment
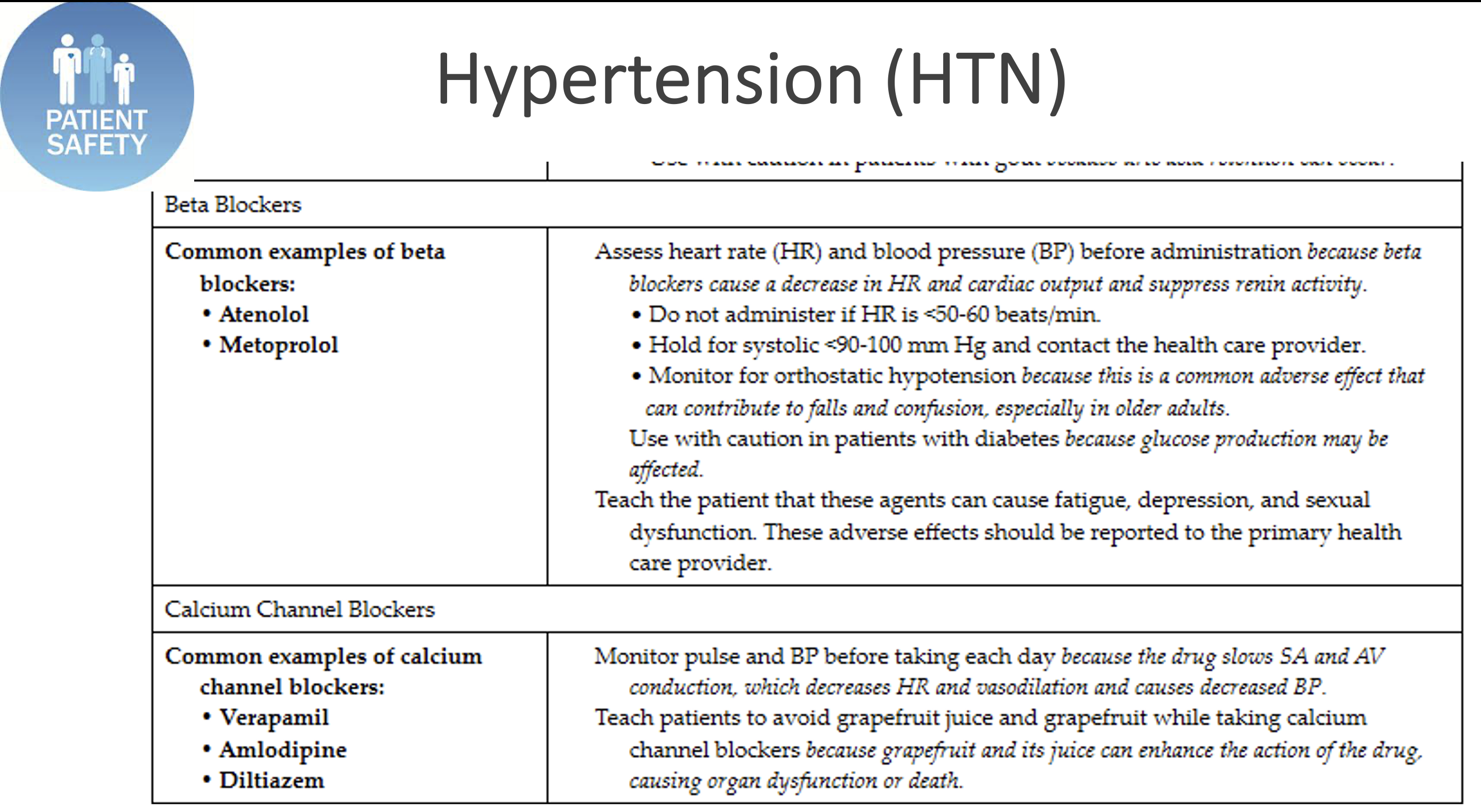
Hypertension (HTN) Meds
Atherosclerosis
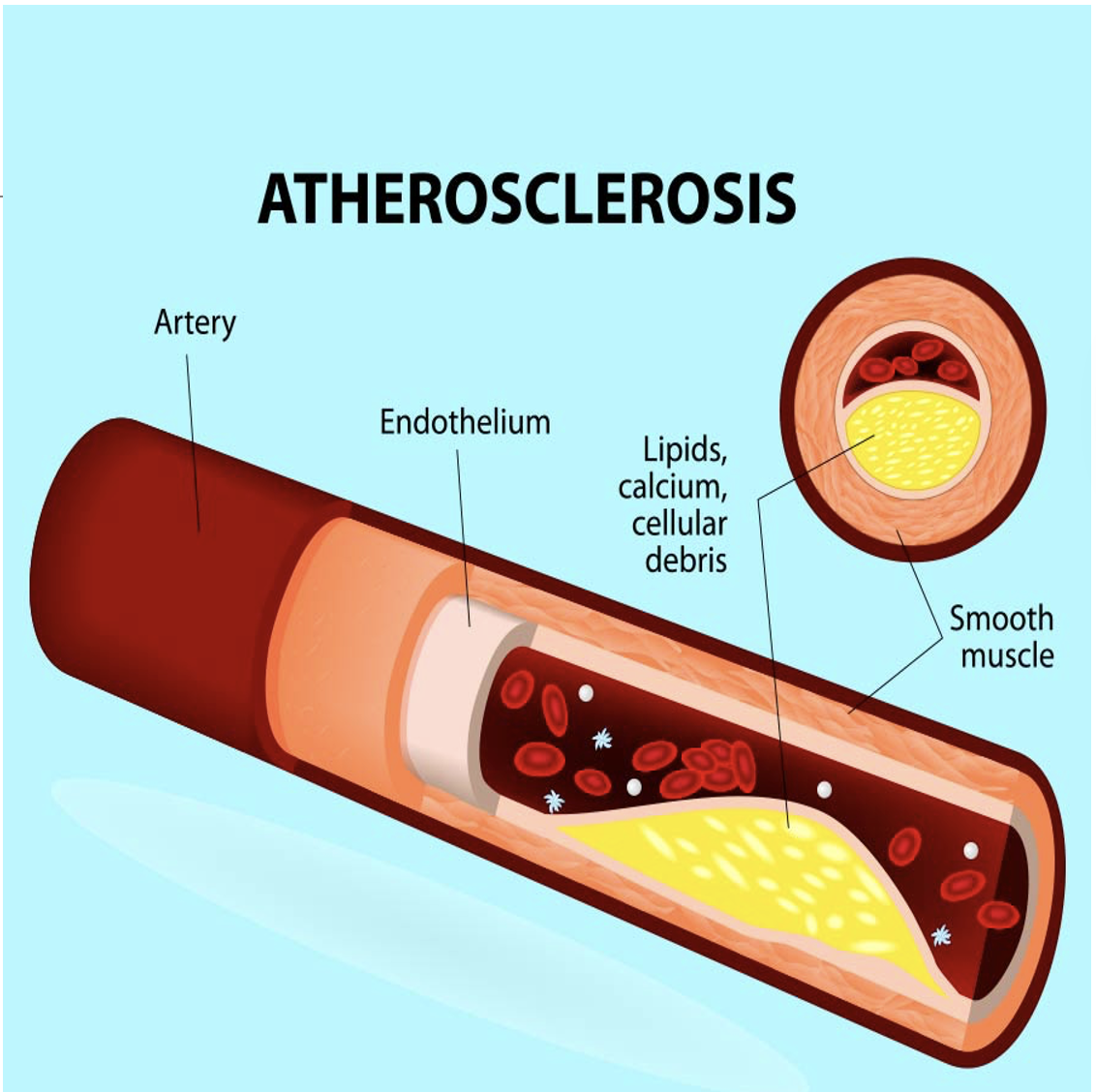
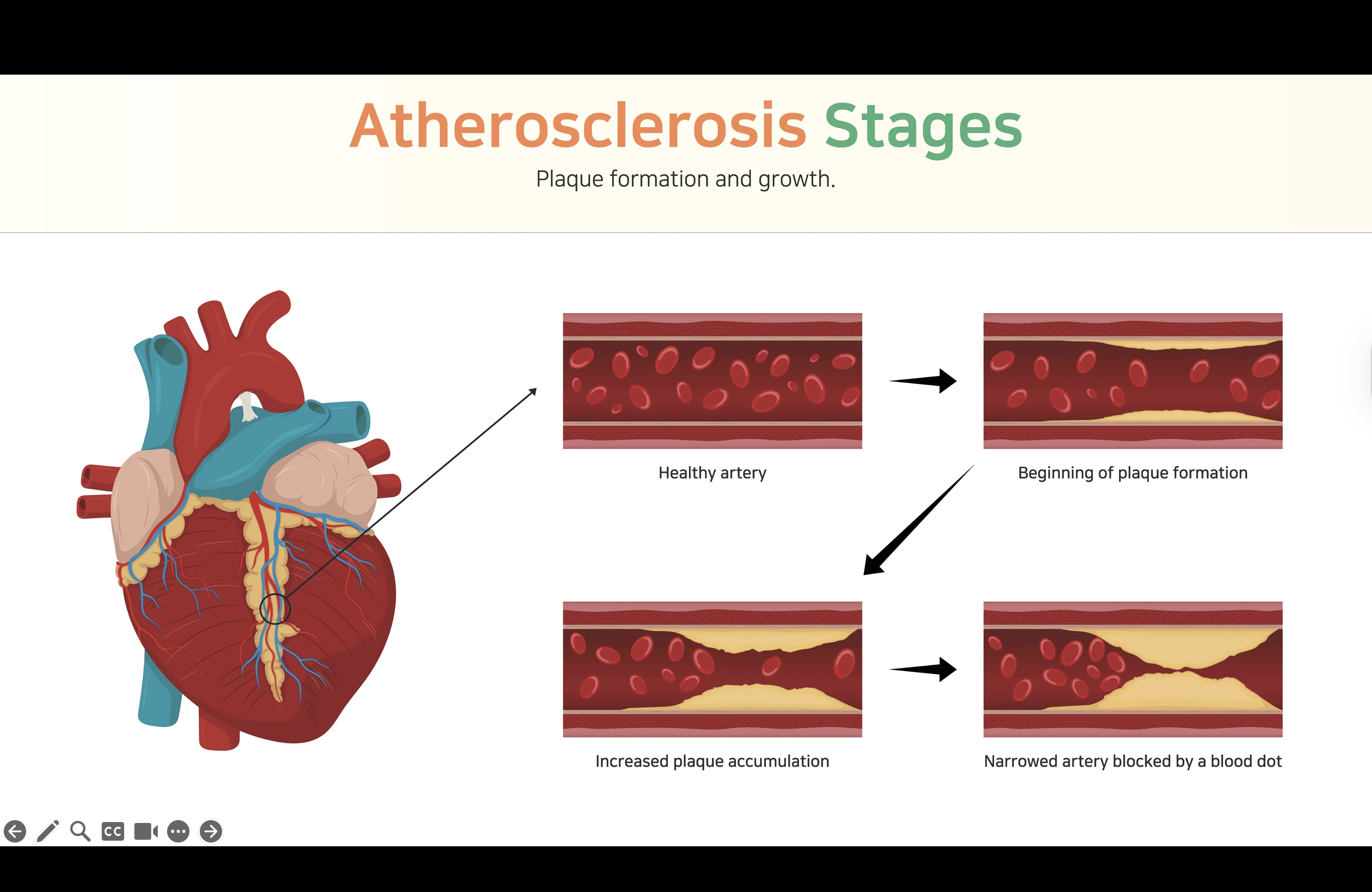
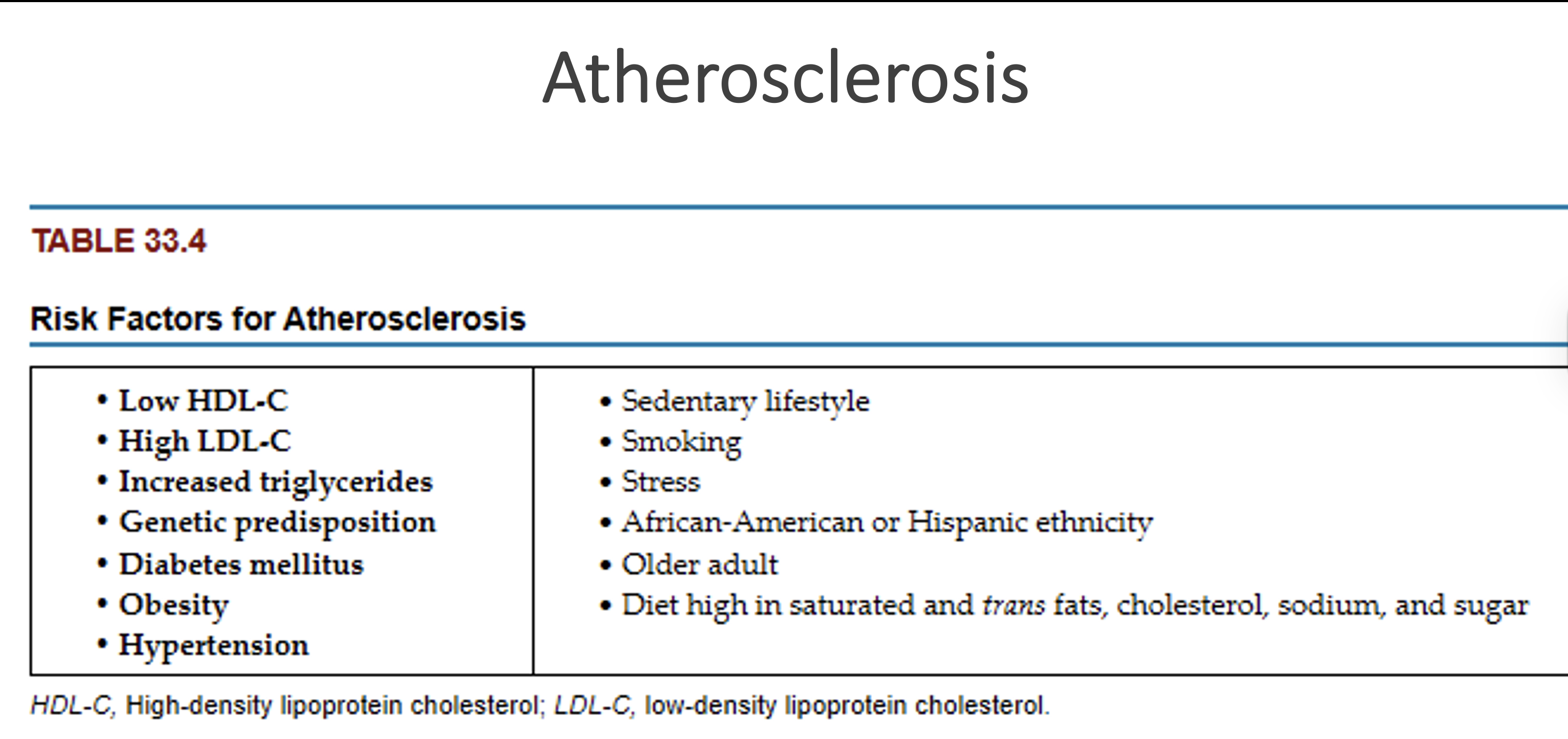
Arteriosclerosis is a thickening, or hardening, of the arterial wall that is often associated with aging → Atherosclerosis, a type of arteriosclerosis
Atherosclerosis involves the formation of plaque within the arterial wall and is the leading risk factor for CVD.
Usually affects the larger arteries, such as coronary artery beds; aorta; carotid and vertebral arteries; renal, iliac, and femoral arteries
Atherosclerosis
Atherosclerosis plaque rupture
Stable plaque rupture - thrombosis (blood clot) and constriction obstruct the vessel lumen, causing inadequate perfusion and oxygenation to distal tissues.
Unstable plaque rupture - causes more severe damage. After the rupture occurs, the exposed underlying tissue causes platelet adhesion and rapid thrombus formation. The thrombus may suddenly block a blood vessel, resulting in ischemia and infarction (ex: MI)
Atherosclerosis
Assessing patients with atherosclerosis
Palpate pulses bilaterally and note any differences. Palpate each carotid artery separately to prevent blocking blood flow to the brain!
Feel for temperature differences in the lower extremities and check cap filling. Prolonged capillary filling generally indicates poor circulation. With severe atherosclerotic disease, the extremity may be cool or cold with a diminished or absent pulse.
These patients may have developed a bruit in the larger arteries. A bruit is a turbulent, swishing sound, which can be soft or loud in pitch. It is heard due to blood trying to pass through a narrowed artery. A bruit is considered abnormal.
Assess cholesterol and triglycerides.
Loss of pulse may indicate that the individual has developed an arterial occlusion. This needs further assessment and notification of the provider.
Atherosclerosis: Taking Action
Individuals at low risk should have total serum cholesterol levels evaluated every 4-6 years
Those with multiple risk factors and older than 40 years of age, should have evaluation more frequently
Focus is on targeting modifiable risk factors
Nutrition (weight management)
Activity
Smoking
Atherosclerosis: Drug Therapy
When individuals do not respond to lifestyle changes, drug therapy should be initiated
HMG-CoA reductase inhibitors (statins)
lovastatin, atorvastatin, simvastatin, etc.
HMG-CoA, 3-hydroxy-3-methylglutaryl coenzyme A – lowers LDL-C and triglycerides
Ezetimibe decreases the absorption of cholesterol in the small intestine
Combination drugs
Vytorin (ezetimibe + simvastatin), Caduet (amlodipine + atorvastatin)
PCSK9 inhibitors for those with familial hypercholesterolemia
monoclonal antibodies like alirocumab and evolocumab
PCSK9 is a protease produced in the liver that increases LDL levels
Venous thromboembolism (VTE)
VTE is a vascular complication that involves both thrombus and embolus complications.
A thrombus is a blood clot believed to result from an endothelial injury, venous stasis, or hypercoagulability. When a thrombus develops, immunity is altered, causing inflammation to occur around the clot, thickening of the vein wall, and possible embolization (the formation of an embolus). An embolus is a blood clot, air bubble, piece of fatty deposit which has been carried in the bloodstream and becomes lodged in a blood vessel
Pulmonary embolism (PE) is the most common type of embolus
Phlebothrombosis is a thrombus in the vein without inflammation.
Thrombophlebitis refers to a thrombus that is associated with inflammation.
Deep vein thrombosis (DVT), is the most common type of thrombophlebitis. Can lead to a PE. With PE, a dislodged blood clot travels to the pulmonary artery—a medical emergency!
DVT develops most often in the legs but can also occur in the upper arms because of increased use of central venous devices.

Deep vein thrombosis (DVT)
Patients with a DVT may have symptoms or may be asymptomatic.
The classic signs and symptoms are calf or groin tenderness and pain and sudden onset of unilateral swelling of the leg.
Nursing considerations:
Teach the patient to elevate his or her legs when in the bed and chair.
Instruct patients with active and resolving DVT to wear knee- or thigh-high sequential or graduated compression stockings for an extended period.
Some health care providers prescribe intermittent or continuous warm, moist soaks to the affected area to promote circulation and reduce pain.
To prevent the thrombus from dislodging and becoming an embolus, do not massage the affected extremity.
Monitor all patients for signs and symptoms of PE, which include shortness of breath, chest pain, and acute confusion (in older adults)
Coronary Artery Disease
Coronary artery disease (CAD) is a broad term that includes chronic stable angina and acute coronary syndrome (ACS).
It affects the arteries that provide blood, oxygen, and nutrients to the myocardium. When blood flow through the coronary arteries is partially or completely blocked, ischemia and infarction of the myocardium may result.
Ischemia occurs when insufficient oxygen is supplied to meet the requirements of the myocardium.
Infarction (necrosis, or cell death) occurs when severe ischemia is prolonged and decreased perfusion causes irreversible damage to tissue.
Coronary artery disease
To prevent CAD, keep lipid levels within normal range:
Total cholesterol less than 200 mg/dL
Triglycerides between 40 and 160 mg/dL for men & between 35 and 135 mg/dL for women
HDL more than 45 mg/dL for men; more than 55 mg/dL for women (“good” cholesterol)
LDL less than 130 mg/dL
Elevated LDL levels are positively correlated with CAD, whereas elevated HDL levels are negatively correlated and appear to be protective for heart disease.
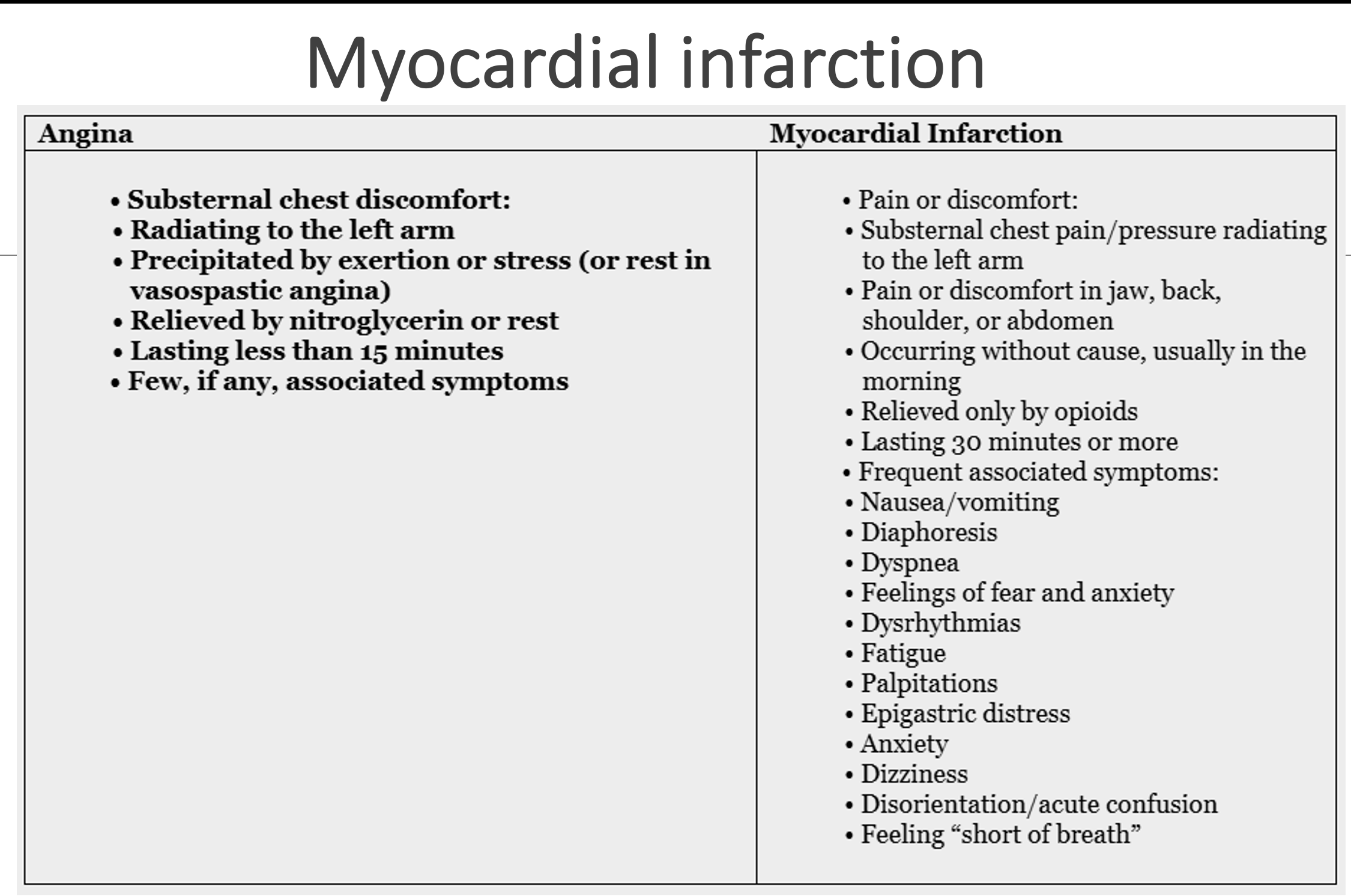
Angina pectoris
Angina pectoris: chest pain caused by a temporary imbalance between the coronary arteries’ ability to supply oxygen and the cardiac muscle’s demand for oxygen. The ischemia that occurs with angina is limited in duration and does not cause permanent damage of myocardial tissue.
Two types: stable angina and unstable angina.
Stable angina: chest discomfort that occurs with moderate-to-prolonged exertion in a pattern that is familiar to the patient. Results in slight limitation of activity; associated with a fixed atherosclerotic plaque; usually relieved by nitroglycerin (NTG) or rest.
Angina pectoris (ACS)
Acute coronary syndrome (ACS) is used to describe patients who have either unstable angina or an acute MI.
In ACS, it is believed that the atherosclerotic plaque in the coronary artery ruptures, resulting in platelet aggregation (“clumping”), thrombus (clot) formation, and vasoconstriction.
Once the artery reaches 50% occlusion, blood flow is impaired, creating myocardial ischemia when myocardial demand is increased.
Angina pectoris - Unstable angina
Unstable angina (UA): chest pain or discomfort that occurs at rest or with exertion and causes severe activity limitation.
An increase in the number of attacks and in the intensity of the pressure
Pressure may last longer than 15 minutes or may be poorly relieved by rest or NTG
Myocardial infarction (MI)
Most serious acute coronary syndrome is an MI.
Undiagnosed or untreated angina can lead to → MI
Occurs when myocardial tissue is abruptly/severely deprived of oxygen. When blood flow is quickly reduced by 80% to 90%, ischemia develops. Ischemia can lead to injury and necrosis of myocardial tissue if blood flow is not restored.
Two types of MI: non–ST-segment elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI).
Myocardial infarction
NSTEMI causes include - coronary vasospasm, sluggish blood flow due to narrowing of the coronary artery, and spontaneous dissection
STEMI is from a rupture of an atherosclerotic plaque leading to platelet aggregation and thrombus formation at the site. The thrombus causes 100% occlusion to the coronary artery → medical emergency and requires immediate revascularization of the blocked coronary artery
Spontaneous dissection is when there is a tear in an artery wall → and it causes blood to build up in that area → which leads to a reduction or blockage of blood flow to your heart, which causes damage to your heart muscle and affects your heart rhythm.
Myocardial infarction - interventions
Priority for MI patients is to restore perfusion to their heart.
Drug therapy:
Aspirin inhibits platelet aggregation and vasoconstriction . We ask pt’s to chew the aspirin so it can dissolve/work faster.
P2Y12 platelet inhibitors such as clopidogrel (Plavix) or ticagrelor (Brilinta)
Glycoprotein (GP) IIb/IIIa inhibitors to prevent fibrinogen from attaching to activated platelets
Anticoagulants
Beta blockers decrease the size of the infarct, the occurrence of ventricular dysrhythmias, and mortality rates in patients with MI.
Priority for MI patients is to restore perfusion to their heart → and time is of the essence for these pts to prevent permanent heart damage and mortality. For a STEMI pt, we want to restore perfusion w/in 60-90 mins, and 4-6 hours for NSTEMIs.
P2Y12 platelet inhibitors - they make the platelets in our blood slippery, so they don’t clump up together and cause a clot.
Cardiac catheterization may be performed to determine the extent and exact location of coronary artery obstructions. It allows cardiologists to identify patients who might benefit from percutaneous coronary intervention (PCI) or from coronary artery bypass graft (CABG).
Myocardial infarction - interventions
Reperfusion therapy:
One of two reperfusion strategies are used to open a blocked artery in an MI patient: thrombolytic therapy or percutaneous coronary intervention (PCI).
Thrombolytics:
Fibrinolytics dissolve thrombi in the coronary arteries and restores myocardial blood flow. Targets the fibrin component of the coronary thrombosis. Examples: Tissue plasminogen activator (tPA, alteplase), Reteplase, Tenecteplase, Streptokinase
Contraindications: Not for NSTEMI patients. Previous intracranial hemorrhage, active bleeding, and significant trauma within 3 months.
NSTEMI the clot is primarily composed of platelets with some fibrin. This "white thrombus" is not easily broken down by fibrinolytic agents, which target fibrin.
Myocardial infarction - Interventions: Reperfusion therapy
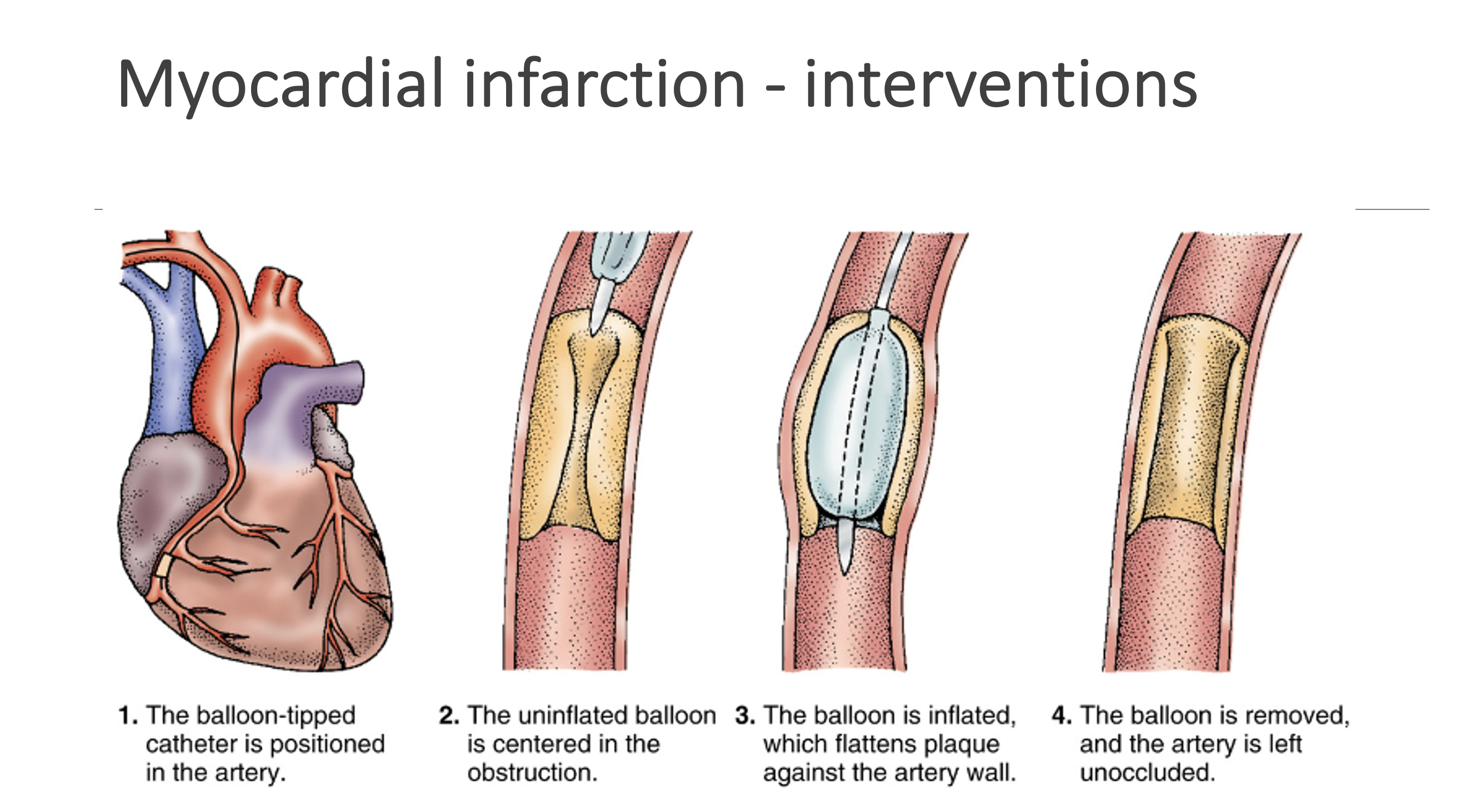
Reperfusion therapy: Percutaneous coronary intervention (PCI):
An invasive but nonsurgical technique that is the treatment of choice to reopen the clotted coronary artery and restore perfusion. Goal is to perform PCI within 90 mins of STEMI patients. Once the clot is found, cardiology removes it with a retrieval device.
Next, a balloon-tipped catheter is inserted to the coronary artery occlusion. Then the small balloon is inflated to force the plaque against the vessel wall (angioplasty) → dilating the wall and reduces or eliminates the occluding clot.
After balloon is inflated, a stent is placed. Stents are expandable metal mesh devices used to keep the blood vessel patent.
PCI: send pt to the cath lab and they insert a cardiac catheter sheath into the pt’s artery to visualize where the clot/obstruction is in their coronary arteries.
Cardiac catheterization may be performed to determine the extent and exact location of coronary artery obstructions. It allows cardiologists to identify patients who might benefit from percutaneous coronary intervention (PCI) or from coronary artery bypass graft (CABG). Usually, they will also put in a stent if doing PCI, due to some redeveloping the blockage after balloon inflation
aspirin and clopidogrel are prescribed together as dual antiplatelet therapy (DAPT) to prevent blood clots in and around a cardiac stent, and keeps stent open
Myocardial infarction - Interventions: Reperfusion therapy
Laser angioplasty
Uses laser device to break up the clot
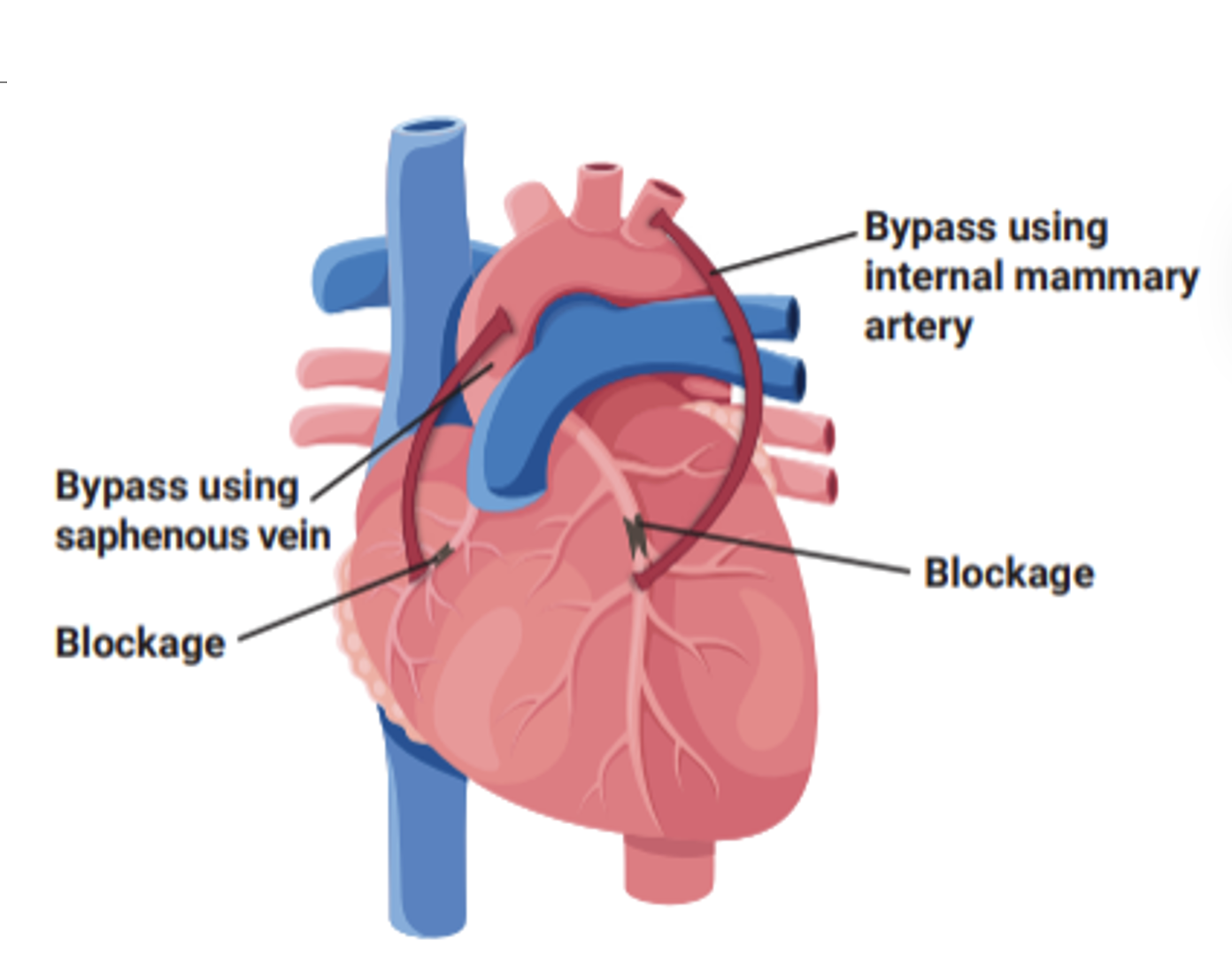
Coronary artery bypass graft (CABG)
The occluded coronary arteries are bypassed with the patient’s own venous or arterial blood vessels or synthetic grafts.
CABG is most effective when adequate ventricular function remains and ejection fraction is close to or greater than 50%.
Invasive - open heart surgery