Human Occ: Chap. 8 M&W Vision
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
Chapter Questions
Question 1:
Based on the above information, Chuck may have difficulty with completing which of the following daily tasks?
Correct Answer:
B. Shaving the left side of his face
✅ Because Chuck has a left visual field deficit, he may not see or notice that he did not shave the left side.
Question 2:
The occupational therapist has delegated to you to perform a quick, objective visual assessment of his HH severity. Which assessment would be most appropriate to quickly assess his HH?
Correct Answer:
B. Have Chuck cross out all the “A’s” on a sheet filled with random letters
✅ This provides a fast, objective measure of his visual field and can be retested to monitor progress.
Question 3:
During a recent therapy session, Chuck asked how soon his vision will return to normal so he can return to work. What is the best approach to take with Chuck when answering this question?
Correct Answer:
B. Communicate to Chuck that it is too soon to tell
✅ This is truthful and acknowledges that recovery from HH varies widely.
Question 4:
How can HH impair his safety in the home?
Correct Answer:
A. He may be unaware of hazards on his left
✅ For example, he may not see a step, a stove burner, or other hazards on his left side.
The Vision Treatment Team
Ophthalmologist
Medical doctor (MD) specializing in eye health and diseases
Diagnoses and treats eye conditions like cataracts, glaucoma, macular degeneration
Performs surgical procedures related to the eyes
Neuro-ophthalmologist
MD with training in both neurology and ophthalmology
Evaluates and manages vision problems caused by brain or nerve conditions (e.g., stroke, MS, tumors)
Assesses visual field loss and eye movement disorders
Optometrist
Doctor of Optometry (OD) focused on vision care and eye health
Performs eye exams, prescribes corrective lenses
Screens for eye diseases and refers to ophthalmologists for advanced care
Behavioral Optometrist (Vision Therapy)
Optometrist with a focus on how vision impacts behavior, learning, and function
Provides vision therapy to improve tracking, focus, eye coordination, and visual processing
Often works with children or clients with brain injuries
Physiatrist
Medical doctor (MD) specializing in physical medicine and rehabilitation (PM&R)
Manages rehabilitation for clients with neurological or musculoskeletal issues
Coordinates care with OT, PT, and SLP; may oversee recovery after stroke or TBI involving vision impairments
Anatomy
Anatomical Feature | Function |
|---|
Lens | Focuses light rays onto the retina |
Cornea | Transparent front layer; allows light to enter the eye |
Pupil | Regulates how much light enters the eye by dilating or constricting |
Iris | Colored part of the eye; controls pupil size |
Vitreous Body | Gel-like substance between lens and retina; maintains eye shape and helps transmit light |
Optic Nerve | Transmits visual information from the retina to the brain’s visual cortex |
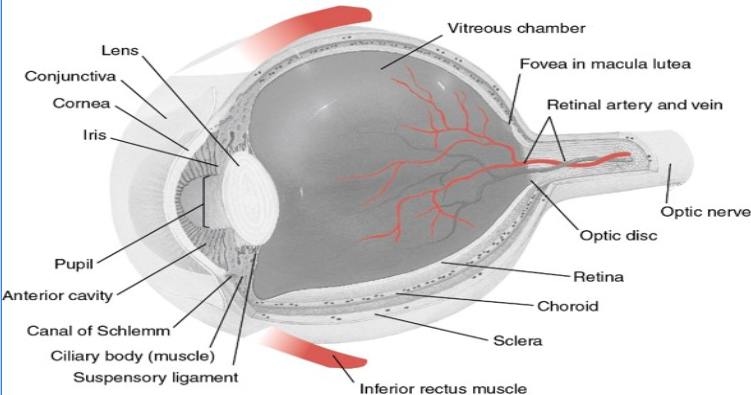
More anatomy of the eye
ANATOMICAL FEATURE OF THE EYEBALL | FUNCTION |
Fovea | Located in the retina, provides the most acute vision |
Macula | Located near the middle of the retina. Enables visualization of objects with great detail |
Retina | Sensory membrane that lines the eye. Receives images from the lens and converts them into signals that reach the brain via the optic nerve |
Choroid | Layer of blood vessel; provides nourishment to the back of the eye |
Sclera | White portion of the eye |
Visual Acuity and Fields
Acuity
Sharpness of vision
Visual field
Extent of visual space that is visible
65o upward
75o downward
95o outward
Functionally 180o horizontally & 125o vertically
Visual field deficits
Blind spots in a portion of the visual field
Types of Loss
Type | Description |
Hemianopsia | Vision loss in one half of the visual field in one eye |
Homonymous hemianopsia | Vision loss in one half of the visual field on the same side of both eyes |
Quadrantopsia | Vision loss in one quarter of the visual field |
Visual Skill Terms
Term | Definition |
|---|---|
Oculomotor Control | Ability to move the eyes smoothly and accurately in all directions |
Convergence | Eyes moving inward together to focus on a near object |
Saccades | Rapid eye movements that shift focus from one object to another |
Fixation | Ability to maintain steady gaze on a single object |
Diplopia (Double Vision) Clinical Observations:
Client may close one eye to avoid seeing double
Complaints of blurred or double images
Difficulty with reading, walking, or ADLs
Head tilt or abnormal posture to compensate
OT Interventions:
Occlusion techniques: Temporary eye patching (alternating or partial occlusion, under physician guidance)
Environmental adaptation: Reduce clutter, improve lighting
Prism training (with supervision): Reinforce awareness and compensatory scanning
Functional tasks: Practice ADLs with visual cueing and guided head movement
Physician Interventions:
Referral to neuro-ophthalmologist or optometrist
Prism glasses prescription
Botox injections (for muscle imbalance)
Surgical correction if persistent and impairing function
Pattern Recognitiona and Visual Memory
Pattern Recognition Definition:
The ability to identify features of an object (shape, color, texture) and distinguish it from others.
OT Interventions:
Matching games: Match shapes, colors, objects, or pictures
Sorting tasks: Categorize items by size, shape, or function
Puzzles: Simple to complex jigsaw puzzles to reinforce visual-spatial awareness
Functional tasks: Sort laundry, organize kitchen tools, or match socks
Spot the difference: Identify changes or missing items in images
Visual Memory Definition:
The ability to recall and recognize visual information after a brief delay.
OT Interventions:
Memory matching cards: Turn over and match images from memory
Copy then recall: Have the client copy a shape or word, remove it, and reproduce it from memory
Repetition drills: Repeated practice with recalling faces, names, signs, or object placements
"What's missing?" tasks: Show an image, remove one element, and ask what’s missing
Functional applications: Remember steps in grooming, location of kitchen items, or visual details in a daily schedule
Visual Perception Definition:
“The dynamic process of receiving the environment through sensory impulses and translating those impulses into meaning based on previously developed understanding of that environment.”
Key Points:
It’s not just seeing, but interpreting what is seen
Involves recognition, interpretation, and response to visual stimuli
Relies on past experiences and learning to give meaning to what is seen
Essential for performing functional tasks like reading, dressing, navigating, and organizing objects
Examples in OT:
Identifying objects during grooming
Reading and writing
Locating clothing in a drawer
Safely navigating a room
Visual Discrimination
Spatial Relations
Definition: Understanding where an object is in relation to self or other objects
Example OT Activities:
Positioning a toothbrush in the holder
Placing dishes into a drying rack correctly
Navigating around furniture during mobility tasks
Form Discrimination
Definition: Recognizing and distinguishing the important features of different objects (e.g., size, shape, texture)
Example OT Activities:
Identifying coins or buttons by feel or sight
Sorting silverware or puzzle pieces
Matching clothing by fit and form (e.g., left shoe vs. right shoe)
Figure Ground
Definition: Differentiating an object from the background or surrounding objects
Example OT Activities:
Finding a pen on a cluttered desk
Locating a sock in a patterned laundry pile
Reading text on a busy or decorative background
Visual Closure and Depth Perception
Visual Closure
Definition: The ability to recognize a complete object or image when only parts are visible
Example OT Activities:
Completing partially drawn pictures or puzzles
Identifying a familiar item when part of it is hidden (e.g., a shoe sticking out under a bed)
Recognizing letters or words when parts are obscured (e.g., smudged handwriting)
Depth Perception
Definition: The ability to judge how far away an object is or perceive the space between objects
Example OT Activities:
Pouring liquids without spilling
Reaching accurately for a cup or utensil on a table
Navigating stairs or curbs safely during mobility
Hemi Deficits
Hemi-Inattention
Definition: Decreased awareness of one side of the body or environment (commonly the left side after right brain injury)
Hemi-Neglect (Unilateral Neglect)
Definition: More severe form of hemi-inattention; the person has no awareness of the affected side and may act as if it doesn’t exist
OT Interventions
Visual scanning training: Teach the client to actively turn head and eyes toward the neglected side
Lighthouse strategy: Guide client to scan left to right repeatedly, like a lighthouse beam
Tactile & verbal cues: Use touch or voice prompts to bring attention to the neglected side
Mirror therapy: Use mirrors during ADLs to increase visual awareness of affected side
Functional tasks: Encourage bilateral tasks (e.g., folding towels, washing face) that require use of both sides
Weight-bearing: Incorporate weightbearing or movement through the neglected side (e.g., leaning on left arm during tasks)
Agnosia
Agnosia – inability to recognize/perceive sensory info
Prosopagnosia – inability to recognize faces
Simultagnosia – inability to perceive entire picture or integrate its parts
Tactile agnosia (astereognosis) – inability to recognize objects by feel
Auditory agnosia – inability to recognize sounds
Object agnosia – inability to recognize objects
Intervention is generally a compensatory strategy
Vision Conditions
Condition | Main Problem | Vision Loss Pattern | Cause | Key Feature |
|---|
Macular Degeneration (most common) | Damage to the macula (central retina) | Loss of central vision | Age-related degeneration | Can’t see fine detail; peripheral vision intact |
Cataracts | Clouding of the lens | Blurry or cloudy vision (global) | Aging, trauma, or medical conditions | Glare sensitivity; colors appear faded |
Glaucoma | Damage to optic nerve from high eye pressure | Loss of peripheral vision (tunnel vision) | Increased intraocular pressure | Often painless and progressive |
Diabetic Retinopathy | Damage to retina’s blood vessels | Patchy vision loss, floaters, blind spots | Uncontrolled diabetes | May lead to total blindness if untreated |
Hemianopsia | Brain damage (usually stroke-related) | Loss of half the visual field (left or right) | CVA or brain injury | Not an eye problem — it's a visual field cut |
Low Vision
Someone with low vision can often complete basic ADLs (like dressing, eating, and personal hygiene) because these tasks don't typically require detailed visual input or can be adapted with touch or other senses. However, they may struggle with work, leisure, and many IADLs due to the higher visual demands:
Driving: Requires clear and precise vision for safety, navigating, and reading signs.
Pet care: Involves visual monitoring of the pet’s health, activities, and behavior, which can be challenging without good vision.
Financial management: Tasks like reading bills, counting money, and using a computer or phone for transactions rely heavily on visual accuracy.
Home management: Activities like cooking, cleaning, or organizing often require the ability to visually locate and identify objects, check expiration dates, or assess cleanliness.
Aids for Low Vision
compensation, adaptations, equipment, and environmental modifications. Here's how OT can help:
Education: Teaching clients strategies to maximize their remaining vision and use other senses to complete tasks.
Environmental Adaptations: Modifying home or work environments to improve safety and function. For example:
Lighting: Increasing light intensity or using task-specific lighting to enhance visibility.
Color Contrast: Using contrasting colors on objects (e.g., white labels on dark containers) to make them easier to see.
Tactile Cues: Adding raised symbols or textures to help with locating objects (e.g., textured labels or knobs).
Aids and Equipment:
Magnifiers: Hand-held or stand magnifiers to enlarge text or images for easier reading.
Writing Aids: Large-print pens, paper guides, or electronic devices that convert text to speech.
Kitchen Aids: Adaptive tools like talking kitchen scales, large-print measuring spoons, or tactile timers to help with cooking and meal preparation.
Reading with Low Vision
Matte Paper: Reduces glare and makes text or images easier to read by using non-reflective surfaces.
Finger Guiding: A technique where the person uses their finger to follow along text or objects, helping to maintain focus and reduce misreading.
Anchor Lines: Horizontal or vertical lines used to help orient the person when reading or writing, assisting with alignment and preventing skipping of lines.
Good Lighting: Proper illumination is essential for maximizing any remaining vision. Using bright, focused lighting helps reduce eye strain and increases contrast.
Contrast: Using high contrast between background and text (e.g., black on white, yellow on black) helps improve readability for individuals with reduced vision.
Larger Font: Increasing the size of text, whether in print or on screens, makes reading easier for individuals with central or peripheral vision impairments.
Adaptations
Read at a table away from a window: Positioning oneself away from a window helps avoid glare and shadows that can make it difficult to see text or objects clearly.
Read on a wooden table instead of glass: Wooden tables are less reflective than glass, reducing glare and making it easier to focus on reading materials.
Enlarge the font on the computer or phone screen: Increasing the font size on digital devices makes text easier to read and reduces the strain on remaining vision.
Put a paperclip on the left-hand page: This creates a tactile cue, helping the individual orient the page and maintain their place while reading, which is especially helpful for individuals with central vision impairments.
More adaptations
Put different colored stickers on medication bottles: Using color-coded stickers helps differentiate between medications, making it easier to identify each bottle, especially when fine details may be hard to read.
Put a colored transparent sheet over the paper: A transparent colored sheet can enhance contrast, making text stand out more clearly against the background, which is helpful for individuals with certain types of vision impairments.
Read books on an e-reader or tablet: E-readers and tablets allow for easy font size adjustments, contrast changes, and background color modifications, providing a customizable reading experience for individuals with low vision.
Turn the head to one side while reading: For individuals with peripheral vision loss, turning the head to one side can help them use the more functional area of their visual field, improving their ability to see text or objects more clearly.