Arrythmia Pharmacology (pdf prof)
1/88
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
89 Terms
are the following examples of supraventricular or ventricular arrythmias?
assystole or pulseless electrical activity (PEA)
atrial flutter
atrial fibrilation
sinus tachycardia/ bradycardia
\paroxysomal supraventrical arythmias
supraventricular
which arrythmias are ventricular? below AV node?
what makes them life threatening?
Non sustained ventricular tachycardia (VTAC) - fixed in 30 seconds
sustained ventricular arrythmia (doesnt self-terminate—torsades de pointes)
ventricular fibrillation
life threatening bc/ cause abrupt decrease in cardiac output
what are some causes of arythmias?
hypoxia (decreased perfusion)
cardiac diseases
drug induced
increased sympathetic activity (exersize increase HR and force of contraction)
electrolyte imbalance
what electrolyte imbalances can lead to arrythmias?
must know magnesium and potassium regular levels!!!
hypo/ hyper
potassium (3.5-5.3)
magnesium (1.5-2.5)
sodium
calcium
hypo
phosphates
which antiarythmics dont fall under the vaghn williams classification?
which antiarrythmics could be considered apart of multiple classes?
digoxin and adenosine dont fall in classes
amiodarone, sotalol, dronedarone
which class medications are used for
rate control
rhythm control
rate = 2( beta blockers) and 4 (calcium channel blockers)
rhythem = 1 (Na+ channel blockers) and 3 (K+ channel blockers)
dogoxin is a cardioglycoside which inhibits ____ and is used for _______ and _______
inhibit Na+K+ATPase
used for
Atrial Fibrilaiton
Chronic Heart Failure
what changes would see on the EKG of a patient on class 1 antiarythmic (Na+ channel blocker)
prolonged QT interval (for 1A that also inhibits K+)
QRS widening (depolarization takes longer with blocked Na+)
how do class 1a (Na+ channel blockekrs) impact
conduction velocity
refractory period
automaticity
decrease conduction velocity
increase refractory period
decrease automaticity
SAME FOR CLASS 2 and 4
how do class 1b (weak Na+ channel blockers) impact
conduction velocity
refractory period
automacity (HR)
decrease conduction velocity
decrease or increase refractory period
decrease automaticity
how do class 1c (strong Na+ channel blockers) impact
conduction velocity
refractory period
automaticity
strongly decrease velocity
no effect on refractory period
decrease automacity
how do class 2 (b-blockers) drugs impact
conduction velocity
refractory period
automaticity
decrease conduction velocity
increase refractory period
decrease automaticity
SAME as 1A and 4
how do class 3 (K+-blockers) drugs impact
conduction velocity
refractory period
automaticity
NO effect on conduction velocity
INCREASES refractory period
minimally effect HR
how do class 4 (CCBs) impact:
conduction velocity
refractory period
automaticity
decrease
increase
decrease
SAME AS CLASS 1A and 3
Amiadorone has class ______ activity
what can it be used for?
3 AND 1, 2, 4
supraventricular arrythmias
ventricular arythmias
heart failure patients
post MI patients
what are some sideeffects of amiodarone (has class 1,2, 3, 4 activity)
cardio: bradyaryhtmia, hypotenison
CNS: tremor, visual changes, ataxia
derm: photosensitivity, blue-grey discoloration of skin
endocrine- HYPO and HYPERthydroidism due to iodine
hepatic: elevated LFT, hepatitis
respiratory: pulmonary fibrosis
opthalmic: corneal micro deposits
what are some drug-drug interactions to look out for on AMIODARONE?
highest dose you can take of simvastatin is 20mg
warfarin increased bleeding risk
digoxin concentration will increase by 100% DONT GIVE WITH DIGOXIN
has high protein binding so dont give with another durg that has high protein binding
Dronedarone is a derivative of amiodarone:
does it also have iodine?
what class activities does it have?
what dose is given
what is it used for?
NO iodine
3 AND 1,2,4
400mg po 2x a day with food
Dronedarone used for
paraoxysomal fibrilation (intermittent)
Persistent Atrial fibrilation
what are common side effects of Dronedarone?
increased sCr and HF exacrerbation
Dronedarone pk/pd:
what is its oral bioavialbility?
protein binding?
how is ti metabolized?
what is t1/2?
F= 15%
more than 98% bound to protein in blood
CYP3A4 in the liver
t1/2 = 20 houes which is less than amiodarone which is 40 days
what black box warning came out after the ANDROMEDA trial?
BBW for dronedarone
do not give to patients with NYKA Class 4 heart failure of those with class 2 and 3 who require hospitalization b/c of INCREASED RISK OF MORTALITY
what class actiivty does sotalol have?
what can it be used for?
how is it eliminated? does it require dose adjustments?
3 and 2 (beta blocker)
A- fib
A- flutter
renally eliminated so it DOES need renal adjustments
what levels should you check for BEFORE giving a patient at the hospital SOTALOL for Afib or Aflutter?
CrCl should be more than 40mL/min
K+ should be more than 4
QT interval should be less than 450msec because it can increase QT iinterval
what are adverse effectss of sotalol (has both 2 and 3 activity)?
QT prolongation
bronchospasm
beta blocker
Dofetilide
used to treat ?
what are some side effects?
how long does a patient need to be in the hospital before considering htis medication?
what should you look out for before giving this medication to a patient?
atrial fib/flutter (like sotalol)
side effects:
QTc prolongation → torsades de pointes
increased Scr (so must be aware of CrCl)
need to be in hopsital for at least 3 days
look for
creatinine clearance (bc/ increse sCr)
magnesium
low potassium
currenet QTc interval
Dofetalide dosing:
bc/ it can increase SrCr how do you dose people with the following CrCl?
CrCl >60 ml/min
CrCl = 40-59
CrCl = 20-39
CrCl= <20
if greater than 60 then 500mcgBID
40-59 = 250mcg BID
20-39 = 125mcg BID
less than 20 = DONT USE (will experience toxic levels of SrCr because your body cant get rid of it)
What drugs CANT you take with Dofetalide
Which drugs SHOULDNT you take with DOfetalide
CANT:
verapamil
HCTZ
trimethoprim
SHOULDNT unless you absolutely have to:
amiodarone
diltiazem
a heartbeat of _____ is considered Sinus Bradycardia
which patient population is seen the most?
causes prolongation of _____ interval but has normal _____
what drug can be used to treat? what is the dosage
heartbeat less than 60bpm
mostly seen in student atheltes
prolongation of RR interval w/ normal RHYTHM
can use ATROPINE to treat (bind to m2 receptor to stop the cholinergic parasympathetic supression of SA excitability)
atropine dosage = 0.5mg every 3-5 minutes (max 3mg)
what are your other options if a sinus bradycardiac patient is not repsonsing to atropine?
dopamine or epinephrine infusion
what if you get a patients EKG with a minimal electrical activity (flat line)?
what do you check for?
what do you give?
CAB
C= circulation
A= airway
B= breathing
Acces for open airway, pt breathing, check for pulse
give Epinephrine (1mg IV every 5 minutes)
if you see a flatline on an EKG what 5Hs and 5Ts could be the caus of the Cardiac Arrest?
Hypothermia
Hypoxia
Hypo/Hyper Kalemia
Hypovolemia
High H+ (acidosis)
Toxins
Tension Pneumothroax
Tamponade
Thrombosis
Trauma
what class drug would you give if the patient is
bradycardic
tachycardia
arrythmia due to SA or AV node
arrythmia due to atrial or ventricular myocytes
bradycardic = atropine (dopamine/ epinpephine), Iv fluids, pacemarker
tachycardia: beta blockers (2) or Ca2+ blockers 4)
SA or AV node= 2 or 4 (B-blocker or Ca2+)
atrial or ventricular myocyte: 1 or 3 (K+ or Na+)
which drugs would cause sinus tachycardia?
beta adrenergic agonsits
epinephrine/norepinephrine
dopamine
albuterol
alpha 1 blockers
prazosin and doxasosin
decreased SVR—> vsodilation —> increase HR
nitrates
nifedipine
hydralazine
recreational drugs
marijuana
cocaine
amphetamines
anticholinergics
diphenhydramine
atropine
what can cause sinus tachycardia (HR>100pbm) and how can you treat it?
anxiety/pain= benzos and opiods
anemia = give blood transfusion
hypovolemia = give fluides (saline)
fever= cooling pads, treat infection
hypERthyroidism= radioactive iodine and propylthiouracil (PTU)
hypoxia = give oxygen
drug induced= take out of treatment
Which wave is missing in Atrial Fibrillation?
How fast is the atrial contraction rate? ventricular contraction rate?
Is the rhythm normal?
arythmias ABOVE the ventricles have a ______ QRS complex
__ intervals occur at irregular intervals
AFib missing P wave (atrial depolarization) before QRS
atrial contraction >300
ventricular contraction >200
ABNORMAL rhythm
NARROW QRS complex
RR intervals irregular (off rhythm beat) no synchorinized depolarization, there are different stimuluses causing the atrial contraction
what is considered
paroxysomal Afib
persistent AFib
longstanding Aib
peramanent Afib
Nonvalvular Afib
self terminates before 7 days
takes longer than 7 days to self terminate
more than 12 months
treatment has failed, nothing more can be done
Af in the absensse of mechanical or biprosethic heart valves
what would lead to paroxysomal afib which is usually recovered less than 7 days
(acute reversible causes) ?
alcohol intoxication / withdrawl
CABG surgery
hyperthyroidism
hypoxia
electroylyte abnormalities
what would lead to persistent AF (Afib longer than 7 days?)
HTN w/ atrial ENLARGEMNT
valvular heart disease
mitral stenoisis
rheumatic heart disease
atrial stretch
MI
HF
what are some signs and symptoms of Afib?
Palpatations
Ischemic Stroke (not meeting oxygen demands) — heart going crazy to meet them w/ increased heart rate
Congestive heart failure
Hemodynamic complications of Afib are due to reductions in _____ _______
due to a loss/ enhancment of the atrial kick or ______ _________ complication
REDUCTION of CO due to LOSS of Atrial kick which increases pressure in atria to allow blood to flow to the ventricles
or thromboembolic complication (stasis of blood in atria)
what should be taken for patients w/ Afib for their
rate control
rhythm control
cardioeversion
Rate control:
beta blockers (2)
CCB (4)
digoxin (stimulate parasympathetic vagus system decrease AV conductio
anticoagulation/antiplatelet
ON THERAPY INDEFINITELY
Rhythm control:
electrically or pharmacologically CARDIOVERT back to normal sinus rhythm
anticoagulation must be given BEFORE and AFTER the attempt
synronized current cardiversion
Cardioversion:
electrical cardioversion (electric shock paddles)
what is cardiac ablasion and when is it used?
insert a catheter into arm or groin vein and apply heat to kill the tissue of the heart that is causing abnormal rhythem
can be used for Afib or Aflutter (most likel)
in Afib you can destroy and take out the patients AV node and replace it with a pacemaker
which medications can you use to maintain a normal sinus rhythm in a patient with Afib who has
normal left ventricle function
NO MI
NO structual heart disease
Dofetallide (3 K+)
Dronedarone (3 K+ )
Flecainide (1C Na+)
Propafenon (1C Na+)
what can be used to RESTORE RHYTHM in a patient with atrial fibrilation WITH structural heart disease
if they are in class 3 or 4 and have also had recent decompensated HF what should you AVOID
Afib with structural disease =
amiodatone (class 3 K+)
dofetalide (class 3 K+)
DONT TAKE DRONEDARONE if youve had decompensated HF!
if patient presents w/ Afib and is hemodymaically stable vs ubstable what do you give them?
if they have valve issues but recover before 48 hours have passed, what can you give them, and if fthey havent recovered after 48 hours what do you do?
if unstable = cardioeversion
if stable = HR medications (CCB, b-blocker, digoxin) + consider heparin
if valve issues less than 48 hours = antiarrythmic treatment- rythm (k+ and Na+ blockers) but if still valve issues then get them a TEE GUIDEED CARDIOVERSION or cardioversion
with cardioversion MUST be on anticogulants for at least 3 weeks BEFORE and at least 4 weeks AFTER
How to go about maintancing the sinus rhytm w/ K+ and Na+ blockers:
if the patient has minial heart disease what can you start them on and what do you do if that doesnt work?
flecainamide
propafenone
sotalol
dronedarone
if that doesnt work go to amiodaroneor dofetalide
if amiodarone dont work TAKE IT OUT (catheter abllation)
How to go about maintancing the sinus rhytm w/ K+ and Na+ blockers:
if the patient has hypertension what can you start them and what do you do if that doesnt work?
check if they have had left ventricular hypertrophy
if they HAD LVF then
amiodarone
if that doesnt work then do cathetar
if they DIDNT have LVF then
flencainabe
profenone
sotalol
dronedaron
doesnt work
amiodarone
dofetalide
that doesnt work TAKE IT OUT (catherer abrasion)
How to go about maintancing the sinus rhytm w/ K+ and Na+ blockers:
if the patient has coronary artery disease what can you start them and what do you do if that doesnt work?
start with K+ blockers (NO Na+ THIS TIME)
dronedarone
sotalol
dofetalide
if that doesnt work then
amiodarone
if amiodarone doesnt work
TAKE IT OUT (abrasion catheter)
How to go about maintancing the sinus rhytm w/ K+ and Na+ blockers:
if the patient has heart failure what can you start them and what do you do if that doesnt work?
start with K+blocker (NO Na+ this time)
amiodarone
dofetalide
if they dont work then
TAKE OUT (catheter abrasion)
ONLY TIME AMIODARONE IS FIRST LINE IS WITH THOSE WITH HEART FAILURE
when treating patients with amiodarone or dofetalide (K+ channel blockers) to avoid torsades de pointes from QTc prolongation WHAT DOSES should you give?
amiodarone = NO MORE THAN 10g (oral , can be IV too)
dofetalide DONT USE IF LESS THAN 20CrCl (just oral)
which patient populations should you avoid Dronedarone?
recent hospitalizations
class 3/4 Heart Failure
what are advantages and disadvantages of the following rate controlled medications used for Afib?
beta-blockers
CCBs
digoxin
b-blockers:
benefit: fast onset, used after surgery
bad: asthma, worsen CHF, bradycardia, hypotension
CCBs:
benefit: fast onset
bad: worsen CHF, hypotension
digoxin
benefit: can help with CHF
bad: slow onset, requires a loading dose and renal adjustment
would you use rate or rhythm control medications for the folloiwng patient type?
older than 65 years
persisten Afib
permanent Afib
rate control
B-blockers
CCBs
Digoxin
would you use rate or rhythm control medications for the folloiwng patient type?
younger generation
new Afib
symtpomatic but able to control rate
unable to control rate
rhtyhm control
K+ blockers (dofetalite, dronedarone, sotalol, amiodarone)
Na+ blockers (flecainamide, proferenone)
what is apart of the CHADS2 score and when do you use it?
use CHADS2 score to determine risk of stroke and whetehre or not you should be put on an antithrombotic for Afib
past TIA and prior stroke = 2 points
older than 75 = 1 point
diabetes= 1 point
hypertension = 1 point
heart failure = 1 point
what are the factors of the CHA2-DS2VASc ?
older than 75= 2 points
65-74 = 1 points
V= vascular disease (MI, PAD) = 1 point
female= 1 point
what is CHAD2 of
78 year old male
new Afib
CHF
HTN
glucoma
arthritis
78= 1 point
CHF= 1 point
HTN= 1 point
3
what CHAD Score would you NOT give anticoagulation therapy?
when would you CONSIDER antiagulation?
when would you HAVE to give anticoagulation DAILY>
NO THERAPY = 0 in men 1 in women
CONSIDER= 1 in men and 2 in women
MEN= 2 for men and 3 for women
a male patient has a CHAD of 2 and female has CHAD of 3 so they MUST be on anticoagulants
what are their options?
Warfarin with heparin or lovenox to reach INR 2-3 (if no valve issues) - if they have valve issues may change INR goal
Dabigitran- Pradaxa (direct thrombin ihibitor) if CrCl less than 15 DONT give
Rivaroxaban- Xarelto- (AntiFactor Xa)
if less than 15 CrCl or on dialysis can STILL GIVE 15mg
Apixaban- Eliquis (Antifactor Xa)
5mg but if SCr>1,5 or age or low body weight then 2.5mg
EndoXaban- Savaysa (Antifactor Xa)
DONT GIVE if CrCl more than 95 or less than 15
Aflutter:
“____ ____” pattern on EKG
which wave is missing
what is the rate of the hearbeat?
Saw tooth EKG
P wave missing
HR= 250 -350 (in Afib >300)
What is the most common type of flutter and which patients is it seen the most in?
paroxysomal (transient- self curing)
irregular HR of 100-130bpm
narrow QRS complex
still regular rhythm
when do reentrant circuits occur? which type of supreventricular arrythmia is caused by this?
they occur when there is another stimulus that allows the signal from SA node to go directly to the ventricles without goin through the AV node first
example Wolf Parkinson White Syndrome (self- sustained Action potential propogating tachycardia)
The most common type of Atrial flutter is paroxysomal atrial flutter which is caused by reentract pathways that can pass sinal to ventricle from atria without going through AV node first
What can be used as treatment?
direct current if acuteley hemodynaic and UNSTABLE
increase vagal tone -
increasing thoracic pressure- holding breath and exhaling as forcefully as you can
carotid sinus massage
holding your nose and breathing out
use meds to stop reentractment
how do you treat a patient with Aflutter?
if they are hemodynamically unstable?
Narrow QRS
Wide QRS
hemodynamically unstable = direcct current
narrow QRS= adenosine (max 30mg) or Ca2 + channel blockers
wide QRS= adenosine OR VTACH meds
NARROW QRS signifies _____ arrythmia
Narrow = Supraventricular
what is the halflife of adenosine?
what follows its use?
when is it used?
Halflife = 10 seconds
MUST FLUSH WITH SALINE AFTER
Aflutter if QRS narrow
Aflutter if QRS wide + VTach treatment
NOT used for Afib b/c of short halflife
what is the treatment for patients who experience sudden cardiac death? is this common for patient with Premature Ventricular COntractions?
defibrillation is the treatment
not common for healthy individuals with ventricular contractions BUT IS common for patients with structural heart diseases
Premature Ventricular Contractions result in bizzare ______ on the EKG
what is treatment?
what should you AVOID bc/ of MORTALITY!
QRS bizzare (could be upsidedown and WIDE)
can be uniform or multiform
USE BETA BLOCKERS UNLESS 3 in a row bc/ then you have VTach not premature at this point
Avoid using CLASS 1C antiarythmics such as (profenone and flecainamide) in premature vesicular contraction with STRUCTURAL HEART DISEASE
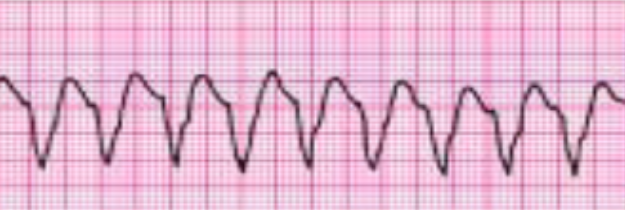
When is one considered to have Vtach?
3 consecutive premature ventricular contraction that appear on the EKG as BIZZARE QRS (widened more than 120 ms) and HR more than 100 bpm
also no P waves
due to REENTRY
what is considered to be non-sustained VT vs what is considered sustained VT?
nonsustained = less than 30 seconds
sustained = more than 30 seconds (NEED DRUGS)
which Vtach ?
due to re-enterant pathway looping in a ventricle that DOESNT allow for signal to propogate further
SOMETIMES generates enough CO to produce pulse for a short time
no P waves / wide QRS
impulse originating in ventricles not SA
monomorphic
what are preventable causes for Vtach?
hypokalemia (K+ supplementation)
Hypoxia (ventilation)
acute MI (post MI care)
digoxin overdose (antidote)
what can cause reoccurent Vtach?
CAD (coronary artery disease)
post MI
Left Ventricular Ejection Fraction less than 40% (ischemic)
how do give drugs to patients with Vtach?
hemodynamically unstable
hemodynamically stable
if unstable work on cardiaversion
if stable
amiodarone (max 2.2g/day or adenosine or cardiaversion
OR
class 1a/ 1b: procainamide and lidocaine
Patient comes in and their heart rate is greater than 150bpm
what if this patient is also experiencing hypotension, altered mental status, shock, chest pain?
where get a EKG and see that their QRS wave is 120ns+ (0.12s) how do you proceed?
if experiencing concurrent issues consider cardioeversion
wide QRS (more than 120ns) = Vtach = adenosine (if regular and monomorphic) or antiarrythmic infusion (amiodarone)
if NOT wide QRS than try vagal maneuvers, adenosine, beta blocker
what is an Implanatable Cardioverter defibrillator (ICD) and when is it used?
if a patient has an implant in, can they still use antiarythmics?
implantable electrical pulse generator
used for patients with monomorphic Vtach or Vfib who are at risk for sudden cardiac death
YES they can still use
sotalol
amiodarone
Polymorphic Vtach:
irrelegular QRS complex — non uniform
torsades de pointes (QTC prolongation) is a type of polymorphic Vtach, what is a normal QT interval?
do all polymoprhic Vtachs include a prolonged QTc?
normally Q to end of T wave is less than 430ms but if its greater than 430 then QTC prolongation
how to count: count small boxes and multiple by 0.04
NO can also have normal QTC if polymorphic Vtach
what are the risk factors of drug induced fatal polymorphic vtach (Torsades de Pointe)?
female elderly
low magnesium, potassium, glucose, and thyroid
hypothermia
bradycardia or HTN
CHF, MI, ischemia, and stroke
QTc: corrected measurement of QT interval for HR variation
QT/ square root RR
which drugs CAN CAUSE torsades de pointes (polymorphic ventricular tachycardia)?
class 1A (moderate) - extend repolarization by blocking K+ channels
quinidine
disopyramide
procainamide
class 3 - increase repolarizing
sotalol
dofetilide
amiodarone
dronedarone
which drugs shuld you avoid that can extend the halflife of QTC prolonging drugs?
how do these drugs extend halflife of QTC prolonging drugs?
QTC prolonging drugs are metabolized by CYP2D6 and 3A4
inhibitors of 2D6
fluoxetine and haloperidol
inhibitors of 3A4:
amiodarone, fluconazole, omeprazole, simetidine, metronidazole, ritonavir, clarithromycin
which drugs can INDUCE torsades de pointes and which cyp inhibitors should you AVOID?
Antibiotics (ertyhromycin, fluroquinolones)
antidepressants (Tricyclic)
atypical antipsychotics (quietapine + clozapine)
barbituates
methadone
what can you use to TREAT drug-induced torsades de pointes?
increase magnesium levels (even if normal)
and increase K+ if less than 4meQ
this will slow the rate of the SA node and prolong the impulse
what is FIRST line therapy BEFORE any medications for a patient experiencing ventricular fibrilation/ tachnycardia?
CPR and Defirbillation every minute delayed = 10% chance increase of death
WHILE you are giving a patient CPR, they can be admiinistered EPINEPHRINE (1: 10,000) 10mL IV
how does each agonism of epinephric help?
a1= increase BP and decrease epiglottal edema
b1= incrase CO and BP
b2= bronchodilate
what are the two antiarrythmic drugs that are used for ventricular arythmias?
amiodarone (3)
class 1b= lidocaine (blocks Na+ channels of ischemic tissues - which can have sporadic stimulation)
be careful of Lidocaine use in patients with
live failure, heart failure, MI
therapetuic levesls - 2-6mg/L (unbound+ bound)
Therapeutic hypothermia is also used for patients with pulsemless VT//Vfib
which temperature do you try to keep the patient in to jumpstart their heart?
what can be an issue of hypothermia?
try to get patient to 32-34 degrees celcius (normal 37) for 12-24 hours who has regained circulation after cardiogenic shock (ROSC)
coagulopathy (blood comming together), hyoerglycemia, electrolyte imbalances
patient comes in with Vfib/tachycardia what do you do IMMEDIATELY?
how long do you wait before starting shock in shockable patients? (Vfib and Polymorphic Ventricular Arythmia/ Torsades de Pointes)
CPR
shock after 2 minutes of CPR
THEN administer epinephrine during next cycle of CPR for two minutes
then shock again and give lidocaine and amiodarone
patient comes in with Vfib/tachycardia what do you do IMMEDIATELY?
what do you do if the patient is unshockable (Asystole/ pulseless electrical activity)
EPINEPHRINE THEN CPR
then
check if you can shock
if you cant
continue CPR and try to treat reversible causes
if you still cant
epinephrine and reversible causes
once you can go back and forth between CPR + infusion THEN (epi) — CPR +infusion THEN amiodarone/lidocaine