Endothelial Function and Peripheral Artery Control - Gow
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
Review Vascular Tree
Two circuit system
arteries/veins are not the same because arteries take blood away from the heart and veins take blood toward the heart
Compliance vessels: veins
expand and hold large volumes of blood.
“Blood reservoir”
Resistance vessels:
arterioles control blood flow and bp.
Vessel Diameter: size, thickness, proportion of elastic and fibrous
Artery:
Largest, thickest
Mostly smooth and elastic, some fibrous
Arteriole:
2nd largest and thickest
No elastic or fibrous, just smooth muscle
Capillary:
Smallest, thinnest
No muscle
Venule:
2nd largest, same thickness as artery
Some fibrous tissue
Vein:
Largest, slightly thinner than artery and venule
Equal amount of elastic, smooth, and fibrous tissue
Small Artery Structure
Layers from outside → inside:
Adventitia – outer protective layer.
Media – smooth muscle that changes vessel diameter.
Intima – inner lining touching the blood.
Elastic lamina (internal/external) – stretchy layers helping arteries expand and recoil.
Arteries are structured to withstand high pressure and regulate blood flow.
Capillary Structure
Basal lamina → supports the capillary
Pericytes → provide stability & regulate flow
Vesicles → move substances across the cell
Fenestrations (pores) → allow faster movement of small molecules
Interdigitated junctions → control what passes between cells
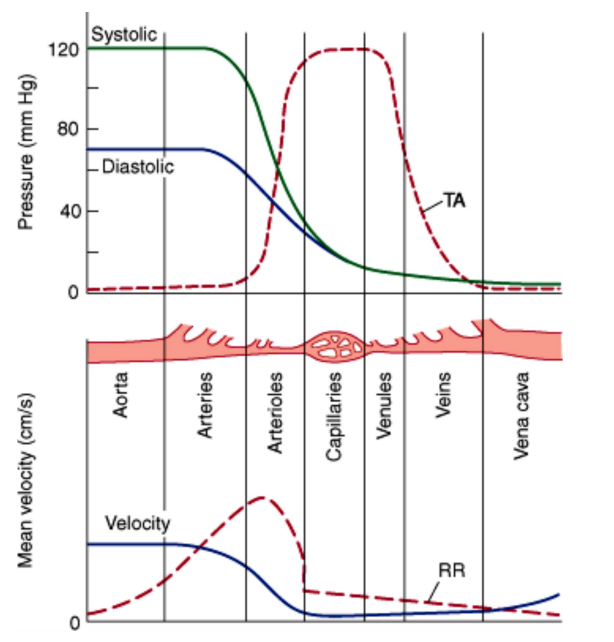
What is vascular pressure determined by? What does the graph show?
diameter
transmural pressure:
P = T/r
Aorta 170kdynes/cm
Capillary 16 dynes/cm
Pressure (Top Graph)
Aorta → arteries → arterioles: Pressure steadily drops
Capillaries: Very low pressure to allow safe exchangs
Systolic & diastolic values only meaningful in large arteries
Velocity (Bottom Graph)
Fastest in aorta and arteries
Slowest in capillaries (allows nutrient/gas exchange)
Speeds up again in veins
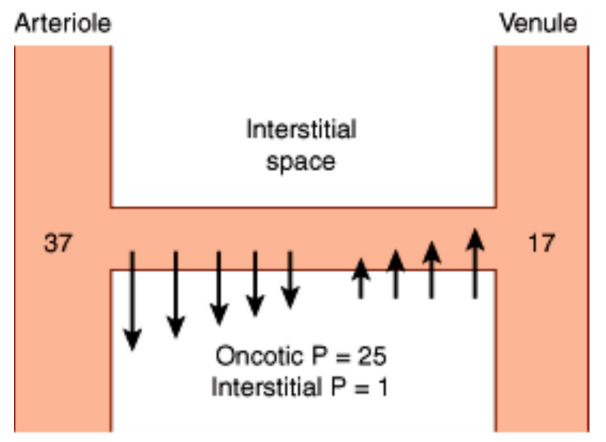
What is fluid flow determined by?
hydrostatic pressure
due to high hydrostatic pressure in the arterioles, fluid is pushed out
oncotic pressure pulls fluid into the interstitial space
due to low hydrostatic pressure in the venules, fluid is reabsorbed into venules
(back and forth motion, vice versa)
How do we regulate vascular function?
Vascular Metabolites: CO2, K+, temp, pH, adenosine
Autoregulation: myogenic response
Endothelial Control: response to shear stress and stretch, long/short term regulation
endothelial control
prostacyclins and thromboxanes: made form arachidonic acid through COX pathway balance each other out
TXA2: produced by platelets which initiate aggregation → vasoconstriction
PGI2: produced by endothelial cells → vasodilation
Aspirin: decreases production of TXA2 and PGI2 (cardioprotective)
What is NO produced by? what are the three isoforms? What turns production on/off?
produced by Nitric Oxide Synthase (NOS)
isoforms: e, n, i
mechanisms:
calcium-calmodulin: increase NO
phosphorylation: both
caveolin: decrease NO
How do we activate NOS? (→ increase NO)
neurohumoral: ACh, Histamine, bradykinin, serotonin, substance P
physical: shear stress
metabolic: NADPH (cofactor for NOS to funciton), Oxygen
What activates Nitric Oxide Synthase (NOS)?
↑ Calcium activates NOS
Requires critical cofactors: heme + tetrahydrobiopterin (BH₄)
Uses substrates: L-arginine, O₂, NADPH
Produces: Citrulline + Nitric Oxide (NO) + NADP
What happens after nitric oxide (NO) is produced by endothelial cells?
NO activates soluble guanylyl cyclase
Converts GTP → cGMP
cGMP causes smooth muscle relaxation → vasodilation
Overall effect: blood vessel widening + improved blood flow
What decreases or interferes with NO production?
ADMA (Asymmetric Dimethylarginine)
Competes with arginine → NOS uncoupling
Oxidative stress reduces NO availability
Nitrites and nitrates can serve as alternative NO sources (backup system)
How does hemoglobin regulate nitric oxide (NO) signaling (endocrine vs paracrine)?
Hb can bind, carry, release, or inactivate NO depending on oxygenation state.
Oxygenated Hb (HbO₂): bind NO → limits NO availability.
Deoxygenated Hb: release NO-related species (RSNOs) → promote vasodil in tissues that need O2
Hb acts as sensor:
High O₂ → NO trapped (paracrine inhibition)
Low O₂ → NO released to dilate vessels (endocrine-like signaling)
Hb helps match blood flow to metabolic demand by controlling NO activity.
Examples of Nitroprusside and Nitrates
ISDN
ISMN (5-mononitrate)
GTN
sodium nitroprusside
Examples of PDE-5 Inhibitors
Sildenafil, Varenafil, Tadalafil used treat erectile dysfunction (ED)
at high dose: treat pulmonary HT by prolonging NO fx
Endothelin (what is it, what does it promote, what is it produced by, how does it work)
21 aa vasocontrictive peptide with inotropic/chronotropic fx
promotes vascular remodeling by inducing fibrosis
produced by endothelial cells in the vascular wall
action:
preproendothelin proteolytically cleaved
prod big endothelin
endothelins by ECE
acts locally through ETA and ETB receptors (GPCRs)
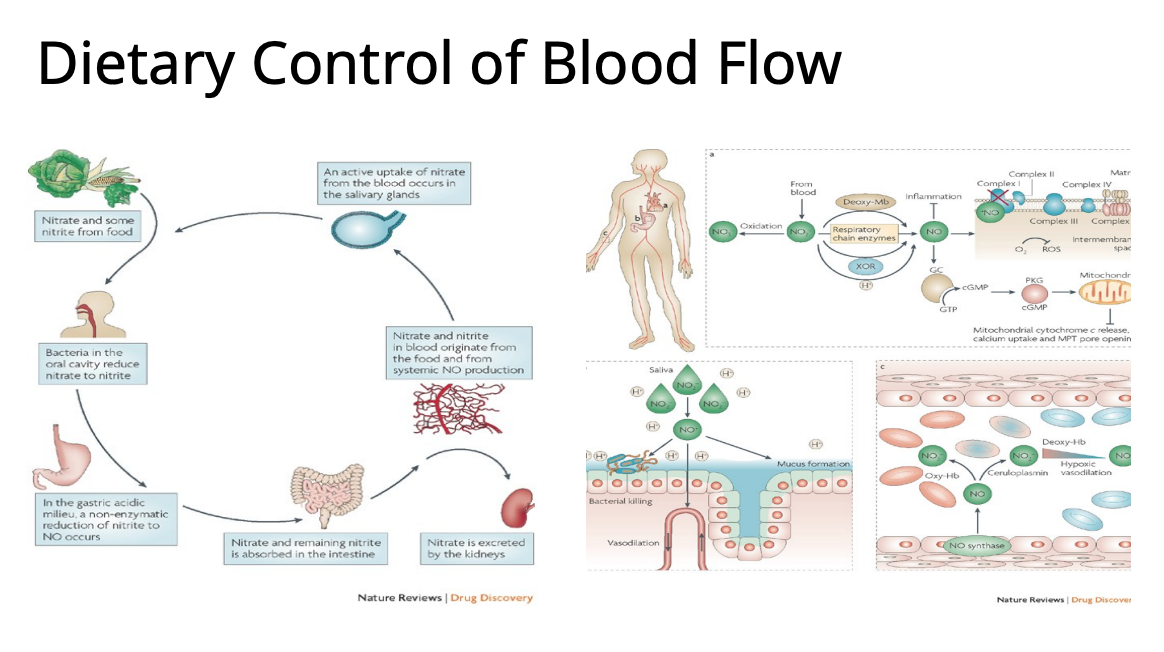
Describe Dietary Control of Blood Flow
Diet Source: leafy greens, veggies
oral bacteria: nitrate → nitrite
stomach enzymes: nitrite → NO
leads to vasodilation, protection in hypoxia, host defense, recycling
What does Beet Juice improve in PAD patients?
Beet juice is rich in nitrates → increase NO in body → vasodilation
improves O2 delivery, enhancing exercise
improves response to claudication time and vascular outcomes