Pathopharmacology Exam #4
0.0(0)
Card Sorting
1/151
Earn XP
Description and Tags
Last updated 2:18 PM on 11/17/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
152 Terms
1
New cards
The circulatory system is composed of...
vessels, fluid, pump
2
New cards
How does blood flow?
from systemic to pulmonary to systemic circulation
3
New cards
5 structures of circulation
arteries (transport blood to the tissues, high pressure system)
arterioles (regulate amount of blood flow to the tissues)
capillaries (exchange of fluid, oxygen, nutrients, hormones and waste products)
venules (collect blood from the capillaries)
veins (transport blood back to the heart, reservoir for blood, low pressure system)
arterioles (regulate amount of blood flow to the tissues)
capillaries (exchange of fluid, oxygen, nutrients, hormones and waste products)
venules (collect blood from the capillaries)
veins (transport blood back to the heart, reservoir for blood, low pressure system)
4
New cards
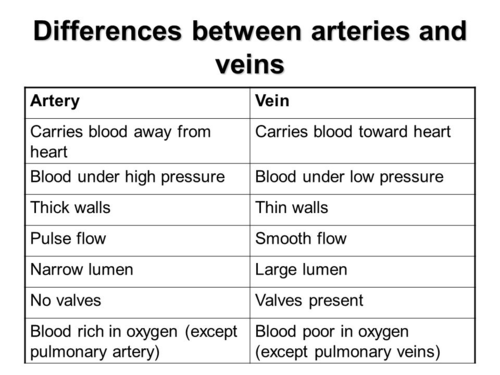
Arteries vs. Veins
-Arteries have *thick walls* to withstand the pressure of blood pumped by the hearts.
-Veins have *walls with a thinner muscle layer and larger lumen.* *valve*
-Veins have *walls with a thinner muscle layer and larger lumen.* *valve*
5
New cards
What does blood flow depend on?
differences between the pressure in the arterial and venous vessels supplying the organ
6
New cards
blood flow resistance
Blood viscosity=thickness
Vessel % of RBCs
length=longer and more resistant
Vessel radium=half diameter
Vessel % of RBCs
length=longer and more resistant
Vessel radium=half diameter
7
New cards
blood flow velocity
velocity decreases as blood moves from the aorta to the capillaries
8
New cards
blood flow vascular compliance
volume the vessel can accommodate for a given increase in pressure
9
New cards
Three facts about the heart (think size, weight, bib)
weighs 1 lb
size of a fist
pumps 2.4 oz of blood per beat
size of a fist
pumps 2.4 oz of blood per beat
10
New cards
Left heart circulatory system
- thick-walled ventricle
- high pressure pump
- receive blood from lungs
- pumps to systemic circulation
- high pressure pump
- receive blood from lungs
- pumps to systemic circulation
11
New cards
Right heart circulatory system
- thin-walled ventricle
- low-pressure pump
- receives blood from the systemic circulation
- pumps to lungs
- low-pressure pump
- receives blood from the systemic circulation
- pumps to lungs
12
New cards
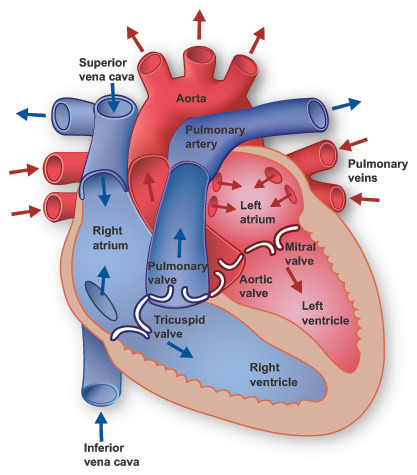
How does blood flow through the heart?
Inferior and superior vena cava (1) dump blood into the right atrium (2)
Right ventricle (3)
2 pulmonary arteries (4) that lead to the lungs (5) where blood becomes oxygenated
Pulmonary veins (6) bring blood from the lungs back to the left atrium (7)
Left ventricle (8) is large and muscular to pump blood into the aorta (9) and to the rest of the body (10)
Eventually blood will be pumped back to each vena cava (1)
Right ventricle (3)
2 pulmonary arteries (4) that lead to the lungs (5) where blood becomes oxygenated
Pulmonary veins (6) bring blood from the lungs back to the left atrium (7)
Left ventricle (8) is large and muscular to pump blood into the aorta (9) and to the rest of the body (10)
Eventually blood will be pumped back to each vena cava (1)
13
New cards
Flow through the chambers of the heart
body-->right atrium-->right ventricle-->lungs-->left atrium--> left ventricle
14
New cards
Anatomy of the heart
refer to picture
15
New cards
Which is the only vein in the body that carries oxygenated blood?
pulmonary veins
16
New cards
Which is the only artery in the body that carries deoxygenated blood?
pulmonary arteries
17
New cards
Layers of the heart wall
pericardium, myocardium, endocardium
18
New cards
Pericardium
- protects against inflammation and infection
- prevents displacement of the heart
- contains pain receptors, elicits changes in BP and heart rate
- prevents displacement of the heart
- contains pain receptors, elicits changes in BP and heart rate
19
New cards
Myocardium
- thickest layer
- cardiac muscle
- cardiac muscle
20
New cards
endocardium
- internal lining of myocardium
- connects with arteries, capillaries, and veins to create continuous closed system
- connects with arteries, capillaries, and veins to create continuous closed system
21
New cards
the cardiac cycle
1. Diastole
- atria fill
- all valves closed
2. Diastole
- increased atrial pressure opens AV valves
- ventricles fill
3. Systole Begins
- atria contract and empty
- ventricles are full
4. Systole
- ventricles begin contraction
- pressure closes AV valves
- atria relax
5. Systole
- ventricles contract
- increased pressure in ventricles
- aortic and pulmonary valves open
- blood ejected into aorta and pulmonary artery
6. Diastole
- ventricles empty
- ventricles relax
- aortic and pulmonary valves close
- atria fill
- all valves closed
2. Diastole
- increased atrial pressure opens AV valves
- ventricles fill
3. Systole Begins
- atria contract and empty
- ventricles are full
4. Systole
- ventricles begin contraction
- pressure closes AV valves
- atria relax
5. Systole
- ventricles contract
- increased pressure in ventricles
- aortic and pulmonary valves open
- blood ejected into aorta and pulmonary artery
6. Diastole
- ventricles empty
- ventricles relax
- aortic and pulmonary valves close
22
New cards
right coronary artery
- Conus: supplies R upper ventricle
- Right Marginal Branch: supplies R ventricle
- Posterior Descending: supplies to smaller branches of both ventricles
- Right Marginal Branch: supplies R ventricle
- Posterior Descending: supplies to smaller branches of both ventricles
23
New cards
left coronary artery
- Left anterior descending artery (LAD): supplies left and right ventricle
- Circumflex artery: supplies left atrium and lateral wall of left ventricle
- Circumflex artery: supplies left atrium and lateral wall of left ventricle
24
New cards
Is coronary blood flow higher during diastole or systole?
Answer: Diastole
*flow is determined by the pressure gradient across the coronary bed*
- diastole: 2/3 resting (filling)
- systole: 1/3 contracting (ejecting)
*flow is determined by the pressure gradient across the coronary bed*
- diastole: 2/3 resting (filling)
- systole: 1/3 contracting (ejecting)
25
New cards
collateral circulation
- normally some arterial anastomoses (connections) exist within the coronary circulation
- when occlusion occurs slowly over time, there's a greater chance of adequate collateral circulation developing
- when occlusion occurs slowly over time, there's a greater chance of adequate collateral circulation developing
26
New cards
What is an occlusion?
closure of a blood vessel due to blockage
27
New cards
myocardial metabolism
cardiac muscle depends on constant production of ATP for energy
energy is used for:
- muscle contraction and relaxation
- electrical excitation
energy is used for:
- muscle contraction and relaxation
- electrical excitation
28
New cards
cardiac output
- volume of blood ejected by ventricle in 1 min (normal for adult is 5L/min)
- cardiac output=heart rate x stroke volume
- others factors determining cardiac output (preload, after load, myocardial contractility)
- cardiac output=heart rate x stroke volume
- others factors determining cardiac output (preload, after load, myocardial contractility)
29
New cards
What is stroke volume?
Amount of blood ejected by the ventricle with EACH CONTRACTION
- applies equally to both ventricles
- important in cardiac output
- correlates with cardiac function
- applies equally to both ventricles
- important in cardiac output
- correlates with cardiac function
30
New cards
How is cardiac output regulated?
extrinsic control (outside the heart)
- autonomic nervous system
- hormones
intrinsic control (inside the heart)
- rhythm and rate
- force of contraction
- end-diastolic volume
- autonomic nervous system
- hormones
intrinsic control (inside the heart)
- rhythm and rate
- force of contraction
- end-diastolic volume
31
New cards
How does sympathetic stimulation regulate the cardiac system?
- increased myocardial contractility
- increased heart rate
- increased venous return
- increased heart rate
- increased venous return
32
New cards
How does parasympathetic stimulation regulate the cardiac system?
- decreased heart rate
33
New cards
How does endocrine responses regulate the cardiac system?
- thyroid hormone
- epinephrine
- epinephrine
34
New cards
Preload
mechanical state of the heart at the end of diastole with the ventricles at their maximum volume
*increased preload increases stroke volume*
factors influencing this:
- the amount of blood entering the ventricle during diastole
- blood left in ventricle after systole
*increased preload increases stroke volume*
factors influencing this:
- the amount of blood entering the ventricle during diastole
- blood left in ventricle after systole
35
New cards
frank sterling law of the heart
The stroke volume of the left ventricle will increase as the left ventricular volume increases due to the myocyte stretch (preload) causing a more forceful systolic contraction
- says the greater the volume of blood within the ventricle the greater the force of contraction
- says the greater the volume of blood within the ventricle the greater the force of contraction
36
New cards
What happens when the heart rate increases?
diastolic filling time is reduced
decreased coronary artery filling
heart has to overcome high pressure in aorta to eject blood (consumers more oxygen)
decreased coronary artery filling
heart has to overcome high pressure in aorta to eject blood (consumers more oxygen)
37
New cards
What increases preload?
-Increased central venous pressure
-Vasoconstriction
-Increased total blood volume
-Decreased heart rate
-Vasoconstriction
-Increased total blood volume
-Decreased heart rate
38
New cards
What decreases preload?
- decreased blood pressure
- decreased blood volume
- gravity (standing upright)
- ventricular diastolic failure (hypertrophy)
- mitral and tricuspid valve stenosis
- decreased blood volume
- gravity (standing upright)
- ventricular diastolic failure (hypertrophy)
- mitral and tricuspid valve stenosis
39
New cards
What is afterload?
Force resistance to eject blood from the ventricles
- determined by peripheral resistance (ex: after load is increased by a high diastolic pressure resulting form excessive vasoconstriction)
- Important determinant of myocardial energy consumption
- determined by peripheral resistance (ex: after load is increased by a high diastolic pressure resulting form excessive vasoconstriction)
- Important determinant of myocardial energy consumption
40
New cards
What increases after load?
aortic and pulmonary valve stenosis
systemic and/or pulmonary hypertension
increased systemic vascular resistance (peripheral vascular resistance)
systemic and/or pulmonary hypertension
increased systemic vascular resistance (peripheral vascular resistance)
41
New cards
Ejection Fraction
Fractions of blood ejected by the left ventricle during systole (calculated by dividing the stroke volume by the end-diastolic volume)
Normal ejection fraction is 60-70%
Increased EF results from sympathetic stimulation
Decreased EF is primary symptom of ventricular failure
Normal ejection fraction is 60-70%
Increased EF results from sympathetic stimulation
Decreased EF is primary symptom of ventricular failure
42
New cards
cardiac reserve
The ability of the heart to increase output in response to increased demand
Components:
- heart rate increases
- stroke volume increases
- cardiac output increases
- oxygen use increases (is supply greater than demand)
Components:
- heart rate increases
- stroke volume increases
- cardiac output increases
- oxygen use increases (is supply greater than demand)
43
New cards
Myocardial Oxygen Supply
Factors that affect supply:
- coronary artery anatomy
- diastolic pressure
- diastolic filling time
- O2 supply vs O2 demand
- coronary artery anatomy
- diastolic pressure
- diastolic filling time
- O2 supply vs O2 demand
44
New cards
What is blood pressure? (diastolic, systolic, MAP)
the pressure in the aorta is caused by the left ventricle as blood is pumped
systolic: arterial pressure during ventricular contraction (affected by stroke volume, aortic stiffness, and ejection velocity)
diastolic: arterial pressure during ventricular relaxation (affected by total peripheral resistance heart rate)
Mean arterial pressure (MAP): average pressure in the arteries during cardiac cycle
systolic: arterial pressure during ventricular contraction (affected by stroke volume, aortic stiffness, and ejection velocity)
diastolic: arterial pressure during ventricular relaxation (affected by total peripheral resistance heart rate)
Mean arterial pressure (MAP): average pressure in the arteries during cardiac cycle
45
New cards
BP ranges (normal, elevated, hypertension stage 1, hypertension stage 2, hypertensive crisis)
normal: 120/80
elevated: 120-129/less than 80
hypertension stage 1: 130-139/80-89
hypertension stage 2: 140 or higher/90 or higher
hypertensive crisis: higher than 180/higher than 120
elevated: 120-129/less than 80
hypertension stage 1: 130-139/80-89
hypertension stage 2: 140 or higher/90 or higher
hypertensive crisis: higher than 180/higher than 120
46
New cards
Baroreceptor control of BP
baroreceptors are stretch receptors in thin areas of blood vessels. send impulses to CV center to regulate blood pressure.
- baroreceptors in aortic walls and carotid arteries
- baroreceptors in aortic walls and carotid arteries
47
New cards
orthostatic hypotension
decrease in both systolic and diastolic pressures with standing
- caused by: immobility, volume loss, medications
- symptoms: dizziness, blurred vision, syncope
- treatment: slow transitions, fluid adjustments, medication
- caused by: immobility, volume loss, medications
- symptoms: dizziness, blurred vision, syncope
- treatment: slow transitions, fluid adjustments, medication
48
New cards
Primary/idiopathic hypertension
Risk factors:
- aging
- male
- African American
- family history
- smoking
- obesity
- stress
- cause of at least 90% of those with HTN
- chronic and progressive
- often no acute symptoms
- sustained BP of great than 140/90 (increased systolic, increase diastole, both)
- aging
- male
- African American
- family history
- smoking
- obesity
- stress
- cause of at least 90% of those with HTN
- chronic and progressive
- often no acute symptoms
- sustained BP of great than 140/90 (increased systolic, increase diastole, both)
49
New cards
Pathology of HTN
- Multi-causal increase in total peripheral resistance
possible defect in sodium excretion
- High metabolic demands of increased body mass
smooth muscle hypertrophy
- Possible defect in sodium excretion
- Smooth muscle hypertrophy
possible defect in sodium excretion
- High metabolic demands of increased body mass
smooth muscle hypertrophy
- Possible defect in sodium excretion
- Smooth muscle hypertrophy
50
New cards
African Americans and HTN
Develop HTN at a younger age
affects women more than men
More aggressive and results in more severe organ damage
Produce less renin (do not respond to renin-inhibiting medication)
- respond better to calcium channel blockers and diuretics
Increased risk of angioedema when taking ACE inhibitors
affects women more than men
More aggressive and results in more severe organ damage
Produce less renin (do not respond to renin-inhibiting medication)
- respond better to calcium channel blockers and diuretics
Increased risk of angioedema when taking ACE inhibitors
51
New cards
Hispanic Americans and HTN
Less likely to receive treatment for HTN
Have lower rates of BP control than Whites and African Americans
Have lower rates of BP control than Whites and African Americans
52
New cards
Gender Differences in HTN
- HTN more common in men before 45 years
- HTN more common in women after 64 years
- HTN is 2-3 times more common in women who take oral contraceptives
- Women (70-79 years) have poorest BP control regardless of treatment
- HTN more common in women after 64 years
- HTN is 2-3 times more common in women who take oral contraceptives
- Women (70-79 years) have poorest BP control regardless of treatment
53
New cards
Secondary HTN
Due to identifiable cause (renal and vascular disease, endocrine disorders)
Possible to treat cause directly
Possible to treat cause directly
54
New cards
Malignant HTN
Rapidly progressing HTN
Diastolic can be greater than 120mm Hg
Diastolic can be greater than 120mm Hg
55
New cards
Treatment of HTN
Lifestyle changes
- stop smoking
- sodium restriction (DASH diet)
- alcohol restriction
- exercise
- weight loss if needed
- proper K and Ca intake
- stop smoking
- sodium restriction (DASH diet)
- alcohol restriction
- exercise
- weight loss if needed
- proper K and Ca intake
56
New cards
Medication that active with RAAS
- angiotensin-converting enzyme inhibitors
- angiotensin II receptor blockers (ARB)
- Direct Renin Inhibitors
- Aldosterone Antagonists
- angiotensin II receptor blockers (ARB)
- Direct Renin Inhibitors
- Aldosterone Antagonists
57
New cards
What does the renin-angiotensin-aldosterone system do?
Regulate BP
Regulate blood volume
Regulate fluid and electrolyte balance
Regulate blood volume
Regulate fluid and electrolyte balance
58
New cards
Order of Renin Angiotensin Aldosterone System
1. drop in BP/fluid volume
2. renin release from kidneys
3. angiotensin from liver
4. renin acts on angiotensin to form angiotensin I
5. ACE release from lungs
6. ACE acts on angiotensin I to form angiotensin II
7. Angiotensin II acts on blood vessels stimulating vasoconstriction
8. Angiotensin II acts on adrenal gland to stimulate release of aldosterone
9. Aldosterone acts on kidneys to stimulate reabsorption of salt and water
2. renin release from kidneys
3. angiotensin from liver
4. renin acts on angiotensin to form angiotensin I
5. ACE release from lungs
6. ACE acts on angiotensin I to form angiotensin II
7. Angiotensin II acts on blood vessels stimulating vasoconstriction
8. Angiotensin II acts on adrenal gland to stimulate release of aldosterone
9. Aldosterone acts on kidneys to stimulate reabsorption of salt and water
59
New cards
angiotensin converting enzyme (ACE)
Mechanism of action: reduces levels of angiotensin II (vasodilation, decreased blood volume/cardiac and vascular remodeling, potassium retention, fetal injury) AND increases levels of bradykinin (vasodilation, cough, angioedema)
Pharmacokinetics: administered orally, converted to the active form in the liver, excreted by the kidney
Adverse effects: persistent dry irritating nonproductive cough, hyperkalemia, renal failure, angioedema, fetal injury during the 2/3 trimester
Pharmacokinetics: administered orally, converted to the active form in the liver, excreted by the kidney
Adverse effects: persistent dry irritating nonproductive cough, hyperkalemia, renal failure, angioedema, fetal injury during the 2/3 trimester
60
New cards
Common ACE inhibitors
end in "pril"
lisinopril
captopril
enalapril
ramipril
lisinopril
captopril
enalapril
ramipril
61
New cards
Angiotensin II Receptor Blockers (ARBs)
Mechanism of action:
- blocks access of angiotensin II to receptors in blood vessels
- prevent angiotensin II from inducing pathologic changes in cardiac structure
- cause dilation of arterioles and veins
- reduce excretion of potassium
- decrease release of aldosterone
- increase renal excretion of sodium and water
*avoid use due to FETAL HARM*
Pharmacokinetics: metabolized in liver AND excreted by kidneys
Adverse effects: dizziness, hypotension, hyperkalemia, increase in BUN/Cr, angioedema
Note: do not inhibit Kinase II or increase bradykinin (reduce risk of developing cough/angioedema in comparison to ACE-I)
- blocks access of angiotensin II to receptors in blood vessels
- prevent angiotensin II from inducing pathologic changes in cardiac structure
- cause dilation of arterioles and veins
- reduce excretion of potassium
- decrease release of aldosterone
- increase renal excretion of sodium and water
*avoid use due to FETAL HARM*
Pharmacokinetics: metabolized in liver AND excreted by kidneys
Adverse effects: dizziness, hypotension, hyperkalemia, increase in BUN/Cr, angioedema
Note: do not inhibit Kinase II or increase bradykinin (reduce risk of developing cough/angioedema in comparison to ACE-I)
62
New cards
Common ARBs
End in "sartan"
Losartan
Valsartan
Candesartan
Losartan
Valsartan
Candesartan
63
New cards
Direct Renin Inhibitors (DRIs) - Aliskiren
Mechanism of action: binds tightly with renin and inhibits cleavage of angiotensinogen into angiotensin I
Administered Orally (bioavailability is decreased when administered with high-fat meal)
Excreted by kidney
Side effects: angioedema, cough, diarrhea, hyperkalemia, fetal injury/death
Administered Orally (bioavailability is decreased when administered with high-fat meal)
Excreted by kidney
Side effects: angioedema, cough, diarrhea, hyperkalemia, fetal injury/death
64
New cards
Aldosterone Antagonists
Used to treat hypertension AND heart failure
Mechanism of action: blocks receptors for aldosterone in kidney AND promotes retention of potassium/excretion of salt + water
Side effects: hyperkalemia
Pharmacokinetics: absorption is not affected by food
Mechanism of action: blocks receptors for aldosterone in kidney AND promotes retention of potassium/excretion of salt + water
Side effects: hyperkalemia
Pharmacokinetics: absorption is not affected by food
65
New cards
Common Aldosterone Antagonists
Spironolactone: older drug - causes more side effects, binds with receptors for other steroid hormones
Eplerenone: selective aldosterone receptor blocker, less selective - has fewer side effects than spironolactone
Eplerenone: selective aldosterone receptor blocker, less selective - has fewer side effects than spironolactone
66
New cards
Vasodilators
Reduce peripheral resistance systemically (reducing workload of heart by dilating veins/arteries)
- this leads to better balance of O2 supply and demand in the heart muscle
- wide variety of therapeutic applications
adverse effects: postural hypotension, reflex tachycardia, expansion of blood volume
- this leads to better balance of O2 supply and demand in the heart muscle
- wide variety of therapeutic applications
adverse effects: postural hypotension, reflex tachycardia, expansion of blood volume
67
New cards
Common vasodilators
- Hydralazine
- Sodium Nitroprusside
- Sodium Nitroprusside
68
New cards
Hydralazine:
- selective dilation of arterioles (decreases after load)
- mechanism of action unknown
- postural hypertension is minimal
therapeutic uses (essential hypertension, hypertensive crisis, heart failure)
adverse effects: reflex tachycardia, increased blood volume, systemic lupus redness, headache
drug interactions: avoid excessive hypotension (so antihypertensive agents), combined with beta blocker
- mechanism of action unknown
- postural hypertension is minimal
therapeutic uses (essential hypertension, hypertensive crisis, heart failure)
adverse effects: reflex tachycardia, increased blood volume, systemic lupus redness, headache
drug interactions: avoid excessive hypotension (so antihypertensive agents), combined with beta blocker
69
New cards
Sodium Nitroprusside
- fast acting antihypertensive agent
- causes venous and arteriolar dilation
- administration: IV infusion
- Onset: immediate (BP returns to pretreatment level in minutes when stopped)
- used for hypertensive emergencies
Adverse Effects: excessive hypotension, cyanide poisoning, thiocyanate toxicity when used for more than three days (disorientation, psychosis, delirium)
- causes venous and arteriolar dilation
- administration: IV infusion
- Onset: immediate (BP returns to pretreatment level in minutes when stopped)
- used for hypertensive emergencies
Adverse Effects: excessive hypotension, cyanide poisoning, thiocyanate toxicity when used for more than three days (disorientation, psychosis, delirium)
70
New cards
What is heart failure?
Heart failure is the inability of the heart to pump sufficient blood to meet the needs for oxygen and nutrients.
- ventricular dysfunction
- reduced cardiac output
- insufficient tissue perfusion
- fluid retention
Symptoms:
- edema and weight gain secondary to fluid retention
- tachycardia
- increased heart size on chest x-ray
- oliguria due to decreased renal perfusion
- ventricular dysfunction
- reduced cardiac output
- insufficient tissue perfusion
- fluid retention
Symptoms:
- edema and weight gain secondary to fluid retention
- tachycardia
- increased heart size on chest x-ray
- oliguria due to decreased renal perfusion
71
New cards
Etiology of Heart Failure
inadequate tissue perfusion, volume overload, chronic hypertension, MI, valvular heart disease, coronary artery disease, congenital heart disease, dysrhythmias, aging of the myocardium
72
New cards
Physiologic changes Cardiac Remodeling
ventricular dilation, ventricular wall hypertrophy, reduced left ventricular EF, increased sympathetic tone through activation of baroreceptors
- increased HR, contractility, myocardial O2 demand
- increased venous return
- increased arterial tone
- increased HR, contractility, myocardial O2 demand
- increased venous return
- increased arterial tone
73
New cards
What does left sided heart failure look like?
- paroxysmal nocturnal dyspnea
- elevated pulmonary capillary wedge pressure
- pulmonary congestion (cough, crackles, wheezes, blood-tinged sputum, tachypnea)
- restlessness
- confusion
- exertion dyspnea
- fatigue
- cyanosis
- elevated pulmonary capillary wedge pressure
- pulmonary congestion (cough, crackles, wheezes, blood-tinged sputum, tachypnea)
- restlessness
- confusion
- exertion dyspnea
- fatigue
- cyanosis
74
New cards
What does right sided heart failure look like?
- fatigue
- increased peripheral venous pressure
- ascites
- enlarged liver/spleen
- may be secondary to chronic pulmonary problems
- distended jugular viens
- anorexia/complaints of GI distress
- weight gain
- dependent edema
- increased peripheral venous pressure
- ascites
- enlarged liver/spleen
- may be secondary to chronic pulmonary problems
- distended jugular viens
- anorexia/complaints of GI distress
- weight gain
- dependent edema
75
New cards
Role of Natriuretic Peptides
stretching of atria and dilation of ventricles stimulates release of ANP and BNP
- promotes dilation of arteries/viens
- promotes loss of salt/water through kidney
- counteracts effect of RAAS
as heart failure progresses, effects of ANP/BNP become overwhelmed by RAAS
- measurement of circulating BNP is important indicator of cardiac status in heart failure patients
- high levels of BNP indicate poor chance of survival
- Normal BNP levels < 100 pictograms/mL
- promotes dilation of arteries/viens
- promotes loss of salt/water through kidney
- counteracts effect of RAAS
as heart failure progresses, effects of ANP/BNP become overwhelmed by RAAS
- measurement of circulating BNP is important indicator of cardiac status in heart failure patients
- high levels of BNP indicate poor chance of survival
- Normal BNP levels < 100 pictograms/mL
76
New cards
Cycle of cardiac compensatory responses
cardiac remodeling --> reduced cardiac output --> compensatory responses (cardiac dilation, activation of sympathetic nervous system + renin-angiotensin-aldosterone system, retention of water and increased blood volume) --> (increased HR Venous Pressure Arterial Pressure) -->
77
New cards
cardiac conduction system
the ability of the heart to pump occurs as a result of electrical stimulation to cardiac cells
- the electrical activity of the heart causes contraction and blood flow
cardiac tissue properties determine the generation and transmission of electrical impulses
- it is possible to have electrical activity without the heart pumping
- the electrical activity of the heart causes contraction and blood flow
cardiac tissue properties determine the generation and transmission of electrical impulses
- it is possible to have electrical activity without the heart pumping
78
New cards
properties of cardiac tissue
automaticity: ability to initiate an impulse
- cells act as a syncytium (work as one, only cardiac cells have this ability)
- spontaneous depolarization of resting cell membrane
conductivity: ability for impulse to move along membrane in orderly manner
- spreads from cell to cell at the same time
excitability: ability to be electrically stimulated
contractility: ability to respond mechanically to an impulse
- determined by how much the muscle fibers are stretched at end of diastole
- cells act as a syncytium (work as one, only cardiac cells have this ability)
- spontaneous depolarization of resting cell membrane
conductivity: ability for impulse to move along membrane in orderly manner
- spreads from cell to cell at the same time
excitability: ability to be electrically stimulated
contractility: ability to respond mechanically to an impulse
- determined by how much the muscle fibers are stretched at end of diastole
79
New cards
The polarized state of the heart is
No electrical activity takes place
the cell is ready to accept a stimulus
- intracellular ion = potassium
- extracellular ion = sodium and calcium
the cell is ready to accept a stimulus
- intracellular ion = potassium
- extracellular ion = sodium and calcium
80
New cards
The depolarized state of the heart is
sodium and calcium move into cell
potassium moves out of the cell
potassium moves out of the cell
81
New cards
The repolarized state of the heart is
potassium moves into the cell
calcium and sodium move out of the cell
calcium and sodium move out of the cell
82
New cards
sinoartrial node (SA node)
located in the upper right corner of the right atrium where the superior vena cava joins the atrium
- hearts pacemaker
- generates impulses 60-100 times per minute
- hearts pacemaker
- generates impulses 60-100 times per minute
83
New cards
atrioventricular (AV) node
located in the floor of the right atrium
responsible for delaying impulses for 0.04 seconds
prevents the ventricle from contracting quickly
allows cardiac muscle to stretch to fullest peak (starlings law)
responsible for delaying impulses for 0.04 seconds
prevents the ventricle from contracting quickly
allows cardiac muscle to stretch to fullest peak (starlings law)
84
New cards
Bundle of His (AV bundle)
tract of tissues that extends into ventricles next to septum
promotes rapid impulse conduction through ventricle
impulse travels faster down the left than the right (supplies left ventricle)
permits both ventricles to contract simultaneously
promotes rapid impulse conduction through ventricle
impulse travels faster down the left than the right (supplies left ventricle)
permits both ventricles to contract simultaneously
85
New cards
Purkinje fibers
extends from bundle of His into endocardium
conducts impulses rapidly through muscle to assist with depolarization/contraction
conducts impulses rapidly through muscle to assist with depolarization/contraction
86
New cards
What is cardiac action potential?
waves of depolarization followed by repolarization
generated by movement of ions
ion fluctuation is related to channels in cell membrane
two types of action potential channels (fast and slow)
generated by movement of ions
ion fluctuation is related to channels in cell membrane
two types of action potential channels (fast and slow)
87
New cards
fast channels
Phase 0 (rapid depolarization, influx Na ions, speed of phase 0 determines velocity)
Phase 1 (rapid partial repolarization, Medications do not affect this)
Phase 2 (Ca enters cell, medications that act on this phase reduce myocardial contractility)
Phase 3 (potassium leaves cell, repolarization is delayed by drugs that block potassium channels)
Phase 4 (gives cardiac cells automaticity, 2 types of electrical activity possible: membrane potential remains stable, membrane goes through spontaneous depolarization)
Phase 1 (rapid partial repolarization, Medications do not affect this)
Phase 2 (Ca enters cell, medications that act on this phase reduce myocardial contractility)
Phase 3 (potassium leaves cell, repolarization is delayed by drugs that block potassium channels)
Phase 4 (gives cardiac cells automaticity, 2 types of electrical activity possible: membrane potential remains stable, membrane goes through spontaneous depolarization)
88
New cards
Slow channels
Phase 0 (slow influx of Ca, rate of depolarization is slow)
Phase 1 (slow channels lack a Phase 1)
Phase 2/3 (medication do not affect)
Phase 4 (Sa/Av node depolarization, Sa depolarizes quick, determines HR)
Phase 1 (slow channels lack a Phase 1)
Phase 2/3 (medication do not affect)
Phase 4 (Sa/Av node depolarization, Sa depolarizes quick, determines HR)
89
New cards
Electrocardiogram
Graphic display of the electrical forces generated by the heart
- records electrical impulses from the surface of the body on graph paper
- used to diagnose
Major components of an ECG:
- p wave (depolarization in atria)
- QRS complex (depolarization of the ventricles)
- T wave (repolarization of ventricles)
(PR interval, QT interval, ST segement)
- records electrical impulses from the surface of the body on graph paper
- used to diagnose
Major components of an ECG:
- p wave (depolarization in atria)
- QRS complex (depolarization of the ventricles)
- T wave (repolarization of ventricles)
(PR interval, QT interval, ST segement)
90
New cards
How does an impulse travel through the cardiac conduction system?
An impulse normally is generated in the sinus node and travels through the atria to the AV node, down the bundle of His and Purkinje fibers, and to the ventricular myocardium
91
New cards
ECG Deflections
P wave - atrial depolarization, SA node fire
QRS complex - ventricular depolarization ventricles contract
T wave - ventricular repolarization
P-R interval - tramission of impulse from Sa to Av node
S-T segment - end of ventricular depolarization and beginning of repolarization reflects ischemia, cardiac injury, potassium abnormalities
Q-T interval - used to measure the effect of cardiac measurements
QRS complex - ventricular depolarization ventricles contract
T wave - ventricular repolarization
P-R interval - tramission of impulse from Sa to Av node
S-T segment - end of ventricular depolarization and beginning of repolarization reflects ischemia, cardiac injury, potassium abnormalities
Q-T interval - used to measure the effect of cardiac measurements
92
New cards
dysrhythmia
Abnormal heart rhythm
- arises from impulse formation disturbances
- tachydysrhythmias: supraventricular (SVT) and ventricular
- virtually all drugs that treat dysrhythmias can also cause them
- arises from impulse formation disturbances
- tachydysrhythmias: supraventricular (SVT) and ventricular
- virtually all drugs that treat dysrhythmias can also cause them
93
New cards
Generation of dysrhythmias is when
One or both of the following situations occurs:
• Disturbed impulse formation or automaticity
• Disturbed impulse conduction (AV block, Reentry)
• Disturbed impulse formation or automaticity
• Disturbed impulse conduction (AV block, Reentry)
94
New cards
Principles of Antidysrhythmic Drug Therapy
-Balancing risks and benefits
•Consider properties of dysrhythmias:
*Sustained vs. nonsustained
*Asymptomatic vs. symptomatic
*Supraventricular vs. ventricular
-Acute and long-term treatment phases
-Minimizing risk
•Consider properties of dysrhythmias:
*Sustained vs. nonsustained
*Asymptomatic vs. symptomatic
*Supraventricular vs. ventricular
-Acute and long-term treatment phases
-Minimizing risk
95
New cards
Classification of antidysrhythmic drugs
Vaughan Williams classification
Class I: sodium channel blockers
Class II: beta blockers
Class III: potassium channel blockers
Class IV: calcium channel blockers
Other: adenosine, digoxin, and ibutilide
Class I: sodium channel blockers
Class II: beta blockers
Class III: potassium channel blockers
Class IV: calcium channel blockers
Other: adenosine, digoxin, and ibutilide
96
New cards
Class 1A agents
Quinidine
Procainamide
effects on the heart
- blocks sodium channels
- slows impulse conduction
- delays repolarization
- blocks vagal input to the heart
effects on the ECG
- widens QRS complex
- Prolongs the QT interval
therapeutic uses
- supra ventricular and ventricular dysrhythmias
adverse effects
- diarrhea (33%)
- cinchonism (ringing in ears, nausea, vertigo)
- cardiotoxicity (reduced conduction throughout the heart)
- arterial embolism
- hypotension
drug interactions
- digoxin
Procainamide
effects on the heart
- blocks sodium channels
- slows impulse conduction
- delays repolarization
- blocks vagal input to the heart
effects on the ECG
- widens QRS complex
- Prolongs the QT interval
therapeutic uses
- supra ventricular and ventricular dysrhythmias
adverse effects
- diarrhea (33%)
- cinchonism (ringing in ears, nausea, vertigo)
- cardiotoxicity (reduced conduction throughout the heart)
- arterial embolism
- hypotension
drug interactions
- digoxin
97
New cards
Class 1B agents
Lidocaine
effect on heart and ECG
- blocks cardiac sodium channels
- reduces automaticity in ventricles and his-purkinje system
- accelerates repolarization
- primary works on ventricular dysrhythmias
adverse effects - CNS effects
- drowsiness
- confusion
- paresthesias
effect on heart and ECG
- blocks cardiac sodium channels
- reduces automaticity in ventricles and his-purkinje system
- accelerates repolarization
- primary works on ventricular dysrhythmias
adverse effects - CNS effects
- drowsiness
- confusion
- paresthesias
98
New cards
Class 1C agents
Flecainide
Propafenone
delay ventricular repolarization
decrease cardiac conduction
all class 1C agents can exacerbate existing dysrthymias and create new ones
Propafenone
delay ventricular repolarization
decrease cardiac conduction
all class 1C agents can exacerbate existing dysrthymias and create new ones
99
New cards
Class 2 beta blockers
Beta-adrenergic blocking agents
Four approved to treat dysrhythmias:
- Propranolol
- Acebutolol
- Esmolol
_ Sotalol
Nonselective beta-adnergic antagonist
effects on heart and ECG
- decrease automaticity of the SA node
- decreased velocity of conduction through Av node
- decreased myocardial contractility
Therapeutic use
- dysrhythmias caused by excessive sympathetic stimulation
adverse effects
- heart block
- heart failure
- Av block
- Sinus arrest
- hypotension
- bronchospasm (in asthma patients)
Four approved to treat dysrhythmias:
- Propranolol
- Acebutolol
- Esmolol
_ Sotalol
Nonselective beta-adnergic antagonist
effects on heart and ECG
- decrease automaticity of the SA node
- decreased velocity of conduction through Av node
- decreased myocardial contractility
Therapeutic use
- dysrhythmias caused by excessive sympathetic stimulation
adverse effects
- heart block
- heart failure
- Av block
- Sinus arrest
- hypotension
- bronchospasm (in asthma patients)
100
New cards
Class 3 agents
channel blockers: Amiodarone
- can be increased by grapefruit juice
- can be reduced by cholestyramine
- risk of severe dysrhythmias increased by diuretics
- combining with a beta blocker can lead to excessive slowing of the heart
therapeutic use
- for life-threatening ventricular dysrhythmias only
- recurrent ventricular fibrillation
- recurrent hemodynamically unstable ventricular tachycardia
effects on the heart and ECG
- reduced automaticity in the SA Node
- Reduced contractility
- reduced conduction velocity
- QRS widening
- prolongation of the PR and QT intervals
drug interactions (increases levels)
- quinidine
- diltiazem
- warfarin
- digoxin
adverse effects
- protracted half-life
- pulmonary toxicity
- cardiotoxicity
- toxicity in pregnancy and breast-feeding
- optic neuropathy
adverse effects
- bradycardia
- hypotension
- heart block
- peripheral edema
- constipation
- can elevate digoxin levels
- increased risk when combined with a beta blocker
- can be increased by grapefruit juice
- can be reduced by cholestyramine
- risk of severe dysrhythmias increased by diuretics
- combining with a beta blocker can lead to excessive slowing of the heart
therapeutic use
- for life-threatening ventricular dysrhythmias only
- recurrent ventricular fibrillation
- recurrent hemodynamically unstable ventricular tachycardia
effects on the heart and ECG
- reduced automaticity in the SA Node
- Reduced contractility
- reduced conduction velocity
- QRS widening
- prolongation of the PR and QT intervals
drug interactions (increases levels)
- quinidine
- diltiazem
- warfarin
- digoxin
adverse effects
- protracted half-life
- pulmonary toxicity
- cardiotoxicity
- toxicity in pregnancy and breast-feeding
- optic neuropathy
adverse effects
- bradycardia
- hypotension
- heart block
- peripheral edema
- constipation
- can elevate digoxin levels
- increased risk when combined with a beta blocker