GEOG 3692 exam 2
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
know the four dimensions and determinants of food security
availability-
domestic production
import capacity
food stocks
food aid
accessibility-
income, own production, power to purchase
food distribution
transport + market infrastructure
utilization-
food safety + quality
clean water
health/ sanitation
care, feeding, and health practices
stability-
weather, seasonality, variability
price fluctuations
political factors
economic factors
food access determinants: income, food distribution, paved roads, NOT FOOD AID
understand the purpose of the most common key indicators to analyze and determine household food security
FEWSNET: phase classification system for food security crises based on a range of livelihood needs
FbF: anticipatory mechanism to enable access to funding before a disaster occurs through impact- based forecasts
FCS: indicator for current food utilization using dietary diversity, food frequency, and nutritional importance as indicators
CSI: developed by WFP+CARE to assess frequency/ severity of different coping strategies in response to food insecurity (increased score= greater insecurity)
→ country typed: based on context-specific strategies + severity scores to measure severe behaviors
→ reduced CSI: measures several common, less severcoping behaviors + allows comparison among areas and countries
HFIAS: developed by USAID which measures what people do when they cannot access food → uses 9 questions to ask people’s feelings on uncertainty or anxiety related to food supply)
MUAC: provides assessment for chronic, nutritional status over time by measuring circumference of mid arm of individuals compared against a standard to establish prevalence of malnutrition
know the benefits and drawbacks to these food security indicators
benefits:
FCS- uses dietary diversity, food frequency, and nutritional importance to determine food utilization
CSI-assesses frequency and severity of coping strategies in response to food insecurity
HFIAS-measures what people do when they cannot access food
drawbacks:
inaccurate representation: may occur if researchers misunderstand indicators of combinations to measure food security
under-coverage bias:data collection overlooks the essential worker experiences, unhoused individuals, as well as migrants/ refugees
differing growth trajectories: nomadic/ pastoralists grow more slowly than western counterparts, so they do not achieve height/weight norms set by the WHO
standardization: MUAC requires standardized set of measurements to determine malnourishment, which may not even exist in certain settings
what coping strategies did the qualitative participant observation and interviews identify to deal with food insecurity in the Papua new guinea highlands?
-store loans as a short term strategy
- migration as a long-term strategy
( high altitude dwellers migrate to lower-altitude food secure areas)
some drivers of food insecurity: poverty, inequality, poor infrastructure, low state capacity, low agricultural productivity
in the focus groups, what are everyday fears of food insecurity that wage locals discussed?
fears mentioned
the frost destroyed vegetation, so one of the greatest fears discussed was dying (especially for the men)
Women were concerned about dying, but were more concerned for their families and children going to bed hungry at night
what does a “horizontal” approach mean? how were rural doctors of India and the “barefoot doctors” of the people’s republic of china examples of a horizontal approach to medicine?
Horizontal approach- comprehensive solutions, like primary healthcare that don’t have a quick fix for tackling diseases
—> these doctors are an example of the horizontal approach because they showed the strengths of community based medicine and integrating biomedical services and drawing on community participation to deliver care (combined western + local medicine practices to demonstrate that healthcare services are deliverable at low costs by encouraging the community’s participation)
why wasn’t the grand vision of “healthcare for all” that was promoted in the Alma Ata ever realized?
because of the sovereign debt crisis in 1980s that left developing countries unable to provide comprehensive local services, and it dried up he international development aid, making “healthcare for all” unattainable and unrealistic
compare and contrast primary health care (PHC) and selective primary health care (SPHC) in regard to their approaches to health care and in practical terms for the health services provided under each approach?
1) philosophical approaches to healthcare:
primary health care- “health by the people” —> attended to the basic needs with handling health services simultaneously
selective primary healthcare- offers a high return in lives saved per dollar spent (effective altruism)
2) practical terms:
primary health care- encourage community participation by delivering basic health care services at low costs —> “healthcare equality for all”
selective primary healthcare-
measles + DPT vaccinations
malaria treatment and therapy
promotion of breast feeding
what are structural adjustment programs by the IMF? what types of reforms do they require?
programs that provide countries with loans in exchange for wide-ranging reforms, to shape their political, economic, fiscal, and administrative parameters with which policies are developed
cut government spending on social programs such as health/education
had to open economies to free trade
led to privatization (selling state assets)
—>reforms: requires removing labor market regulations in all these parameters, which impacts health (countries had to liberalize and deregulate their economies)
how do structural adjustment programs impact health system access and neonatal mortality?
the impact was that market- oriented policies mandated by the IMF worsen health system access and increase neonatal mortality in borrowing countries, which can be explained by the labor market reforms (causes deleterious effects on health equity)
For the world bank, world health organization and UNICEF, know: the mission of the organization, their approaches/ known programs and critiques
world bank:
mission - end extreme poverty by promoting shared prosperity in a sustainable way
approaches and known programs - provides loans to developing countries (12,000 projects) and focused aid on education and health —> health as a human right rather than as cost-effectiveness
critiques -
governed the wealthiest countries and represents their interests
SAPs often negatively impact underserved, struggling countries
World Health Organization:
mission - attainment by all people of the highest level of health
approaches and known programs - member states vote in world health assembly (one country, one vote)
-funded by dues from member states and private donations
- in practice: doesn’t provide health services, but develops guidelines, convenes experts, provides expertise, and leads major public health campaigns
critiques - inflexible to local circumstances: voluntary donors now decide financial priorities more than the assembly
UNICEF:
mission - advocation for the protection of children’s rights + meet their basic needs
approaches and known programs - focuses on childhood and maternal nutrition to promote education/ sanitation
- provides emergency relief in response to disasters and was involved in getting days of tranquility for national immunization days
-Immunization successes with many global health actors involved(met many of its targets)
critiques - GOBI-FFF didn’t achieve goal of primary healthcare for all (only focused on O/I of GOBI)
- GOBI did not offer global health solutions, but was only offered temporary/ technical fixes as band-aids rather than sustainable solutions
know what each of the following approaches are: primary health care (PHC) and selective primary health care (SPHC)
PHC: access to basic care + equitable distribution of resources (local participation to achieve health that enables productive lives)
oriented towards goal of global health equity
avoided many problems of top-down, vertical programs
emphasized systems building
SPHC: focuses on prevention of diseases with the highest mortality and morbidity rates for effective interventions
still a top-down, vertical program
not a participatory or engaging sector outside of health goals because there was nor a plan for meeting the healthcare needs of WHOLE populations
know what the alma Ata and the Bellagio conferences relate to global health (who was there, what key message espouse, how they differed)
Alma Ata:
was attended by UN member countries and espoused primary healthcare as the key to achieving the goal of health for all in 1978
Bellagio:
was attended by just the wealthiest countries and espoused selective primary healthcare for their interim strategy to put forward in 1979
know the basis about GOBI-FFF (unicef’s SPHC strategy)
-saw Selective primary healthcare as politically realistic with measurable, time-bound targets with scarce resources
GOBI-FFF: represented a more vertical, top down approach
growth monitoring
oral rehydration therapy (ORT)
breastfeeding
immunizations
food supplementation
female literacy
family planning
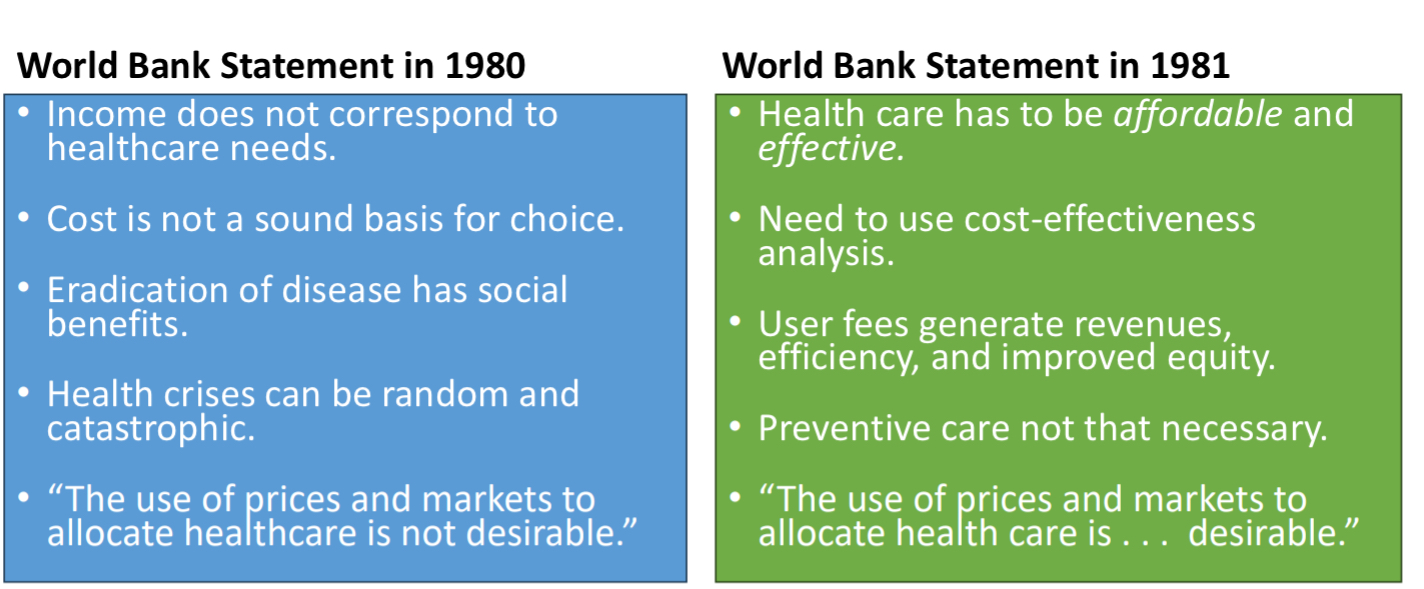
be able to articulate how neoliberalism impacted public health starting in the 1980s
this brought emphasis on free markets with no government involvement
health was seen as a commodity that should be delivered within a market context (rather than a human right for all)
IMF and World Bank directors were appointed with neoliberal orientations in 1980s implemented by Reagan and Thatcher policies in the 1980s
emphasis on private sector and fees for service by the World Bank
what single source provided the most DAH in 2021 (26.21% of spending)? what is the second biggest source (20.81% of spending)?
single source: United States (26.21% )
second biggest source: Other sources (20.81%) like development banks/ GAVI/ UN
what is the percentage of total DAH funding that went to debt repayments in 2021?
the percent of total DAH from funding that went to debt repayments in 2021 was 70.42%
Debt repayment
money spent by developing countries to pay back loans to the world bank and IMF
is the US funding DAH more or less in 2021 than 1990? during what time period did DAH funding by the U.S. start to increase for HIV?
the US is funding more in 2021 than 1990. The HIV funding increased above $1B in 2001-2002, and it passed $5B in 2009-2010.
how was the funding by the U.S. though the WHO+ UN agencies changed over time? How was funding for DAH from the U.S. through NGOs changed over time? what about through the global fund and Gavi?
WHO/UN agencies-funding has significantly decreased by about 50%, but the UN funding is still steadily increasing
NGOs- rapidly increased from 1990-2010, but has been pretty steady around 4.5-4.6 billion since then
Global Fund + Gavi- global fund is increasing exponentially while GAVI was only founded in 2002, and has only slowly increased since then
what percent of DAH in 2021 was spent on SWAP & HSS? what percent was spent on non-communicable diseases? what percent was spent on infectious diseases combined (HIV/AIDS, Malaria, other infectious diseases, and tuberculosis)?
the percent of DAH spent on SWAPs + HSS in 2021 was 10.6%
the percent spent on non-communicable diseases was 1.60%
the percent spent on HIV, Malaria, TB, and other infections combined was 54.15%
know how the funding structure of global health aid has shifted and impacts of these changes
the classic institutions for funding used to be WHO and the World Bank but now includes Global Fund to fight AIDS, TB, and Malaria and the Gavi (vaccine alliance)
WHO is shifting the countries which are donated to, as well as initiatives to fund specifically (no longer just one country, one vote but different sources are funding targeted issues as a more wholistic approach by fixing it from the inside out (COVID shifted the double burden of infectious diseases/ non-communicable diseases)
impacts:
consolidation of influence in global health actors: impose priorities of powerful donors on low-income countries with little input
towards more discretionary funding and away from long-term funding
defined multi-stakeholder governance and way from traditional government-centered representation and decision making: possible increase in global health funding
towards narrower mandates or problem-focused vertical initiatives- underinvestment in public health capacities like surveillance, education campaigns, health systems strengthening
know the strengths and critiques of the role of NGOs in global health
strengths:
seen as government alternative- third sector/ private sector of civil society
more efficient
donors minimize government involvement
vehicle of democratization
in the absence of state, NGOs fill the population vacuum
innovative and cost effective in delivery service
greater ability to target impoverished + develop community- based institutions
better able to promote participation
critiques:
dependent on donor money and tied to the policies of donor states
patron-client relationship: subordinate to donor goals
lack of accountability to local populations in country of region
payment = “ participation”
not often innovative, but rather recycles donor ideas
does not always reach the actual impoverished individuals
democratization: top- down approach where participation is often misused —> means getting the community to agree
understand the origins, similarities, and differences between the ICRC and MSF
Similarities-
both emerged to respond to conflict conditions
respond to suffering in health framework (not hunger or poverty)
provide health care and humanitarian aid in conflict (often work together)
they often work together throughout their global health
Differences-
vary on principles of neutrality, impartiality, confidentiality and independence
independence:
MSF- set up medical services ASAP, even if illegal
ICRC- works with legal authorities to set up medical services
denouncing or speaking up= denouncing inhibits access to local patients, but at some point silence is equal to group complicity in adverse situations
what is the overarching objective of the millenium development goals?
committed nations to a new global partnership to reduce extreme poverty
focus on achievable, sustainable, and multi-sectional action + development
know what four crises currently threaten sustainable development goals’ progress
climate crisis
conflicts/ wars
gloomy global economy outlook
lingering COVID-19 effects
why are our traditional approaches to malaria (top-down/ technical fixes) becoming less effective?
malaria spreads through mosquitos, and this top-down approach is no longer effective because the economic costs that this disease is causing is no longer working
( it is one of the most deadly diseases, so the burden of disease will only continue to increase)
how is ‘steve’ the mosquito so adaptable with breeding/ feeding?
the mosquito is adaptable because it breeds all year round rather than having a malaria season
very competent vector: really easy to transmit malaria through its bites
steve is great at high temperatures and also when it is dry
malaria was once a rural disease, but steve made it more urbanized in africa
this species has rapidly adapted to live, feed, and breed in new environments and resist insecticides
what is a vertical health program? know some critiques and benefits
critiques
limited to local output, which is not looking at the social or health policy determinants that cause the high rates of disease
Benefits
minimizes/ eliminates threat of a given disease in a population
can led to benefits for co-morbidities
leads to health infrastructure improvements
easier to get funding for initiatives that are focused on one disease with a clear, technical fix
herd immunity
the concept when very few people can carry a disease, so the virus cannot find a host so the disease will not spread in that population
successes and failures of vaccine campaigns globally, including the impact of COVID-19
successes:
vaccination rates increased in treatment states compared to non-treatment states
more pro-vaccination social norms at one time are associated with higher vaccination rates at a later time point
failures:
there was a lot of misinformation shared by people who did not intend to mislead others, which led to anti vaccine content
vaccine hesitancy and societal norms related to this were important factors in promoting COVID vaccination routines in Nigeria
understand the characteristics of a disease that may help make an eradication campaign successful (or unsuccessful)
transmission: direct human-to-human contact
recurrence: permanent immunity from a single infection or vaccination
latency(time between exposure and symptoms): short and known latency period of 7-14 days
case-identification: infectious is obvious(distinctive rash)
prevention: vaccine is extremely effective and didn’t require a cold chain (temperature-controlled environments)
compare and contrast smallpox, malaria, and polio eradication efforts
smallpox:
transmission: direct human- to human contact
recurrence: permanent immunity from a single infection or vaccination
latency: short and known latency period of 7-14 days
case-identification: infection is obvious- distinctive rash
prevention: vaccine was effective + did NOT require a cold chamber for temperature regulation
eradication efforts:
surveillance and containment
selectively vaccinated people who had only been in contact with an infected person
malaria:
transmission: mosquito/parasite (combat it as they evolve)
recurrence: occurs many times (vaccines don’t work, so no lifetime immunity)
latency: remains in body for months without symptoms
case-identification: symptoms resemble other diseases (slower to intervene)
prevention: very hard (mosquito killing, but the technical fixes do not work)
eradication efforts: use of insecticides as the method of eradication as well as development of a possible 2nd variant for the malaria vaccine, R-21
polio:
transmission: polio comes from respiratory droplets (contaminated water)
recurrence: 25-40% have post polio syndrome when older
latency: not long~7-10 days but can be raised for 4-35 days
case-identification: often doesn’t present symptoms or flu-like symptoms, making it very hard to diagnose
prevention: oral vaccine with multiple doses + Cold chamber (temperature regulated)
eradication efforts:
-nationwide acute flaccid paralysis surveillance: reports children with AFP and map virus to determine origin of the strain
-environmental surveillance- fest sewage for the presence of poliovirus (target of 100% immunization with national immunization days)
be able to explain what easterly means by planners vs searchers?
planners- aid officials seeking to impose top-down solutions to poverty and other problems of development
Searchers- individuals in poor countries who start businesses or find creative solutions to reducing poverty and solving social problems
describe examples of the 8 principles of accompaniment
favor institutions that the poor identify as representing their interests- starts with beneficiaries believed to be acting in their interests
fund public institutions to do their job- supporting NGOs only drains resources and skilled personnel
make job creation a benchmark of success- achieve job autonomy to stimulate local economies and strengthen national tax
buy and hire locally- creates jobs, develops local markets, boosts tax revenues, stimulates entrepreneurship
co-invest with governments to build strong civil services- shore up/ modernize HR systems (cambodian government)
work with governments to provide cash to the protest- cash transfers are useful tools to reduce poverty (south africa, mexico)
support regulation of international non-state service providers- Haiti, uses NGOs without regulation or government coordination (increases efforts of generating lasting changes)
apply evidence-based standards of care that offer the best outcomes- premised on equity: demands raising the standard of care in resource- poor settings to a level acceptable for the more affluent settings
what are some arguments in favor of and against NGOs working in global health?
favor:
do valuable work in less fortunate countries
NGOs provide resources to avoided areas
against:
without regulation, they are duplicative, inequitable, and unaccountable to communities
funding them drains public sector of resources and skilled personnel
what is an argument that refutes the argument that there is not enough money to provide primary healthcare to the world’s poorest?
development could be strengthening by increasing aid outlays because the use could provide $40 billion to the poorest and still remain under the UN target
the reality for how much the U.S. spends towards supporting U.S. global health program and what is perceived has so much variation
medical voyeurism
the act of going to observe other people as tourists with no commitment to genuinely help the community but to learn and watching people educationally (zoo-like)
medical tourism
going to a different location for surgery, or students seeking opportunities to practice medical work in different countries (humanitarian projects)—> short-term medical interventions in resource-poor settings getting help from research rich settings that students take a part of
in what ways can student presence in developing country contexts be drains on the health system and staff?
student presence drain health by taking the resources away from a place that is already resource deprived
-questions ethics for why people actually go abroad
-requires more funding + health professionals, which takes more than they give by taking the attention of professionals away from the needs of patients ( nurses being used as translators rather than giving care)
-takes away from the needs of the medical students of that counties trying to learn by focusing more time and attention of abroad students from the actual physicians
the ethical dilemma of medical volunteering in resource poor countries
students of health professionals may misunderstand their roles
language + cultural barriers may interfere with respectful engagement
working in resource poor settings may raise issues that professionals/ students have
presence of volunteers can burden communities and waste resources
students may participate in research unknowingly and without the appropriate training
risk that being in a resource poor environment can serve to reinforce the existing stereotypes
know the recommendations of how to reduce negative unanticipated consequences of medical volunteering in resource poor countries
solutions to the ethical issues
doing pre-training lessons + useful thought understandings to understand why
learn more about the culture/ community before leaving
consider issues before going—> implementing structures that will only do what is the “trained” work
not taking up too much time of professionals but learn more outside of class ( ask locals what they need or want from you—> playgrounds)
receive training on research before (informed consent shouldn’t be done if out of ability)
not putting individual responsibilities on issues related to structural systems but encouragement to do more than training or HW
what social determinants of health contribute to unequal risk of being diagnosed with and dying from AIDS in brazil?
education, poverty and race: people who are not well educated in brazil, are poor, and Black have the highest risk of being diagnosed with AIDS, and dying as a result from it
what health services does brazil provide for citizens related to HIV/AIDS?
Brazil provides free HIV testing and provides free antiretroviral therapy or ART to all people living with HIV
how do AIDS cases and related deaths exemplify the concept of intersectionality
race and poverty levels are overlapped in creating higher HIV/AIDS diagnosis risk and death than either of them alone, representing intersectionality
how much more do j&j charge south africa for COVID 19 vaccines compared to the european union and their not-for-profit price?
johnson and johnson charged south africa 15% more per dose than the european union, and 25% more than the estimated not-for-profit prices
what is evergreening and how did j&j use it to extend their drug potent? how can south africa learn from india to help prevent this in the future?
this is the process by which pharmaceutical manufacturers make small, trivial changes to medicine for their use in order to keep their monopoly in the market
—> J&J used this to extend their drug patent by preventing competitors from making the same products for cheaper and entering the market
—> south africa can learn from india to prevent this by using strict reviews of patent applications, which examine the novelty of a medicine that company extends patents for (allows for sale of generic bed-aquiline)
list the year that the first effective treatment (combination of 3 antivirals) was available and what was the cost per year per patient
first available treatment : 1996
the cost per year per patient: $15,000
james love went to dc to lobby for support of generic drugs in africa. what was the one reason why they were opposed to supporting generic drug use in africa?
they were opposed to generic drug use in africa because the drug was not cared for, so they assumed it would be misused and causing mutations that would lead to resistance (the west assumed this would create a variant that would return to the U.S)
know why governments of poor countries back off from challenging the drug patients
they won’t challenge the drug patients in poor countries because they were worried it would lead to severe consequences, such as the companies would take over the government sanctions list
example 1 of blocking access to generic drugs- the u.s. response when the south african government was considering generic HIV drugs
the U.S. simply claimed that patents was all that could be used, and threatened that it would create sanctioned- watch lists for countries using generic HIV drugs
example 2 of blocking access to generic drugs- responses of european leaders and pharmaceutical companies to the indian company Cipla’s offering of HIV triple therapy of $800 per year
europeans did not change to improve the society by lowering HIV prices, making them generally more available for even poor communities
—> nobody took the $800 deal
example 3 of blocking access to generic drugs- the u.s. response to the immediate need for cipro to be available for treatment of anthrax exposure and why this relates to HIV drugs
the US suspended the patent: pushed down the price by force, so the U.S.government threatened to punish them if they chose not to lower their prices —> allowed for generic drug use ( implies that the government could also easily do this for HIV funders also)
example 4 of blocking access to generic drugs- the u.s. response to the Global Fund’s plan to purchase generic drugs
claimed that the U.S. government would pull out its commitment to the global fund if they purchased generic drugs —> president gave PEFFAR fund to african countries to decrease the aid prices with a total fund of $15 billion
one argument for supporting drug patent is they ensure companies could profit from a certain drug for a number of years. what are 3 critiques offered against drug patents:
1) the percentage of profits spent on r&d: 1.3%
2) percentage of global medication research funded by governments & public sources: 84%
3) large pharmaceutical companies are already among the most profitable companies in the world
know the difference between HIV and AIDS
HIV
caused by unprotected sex with infected partner, vertical transmission during pregnancy or infection drug use
AIDS
caused by having 200 or lower CD4 cells or having opportunistic infection and being HIV (+)
understand how HIV causes opportunistic infections
not having enough immune cells to fight off infections creates a higher chance for developing other diseases (more susceptible- HIV targets the CD4 cells to increase the chances of being infected by weakening the immune system with an opportunistic disease)
know the difference between PrEP, PEP, and ART, for HIV
PrEP- taken daily by people at risk for HIV (in preparation)
PEP- post exposure: taken ASAP with 72 hours of HIV exposure
ART- antiretroviral therapy: standard daily treatment, consisting of a combination of drugs that suppress HIV replication
—> goal: reduce viral load to undetectable (prospect for normal lifespan)
Look for examples of how the 8 aspects of PIH’s healthcare delivery model looked on the ground in rwanda
strengthening access to primary health care:
PIH focused on comprehensive primary health care
providing health care and education for the poor:
PIH’s focus was on rural rwandans
relying on community partnerships/health workers:
PIH established an organization committed to addressing health problems in rural rwanda
addressing basic social and economic needs:
community health workers ensured patients had access to basic needs
working to improve the public health sector:
PIH focused on strengthening the public health sector there so that they would not have to work there for long
focusing on the women and children
improving technology/communication programs
built labs, pharmacies, and operating rooms there
sharing lessons learned with the healthcare workers in rwanda
describe the role of accompagnatuers in the successful treatment of HIV
accompagnatuers are paid community health workers, who made home visits to ensure medication ingestion and patients had food access as well as ARVs
understand the mutuelle health insurance plan
insurance plan that mandated every citizen to purchase health insurance. Those who were not registered had to pull pay out of pocket expenses, but this plan was only $2
what was fundamentally different about the relationship between (PIH/IMB) NGOs and the rwandan government in comparison to most NGOs?
PIH/MIB worked closely with the rwandan government to “work itself out of the job” instead of establishing a longstanding presence. many activities are jointly produced with an eye towards the rwandan government taking over instead of PIH trying to maintain an active hold
Do high-income countries have a nursing shortage? what root causes contribute to the vacant nursing conditions?
no. high income countries have a shortage of healthcare institutions with necessary working conditions, but not a shortage of nurses. the root causes of this vacancy is:
mandated staffing ratios are ignored
workplace violence
high workloads/ short staffing
burnout
lower job satisfaction
lack of management support
downward pressure of nursing wages
how was nursing recruitment from low and middle income countries worsen equity in healthcare around the world?
this will only deepen the maldistribution of nurses globally. This causes brain drain and the shortage will disproportionately affect southeast asia, eastern mediterrian, and africa
they have an increased risk of exploitation, unfair wages, and stressful immigration barriers (longstanding systemic problems and racism)
according to the authors, what changes should governments and health systems enact to retain local nurses?
the government should enact these changes:
change language around the issue and address it directly
establish safe nursing ratios (gendered work )
cease unethical recruitment practices from lower/ middle income countries
develop policies facilitating violence reports/ sexual harassment in the work place
invest more in recruitment and nurse retention with the lower/ middle income country systems of health to address UHC
know the goals and function of a health system
keep people healthy/ prevent disease: public health focuses on prevention as part of a health system
treat people who are sick- medicine is focused on treatment
protect people from financial ruin due to costs of medical care
“ all actors, institutions, and resources that undertake health actions- where a health action is one where the primary intent is to improve health”
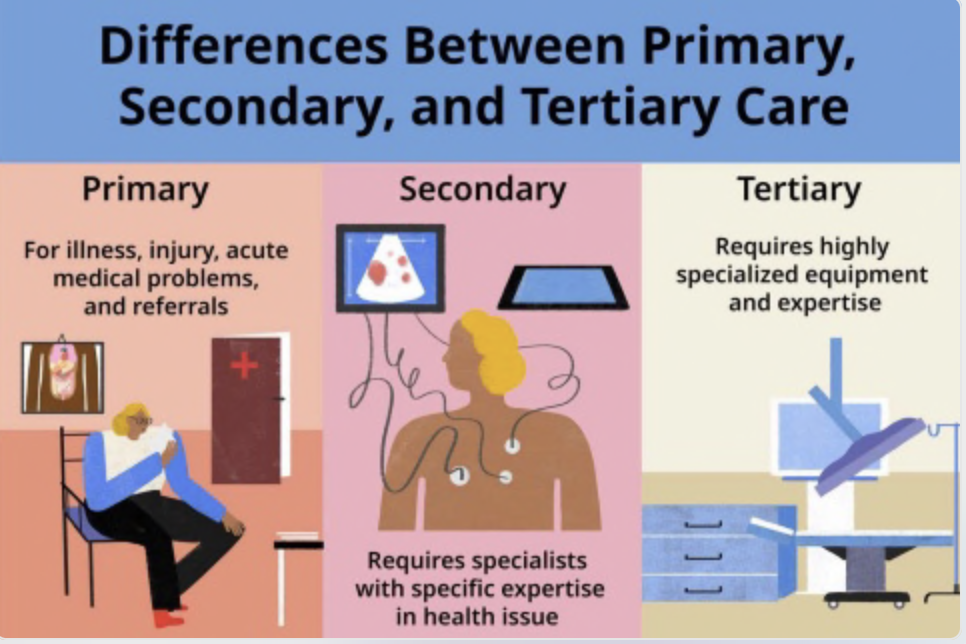
understand the 3 levels of healthcare
primary - the first level of health services offered for illness, injury, acute medical problems, and referrals by physicians
secondary - requires a specialist with specific expertise in a health issue
tertiary- requires highly specialized equipment and expertise (rarest form)
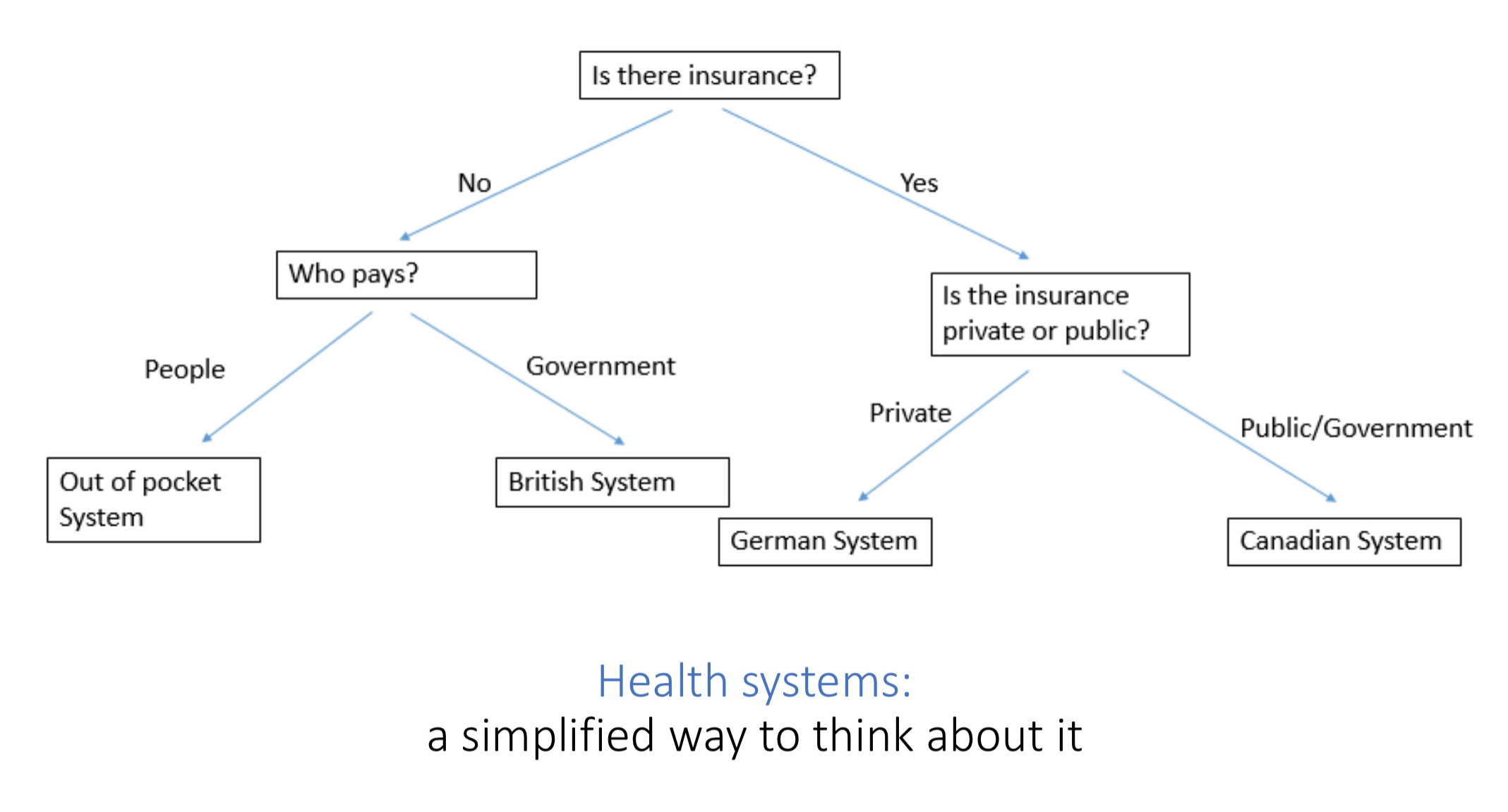
know the differences between national health service systems, national health insurance systems, and out of pocket systems
National Health Service:
comprehensive health services to all people regardless of ability to pay (healthcare is a human right univerally)
mostly public financing through taxes (NO INSURANCE!!)
Example- UK
National health insurance(public):
universal coverage for hospitals/doctors visits which is payed via taxes
single payer- no profit or financial motive to deny claims (has long wait time and focuses on medical care, not prevention)
Example- Canada
National health insurance (private):
sickness funds regulated by the government through non-profits (multi payer system with different funds)
sickness funds: universal coverage + partly employer funded
Example- Germany
Out of pocket system:
many low and middle income countries have no established health care system
rich get access to medical care, while the poor don’t (only model where any medical care is paid for by patients) → creates expenses within health systems
Example- United States
health insurance
insurance is a way to protect someone from the financial harms of a loss
which type of healthcare system does cuba have? what is the cuban healthcare system known for?
cuba has universal health coverage and its healthcare system is known for having a government-operated health systems (all clinics hospitals, services, staff) with an average of 9 doctors and nurses per 1,000 inhabitants which is much higher than France,Australia, and the U.S.
know what is meant by universal healthcare coverage by the WHO and what two metrics they use to measure UHC
UHC means all people have access to the full range of quality health services they need, when and where they need them, without any financial hardship
** DOES NOT MEAN FREE COVERAGE
WHO measuring metrics:
the proportion of a population that can access essential quality health services
the proportion of the population that spends a large amount of household income on health
what is brain drain and how can it play out internally within a country and externally between countries?
brain drain: the depletion of health workers from LMICs and countries, such as the U.S. encourage foreign workers to come
when skilled workers leave resource poor environments
externally- this leaves the home country resource deprived and even more deprived than it was before
internally- this represents a quick fix to health services (Italy’s use of this represents vertical approaches/ colonialist ideas
**brain drain is a form of structural violence by preventing people from meeting their basic needs