Wk3 Biomechanics of synovial joints
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
What are the functions of synovial joints
1) Load transfer
2) Allow movement
What are 3 factors of load transfer
Graduated flexibility
Increased surface area
Variable bearing area
What is Graduated flexibility
If you would place 2 rigid surface against each other, then it will have high contact stresses when under load ->There is decrease in stiffness and increase in compliance from compact bone to cartilage ->To facilitate shock absorption and load transfer
Decreasing compressive stiffness and increasing compliance as you go down the limb decreases peak contact stress at the articular surface which helps facilitate shock absorption
What does Increased surface area do
Increased area of the articular surface reduces stress
From the shaft to the epiphysis, there is a widening of the bone, increasing the contact area and distribution of the load
Menisci's also increase contact area
What does Variable bearing area do
Bearing area is a structure that constrain movement to desire amount while minimising the friction between the moving parts
The entire surface of an articular surface isn't always in contract with one another and the contact area isn't always the same which affects amount of stress applied
What is the function of hyaline cartilage
- To withstand and distribute the applied load to protect underlying subchondral bone from high contact stresses
- Allowing relative motion of articulating surfaces with low friction and minimal surface wearing (Bearing area function)
What is the general structure of hyaline cartilage
<10% chondrocytes (Very little cartilage cells maintaining the cartilage)
90% extracellular matrix = 80% is water + second most abundant is Collagen type 2 fibrils + Proteoglycan aggregates = 7%
Avascular
What are the 3 zones of hyaline cartilage
Superficial 10-20%
Middle 40-60%
Deep 30
what is the Superficial zone
-Relatively thin layer on the surface, where the collagen fibrils are very densely packed (This is where most of them are)
- Fibrils are parallel to bone surface which makes them resistant to friction from opposing articular surface
- Provides superficial interstitial fluid support
what is the Middle zone
Fibrils are less dense, and forms in multiple direction in a mesh pattern
Mostly where proteoglycan aggregate are present (NOT as many in the deep or superficial zone where collagen is denser)
What is the Deep zone
Fibrils are perpendicular to surface of bone that extends through the tidemark
Extensions of deep zone fibrils from the bone through the tidemarks, helps provide a secure connective between cartilage and bone
Tidemarks are border between the calcified and non-calcified cartilage
What is the most common aggrecan in hyaline cartilage and what is it
Aggrecan (7% of hyaline cartilage)
Large protein
Proteoglycan with protein core and side chains of GAGs (which contain negatively charged ions)
What do Aggrecans bind with
Hyaluronan to form Proteoglycan aggregate (Large and immobile)
What effect does the fixed negative charge from GAGs do
-The sulphate and carboxyl groups on GAG’s which are negatively charged attached to the aggrecan dissociates in solution, leaving a high concentration of fixed negative charges
-The charge-charge repulsion extends and stiffens the proteoglycan aggregate by making the charges push against each away, This makes the proteoglycan aggregate to take up as much space as it wants
-SO, when you try to apply force on the proteoglycan aggregate, there is an inherent resistance of the molecule
What is the Donnan osmotic swelling effect
Negative charges attracts positively charge ions from synovial fluid into the cartilage
This causes a charge gradient, which then causes water to go into the higher concentration cartilage from the synovial fluid
Causes the cartilage tissue to swell up with water from the synovial fluid
What is the interaction between Proteoglycan aggregate and collagen
-The mesh of Interwoven collagen type 2 fibrils confines the PG aggregates to 1/5 of their natural domain that they would like to expand to
-The proteoglycan aggregate wanting to expand creates a tension within the collagen fibrils
-Both the collagen fibrils and proteoglycan aggregate is pre-stressed from tension due to the Proteoglycan aggregate wanting to expand
-creates a stiff extracellular matrix that is resistant to compression and shearing (but not tension)
What are the 2 phases of the biphasic cartilage model
1) Fluid phase
2) Solid phase
What is the Fluid phase
-Initially hydrostatic pressure in the interstitial fluid (water) supports the initial compressive load
-The hydrostatic pressure can load up to 90% of initial load, depending on rate of compression because viscoelastic properties
What is the Solid phase
-Refers to the PG aggregates and collagen interaction, and their pre-stress state
-There is Compressive and Shear stiffness provided by the PG-Collagen network
Is the PG collagen network a porous, permeable solid swollen with interstitial fluid
Yes, the compliance of cartilage is partly determined by flow of interstitial fluid
When there is water movement, it creates frictional drag due to the presence of PG aggregates and collagen fibrils
How is frictional drag involved in movement of interstitial fluid
-Created by interaction between the fluid and solid components
- Increased by decreasing pore size
- Increased by increasing the number of collagen fibrils and proteoglycan aggregate
- increasing compression of tissue
- increasing the viscosity of fluid
How is porosity involved in movement of interstitial fluid
-spaces in the tissue
- The fewer and smaller the space, will more greatly restrict the movement of fluids
- Extrinsic force will decrease the size of the pores, which will decrease flow of fluids due to greater frictional drag
How is permeability involved in movement of interstitial fluid
-ease of fluid to flow through a material
- This is inversely proportional by frictional drag (Created by interaction between the fluid and solid components)
- Very low matrix permeability due to the spatial arrangement of the PG-collagen solid matrix and partly due to viscosity of interspatial fluid
- The more pores and larger the pore spaces, the more permeable
Due to the low permeability of the hyaline cartilage, external compression is initially resisted by hydrostatic pressure in the interstitial fluid - True or false
True
When hydrostatic pressure exceeds that of the osmotic swelling pressure (all the PGs that drawn in water), the fluid can flow- True or false
True
- Rate of fluid flows DOES NOT depends on porosity and permeability (inverse of frictional drag) - True or false
False
Frictional drag increases with an increasing rate of flow - True or false
True
Redistribution of fluid transfers stress to solid components - True or false
True, so Health wise, it is best to stay within the fluid phase, if you stay prolonged on the solid component, it will break down
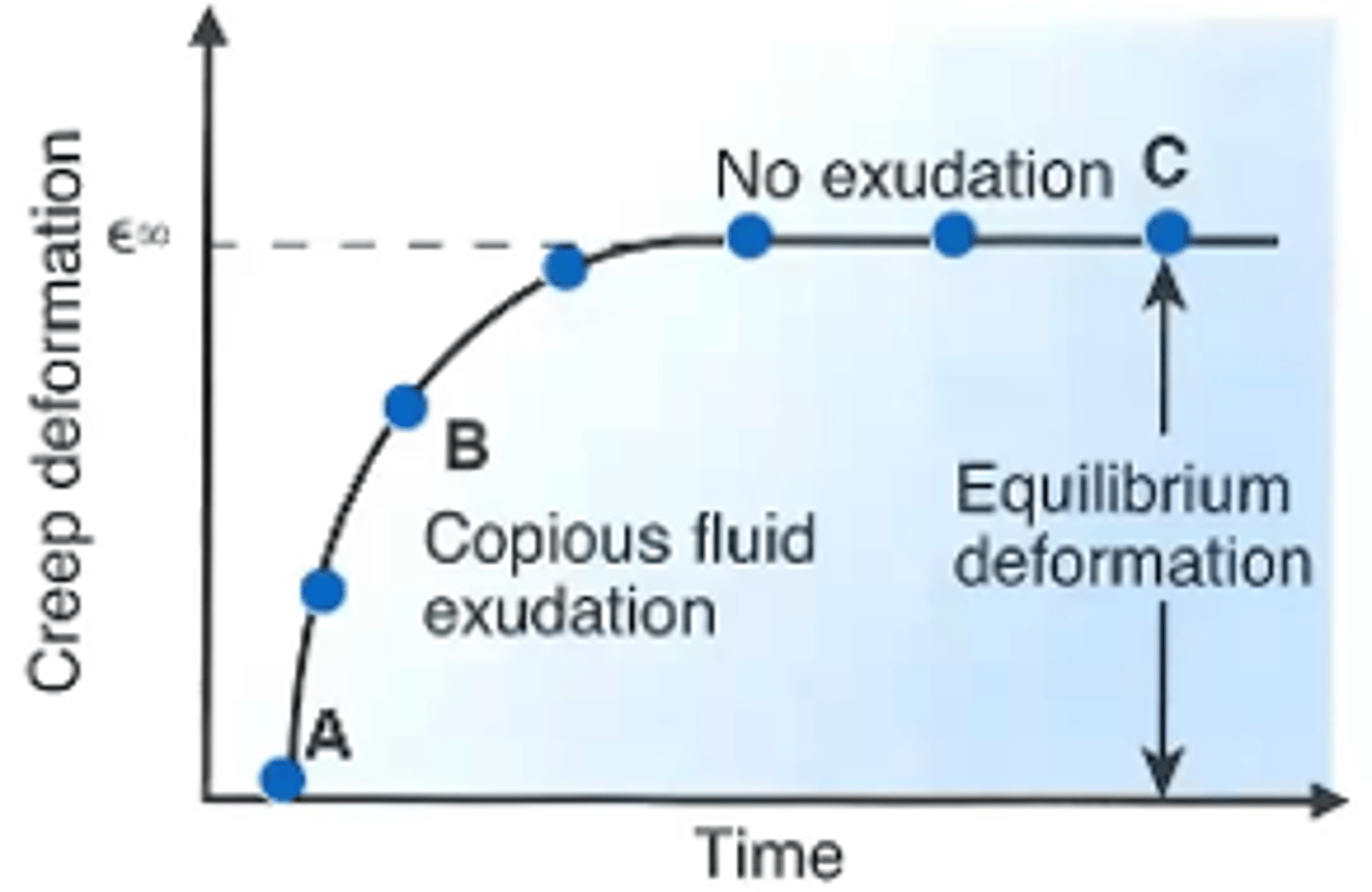
What happens when you creep hyaline cartilage
The tissue rapidly strains due to fluid movements, and then plateaus off when the tissue components redistribute so that the internal stress is equal to the externally applied stress
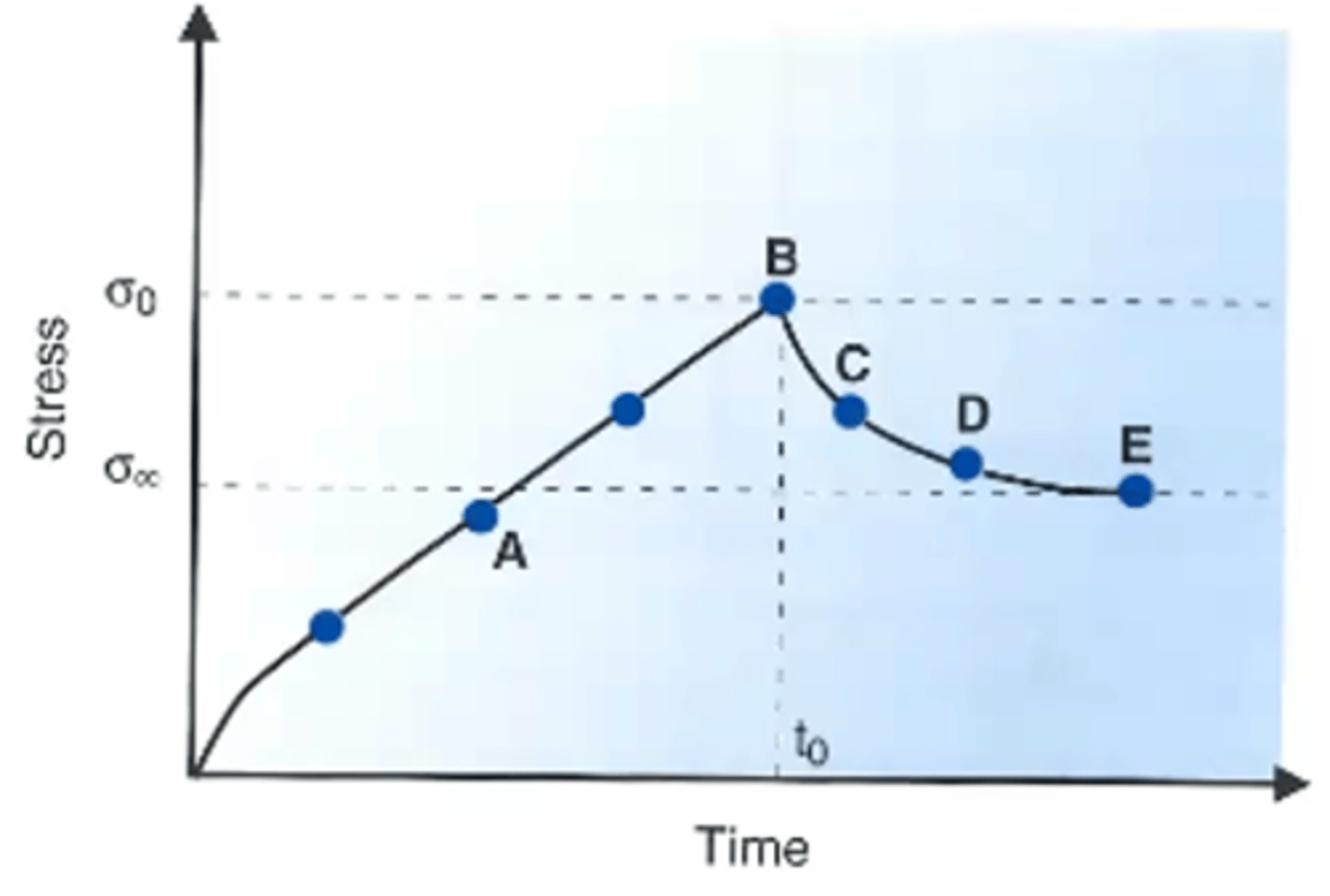
What happens to hyaline cartilage during stress relaxation
Initially the stress is building up
Keeping it at the same strain, will eventually causes the stress to relax and lower to an equilibrium this is due to the fluids flowing and redistributing the stress to a new equilibrium
What happens if you increase the rate of strain to hyaline cartilage
If you increase the speed of strain, you get increased stiffness until it plateaus
What happens to hyaline cartilage during low strain rate
- Gives the fluid time to move at a low rate of strain
- Results in low frictional drag
- The fluids redistributes and there's a local indentation
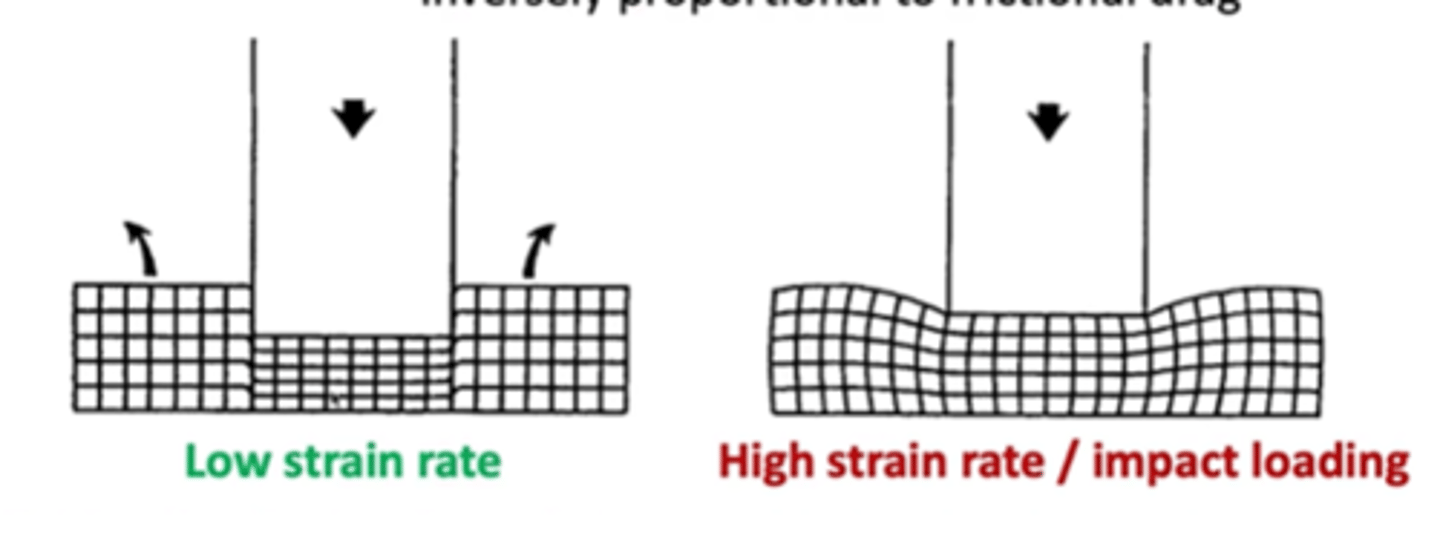
What happens to hyaline cartilage during high strain rate
- Fluid has no time to move, so the fluid is met with high frictional drag
- Becomes more resistant
- Significant lateral distortion
How does Articular surface roughness affect friction force
-Microscopically, articular surfaces are rough with peaks and troughs
-The greater the roughness and heights of peaks, the greater the friction
What are the 4 factors affecting friction force
1) Articular surface roughness
2) Normal load (N) (Friction = Coefficient of friction x Load)
3) Static vs kinetic conditions
4) Mode of lubrication (boundary, fluid-film, mixed)
How does Normal load (N) affect friction force
The Frictional force = coefficient of friction x Normal load. So, increasing the loading, the frictional force is higher
How does Static vs kinetic conditions affect friction force
-Static friction forces are greater than kinetic friction forces because in kinetic conditions, the atomic bonds in the asperities can't be made, so its easier to flow while moving
-In static when you stop, the asperities undergo stress over time (Creep) and the atomic bonding will form
What 2 macromolecules are important for synovial lubrications
- Hyaluronan
- Lubricin
- They are large macromolecules that are Hydrophilic
When does boundary layer lubrication occur and how much coefficient of force does it produce
- Experience it under high loads and/or at high speeds
-Produces Greatest Coefficient of Friction
What happens in boundary layer lubrication
Collagen type 2 fibres at the cartilage surface (the layer that is parallel) forms molecular links with lubricin and hyaluronan in synovial fluid
A sacrificial layer is formed between these molecules that protects articular cartilage damage by each other
In healthy cartilage, you can replenish 10x as much then what is depleted
When does fluid-film lubrication occur and how much coefficient of force does it produce
- Occurs at high articulation speeds and low loads
-Least coefficient of friction
What happens in fluid film lubrication
- The articular surfaces are separated by a fluid film
- The fluid film’s distance is greater than the asperities of the articular surface (3x the distance of the asperities) to avoid contact of asperities
- Load is supported by the pressure generated in the fluid, hydrostatic pressure in the synovial fluid
- Frictional resistance is low because the friction arises entirely from the shearing of the viscous fluid
What is the interaction between hyaluronan between lubricin and hyaluronan during fluid film lubrication AT REST
-In synovial fluid, Lubricin facilitates hyaluronan chains to create coil configuration that are rigid to external stress but not high enough to resist yield stress when you move, so you can break the bonds
-Acts like a solid
What is the interaction between hyaluronan between lubricin and hyaluronan during fluid film lubrication DURING IMPACT/INSTANT LOADING
- The Hyaluronan chains remained coil and linked to each other
-The synovial fluid behaves elastically like a solid to bear the intensive loading
What is the interaction between hyaluronan between lubricin and hyaluronan during fluid film lubrication DURING SLOW LOADING (walking)
-Hyaluronan chains are broken, and align parallel so they slip past each other smoothly,
-behaving like a viscous fluid
What is a Newtonian fluid
Have a constant viscosity across shear rate, whether it be high or low depends on the fluid
There is a Linear relationship between shear rate and shear stress - So the viscosity stays constant
What is a Non-Newtonian fluid (synovial fluid)
Exhibits a decrease in viscosity with increasing shear rate
What is mixed lubrication
Has coefficient of lubrication between boundary layer and fluid film
All 3 lubrication types can happen at once
Why does fibrocartilage have a stiffer tensile modulus of elasticity and greater ultimate tensile stress compared to hyaline cartilage
Because fibrocartilage comprise of type 1 collagen which are larger and are more suited at resisting tensile load
Why does hyaline cartilage have a stiffer compressive and shear modulus of elasticity and greater ultimate compressive and shear stress compared to fibrocartilage cartilage
1) It has a higher compressive modulus due to its higher count of proteoglycans, which creates a higher osmotic swelling pressure
2) the proteoglycans aggregate form a matrix with the collagen type 2 fibrils, this pre-stresses them and helps resist against shearing and compression
How does fibrocartilage's mechanical properties relate to its function
Fibrocartilage is stronger and stiffer at tensile load but more compliant in terms of compression and shear
This suits the fibrocartilage's function of shock absorption and being able to deform without tearing damage thanks to tensile strength
This fulfils the gradual flexibility requirement from cortical bone -> Spongy bone -> Hyaline cartilage -> Meniscus
What are the 5 functions of a meniscus
1) Distributes load to decrease stress (They double contact area between femur and tibia)
2) Shock absorption (absorbs by deforming but having good tensile strength)
3) Enhances Joint stability (Improve joint congruency)
4) Enhances Proprioception (horns have mechanoreceptors)
5) Lubrication (They help with lubrication by spreading out synovial fluid)
Where is force transferred through greatest in a meniscus
medial compartment of the knee
the more we put our knee into flexion, there is an increase amount of force moving through the posterior horn hence why it's important the medial meniscus has a larger posterior horn
Which meniscus covers more of its' plateau
- Whilst the medial meniscus is larger than the lateral, the medial plateau is also larger so that means that: Medial meniscus Only covers 50-75% of its' plateau
The lateral meniscus covers more of its plateau at 75-93% of its' plateau
Are cells within a meniscus all similar during early development
Yes
What is the internal structure of the outer-zone
-80% type 1 collagen, this is where most collagen type 1 is
-Has a lot of fibro-blasts
What is the internal structure of the inner-zone
-Resembles more like hyaline cartilage
-70% type 2 collagen, so more type 2 rather than type 1
-Inner 2/3rds does has higher proteoglycan, but not as much as in Hyaline cartilage
Where are progenitor cells mostly present
Superficial zone
How does vascularity change from birth, 10 years and adulthood in meniscus
At birth: 100% of the menisci is vascularised
10 years: 10-30% vascularised
Adult: Only on the periphery, 10-25%
BONUS: Outer 1/3 vascular zone is innervated and there is mechanoreceptors especially present within the horns
Why is the different composition of collagen type important throughout the different zones of a meniscus important
-In weight bearing, diagonal femoral force is generated which can be made up of a vertical and horizontal force
-This means that although the main force generated is compressive, it is actually fitting because it is directed at the inner zone where Type 2 collagen is present
-there is also horizontal forces that wants to displace the meniscus radially which creates a circumferential force, where type 1 collagen is most present. This is good to prevent it from tearing
What are changes to meniscus due to aging
-Becomes opaque, yellowish brown
-Surfaces roughens with fibrillation and there less progenitor cells to repair the surface abrasions
-Becomes harder and loses elasticity
-Changes occur early along the inner rim but the anterior horns are less affected age and OA (As it is less exposed to load), as posterior horn is more exposed to load
What are other changes to meniscus from aging
-Cells slow down and becomes less dense through less proliferation
-Abnormal proteoglycan structures and concentration of them
-Collagen amount increases from birth to 30 years, and then stays stable
-Collagen fibrils diameter increases
-Increased cross-linkage between the fibrils
-Calcification in the extracellular matrix
-Myxoid intrasubstance degeneration (areas becomes fatty and replaces normal ECM components)
Does tensile strength increase with age
Yes, thanks to cross linkage between fibrils
What are degenerative changes to meniscus
- Begins the Extracellular matrix
- Abnormal cells, cell hypertrophy and abnormal cell clusters
- Decrease in concentration and quality of proteoglycan
- Severe separation of ECM
- Tears, and fraying of the meniscus
- Calcification
How can you classify tears
Can either be Traumatic or Degenerative
Depth: Does it go through from the upper aspect to inferior aspect of meniscus (partial or complete)
Location: Rim: Circumferential zone 1, 2, 3 Or Radial: Anterior, middle, or posterior
Tear patterns
What are common tear patterns
- Longitudinal: Happens in young people
- Bucket handle: A larger longitudinal tear
- Horizontal: Arise from degenerative tears
- Radial: Most common type in young adults, at the 1/3rd junctions
What are healthy old normal articular cartilage like
-Discoloration due to accumulation of advanced glycation end products (AGEs)
-Reduced cartilage thickness
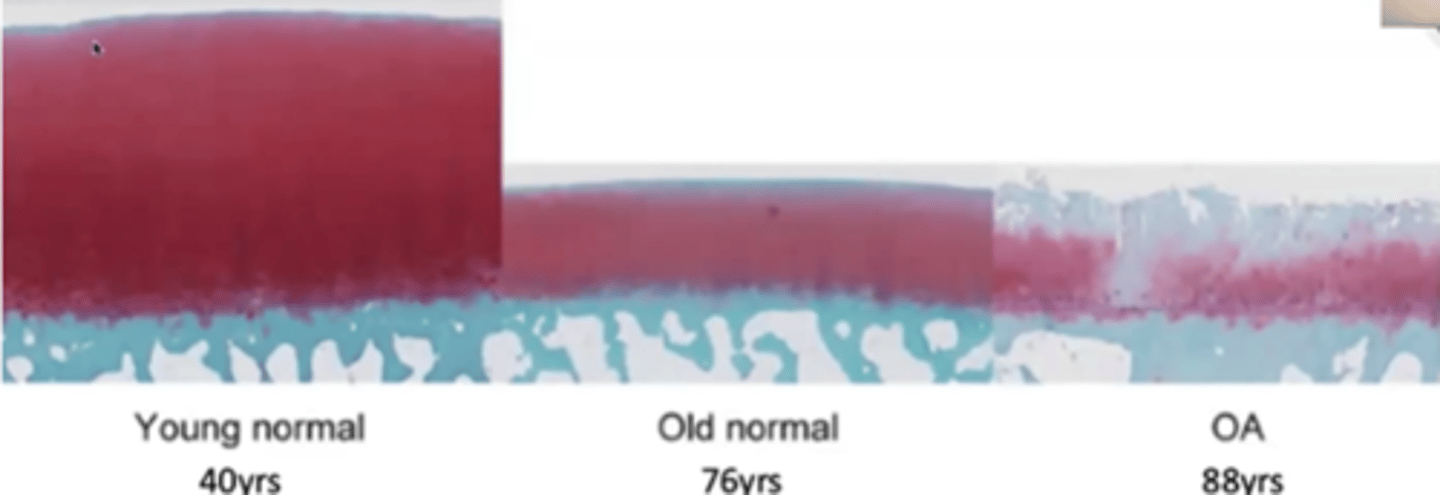
What are OA femoral articular cartilage like
-Can be loss of cartilage
-Can be osteophytes present
-Loss of superficial and middle zone
-Fibrillation that goes into the deep zone
-Areas of low cellular density AND areas of cell clumping at the same time
-Duplicated tidemarks
What are the normal age-related changes in hyaline cartilage cells
-Decreased chondrocyte density (Especially in superficial zone)
-Decreased chondrocytes = less lubricin being produced
-Less lubricin = less boundary layer lubrication to protect against wear and tear
Why are there less chondrocytes in older age
-Body does chondrocytes apoptosis to get rid of dysfunctional cells to maintain homeostasis
-There is hypertrophic changes in chondrocytes, as during endochondral ossification later in age, some chondrocytes are not preserved while undergoing ossification
-Decreased capacity to synthesise
-Chondrocytes begins to produce inflammatory and enzyme degrading mediators
What effect does the long turnover rate of proteoglycan has on the hyaline ECM
-Makes it more susceptible to advanced glycation end products (AGEs)
What happens to the Hyaline cartilage ECM with age
-Aggrecan decrease in size, composition and concentration
-Old dysfunctional aggrecan fragments take up space that new aggrecans would bind to
-Collagen starts to cross link, becoming stiffer but more brittle
-ECM calcifies
-Hyaline cartilage thins
-Increased tidemarks
-Tidemarks move into deeper zone
-Lower calcified cartilage gets turned into bone
What effect does Old dysfunctional aggrecan fragments taking up space that new aggrecans would bind to has on the ECM
-Increases ECM permeability and porosity
-Decreases its ability to retain water
-Reduces cartilage's resistance to shear and compression
What are risk factors for OA
-Age (biggest correlator)
-Female
-Obesity
-Previous injuries
-Genetics
-Metabolic disease (diabetes)
-Endocrine disorders
-Other rheumatic diseases (Rheumatoid arthritis, gout)
How does OA alter lubrication
-Decrease in concentration and size of Hyaluronan
-Synovial fluid becomes less viscous and loses the shear-thinning behaviour
-Decrease synthesis of lubricin
How does OA alter chondrocyte activity
- Resemble terminally differentiated chondrocytes in growth plates
- Cell clumping
- Produces pro-inflammatory mediators and matrix degrading enzymes
What are other changes with OA
-Degradation of collagen -> Bearing surface failure and fibrillation (increasing coefficient of friction)
-Degradation and loss of aggrecans, harder to keep water in the cartilage
-Cartilage is more easily deformed
-Subchondral bone is expose; cysts can develop as synovial fluid is toxic to bone marrow
-Altered subchondral bone stiffness
-Osteophytes (bony spur) formation and hypertrophy of bone at the margin
-Synovitis (inflammation of synovial lining), due to proliferation and hyperplasia of lining cells, these cells release inflammatory markers causing inflammation
-Intra-articular and periarticular structures (ligaments around the area) are affected
What are the 4 modes of altered loading to hyaline cartilage health
1. Excessive impact load
2. Prolonged static load
3. Absence of load
4. Change
What is Excessive impact load
Dynamic stiffening: frictional resistance to fluid increases with increasing velocity but can tear the cartilage if it's too high
What is Prolonged static load
Gives time for the fluid to flow and you lose the fluid phase of support via the hydrostatic pressure
The load is transferred to the solid component, the coefficient of friction is greater in the solid phase
What is Absence of load
Not enough stimuli for chondrocytes to maintain the matrix
What is Change
Change in the distribution or rate of loading
cartilage is slow to adapt
- You change the load of training or exercise regime or there is an injury, the cartilage is slow to adapt to the change
Why is Hyaline cartilage is bad at healing
- Its avascular, a-lymphatic and no neural innervation
- Low cellular density
- Low metabolic activity
- Inability to migrate to the site of injury