IB Bio Exam Review- D3.1 Reproduction (copy)
1/67
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
what is nondisjunction in meiosis?
anomaly that occurs during cell division where homologous chromosomes (sister chromatids) fail to separate properly, leading to gametes (sperm or egg cells) with an abnormal number of chromosomes, a condition known as aneuploidy. this causes abnormal chromosome number in the zygote.
what are examples of nondisjunction in meoisis?
Down syndrome (trisomy 21 ): person has 3 copies instead of 2 of this chromosome
causes developmental delays, intellectual disabilities, and characteristic physical features
Turner syndrome (monosomy X): females having only one X chromosome instead of the usual two
causes short stature, infertility, and heart and kidney abnormalities.
Klinefelter syndrome (XXY): males have an extra X chromosome
causes hypogonadism, reduced fertility, and sometimes learning difficulties.
what are factors contributing to nondisjunction?
Maternal age
Genetic factors
Environmental factors
all plants and animals are _____ with different sized male and female gametes.
anisogamous
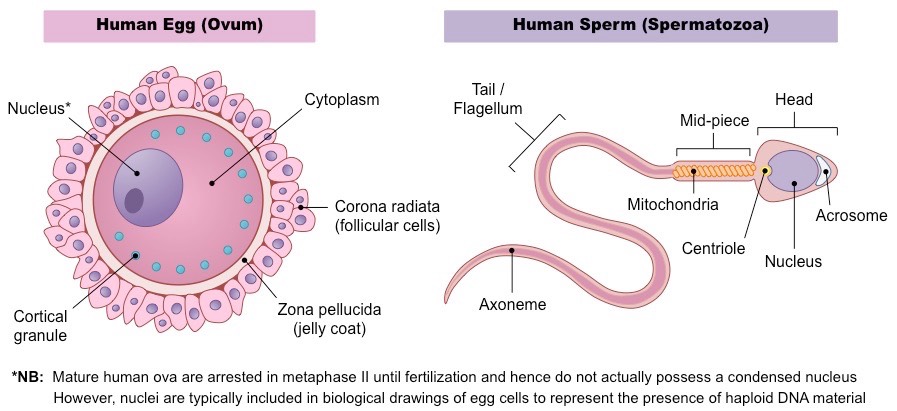
what are the characteristics of male gametes?
male gametes travel to the female
they are smaller than female gametes
faster movement
smaller food reserves
produced in large numbers
what are the characteristics of female gametes?
non-motile (don’t move on their own)
larger size because of food reserves
for the embryo
smaller numbers
who came up with the theory that all life comes from the egg (as opposed to the sperm)?
william harvey in 1651
what is fertilization?
the fusion of a sperm with an egg to form a zygote
how does the sperm locate the egg?
receptors in the plasma membrane of sperm allow the detection of chemicals released by the egg, allowing for directional swimming
what is the proccess of fertilization?
sperm attached to the cell’s corona radiata break through the barrier of the granulosa cells and approach the zona pellucida
contact with the zona pellucida triggers the acrosome reaction, causing sperms to secrete enzymes that break down the glycoprotein membrane of the zona pellucida and help to expose the oocyte’s plasma membrane
a single sperm makes it through the corona radiata and zona pellucida, making contact with the oocyte’s plasma membrane, fusing the two, which causes the sperm to release it’s nucleus into it’s cytoplasm
what is the corona radiata?
the first layer sperm must get through, the outer layer of cells surrounding the egg
THINK: corona —> granulosa —> zona, c —> g —> z in alphabetical order
what are granulosa cells?
the second layer spem must get through, cells forming a protective barrier around the egg.
what is the zona pellucida?
thick layer of glycoproteins surrounding the eg
what is the order of barriers the sperm must get through to reach the egg’s genetic material?
corona radiata —> zona pellucida —> plasma membrane —> cytoplasm
what is an oocyte?
known as an egg cell or ovum, is the female gamete (sex cell) involved in sexual reproduction, created through oogenesis, maturing within structures called follicles
what is an ovary?
where oocytes mature prior to ovulation (release)
it also secretes estrogen and progesterone
what is the fimbria?
fringe of tissue next to the ovary that sweeps the oocyte into the oviduct
what is an oviduct?
aka the fallopian or uterine tube, transports the oocyte to the uterus
where fertilization occurs
what is a uterus?
organ where fertilized egg implants and develops, becoming an embryo
what is the endometrium?
mucous membrane lining of uterus that prepares for implantation by thickening, and is shed during menstruation
what is the vagina?
passage leading to the uterus by which the penis can enter
what is the cervix?
narrow, cylindrical structure that forms the lower portion of the uterus, connecting and protecting the vagina
what are the testis?
Male reproductive organs located in the scrotum.
Produce sperm cells through spermatogenesis in seminiferous tubules.
Essential for sperm and hormone production in males.
what is the epididymis?
tightly coiled tube located on the posterior surface of each testis, stores and transports sperm cells produced in the testes
sperm move from the _____ to the vas deferens during ejaculation.
what is the vas deferens?
a muscular tube that transports sperm from the epididymis to the ejaculatory duct
Travels from the scrotum through the inguinal canal, loops over the bladder, and joins the ejaculatory duct near the prostate gland.
how does sperm move through the vas deferens?
peristalsis (muscular walls contract)
what is the seminal vesicle?
gland located near the base of the urinary bladder, produces a significant portion of the fluid that makes up semen
secretions contain fructose (to provide energy for sperm), prostaglandins (to facilitate sperm motility), and other substances.
what is the prostate gland?
a walnut-sized gland located just below the bladder, carries urine and semen out of the body
secretions contain enzymes, citric acid, and zinc
what is the urethra (in males)?
tube that carries urine from the bladder to the outside of the body during urination and serves as a passageway for semen during ejaculation
contains 3 parts:
the prostatic ____ (passes through the prostate gland)
the membranous ____ (passes through the pelvic floor muscles)
the spongy or penile _____ (passes through the penis).
explain the process for IVF
Ovarian stimulation: LH and FSH are used to cause multiple egg release
Egg retrieval: once the ovarian follicles containing mature eggs reach the desired size, injection of hCG
Fertilization with collected sperm and incubation
Viable fertilized blastocysts are selected to develop into embryos
Implantation of embryos to uterus
Pregnancy test
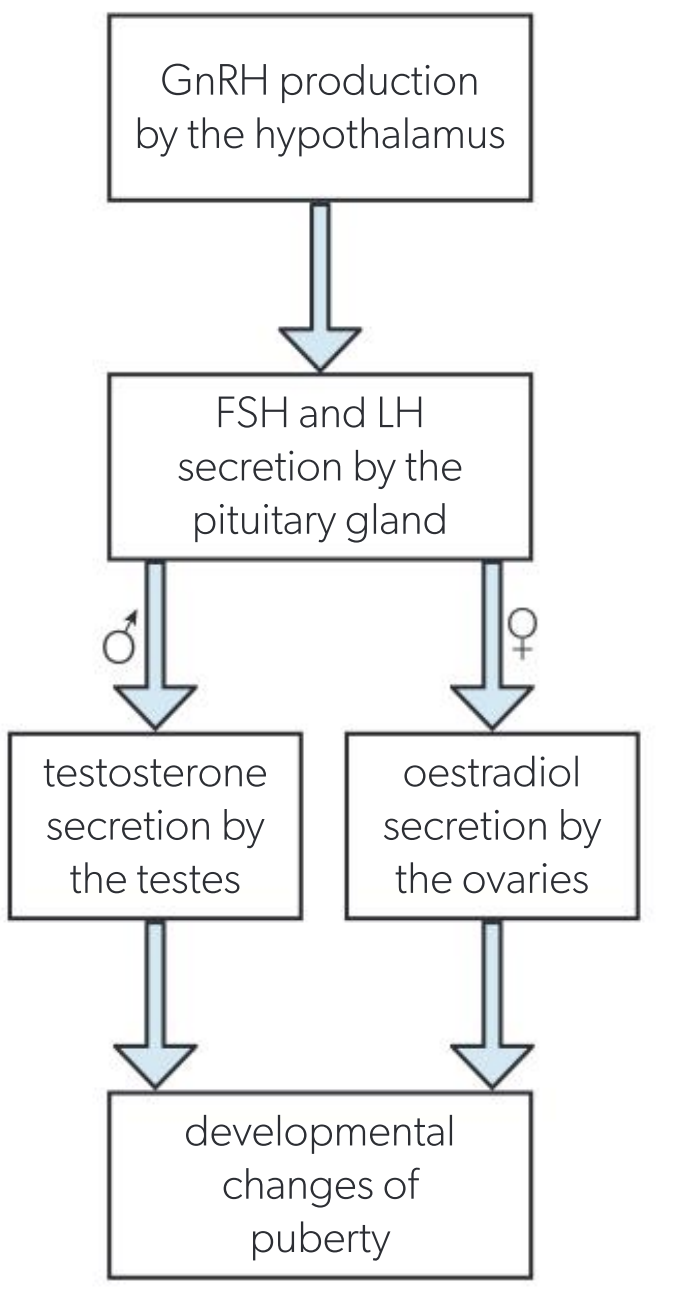
what is LH?
aka luteinizing hormone, produced by the anterior pituitary gland
what is FSH?
aka follicle-stimulating hormone, produced by the anterior pituitary gland
what does LH do?
in females: stimulates the ovaries to produce estrogen and progesterone and triggers the release of a mature egg from the ovary during ovulation
in males: stimulates the Leydig cells in the testes to produce testosterone, the primary male sex hormone
what does FSH do?
in females: stimulates the growth and development of ovarian follicles (small sacs within the ovaries) and promotes the maturation of eggs (oocytes) within these follicles.
in males: stimulates the Sertoli cells in the testes to support spermatogenesis, the process of sperm production.
what is the main function of the zona pellucida?
to prevent polyspermy, which is the fertilization of an egg by more than one sperm cell
during which phase of the menstrual cycle does ovulation typically occur?
the luteal phase
what happens during ovulation?
a mature egg is released from the ovary around the middle of the cycle.
following _____, the empty follicle transforms into a structure called the corpus luteum, which produces progesterone to prepare the uterine lining for potential embryo implantation.
if fertilization and implantation do not occur, progesterone levels decline, leading to the shedding of the uterine lining during menstruation.
what are the stages of the menstrual cycle?
Menstrual (Days 1-5)
Follicular (Days 1-13)
Ovulation (Day 14)
Luteal (Days 15-28)
what happens during the menstrual phase?
occurs days 1-5
shedding of the uterine lining
low levels of estrogen and progesterone
what happens during the follicular phase?
days 1-13
growth of ovarian follicles, where the egg matures
increasing levels of FSH (Follicle-Stimulating Hormone) and estrogen
"Follicles flourish" (Follicles start to grow)
what happens during ovulation?
day 14
release of a mature egg from the ovary
surge in LH (Luteinizing Hormone)
ovo = egg = ovulation = egg release
what happens in the luteal phase?
Days 15-28
formation of the corpus luteum, which secretes progesterone
high levels of progesterone and estrogen
"Follicles Start Here"
FSH (follicle-stimulating hormone) stimulates follicle growth
"Lets Hatch"
LH (Luteinizing Hormone) triggers ovulation, releasing an egg
"E for Establishing the lining"
Estrogen peaks before ovulation, rebuilds the uterine lining.
"P for Preparing for Pregnancy"
Progesterone: Maintains the uterine lining.
whats a mnemonic for the menstrual cycle?
"Follicles flourish in the follicular phase, ovulation the egg goes on its ways, luteal phase prepares the place, and menstruation clears the space."
what is progesterone’s function, when does it rise, and what type of feedback loops are it part of?
function: promotes endometrial thickening
rises: start of luteal phase
feedback: inhibits FSH + LH (negative feedback)
what are the protein hormones?
FSH and LH
what is LH’s function, when does it rise, and what type of feedback loops are it part of?
completes meiosis in egg, digests follicle wall for ovulation, promotes corpus luteum
rises: end of follicular phase
feedback: promotes corpus luteum, which secretes estradiol and progesterone (positive)
what is FSH’s function, when does it rise, and what type of feedback loops are it part of?
stimulates development of hormones + secretion of estradiol
Rises: towards end of menstrual cycle
Feedback: negative, inhibited by high estradiol levels
progesterone
function: stimulates
endometrial thickening/lining during ovulation/luteal phase
Rises: end of follicular phase
Feedback: inhibits FSH,
promotes LH
what are some common features of a pollinator?
Flowers have large, brightly coloured petals that advertise the flower, act as a landing stage and guide the insect’s movements to the anther or stigma.
Scent is secreted from the petals to advertise the flower.
Pollen grains are large and spiky so they stick to insects and are attractive as a protein-rich food.
Stigma is large and sticky to collect pollen from visiting insects.
Glands called nectaries secrete a sugar solution (nectar) that is attractive to insects as an energy source.
Nectaries are positioned deep inside the flower so insects can only reach them by brushing past the anthers and stigma
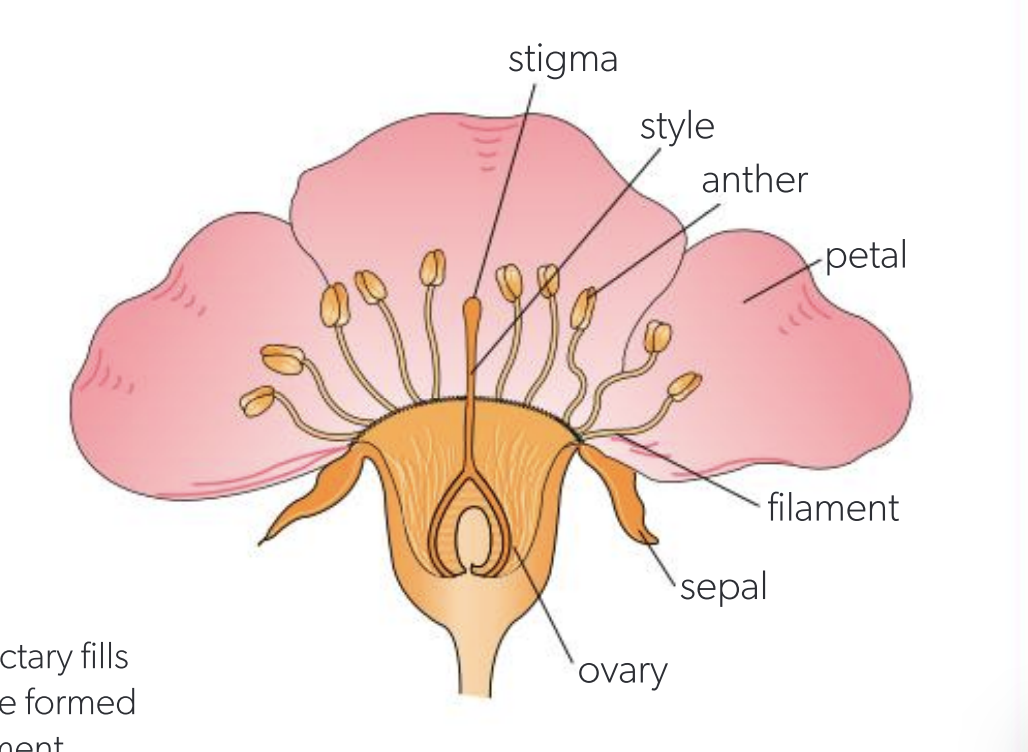
what are the parts of a flower’s reproductive system?
Petals help insects to find the flower
Sepals protect the floral organs during development
Anthers produce pollen containing the male gametes
Filaments hold the anthers in a position where they are likely to brush pollen onto visiting insects
Stigma captures pollen from insects
Style positions the stigma where insects brush past and also guides the growing pollen tube to the ovary
Ovary holds the ovules until fertilization and then develops into a seed-containing fruit
Ovules hold the female gamete and develop into a seed after fertilization
what is cross-pollination and why is it important?
transfer of pollen from an anther in a flower on one plant to a stigma of a flower on another plant
promotes genetic variation and evolution
promotes “hybrid vigour”, which is where crosses between genetically unrelated plants tend to be healthy and grow strongly due to having different alleles of many genes rather than being homozygous.
what strategy do
Phyllostachys bambusoides (madake) use the wind for
Vanilla planifolia (vanilla orchid) use Eulaema bees for
adaptations to facilitate transfer of pollen from one plant to another by an outside agent
what strategy do
Zea mays (corn/maize)
Betula papyrifera (paper birch)
use?
separation of anthers and stigmas/styles/ ovaries in separate male and female flowers on the same plant
what strategy do Ginkgo biloba (ginkgo tree) and Urtica dioica (stinging nettle) use?
separation of anthers and stigmas/styles/ ovaries in separate male and female flowers on different plants
what strategy do Nelumbo nucifera (sacred lotus) (protogynous) and Digitalis purpurea (foxglove) (protandrous) use?
anthers and stigmas maturing at different times
protandry = anthers first
protogyny = stigma first
what is self-incompatibility in plants?
mechanisms that increase genetic variability by making plants with alleles that cannot pollinate plants with the same alleles
how is puberty controlled through hormone secretion (gonadotropin-releasing and steroid sex hormones)?
characteristics of spermatogenesis
number of gametes from 1 meiosis: 4
rate of production: millions per day
released during ejaculation
timing of production and release of gametes: produced from puberty onwards, taking about 75 days, and released during ejaculation
amount of cytoplasm: sperm have little cytoplasm, helping them to swim faster
characteristics of oogenesis
number of gametes from one meiosis: 1
rate of production: 1 per month usually
released at ovulation, on about Day 14 of the menstrual cycle
timing of production and release: production initiated in female foetuses and completed during the menstrual cycle, with release on about Day 14, from puberty onwards until menopause
amount of cytoplasm: eggs contain more cytoplasm than any other human cell to provide food reserves for the embryo
what is the acrosome reaction?
acrosome: large membrane-bound sac of enzymes in the head of a sperm.
zona pellucida: coat of glycoproteins that surrounds and protects the egg.
Sperm bind to specifc glycoproteins in the zona pellucida.
Triggers release of the contents of their acrosome.
Enzymes from the acrosome start to digest the glycoproteins, weakening the zona pellucida.
Sperm can generate enough force to make it inside
what is the cortical reaction?
(cortical granules: enzyme-containing vesicles located near the egg cell’s plasma membrane)
nucleus of the first sperm penetrates the zona pellucida enters the egg
fertilizes and activates the egg
the cortical granules move to the plasma membrane of the egg cell and release their contents by exocytosis
the released enzymes cause a general toughening of the zona pellucida making it very difficult for any more sperm to penetrate it
enzymes also change specific glycoproteins in the zona pellucida to which sperm bind, so this can no longer happen.
how is hCG used to detect pregnancy
0-10 weeks: hCG stimulates the corpus luteum
to develop and to secrete progesterone (as it prevents break down of uterine lining)
8-12 weeks: the placenta starts to secrete progesterone in response to hCG
corpus luteum stops hormone production
and breaks down
trophoblast cells in the placenta continue to secrete hCG throughout pregnancy
stimulates progesterone secretion
by placenta cells and maintains the endometrium
how are monoclonal antibodies used in hCG pregnancy tests?
tip of the test stick is dipped in a urine sample
the urine (may contain hCG), is drawn down the centre of the stick.
As the urine moves, it first meets antibodies with blue dye bound to them.
Any hCG binds to the antibodies and the antibodies move on with the urine.
Further down inside the stick, immobilized antibodies trap any passing hCG, which already has antibody plus blue dye attached, so a blue band develops at this point.
Even further down inside the stick, different immobilized antibodies trap any passing antibodies that are not carrying hCG plus dye, so a blue band develops.
Two blue bands = positive, 1 blue band = negative
what is the makeup of the placenta?
The placenta is made of foetal tissues, contact w/ maternal tissues in the uterus wall.
The foetus also develops the amniotic sac (membrane).
This contains amniotic fluid, which supports and protects the developing foetus.
The basic functional unit of the placenta is foetal tissue called a placental villus.
they increase during pregnancy deal with fetus-mother exchange of materials