D3.3 Kidney HL
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
State two functions of the kidney
Unit for Osmotic Concentration:
Production of hormones: The kidneys produce hormones that help regulate various body functions, including erythropoietin for red blood cell production and renin for blood pressure control.
Control of blood pressure: The kidneys play a role in regulating blood pressure, largely through the renin-angiotensin-aldosterone system (RAAS).
Unit for Osmotic Concentration:
osmoles per litre (Osm/L) or milliosmoles per litre (mOsm/L).
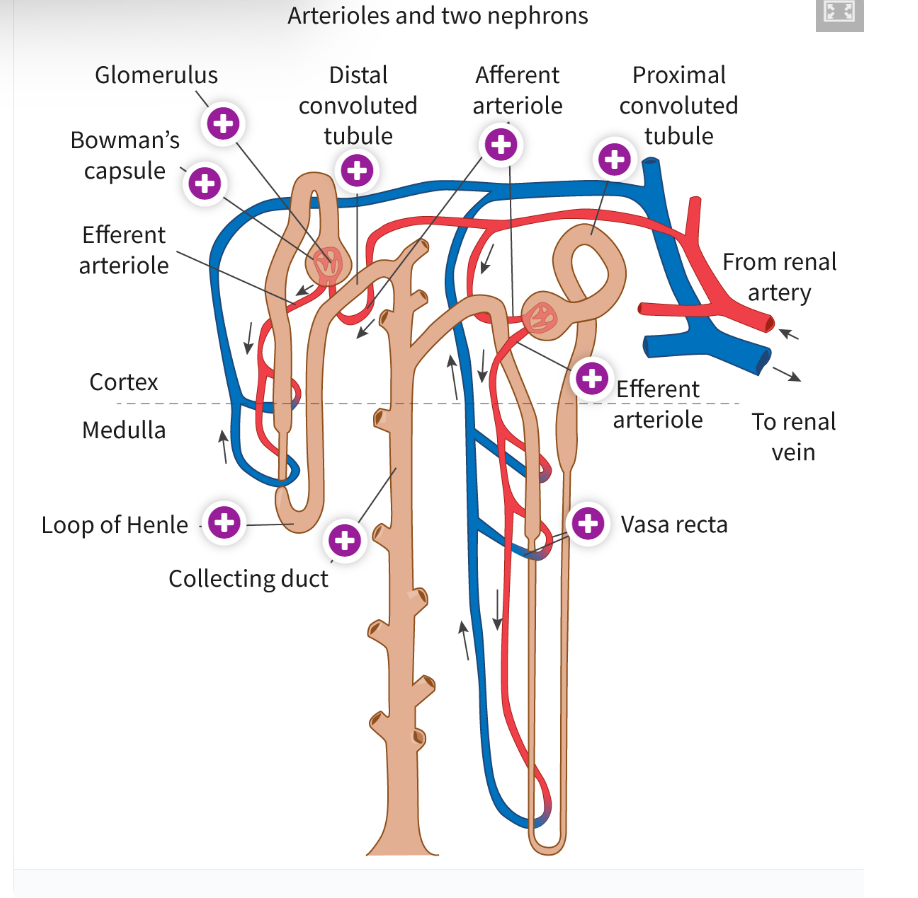
Structure of a Kidney Nephron:
Bowman's Capsule: The initial structure where blood filtration begins.
Glomerulus: A network of capillaries inside the Bowman's capsule where ultrafiltration takes place.
Proximal Convoluted Tubule (PCT): A twisted tube where most reabsorption of nutrients like glucose and amino acids occurs.
Loop of Henle: Involved in concentrating urine by reabsorbing water and salts.
Distal Convoluted Tubule (DCT): Further reabsorption and secretion of ions.
Collecting Duct: Collects urine and plays a role in water reabsorption.
Processes of Osmoregulation and Excretion in a Kidney Nephron
Ultrafiltration: Blood is filtered in the glomerulus, with small molecules (e.g., glucose, salts, urea) passing into the Bowman’s capsule, while larger molecules (e.g., proteins, blood cells) are retained.
Reabsorption: Essential nutrients, water, and ions are reabsorbed in the PCT, Loop of Henle, and DCT into the blood.
Secretion: Waste products like hydrogen ions and potassium are secreted into the nephron.
Excretion: The remaining filtrate, containing waste products and excess water, is excreted as urine.
Process of Ultrafiltration at the Glomerulus and Bowman’s Capsule
Blood enters the glomerulus under high pressure.
The fenestrations (small pores) in the capillaries allow small molecules and water to pass through into the Bowman’s capsule, but larger molecules (like blood cells and plasma proteins) are retained due to the size-selective barrier of the basement membrane and podocytes.
The pressure forces the filtrate (a solution of water, ions, glucose, urea, etc.) into the Bowman’s capsule.
Definition of Filtrate
The fluid that passes from the blood into the Bowman’s capsule during ultrafiltration, containing water, ions, small molecules, and waste (e.g., urea), but lacking blood cells and large proteins.
Why Plasma Proteins and Blood Cells Are Not Part of Glomerular Filtrate:
Plasma proteins and blood cells are too large to pass through the fenestrations of the glomerular capillaries or the selective filtration slits formed by the podocytes.
The basement membrane further restricts their movement into the filtrate.
Process of Selective Reabsorption at the Proximal Convoluted Tubule
Active Transport: Sodium ions (Na+) are actively transported out of the proximal convoluted tubule cells into the surrounding capillaries using ATP. This creates an electrochemical gradient.
Secondary Active Transport: Glucose, amino acids, and other small molecules are reabsorbed via co-transport with Na+. As Na+ is actively transported out, these substances move against their concentration gradient into the cells and then into the bloodstream.
Facilitated Diffusion: Glucose and amino acids, once inside the tubule cells, diffuse into the blood through specific carrier proteins, following their concentration gradient.
Osmosis: The reabsorption of Na+ and other ions creates an osmotic gradient, causing water to move passively from the filtrate back into the bloodstream.
Microvilli: The epithelial cells of the proximal convoluted tubule have microvilli, increasing surface area to maximize absorption efficiency.
Reabsorption of Key Substances: All glucose, amino acids, and most ions (Na+, K+, Cl-) are reabsorbed, ensuring the body retains essential nutrients and maintains osmotic balance
If a healthy person’s filtrate sample from the Bowman’s capsule contains 0.2 mg/100 ml glucose, estimate the concentration of glucose (mg/100ml) in the same sample at the end of proximal convoluted tubule. Give your answer in numerals only.
0 as Glucose is reabsorbed 100% in the proximal convoluted tubule.
Compare the location and osmotic concentrations of the kidney cortex and medulla.
Cortex: Located on the outer part of the kidney, with an osmotic concentration of 300 mOsm/L, similar to other body fluids, supporting filtration processes.
Medulla: Located deeper within the kidney, beneath the cortex, with an osmotic concentration that increases from 300 mOsm/L near the cortex to 1200 mOsm/L at the core.
State the overall function of the loop of Henle.
Concentrates urine by establishing a gradient of osmotic concentration in the medulla.
Describe the structure and function of the descending limb of the loop of Henle.
Structure: Permeable to water; no sodium transport.
Function: Water reabsorbed passively into surrounding hyperosmotic tissue due to osmotic gradient.
Describe the structure and function of the ascending limb of the loop of Henle.
Structure: Impermeable to water; active transport of Na+, Cl-, K+ ions.
Function: Solutes actively transported out, decreasing urine solute concentration
Outline the effects of dehydration and hyperhydration on the osmotic concentration of blood.
Dehydration: Blood osmolarity increases, triggering ADH release.
Hyperhydration: Blood osmolarity decreases, inhibiting ADH release.
Outline the regulation of blood osmotic concentration
Chemoreceptors in hypothalamus detect osmolarity changes.
ADH released from pituitary to regulate water reabsorption.
ADH increases aquaporins in collecting ducts, aiding water reabsorption.
Explain how the collecting ducts of the kidney increases or decreases the blood osmotic concentration.
Condition | Response | Effect on Collecting Ducts | Effect on Urine |
Increasing Blood Osmolarity (Dehydration) | High solute concentration in blood detected by osmoreceptors in the hypothalamus. | ADH released from posterior pituitary; collecting ducts become more permeable to water (aquaporins increase). | More water reabsorbed; urine volume decreases, concentrated. |
Decreasing Blood Osmolarity (Overhydration) | Low solute concentration in blood detected by osmoreceptors in the hypothalamus. | Reduced ADH secretion; collecting ducts become impermeable to water. | Less water reabsorbed; urine volume increases, diluted. 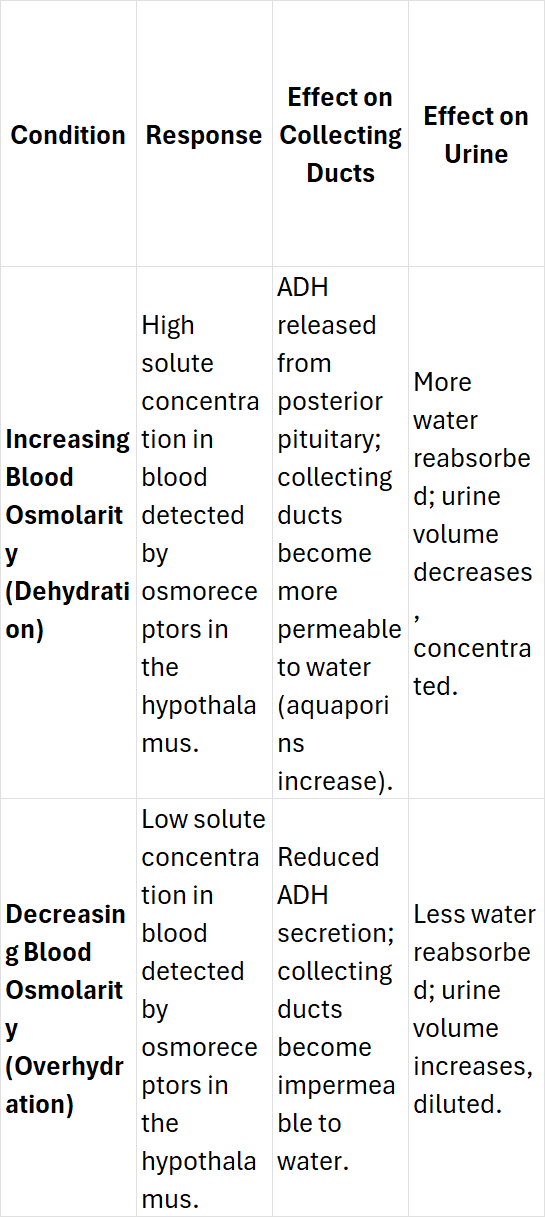 |
Outline the effects of low and high blood solute concentration on urine volume, urine solute concentration, and water reabsorption in the kidney.
Condition | Urine Volume | Urine Solute Concentration | Water Reabsorption |
Low Blood Solute Concentration | High | Low | Decreased in distal convoluted tubule/collecting duct |
High Blood Solute Concentration | Low | High | Increased in distal convoluted tubule/collecting duct 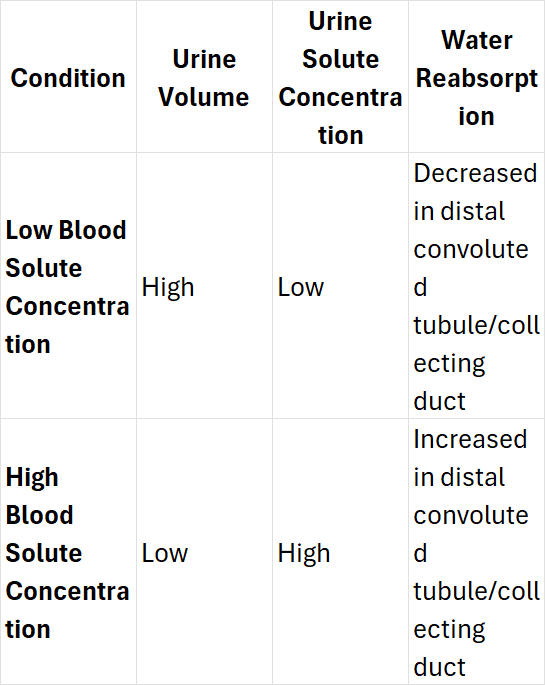 |
Outline benefits of regulating blood supply to organs in response to changes in activity.
Ensures optimal oxygen/nutrient supply and waste removal based on activity.
Outline the cause and consequences of vasoconstriction and vasodilation.
Process | Cause | Consequence |
Vasoconstriction | - Triggered by signals from the nervous system and hormones (e.g., norepinephrine, angiotensin). | - Blood vessels narrow, reducing blood flow to certain organs. |
- Occurs during stress, cold exposure, or when blood flow needs to be redirected. | - Reduces heat loss, prioritizes oxygen supply to vital organs (e.g., brain, heart). |
Compare blood flow to skeletal muscle, gut, brain, and kidneys during sleep, vigorous physical activity, and wakeful rest.
Organ | Sleep | Vigorous Physical Activity | Wakeful Rest |
Skeletal Muscle | - Blood flow is low, as muscles are inactive. | - Blood flow increases significantly to provide oxygen and nutrients for muscle contraction. | - Blood flow is moderate, depending on the level of physical activity. |
Gut | - Blood flow is relatively high to support digestion. | - Blood flow decreases as more blood is directed to active muscles. | - Blood flow is moderate, supporting normal digestion processes. |
Brain | - Blood flow remains steady to maintain normal brain function, but slightly reduced. | - Blood flow increases to provide oxygen for higher brain activity and processing. | - Blood flow is steady, supporting normal cognitive functions. |
Kidneys | - Blood flow is moderate as kidney function is less critical during sleep. | - Blood flow is reduced, as the body's priority shifts to muscles and other active organs. | - Blood flow is moderate, supporting filtration and homeostasis processes. |