
Looks like no one added any tags here yet for you.
purpose of microscopic examination
to detect and ID insoluble materials present in urine
items that contribute to formed elements include:
blood
kidney
lower genitourinary tract
external contamination
the formed elements within urine can include:
RBCs
WBCs
epithelial cells
bacteria
yeast
parasites
spermatozoa
mucus
casts
crystals
artifacts
what is microscopic examination of urine MOST COMMONLY used to detect?
renal disease and/or urinary tract disease
when is microscopic examination MOST necessary? q
abnormal findings present on chemical/physical analysis
requested by physician based on patient’s condition/history
lab specified population being tested
pregnant women
pediatric or geriatric
immunocompromised
renal patients
first procedure used to standardize quantitation of formed elements in urine; utilized a hemocytometer to count numbers of cells in a 12 hr urine specimen
Addis count
specimen requirements for microscopic examination
freshly voided specimens are preferred; 10-15 mL is optimal; formed elements can disintegrate rapidly in dilute or alkaline urines (RBCs, WBCs, and hyaline casts)
what should you do if microscopic examination of urine is delayed?
refrigerate if it cannot be performed within 2 hours
refrigeration may cause precipitation of amorphous urates and phosphates and nonpathogenic crystals; warm specimen back to RT to dissolve crystals before examination
specimen prep for microscopic analysis
centrifuge specimen in the conical tube at 2,000 RPM for 5 min; decant supernatant with a pipette; leave 1 mL of sediment; resuspend for equal distribution by gentile agitation; examine sediment
microscopic examination of urine:
count at least 10 fields on both low (10X) and high (40X) power
examine under LPF first to detect/count casts and obtain general composition of sediment
NEXT, examine/enumerate other formed elements on HPF
how are RBC reported?
#RBCs/hpf
how are WBCs reported?
#WBCs/hpf
how are casts reported?
#casts/lpf (notice, low power field is where casts are counted)
how are epithelial cells, crystals, and other elements reported that aren’t RBCs/WBCs/casts?
semiquantitative terms (rare, few, moderate, many OR 1+, 2+, 3+, 4+)
what should be done w/ microscopic results that do not correlate w/ physical/chemical tests?
results should be rechecked for technical/clerical errors
color signifiance
usually pertaining to blood
clarity signifiance
can help distinguish hematuria vs hemoglobinuria/myoglobinuria; can also help confirm pathological vs nonpathological cause of turbidity
.
significance of blood in screening tests
presence of blood/RBC casts
protein significance
can indicate casts/cells present
nitrite significance
bacteria/WBCs present
leukocyte esterase significance
WBCs/WBC casts/Bacteria present
glucose significance
yeast (among other things)
purpose of sediment stains
increase overall visibility of sediment elements being examined using bright-field microscopy — can impart identifying characteristics to cellular structures, such as nuclei, cytoplasm, and inclusions
stains — action/function: sternheimer-malbin (made of crystal violet and safranin O)
delineates structure/ contrasting colors of nucleus and cytoplasm; ID’s WBCs, casts, and epithelial cells
stains — action/function: toluidine blue
enhances nuclear detail; differentiates WBCs from renal tubular epithelial cells
stains — action/function: 2% acetic acid
lyses RBCs and enhances nuclei of WBCs; distinguishes RBCs from WBCs, yeast, oil droplets, and crystals
stains — action/function: lipid stains — oil red O and sudan III
stains trigs and neutral fats orange-red; ID’s free fat droplets and lipid-containing cells/casts (does NOT stain cholesterol)
stains — action/function: gram stain
differentiates GP and GN bacteria; ID’s bacterial casts
stains — action/function: hansel stain
methylene blue and eosin Y stains eosinophilic granules; ID’s urinary eosinophils
stains — action/function: prussian blue stain
stains structures containing iron; ID’s yellow-brown granules of hemosiderin in cells/casts
phase contrast purpose in UA
enhances visualization w/ low refractive indices
polarizing microscopy purpose in UA
aids in ID of oval fat bodies, fatty casts, and crystals
bright field microscopy purpose in UA
used for routine UA, must examine the sediment under reduced light
dark field microscopy purpose in UA
enhances visualization of specimens that cannot be easily seen w/bright field microscope; aids in the ID of Treponema pallidum
Fluorescence microscopy purpose in UA
allows visualization of naturally fluorescent microorganisms or those stained by fluorescent dye
interference-contrast microscopy purpose in UA
produces a 3D image and layer-by-layer imaging
normal RBC urine sediment
0-3/hpf
normal WBC urine sediment
0-8/hpf
hyaline casts normal urine sediment
0-2/lpf
what factors must be considered when looking at microscopic results?
recent stress
exercise
menstrual contamination
presence of other sediment constituents
etc.
the primary stain of UA sediments
Sternheimer-malbin stain
RBCs appear as…
smooth, nonnucleated, biconcave disks measuring about 7 microns in diameter; they are ID’d using hpf objective and reported as an average of 10 fields
concentrated (hypersthenic) urine may demonstrate RBCs that appear _______ due to loss of water/shrinkage
crenated
in dilue (hyposthenuria) urine, RBCs absorb water, swell, and lyse rapidly, releasing _____ and leaving only the cell membrane. these largely empty cells are called _____ cells — these cells can be easily missed if specimens are not examined under reduced light
hemoglobin; ghost (cells)
hematuria causes what color of urine?
red to brown cloudy urine
what are RBCs easily confused with?
yeast cells, oil droplets, and air bubbles
RBCs are susceptible to lysis w/ addition of which substance?
acetic acid

yeast

oil droplet
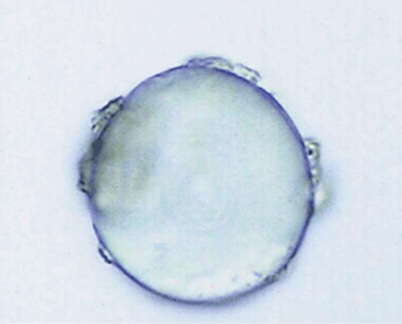
air bubble
dysmorphic RBCs…
vary in size; have cellular protrusions or fragments
large number assoc w/ glomerular bleeding
acanthocyte w/ multiple protrusions is most associated
demonstrated after strenuous exercise, indicating glomerular origin
caused by differences in urine conc…
RBCs lyse most rapidly in what type of urine?
dilute, alkaline urine

normal vs ghost RBC

created RBC vs. normal RBC from a side view
what are ways RBCs can be differentiated from other sediment features?
refractivity of oil droplets/air bubbles — can be seen w/ fine focus adjustment up and down; they may also appear in a different plane from other constituents
rough, crenated RBCs may resemble WBCs, but they are generally much smaller
acetic acid to lyse RBCs — everything else remains in tact
budding of yeast present
supravital staining
presence of RBCs in urine is associated w/ damage to…
the glomerular membrane
vascular injury within the genitourinary tract
true or false: number of RBCs present in urine indicates the extent of damage/injury
TRUE
RBCs detected in urine can aid in early diagnosis of what? what else is it associated with?
early diagnosis for:
glomerular damage
malignancy of the urinary tract
confirm presence of renal calculi
also assoc. w/:
trauma
acute infection
inflammation
coagulation disorders
contamination
exercise
characteristics of MACROscopic hematuria:
urine appears cloudy w/ red to brown color
>100 RBCs/hpf
associated w/ advanced glomerular damage
also seen with damage to vascular integrity of the urinary tract caused by trauma, acute infection, or inflammation
also associated with coagulation disorders
characteristics of MICROscopic hematuria:
can be critical to the early diagnosis of glomerular disorders and malignancy of the urinary tract as well as to confirm the presence of renal calculi
may also see hyaline, granular and RBCs casts following strenuous exercise
can be seen with nonpathological or pathological origins
menstrual contamination can also be associated
predominant WBC found in urine
neutrophils
WBCs vs RBCs
larger than RBCs, measuring an average of 12 microns in diameter; nucleated
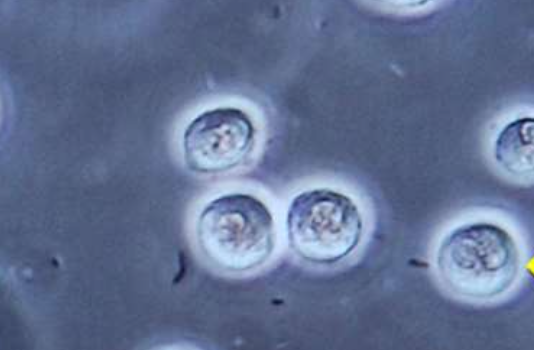
what type of urine can lyse neutrophils?
dilute, alkaline urine
what type of movement is seen in the granules of neutrophiles when they swell from hypotonic urine
Brownian movement
what are glitter cells?
when the neutrophils produce a ‘sparkling appearance’ from the Brownian movement of their granules in hypotonic urine; not clinically significant
what stain can be used for urine eosinophils?
Hansel stain (wright’s or Giemsa can also be used, but are not preferred)
are eosinophils normally found in urine?
NO
what % of urine eos is signifiant?
more than 1% out of 100-500 cells counted is considered significant
when can urine eosinophils be seen?
drug-induced interstitial nephritis
UTI
renal transplant rejection
what can be done to differentiate mononuclear cells from RTE cells in urine sediment?
supravital staining
addition of acetic acid for nuclear clarity
cytodiagnostic urine testing
higher amounts of WBCs are seen in men or women?
women
WBCs and RBCs may enter the urine through ____ or _____ trauma, but they can also enter through amoeboid action…
glomerular or capillary
what type of action do WBCs use to migrate through tissues to sites of infection?
amoeboid action
pyuria
increased WBCs in urine; indicates infection or inflammation in the genitourinary system
bacterial infections associated w/ pyruria include:
pyelonephritis (kidney)
cystitis (bladder)
prostatitis
urethritis
non-bacterial inflammation associated with pyruria includes:
glomerulonephritis (post-strep infection antibody complexes deposit)
lupus erythematosus
interstitial nephritis
tumors
epithelial cells can be found in the urine normally, as long as they are not present in large numbers or abnormal forms; they represent normal sloughing of old cells. the three types of epithelial cells seen in urine include:
squamous
transitional (urothelial)
renal tubular
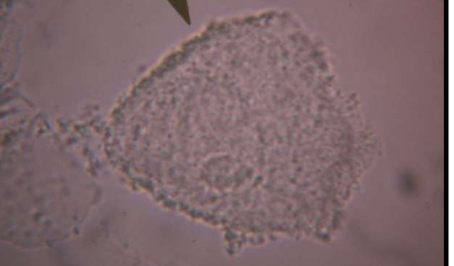
squamous epithelial cells

largest found in urine sediment; may contain abundant, irregular cytoplasm and a prominent nucleus about the size of an RBC; may be folded; may resemble casts; disintegrate in old urine; a few can normally be found in urine; usually reported as rare, few, moderate, or many
where do squamous epithelial cells originate from?
linings of the vagina and female urethra and the lower portion of the male urethra; represent normal cell sloughing and have no pathological significance; inc amounts seen more frequently in female urine — this is why clean catch urine is preferred…
what form of squamous epithelial cells HAS clinical significance?
clue cells
clue cell…
variation of squamous epithelial cells; clinical significance: indicative of vaginal infection by a bacterium known as Gardnerella vaginalis.
Appears as squamous epithelial cell covered w/ coccobacillus organism; routine testing is ID’d by vaginal wet preparation; small numbers of clue cells may be present in urinary sediment
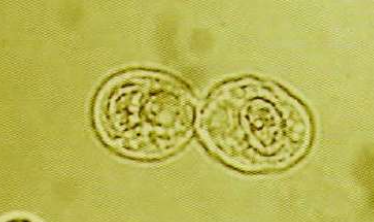
AKA urothelium or uroepithelium; this type of epithelium that lines much of the urinary tract, including the renal pelvis, the ureters, the bladder, and parts of the urethra; they are smaller than squamous cells and appear in various forms due to their ability to absorb large amounts of water. the three forms include: ________,________, and _________. all forms have a distinct, ______ located nuclei.
spherical
polyhedral
caudate
CENTRALLY (located nuclei)
transitional epithelial cells presence in urine
present in small numbers in normal urine — represent normal cell sloughing; increased numbers seen singly, in pairs, or in clumps — present following invasive urologic procedures, such as cetherization or cytoscopy
syncytia
group of cells with/ continually joining cell walls
transitional epithelial cells have no clinical significance unless morphologically abnormal, such as…
vacuoles or irregular nuclei that may indicate malignancy or viral infection

polyhedral transitional epithelial cell

spherical transitional epithelial cell

caudate transitional epithelial cell
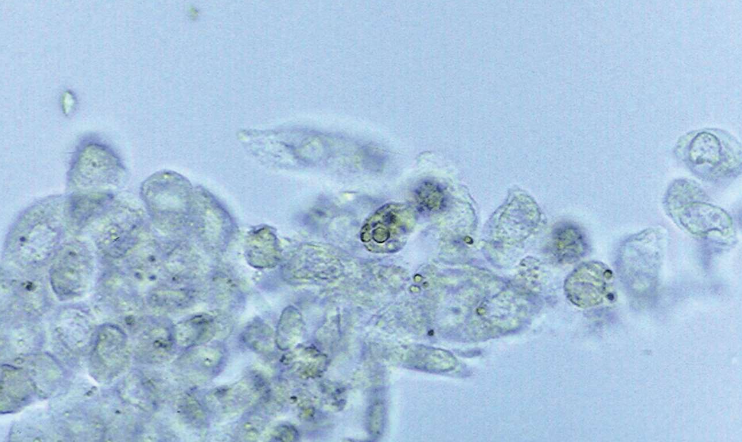
syncytia (transitional)
are RTEs normally found in urine in any circumstances?
NO
what is the criterial for calling something an RTE?
nucleus present
large and eccentric nucleus
RTE cells come from various areas of the ______, and they vary on size and shape depending on which area they come from
tubules
RTEs that originate from the proximal convoluted tubule
large and rectangular w/ coarse granular cytoplasm; referred to as columnar or convoluted cells often resembling casts
RTEs from the distal convoluted tubule
cells are smaller and round to oval; mistaken for WBCs and spherical transitional epithelial cells
RTEs of the collecting duct
cuboidal and are NEVER round; has at LEAST one straight edge; may occur in groups of three or more called renal fragments

more than 2 RTEs/hpf indicates what type of injury?
tubular injury
increased numbers of RTEs indicate necrosis of the renal tubules with the possibility of it affecting overall renal function:
heavy metal exposure
drug-induced toxicity
hemoglobin/myoglobin toxicity
viral infections (i.e., hep b)
pyelonephritis
allergic reactions
malignant infiltrations
salicylate poisoning
acute allogenic transplant rejection
also seen as secondary effects of glomerular disorders
renal fragments (groups of RTEs) represent…
severe tubular injury w/ basement membrane disruption
since RTEs funciton to reabsorb glomerular filtrate, it can absorb things such as…
bilirubin
hemoglobin —> hemosiderin granules (prussian blue can pick up)
lipids
oval fat bodies are..
RTEs that have absorbed lipids present in the glomerulus…