The kidneys
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
54 Terms
what is the kidney responsible for ?
Its responsible for filtering blood and controlling water balance
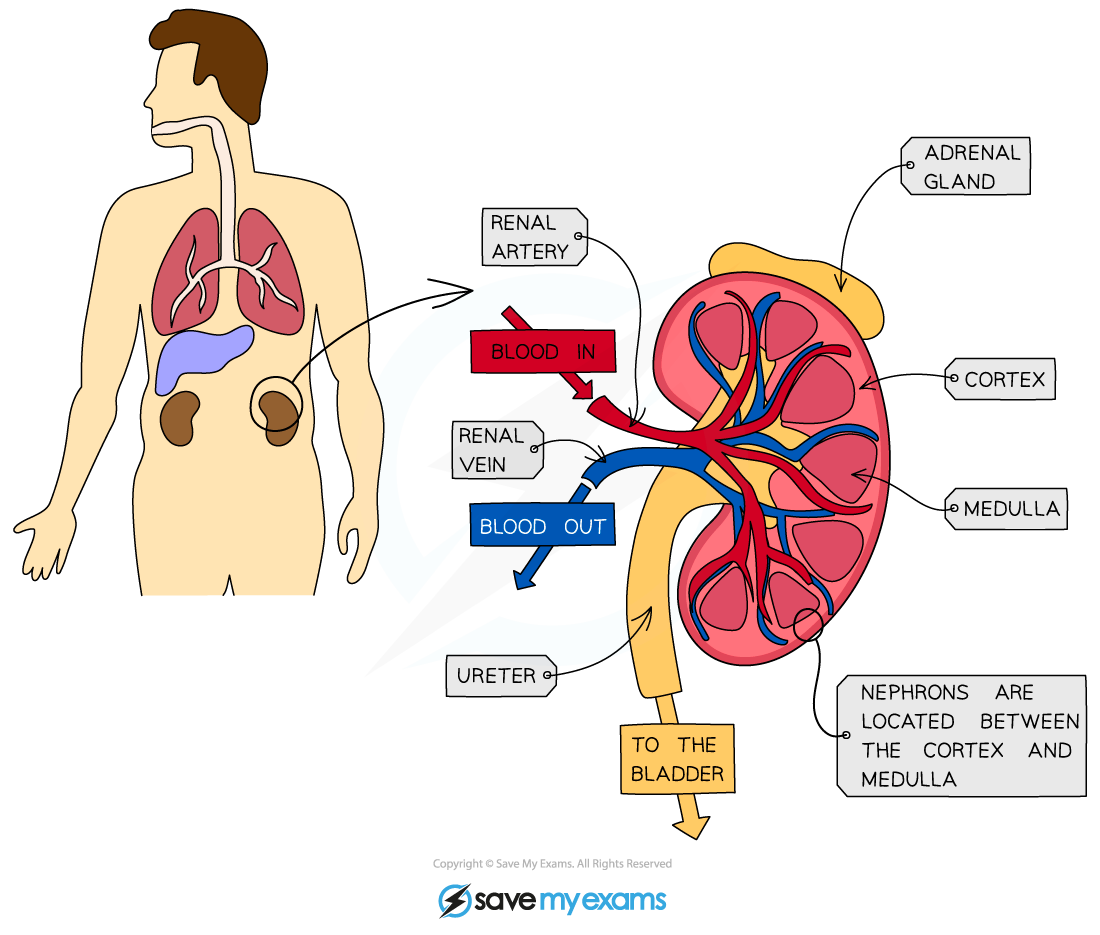
Draw a diagram of the gross morphology
what does the term ultrafiltration means ?
Filteration at the kidneys removes glucose, amino acids , water and urea from the blood. Or any molecule that’s smaller than 69,000 kDa, will be filtered out of the blood.
It occurs in the nephrons
where do we find the nephrons ?
The nephrons is mainly in the renal cortex with loops of henlé snd collecting ducts extending into the renal medulla
where does the collecting ducts join together ?
The collecting ducts all join together at the pelvis , where urine flows out of the kidneys into the bladder via the ureters.
what are the functions of the renal artery ?
takes blood to the kidney, caries oxygenated blood , rich in dissolved substances including the urea from deamination of amino acids via the ornithine cycle in hepatocytes.
Divides to form arterioles and capillaries which form glomeruli in the renal cortex. the blood is filtered under pressure with the kidneys filtering approx 180 dm3 of blood per day. ← Selectively reabsorbed
The nephron - ultrafiltration
what is the definition of ultrafiltration ?
Is the filtering of blood at the molecular level. Blood entering the glomerulus through the afferent arteriole, which is wider than efferent arteriole that carries blood away from the glomerulus.
what is the function of the Bowman’s capsule ?
The contents of the blood are pushed out of the blood by glomerulus into the bowman’s capsule.
what is consist between the blood in the lumen of capillaries of the glomerulus and the bowman’s capsule ?
3 layers
Endothelium of the capillary
Basement membrane
Epithelium of the Bowman’s capsule
Layer: what is the Endothelium of the capillary
Is a narrow gaps allow blood plasma and dissolved substances to leave the capillary, Cells of the endothelium also contain pores.
what is fenestrations ?
Cells of the endothelium that contain pores.
Layer: what is the Basement membrane
It’s a fine mesh of collagen and glycoproteins. The mesh acts as a filter. Anything substances greater than 69,000 KDa or RMM ( Relative molecular mass) cannot pass through the basement membrane thus stays in the blood.
Layer: what is the Epithelium of the Bowman’s capsule
Specialised cell called Podocytes, have specialised extensions called major processes. They provide space for ultrafiltration.
what substances will pass out of blood at the glomerulus into the bowman’s capsule .
Water, amino acid, glucose , vitamin + mineral ions , Urea , small proteins
what does the bowman’s capsule contains ?
Bowman’s capsule contains filtrates
What are the key structure of the human kidney nephron ?
Efferent and Afferent arteriole.
Glomerulus
Bowman’s capsule
Proximal convoluted tubule
Loop of henlé
Distal convoluted tubule
Collecting duct
add pic of nephron
Selective reabsorption in the nephron
what does the term selective reabsorption means ?
Use substances such as glucose, amino acid , water etc are reabsorbed back into the blood via proximal convoluted tubule passes through the blood capillaries.
Draw a diagram of the mechanism of selective reabsorption
add pic
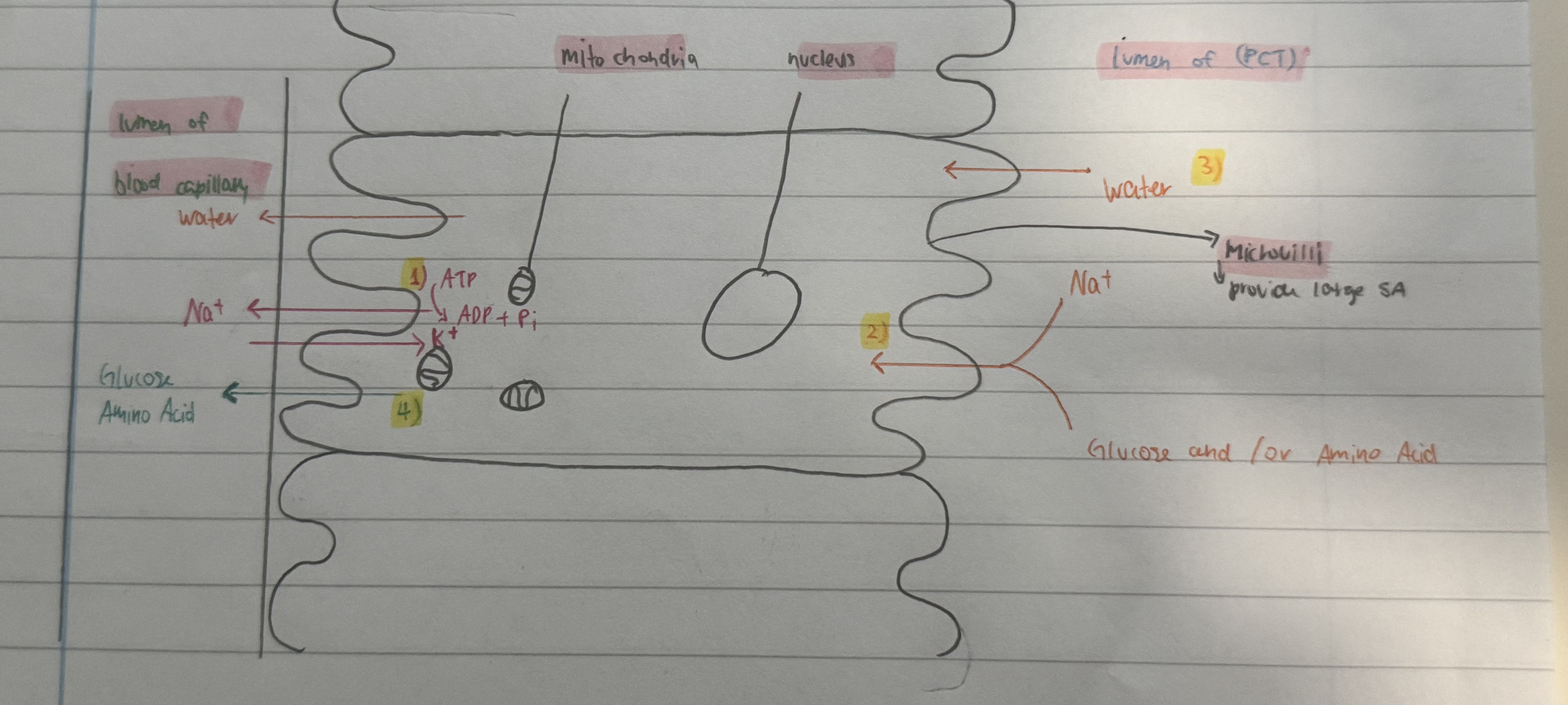
Stage 1 of selective reabsorption
Sodium ions Na + are actively pumped out of the cells lining PCT into the blood capillary, in term this lowers the concentration of Na+ in the cells.
Stage 2 of selective reabsorption
Na+ diffuses into the cells lining the PCT down a concentration gradient via a cotranpsort protein.
As the Na+ moves into the cells, glucose or amino acids also moves in via by facilitated diffusion.
Stage 3 of selective reabsorption
The movement of Na+, glucose and amino acids into the cells reduces the water potential. Thus water moves into the by osmosis down a concentration gradient.
Stage 4 of selective reabsorption
Glucose and amino acids now diffuses out of the cells lining the PCT into the blood plasma in the capillary
what is the structure called that lines on the cells lining the PCT
Microvilli
what are the functions of microvilli
It provide large surface area / increases the SA for effective reabsorption.
what are the filtrates that enters the PCT contains ?
Water, urea, glucose , amino acids, Na+ / Cl- , small soluble substances, small hormones , mineral ions, vitamins .
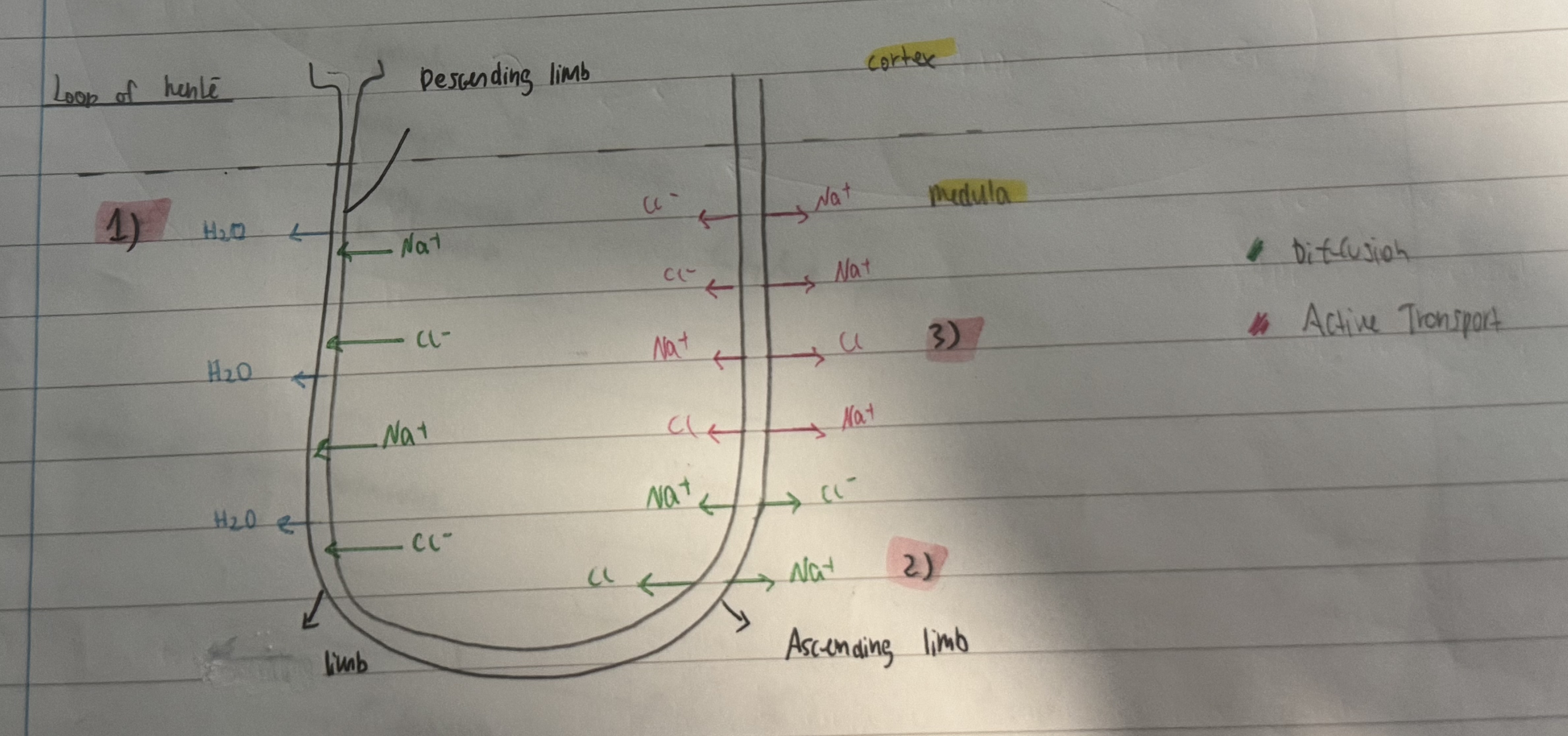
The nephron - Loop of henlé
what are the main functions of the loop of hence
Produce a Lowe water potential in the medulla of the kidney, by acting as a countercurrent multiplier to produce concentration gradient .
Concentrate urine and conserve water by creating an osmotic gradient in the kidney’s medulla.
To make the medulla salty
what are the main 2 part of the loop of heel ?
Descending and Ascending limb
what does the filtrate contains when its enters the descending limb ?
Water, Na+, Cl-, urea , and other substances not selectively reabsorbed
Stage 1 of loop of hence function
The filtrate entering the descending limb is a dilute solution of mineral ions ( Na+ and Cl-. The medulla has a lower water potential than the filtrate so water moves out by osmosis.
Na+ and Cl- diffuse into the descending limb down their diffusion gradient from the salty medulla into the filtrate. = Water potential of of the descending limb decrease further into the medulla.
Stage 2 of loop of hence function
At the start of the ascending limb Na+ and Cl- diffuse into the medulla from the filtrates.
Stage 3 of loop of hence function
The ascending limb is impermeable to water, Na+ and Cl- are actively pump put of the filtrate into the upper part of the ascending limb.
Outcome of this process is to make the medulla salty, this allows effective water reabsorption from the collecting duct.
Draw a diagram of the Loop of henlé
Collecting duct & ADH - The nephron
where is the collecting duct ?
In the renal medulla
What does ADH refers to ?
Antidiuretic hormone
Where does the filtrate goes after the loop of henlé ?
the filtrate leaves the ascending limb of the loop of henlé enters the distal convoluted tuble ( DCT )
What happens in the DCT ?
At the DCT, Na+ and Cl- are reabsorbed , other mineral ions balance ( Ca2+ , Mg2+ , K+) is regulated with the majority being reabsorbed.
what happens to the filtrate after DCT ?
The filtrate enters the collecting duct.
where does the collecting duct passes through ?
The collecting duct passes through the medulla.
What happens in the collecting duct ?
Water can be reabsorbed into the capillaries of the medulla by osmosis.
what does this process requires - “Water can be reabsorbed into the capillaries of the medulla by osmosis. “
This process requires the presence of scientific water channel proteins called “ Aquaporins “
what are the functions of Aquaporins ?
specific channel proteins that allow water to move rapidly across cell membrane through facilitated diffusion.
The role of ADH
what is other term for water potential?
Osmotic potential
how is the osmotic potential being monitored ?
The osmotic potential of the blood is monitored by the osmorecptors in the hypothalamus of the brain.
What happens when the water potential of the blood is low ?
The osmorecptors lose water by osmosis and shrink.
what is linked after the shrinkage ?
this stimulates specialise neurosecretory cells which produce and secrete ADH, into the blood of the posterior pituitary gland .
What does the ADH do ?
ADH travels in the blood and binds to ADH receptors on the cell surface membrane of the collecting duct. The bind of ADH to its receptors, causes vesicles containing aquaporins to move and fuse with the cell surface membrane.
What happens to the cells of the collecting duct ?
It becomes “ more permeable “ to water , more water will be reabsorbed out of the filtrate by osmosis. =) Smaller volume of more concentrated urine and less water loss.