Lower GI Disorders: Nursing Care and Interventions
1/143
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
144 Terms
What are the common diagnostics tests for lower GI disorders?
Barium Enemas, Colonoscopy, Abdominal x-ray, CT Scan of Abdomen and Pelvis, Ultrasound of Abdomen, MRI of Abdomen, Stool Specimens, Labs (CBC, CMP, electrolytes).
What are the common symptoms of lower GI disorders?
Diarrhea, Constipation, Abdominal Pain (acute or chronic), Nausea/Vomiting.
What defines diarrhea in terms of stool frequency?
At least 3 loose or liquid stools a day.
What are some etiologies of diarrhea?
Infectious organisms, food intolerance, contaminated food, medications.
What are the pathophysiological mechanisms involved in diarrhea?
Decreased absorption, increased secretion, motility disturbances, inflammation, combination.
What are the clinical manifestations of acute diarrhea?
Watery stools, abdominal cramping, nausea/vomiting, and sometimes fever.
What diagnostics are used to identify the cause of diarrhea?
Stool specimen analysis, CBC, CMP, ABGs.
What should be checked in stool specimens for diarrhea diagnosis?
Blood, mucous, WBCs, culture, O & P, and C. Diff.
What nursing assessments are important for patients with diarrhea?
History and physical assessment, stool assessment, food intake, medications, dehydration, and infection.
What are the nursing interventions for managing diarrhea?
Oral or IV fluids/electrolyte replacement, administer antidiarrheal medications or antibiotics with caution.
Why should antidiarrheal medications be used with caution?
They should not be used if the diarrhea is caused by an infectious disease.
What patient teaching is important for diarrhea management?
Infection control, good handwashing, proper food handling, and completing antibiotics.
What nursing diagnoses might be relevant for a patient with diarrhea?
Hypotension, electrolyte imbalances, acid-base imbalance.
What is C. Diff and why is it significant?
Clostridium Difficile is a hazardous bacterial infection that causes severe diarrhea.
What are the risk factors for C. Diff infection?
Infection control issues, highly infectious nature, healthcare-associated infection.
What precautions should be taken for C. Diff patients?
Contact precautions and strict hand hygiene.
What antibiotics are used to treat C. Diff?
Oral Vancomycin, Fidamoxicin, or Metronidazole (Flagyl), or IV.
What teaching should be provided to patients and families regarding C. Diff?
Importance of infection control, hand hygiene, and understanding treatment.
What is the importance of prioritizing nursing care for lower GI problems?
To ensure effective management of symptoms, prevention of complications, and optimal patient outcomes.
What is the nursing process in caring for patients with lower GI problems?
Assessment, diagnosis, planning, implementation, and evaluation.
What are the learning objectives for understanding lower GI disorders?
Describe common etiologies, clinical manifestations, diagnostics, and interventions; apply the nursing process; prioritize nursing care.
What is the primary etiology of constipation?
Slowed GI motility.
What are common causes of constipation?
Medications, poor oral fluid and fiber intake, lack of physical activity, ignoring the urge to defecate, anxiety, stress, depression, some diseases, and chronic laxative use.
What are the clinical manifestations of constipation?
Hard, dry infrequent stools that are difficult to pass, abdominal discomfort, distention, bloating, gas pains, rectal pressure, and possibly severe pain.
What is obstipation?
No passage of stool or flatus.
What are some complications of constipation?
Fecal impaction, perforation, rectal ulcers/fissures, hemorrhoids, and diverticulosis.
What diagnostic studies are used for constipation?
Abdominal x-ray (obstruction series), barium enemas, and stool specimen analysis.
What should be assessed in a patient with constipation?
Bowel pattern, diet, exercise, health conditions, and medications, especially laxatives.
What are some collaborative care strategies for constipation?
Increase fiber/fluid intake, exercise, proper positioning, timing, and privacy; use short-term enemas/laxatives, then add bulking agents and stool softeners.
What characterizes acute abdominal pain?
New or recent onset of pain requiring timely, emergent workup and treatment.
What are possible causes of acute abdominal pain?
Appendicitis, bowel obstruction, cholecystitis, diverticulitis, pancreatitis, perforation, peritonitis, ruptured ectopic pregnancy, and ruptured aneurysm.
What assessments are important for acute abdominal pain?
Vital signs monitoring for signs of shock/infection, history and physical examination, pain assessment, and patient positioning.
What diagnostic workup is typically done for acute abdominal pain?
CT abdomen, EKG, CBC, UA, and culture/sensitivity; surgery consult may be needed.
What is the nature of chronic abdominal pain?
Dull, achy pain that is less emergent than acute pain.
What are possible causes of chronic abdominal pain?
Irritable bowel syndrome (IBS), peptic ulcer disease (PUD), chronic pancreatitis, hepatitis, pelvic inflammatory disease, and surgical adhesions.
What is the most common cause of acute abdominal pain?
Appendicitis.
What age group is most commonly affected by appendicitis?
Usually occurs between 10-30 years of age, with 10-19 being the most common.
What is the classic clinical manifestation of appendicitis?
Pain starting at the umbilicus and then moving to the right lower quadrant at McBurney's point, along with rebound tenderness, nausea/vomiting, low-grade fever, and increased pain after coughing/sneezing.
What complications can arise from appendicitis?
Ruptured or perforated appendix, peritonitis, and gangrene.
What is McBurney's point?
The location in the right lower quadrant where pain is typically felt in appendicitis.
What diagnostic workup is used for appendicitis?
X-ray first, then CT scan or ultrasound to check for rupture, along with CBC.
What nursing care is essential for a patient with appendicitis?
Monitor vital signs, maintain NPO status, administer IV fluids and antibiotics, and prepare for surgery (appendectomy).
What are important postoperative care considerations for appendicitis?
Slowly advance diet, encourage early ambulation, use incentive spirometry, and monitor for signs of infection.
What are important diagnoses related to appendicitis?
Risk for shock or sepsis related to ruptured appendix, and acute pain/altered comfort requiring pain management.
What is the primary cause of primary peritonitis?
Usually caused by infections or liver issues such as cirrhosis.
What are the clinical manifestations of peritonitis?
Severe abdominal pain, spasms, shallow respiratory rate, muscle rigidity, abdominal distention, fever, tachycardia, increased respiratory rate, and lower blood pressure.
What complications can arise from peritonitis?
Sepsis, hypovolemic shock, abscess formation, paralytic ileus, and acute respiratory distress.
What diagnostic studies are used for peritonitis?
CT scan or ultrasound of the abdomen, X-ray, CBC, and analysis of peritoneal fluid.
Why is it important to analyze peritoneal fluid in suspected peritonitis?
To check for infection by analyzing WBC count and determining if there is bleeding or infection.
What nursing assessments should be performed for peritonitis?
Assess the abdomen and monitor vital signs for fever, sepsis, or hypovolemic shock.
What are the medical management strategies for peritonitis?
Keep the patient NPO, administer IV fluids, antibiotics, analgesics, NG tube, and anti-nausea medications.
What nursing interventions are important post-surgery for peritonitis?
Drain care, IV fluid support, analgesics, patient teaching, early ambulation, and diet advancement.
What are the signs and symptoms of Irritable Bowel Syndrome (IBS)?
Abdominal pain, diarrhea and/or constipation, abdominal distention, bloating, excessive flatulence, urgency, and feeling of incomplete emptying.
What psychological factors can aggravate IBS?
Stress, depression, anxiety, PTSD, and abuse.
What diagnostic criteria are used to diagnose IBS?
Rome IV or Manning criteria.
What dietary recommendations are suggested for managing IBS?
Adequate fiber intake, increased fluid intake, and avoidance of certain trigger foods.
What is a recommended strategy for patients with IBS to track their symptoms?
Keeping a food/symptom diary to document everything they eat and any symptoms experienced.
What nursing diagnoses might apply to a patient with peritonitis?
Risk of infection, impaired perfusion, and potential respiratory distress due to increased pressure from infected fluid.
What is the significance of shallow respiratory rate in peritonitis patients?
It indicates the patient is trying to avoid movement and pain, which may be associated with severe anxiety.
What are the potential effects of peritonitis on blood pressure?
It can lead to hypotension due to fluid loss and sepsis.
What is the role of analgesics in the management of peritonitis?
To manage pain and improve patient comfort.
What is the purpose of NG tube placement in peritonitis management?
To decompress the stomach and manage symptoms.
What are the signs of severe anxiety in patients with peritonitis?
Muscle rigidity, shallow respiratory rate, and avoidance of movement.
What is the importance of early ambulation post-surgery for peritonitis?
To promote recovery and prevent complications such as pneumonia.
What is the relationship between IBS and food intolerances?
Food intolerances and allergies can trigger or aggravate IBS symptoms.
What is a common psychological intervention for patients with IBS?
Counseling and stress management techniques.
What are the two main types of Inflammatory Bowel Diseases (IBD)?
Crohn's Disease and Ulcerative Colitis.
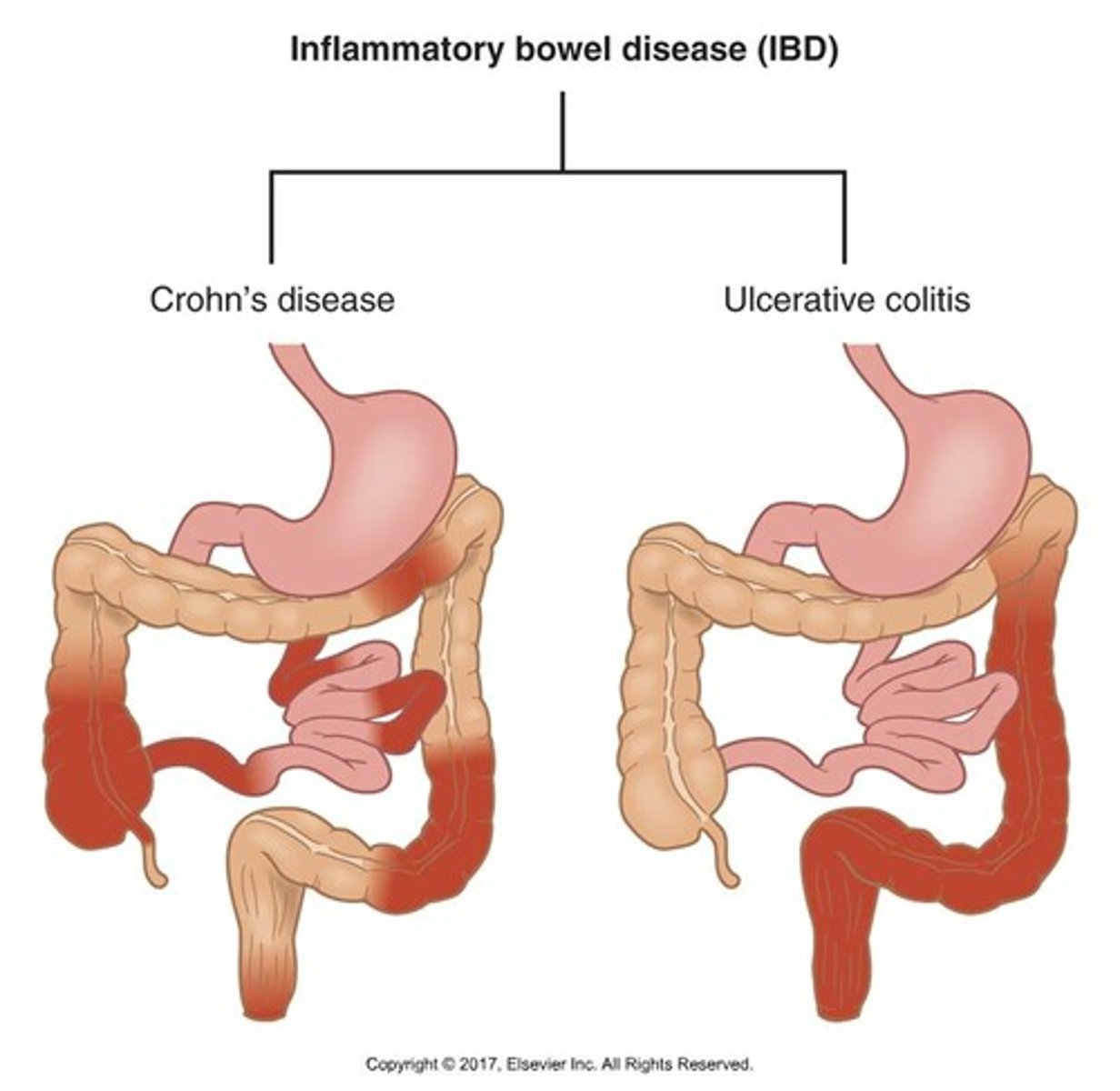
What characterizes the inflammation in Inflammatory Bowel Diseases?
Chronic inflammation of the GI tract with periods of remission and exacerbation.
What are common environmental factors that may contribute to IBD?
Diet, foods, and stress.
Which demographic is at the highest risk for developing IBD?
Individuals of Jewish and middle European descent.
What are some clinical manifestations of IBD?
Abdominal pain, diarrhea, fluid/electrolyte imbalance, fever, weight loss, malnutrition, and anemia.
What diagnostic tests are commonly used for IBD?
CBC, electrolytes, protein levels, ESR, C-reactive protein levels, stool specimens, colonoscopy, ultrasound, CT scan, and MRI of the abdomen.
At what ages is Ulcerative Colitis most commonly diagnosed?
Between ages 15 to 25 and 55 to 65.
How does inflammation spread in Ulcerative Colitis?
It begins in the rectum and then spreads up the colon in a continuous manner.
What are the clinical manifestations specific to Ulcerative Colitis?
Bloody diarrhea (with or without pus and mucus), lower abdominal pain (LLQ), cramping with diarrhea, and systemic symptoms.
What are some complications associated with Ulcerative Colitis?
Bleeding, chronic abdominal pain, toxic megacolon, malabsorption, septic shock, and anemia.
What are the main drug therapies used in the treatment of Ulcerative Colitis?
Antimicrobial, 5 Aminosalicylates, corticosteroids, anticholinergics, sedatives, antidiarrheals, immunosuppressants, immunomodulators, and vitamins.
What surgical options are available for Ulcerative Colitis?
Total proctocolectomy with ileal pouch/ileal anal anastomosis (IPAA), total proctocolectomy with permanent ileostomy, and total proctocolectomy with continent ileostomy (****'s pouch).
What dietary recommendations are suggested for patients with Ulcerative Colitis?
Consult with a dietician for a balanced diet avoiding high fat, dairy, high fiber, and cold foods, along with vitamin/mineral supplements.
What age range is Crohn's Disease most commonly diagnosed?
Between ages 15 to 35.
Where can Crohn's Disease occur in the GI tract?
It can occur anywhere within the GI tract.
What is a characteristic presentation of Crohn's Disease?
Skip lesions, thickening of the bowel wall, narrowing of lumens (strictures), and scarring.
What are some complications associated with Crohn's Disease?
Abscesses, fistulas, peritonitis, and bowel obstructions.
What are the clinical manifestations of Crohn's Disease?
Diarrhea (less severe than UC), possible bleeding (not bright red), abdominal pain, weight loss, and nutritional abnormalities.
What is the typical appearance of diarrhea in Crohn's Disease?
More pus-like diarrhea, and it may not be bright red or fresh.
What is the common surgical intervention for Crohn's Disease?
Surgery is uncommon and usually performed for complications, such as ileostomy to rest the bowel.
What dietary considerations are important for patients with Crohn's Disease?
Consult with a dietician for an elemental diet, similar to baby formula, and ensure proper calculation of nutrients.
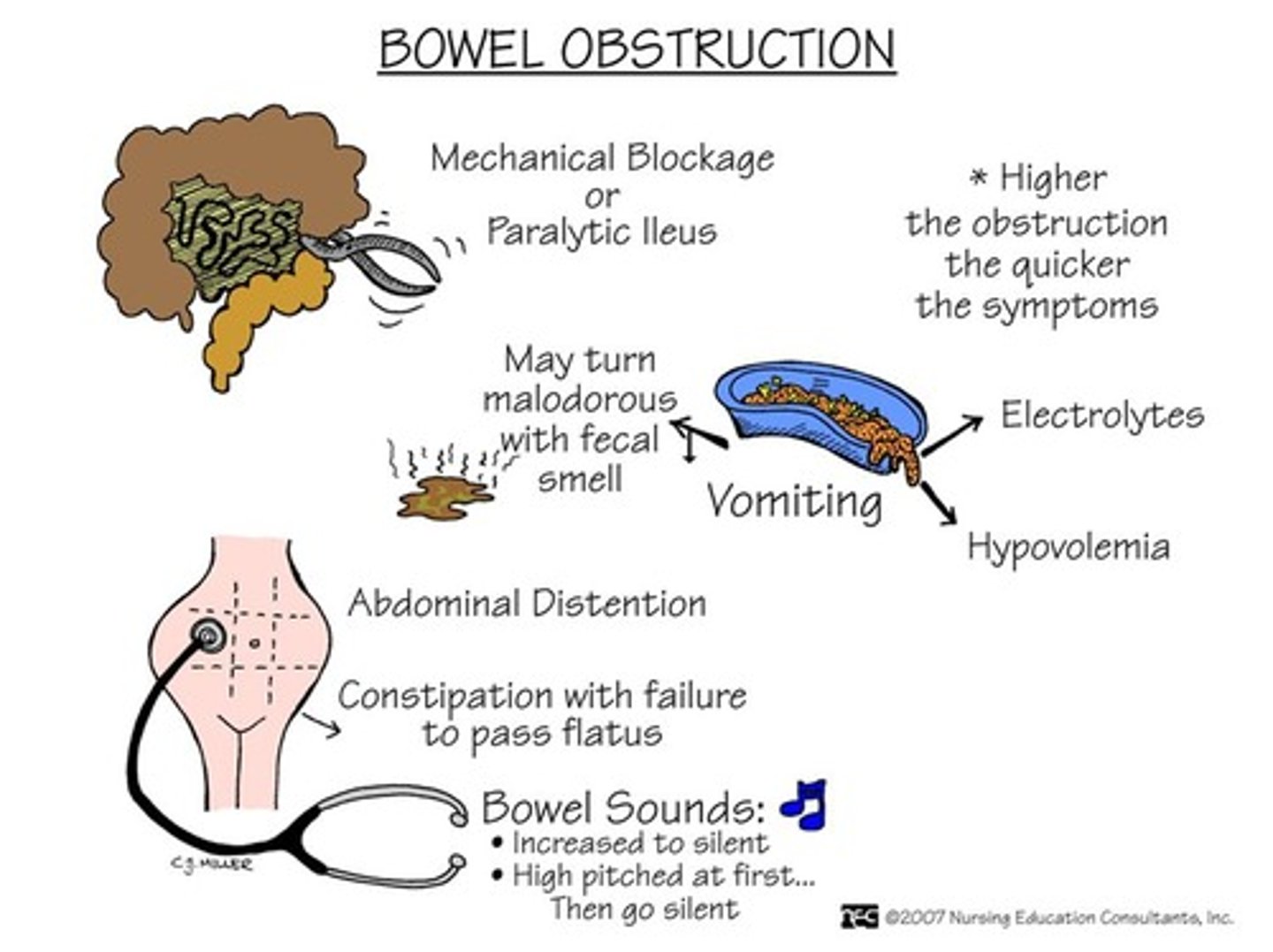
What are the two main types of bowel obstructions?
Mechanical and nonmechanical obstructions.
What causes mechanical bowel obstructions?
Causes include cancer, surgical adhesions, hernias, and strictures from Crohn's disease.
What are the symptoms of mechanical bowel obstructions?
Pain that comes and goes in waves.
What characterizes nonmechanical bowel obstructions?
Constant, generalized discomfort and lack of intestinal peristalsis.
What is a common cause of nonmechanical bowel obstruction?
Paralytic ileus, often post-operative.
What are the symptoms of small bowel obstruction (SBO)?
Projectile vomiting (feces smells), small amounts of liquid stool, and high-pitched bowel sounds.
What are common causes of small bowel obstruction?
Surgical complications, adhesions, hernias, tumors, volvulus, intussusception, and gallstones.
What are the symptoms of large bowel obstruction (LBO)?
Severe constipation lasting 7-10 days, possible abdominal distention, and hypoactive or absent bowel sounds.
What are common causes of large bowel obstruction?
Tumors, volvulus, hernia, adhesions, strictures, diverticular disease, and intussusception.
What happens proximal to a bowel obstruction?
Build-up of fluid, gas, and intestinal contents occurs, leading to increased pressure and distention.
What are classic clinical manifestations of bowel obstruction?
Abdominal pain, nausea & vomiting, distention, and constipation.
What are the differences in clinical manifestations between small and large bowel obstructions?
Small bowel obstruction has rapid onset, colicky pain, frequent nausea/vomiting, and diarrhea; large bowel obstruction has gradual onset, persistent pain, rare vomiting, and no bowel movements.
What diagnostic studies are used for bowel obstructions?
Abdominal X-ray, CT scan, and sometimes Barium enema or colonoscopy.