1. Health Assessment & the Nurse
1/20
Earn XP
Description and Tags
(1/23/24) lecture by sir james d. lim
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
21 Terms
assessment
A deliberate and systematic form of data collection to determine client's current and past health status, functional status and to determine client's present and coping patterns.
purpose: to formulate nursing problems/diagnosis
nursing process
a continuous process of systematic problem-solving method and rational planning method
assessment
most important step that sets the tone for the rest of the process
method to help establish baseline
diagnosis
planning
setting goals and outcomes
implementation
evaluation
types of assessment
comprehensive
thorough and detailed health history & physical examination
examines patient's overall health status
time-consuming
focused
problem-oriented
perform on an on-going basis to monitor and evaluate patient's progress, intervention, and response to treatment
assessment skills
interpersonal/affective skills
assessment is a "feeling" process.
affective skills are needed to develop caring, therapeutic nurse-patient relationships
the quality of assessment depends on the relationship you developed with your patient.
establishing trust and mutual respect is essential before you begin the assessment.
cognitive skills
assessment is a "thinking process"
critical thinking is reflective, reasonable thinking. It is not just doing, it is asking "why?"; it involves inquiry, interpretation, analysis, and synthesis.
a scientific method of problem solving.
needed in clinical decision making.
psychomotor skills
skills needed to perform the four techniques of physical assessment. Most important skill
inspection
palpation
percussion
auscultation
ethical skills
assessment is being responsible and accountable.
patient advocate
respect patients' rights
assure confidentiality
communication
-a process of sharing information and meaning, of sending and receiving messages.
verbal
nonverbal
vocal cues
quality of voice
tone, intensity
speed
action/kinetic cues
body movements
posture, arm position
hand gestures
facial expression, eye contact
object cues
your appearance is equally important
grooming and dress should be appropriate for the situation
communication techniques
affirmation
acknowledges patient's responses.
silence
allow patient to collect his thoughts.
restating
helps clarify and validate what the patient has said.
active listening
conveys interest and acceptance.
broad & general openings
effective when you want to hear what is important to your patient.
use open-ended questions.
how you communicate
genuineness
be open, honest, and sincere with your patient.
respect
everyone should be respected as a person of worth and value.
empathy
knowing what your patient means and understanding how she or he feels.
personal space
the territory surrounding a person that he perceives as private or the physical distance that needs to be maintained for the person to feel comfortable.
defined by culture and situation
four distinct zones
intimate (0-2 ft)
personal (2-4 ft)
social (4-12 ft)
public (more than 12 ft)
touch
person's response to touch depends on trust formed within a relationship.
conveys feelings, such as anger and care.
a. data collection
subjective
covert, not measurable
referred to as “symptoms”
thoughts
beliefs
feelings
sensation
perception
objective
overt, measurable
referred to as "signs"
physical exam
diagnostic studies
sources of data
primary data source
patient
secondary data source
family members
friends
other health providers
old medical records
methods of data collection
interview
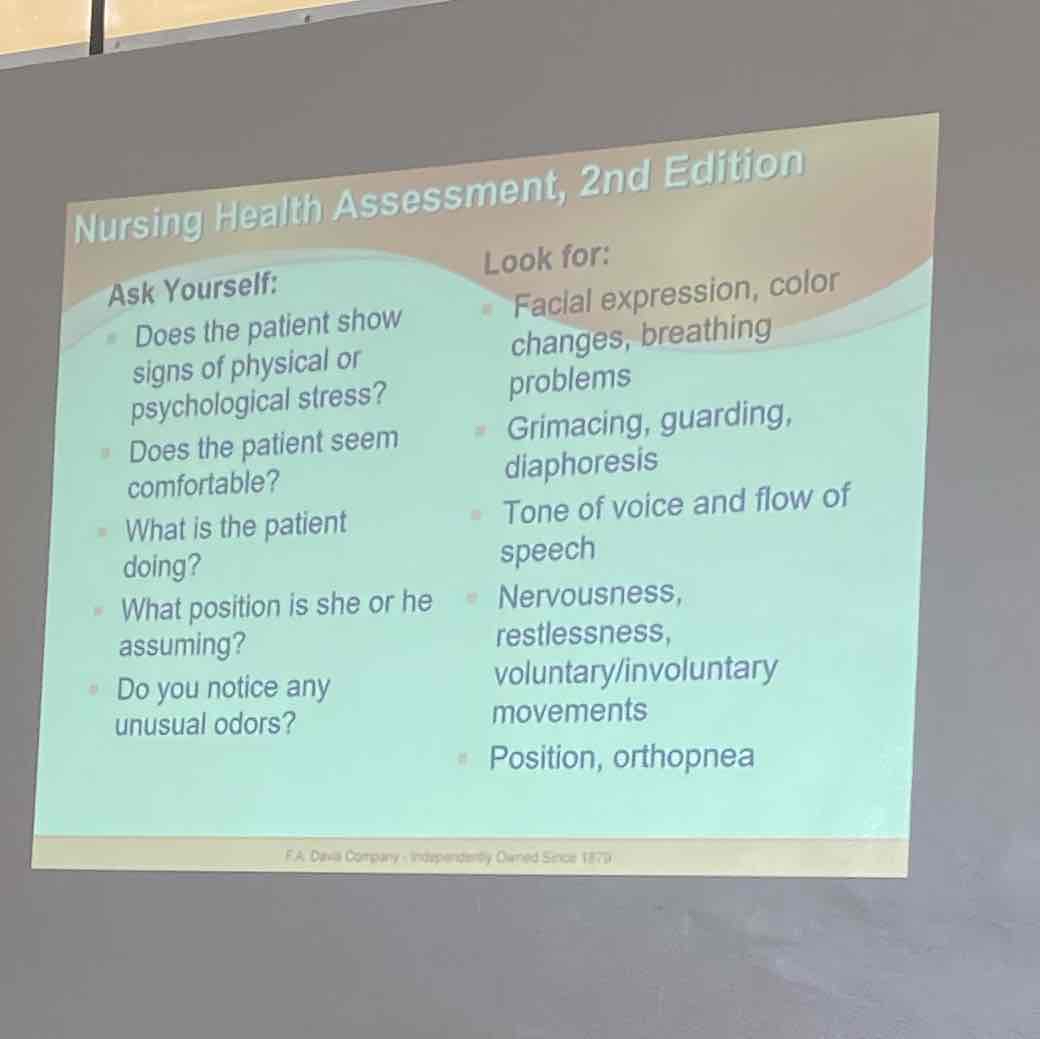
observation
physical assessment
interview
types:
directive
structured with specific questions and controlled by the nurse.
require less time, very effective for obtaining factual data.
non-directive
controlled by the patient.
very effective at eliciting patient's perceptions and feelings.
require more time.
phases of the interview:
introductory phase
introduces self
explains the purpose of interview
explains time frame
working phase
data collection phase
longest phase
termination phase
end of interview
summarize & restate findings
observation
uses all of your senses
examines the patient and environment
physical assessment
inspection
involves looking at your patient and compare her or his appearance with what you know as normal.
palpation
examining with the hands, feeling for organs and masses.
light
use to assess surface characteristics (1")
deep
assess organs and masses (2-3")
percussion
tapping a body surface area to determine the density of a part by the sound it produce.
elicits area of tenderness
rebound tenderness- a clinical sign in which there is pain upon removal of pressure rather than application of pressure to the abdomen.
auscultation
listening to the sounds made by various body structures through a stethoscope.
b. validating data
compare subjective and objective data.
ask patient to validate assessment data.
use other sources to validate data
family members
healthcare providers
old records
diagnostic tests
c. organizing/clustering data
methods:
Maslow's Hierarchy of Needs
Roy's Adaptation Theory
Gordon's Functional Health Patterns
d. prioritizing data
primary or top priority
life-threatening problems
Airway
Breathing
Circulation
secondary
problems affecting basic needs requiring prompt attention to prevent deterioration in patient's condition
pain
tertiary
problems affecting psychosocial needs
anxiety
fear
loneliness
documenting data methods
SOAPIE
subjective data
objective data
assessment/clinical judgment
plan
interventions
evaluation
DAR
data
action
response
PIE
Narrative
documentation tips
be brief and to the point.
use acceptable abbreviations.
if documentation is handwritten, make sure writing is legible.
no need to write in complete sentences.
state the facts. Avoid interpretations.
avoid terms such as "normal," "good," "usual," and "average”.
avoid generalizations.
document sequentially, in chronological order.
do not leave blanks or skip lines.
use correct spelling and grammar.
no erasures or whiting out.
record date and time and sign your full signature